Abstract
Introduction
Invasive lobular carcinoma is the second most common type of invasive breast carcinoma (between 5% and 15%). The incidence of invasive lobular carcinoma has been increasing while the incidence of invasive duct carcinoma has not changed in the last two decades. This increase is postulated to be secondary to an increased use of combined replacement hormonal therapy. Patients with invasive lobular carcinoma tend to be slightly older than those with non-lobular invasive carcinoma with a reported mean age of 57 years compared to 64 years. On mammography, architectural distortion is more common and microcalcifications less common with invasive lobular carcinoma than invasive ductal carcinoma. The incidence of extrahepatic gastrointestinal (GI) tract metastases observed in autopsy studies varies in the literature from 6% to 18% with the most commonly affected organ being the stomach, followed by colon and rectum. Gastric lesions seem to be slightly more frequent, compared to colorectal lesions (6–18% compared to 8–12%, respectively).
Presentation of case
We present the case of a 70-year-old woman who was referred to our institution with a concurrent gastric and rectal cancer that on further evaluation was diagnosed as metastatic invasive lobular carcinoma of the breast. She has a stage IV clinical T3N1M1 left breast invasive lobular carcinoma (ER positive at 250, PR negative, HER-2/neu 1+ negative) with biopsy proven metastases to left axillary lymph nodes, gastric mucosa, peritoneum, rectal mass, and bone who presented with a partial large bowel obstruction. She is currently being treated with weekly intravenous paclitaxel, bevacizumab that was added after her third cycle, and she is also receiving monthly zoledronic acid. She is currently undergoing her 12-month of treatment and is tolerating it well.
Discussion Breast cancer is the most common site-specific cancer in women and is the leading cause of death from cancer for women aged 20–59 years. It accounts for 26% of all newly diagnosed cancers in females and is responsible for 15% of the cancer-related deaths in women.9 Breast cancer is one of the most common malignancies that metastasize to the GI tract, along with melanoma, ovarian and bladder cancer.
Conclusion
We present one of the first reports of metastatic lobular breast cancer presenting as a synchronous rectal and gastric tumors. Metastatic lobular carcinoma of the breast is a rare entity with a wide range of clinical presentations. A high level of suspicion, repetition of endoscopic procedures, and a detailed pathological analysis is necessary for early diagnosis, which might help to avoid surgical treatment due to incorrect diagnosis. Patients with a history of breast cancer who present with new gastrointestinal lesions should have these lesions evaluated for evidence of metastasis through histopathologic evaluation and immunohistochemical analysis. Differentiating between a primary GI lesion and metastatic breast cancer will allow initiation of appropriate treatment and help prevent unnecessary operations.
Keywords: Invasive lobular carcinoma of the breast, Metastatic lobular carcinoma of the breast, Metastatic disease to the rectum and stomach from breast cancer
1. Introduction
Invasive lobular carcinoma is the second most common type of invasive breast cancer. In most series, these tumors account for approximately 5–10% of invasive breast carcinomas. The reported incidence of this tumor type has ranged, between 1% and 20%.1,2 Most of these differences are related to diagnostic criteria as well as the variability in patient populations.2 The incidence of invasive lobular carcinoma has been increasing while the incidence of invasive duct carcinoma has not changed in the last two decades. This increase is postulated to be secondary to an increased use of combined hormonal replacement therapy.3 Patients with invasive lobular carcinoma tend to be slightly older than those with non-lobular invasive carcinoma, with a reported mean age of 57 years compared to 64 years.1 Invasive lobular carcinomas are characterized by multifocality in the ipsilateral breast and appear to be more often bilateral than other types of invasive breast cancer, although the reported range of bilaterality has been broad 96–46%).3,4 On mammography, architectural distortion is more common and microcalcifications less common with invasive lobular carcinoma than invasive ductal carcinoma. At the time of diagnosis, 60% of patients will have lymph node or distant organ metastases, and about 30–80% of patients will develop metastatic disease following surgery and/or chemotherapy, radiotherapy, or endocrine therapy.4
Lobular carcinoma tends to spread to bones, gynecological organs, peritoneum and retroperitoneum, and is less likely to involve the gastrointestinal tract (GI).5–7 The incidence of extrahepatic gastrointestinal (GI) tract metastases observed in autopsy studies varies in the literature from 6% to 18% with the most commonly affected organ being the stomach, followed by colon and rectum. Gastric lesions seem to be slightly more frequent, compared to colorectal lesions (6–18% compared to 8–12%, respectively).8
We present the case of a 70-year-old woman who was referred to our institution with a concurrent gastric and rectal cancer that on further evaluation was diagnosed as metastatic invasive lobular carcinoma of the breast.
2. Presentation of case
This is a 70-year-old woman with a 3-month history of decreased stool caliber, alternating episodes of diarrhea and constipation, and increased flatulence. Two months previously she had a fall from standing height that required her to take codeine. This led to constipation and abdominal pain. She then presented to a local emergency department for persistent abdominal pain where a CT scan of the abdomen and pelvis was performed and interpreted as negative. She subsequently underwent diagnostic colonoscopy demonstrating a circumferential obstructing rectal mass that required the use of a pediatric colonoscope to advance beyond the lesion. The lesion measured 4 cm in length, starting at 3 cm from the anal verge to approximately 7 cm proximally, multiple biopsies where taken. She also underwent upper endoscopy demonstrating an area of mucosal thickening which was biopsied. She had continued intermittent abdominal pain, colicky in nature associated with diarrhea. She lost approximately 10 pounds in a month.
The pathology report from the rectal and gastric biopsies showed non-specific inflammation and poorly differentiated invasive carcinoma which was noted to be ER/PR positive. A repeat CT scan of the abdomen and pelvis revealed circumferential thickening of the rectum. It extended from the junction of the rectum and sigmoid colon towards the anus with two liver lesions 2 mm and 5 mm in size (Fig. 1). On physical examination she was found to have a palpable mass in the left upper outer quadrant of the breast, as well as a left axillary mass.
Fig. 1.

CT scan of the abdomen and pelvis showing the nearly obstructing rectal mass.
Upon further questioning she revealed that approximately 1 year before the onset of her gastrointestinal symptoms she had felt a breast mass, but had never brought it to anyone's attention. A month prior to the onset of her gastrointestinal symptoms she had her annual bilateral screening mammogram that revealed no suspicious masses or lesions. A CT of the chest revealed multiple enlarged left axillary lymph nodes, no mediastinal adenopathy, and a solitary pulmonary nodule in the right upper lobe measuring 6 mm (Fig. 2). Repeat EGD (Fig. 3) and colonoscopy (Fig. 4) with biopsies were done which revealed lobular carcinoma consistent with a breast primary. An ultrasound guided biopsy of the axillary lymph node was performed revealing metastatic invasive lobular carcinoma. She underwent bilateral breast MRI and this again revealed left axillary adenopathy, the largest 3.1 cm × 2.1 cm (Fig. 5). In the posterior lateral central left breast there was a 7.4 cm × 1.8 cm × 6.6 cm area of irregular heterogeneous enhancement. Due to persistent abdominal pain consistent with a partial large bowel obstruction, she underwent exploratory laparotomy with peritoneal nodule biopsy and diverting colostomy. She also underwent rectal mass core biopsy, as well as left breast core biopsy. All of the areas biopsied revealed invasive lobular carcinoma consistent with a breast primary. They were ER positive, PR negative, HER-2/neu 1+ negative.
Fig. 2.

CT scan of the chest showing a right upper lobe nodule and left axillary lymph node.
Fig. 3.
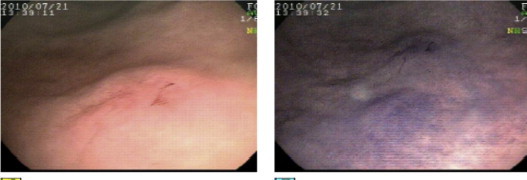
Gastric mucosa thickening and erosion in the fundus.
Fig. 4.

Rectal mass at approximately 5 cm from the anal verge.
Fig. 5.
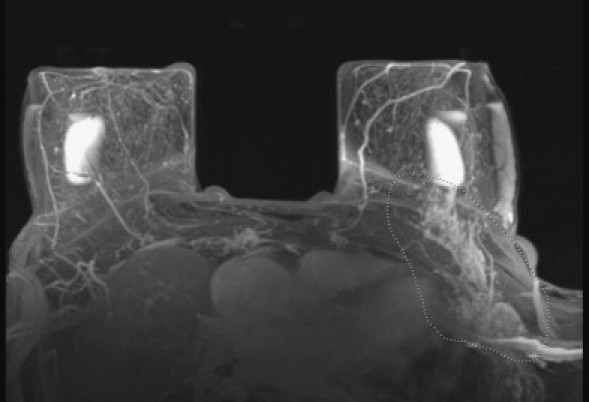
MRI of the breasts showing an abnormality of the left upper outer quadrant.
In summary this 70-year-old woman had a stage IV clinical T3N1M1 left breast invasive lobular carcinoma (ER positive at 250, PR negative, HER-2/neu 1+ negative) with biopsy proven metastases to left axillary lymph nodes, gastric mucosa, peritoneum, rectal mass, and bone who presented with a partial large bowel obstruction. She is currently being treated with weekly intravenous paclitaxel, bevacizumab that was added after her third cycle, and she is also receiving monthly zoledronic acid. She is currently undergoing her 12-month of treatment and is tolerating it well. She has a grade I neuropathy and grade II nail changes which is not interfering with her activities of daily living. Our plan at this point is to continue on her current treatment protocol for one additional cycle and then restage her with a CT scan of the chest, abdomen and pelvis, and bone scan. We did discuss the possibility of taking a break from the paclitaxel if things continue to look good and since she is having painful nail changes. She is ER positive and we could potentially consider antiestrogen therapy at some point in the future.
2.1. Pathology
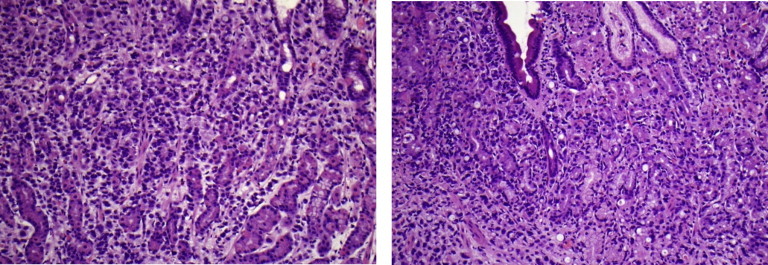
The left breast and axillary lymph node ultrasound guided core biopsy demonstrated metastatic lobular carcinoma. Immunohistochemistry performed with good positive and negative controls revealed tumor cells staining strongly positive for ER (250) and focally positive for CEA and BRST-2. They were negative for CK20, CDX-2 and PR (Figs. 6 and 7).
Fig. 6.
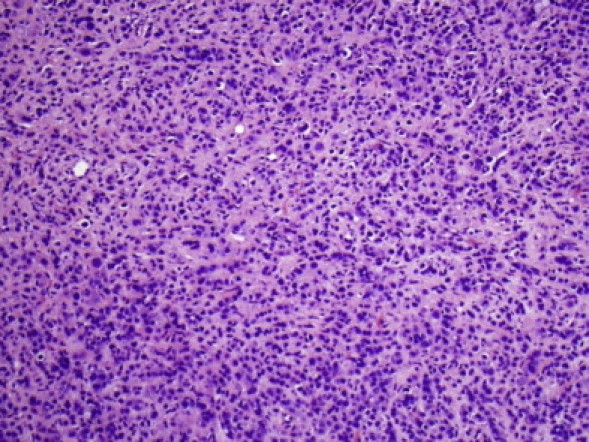
Core needle biopsy of breast mass.
Fig. 7.
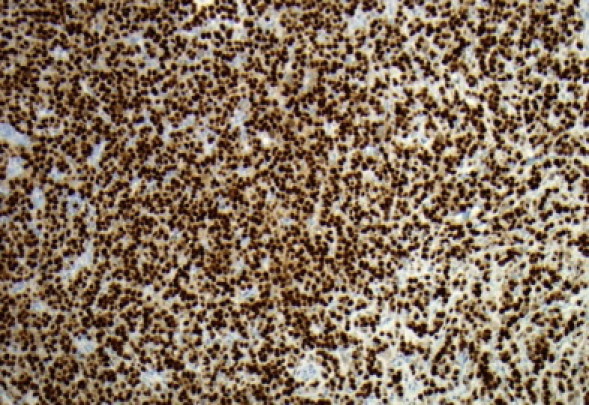
Core needle biopsy of breast mass.
The biopsies obtained from the greater curvature of the stomach and duodenum showed metastatic lobular carcinoma from the breast. Immunohistochemistry performed on the specimen with good positive and negative controls revealed tumor cells staining strongly positive for ER (250) and PR (200) and focally positive for CEA and BRST-2. They were negative for CK20 and CDX-2 (Figs. 8 and 9). The needle core biopsy of the rectum, the multiple biopsies of the peritoneum and falciform ligament also demonstrated metastatic lobular carcinoma from breast (Fig. 10).
Fig. 8.
Gastric and duodenal biopsies.
Fig. 9.
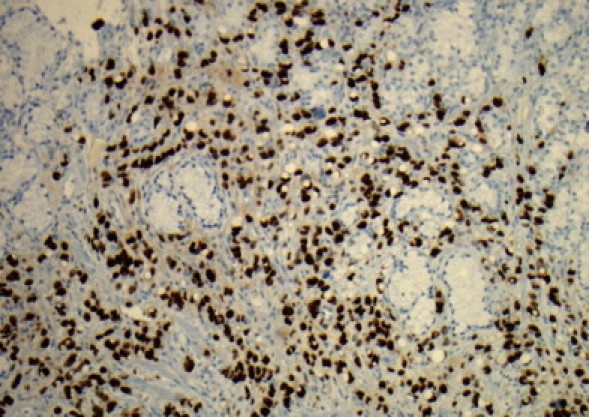
Gastric and duodenal biopsy.
Fig. 10.
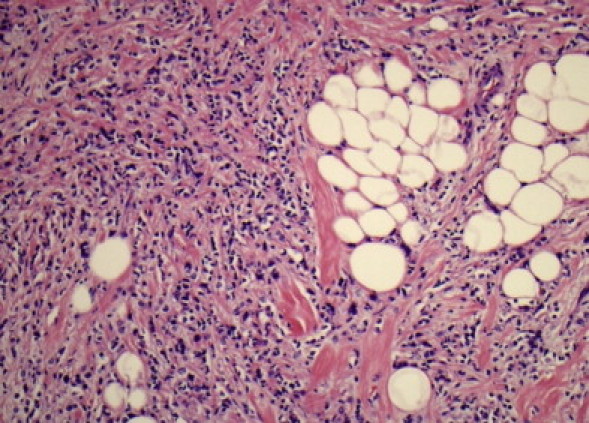
Core biopsy of the rectum.
3. Discussion
Breast cancer is the most common site-specific cancer in women and is the leading cause of death from cancer for women aged 20–59 years. It accounts for 26% of all newly diagnosed cancers in females and is responsible for 15% of the cancer-related deaths in women.9 Breast cancer is one of the most common malignancies that metastasize to the GI tract, along with melanoma, ovarian and bladder cancer.10 Breast cancer rarely metastasizes to the colon or rectum, more commonly metastasizing to the stomach or small bowel. There tends to be a histological preference for the site of distant metastasis, invasive ductal carcinoma of the breast has a tendency to metastasize more commonly to the liver, lung, and brain compared to lobular carcinoma that tends to spread to bones, gynecological organs, peritoneum, retroperitoneum, and the gastrointestinal tract.11,12 The reason for this has not been identified.
An interesting aspect of our case is the involvement not only of the rectum but also of the stomach and peritoneum synchronously. Gastric metastases from mammary carcinomas frequently develop many years after the primary tumor, raising suspicions about a new primary cancer within the stomach. In our case the tumors were synchronous with the primary breast cancer. The time interval between primary breast cancer and gastrointestinal involvement may range from synchronous presentation to as long as 30 years but reverse is also true, with the GI manifestation preceding a diagnosis of breast cancer.13–15 Invasive lobular carcinoma of the breast that metastasizes to the stomach may occur as discrete lesions (nodules, erosions, and/or ulcerations) or as linitis plastica with diffuse infiltration of the submucosa and muscularis propria.
The clinical manifestations that metastatic breast cancer to the GI tract can have are variable. Symptoms may range from non-specific complaints to acute GI symptoms. The diagnosis of metastatic lesions to the GI tract becomes even more unlikely on the rare occasion when it represents the first manifestation of breast cancer.16 In our case the patient presented initially with GI symptoms that made her seek medical attention without taking into account the breast lesion that she had noticed previously.
Histologic diagnosis of metastatic lesions can be difficult. The lack of dysplasia or atypia of the rectal epithelium and the glands surrounding the malignant cells is often helpful in distinguishing between a primary and a metastatic lesion, but immunohistochemistry will allow for the most accurate diagnosis. Markers that help confirm the diagnosis are gross cystic disease fluid protein-15 (GCDFP-15), estrogen (ER) and progesterone (PR) receptors. The GCDFP-15 and the ER and/or PR are positive in metastatic lesions of the breast, in contrast to most colorectal or gastric carcinomas, which are usually negative. One report showed that primary gastric carcinomas can express the ER in approximately 20–28% of the time.17 The signet-ring morphology of lobular carcinoma may mimic gastric carcinoma. Some authors suggest that given the high incidence of breast cancer and the low incidence of diffuse-type gastric cancer in the USA, we should consider the presence of metastatic lobular carcinoma of the breast in every woman diagnosed with diffuse-type gastric cancer.13
Systemic treatment with chemotherapy, endocrine therapy or a combination of both is usually started in patients with breast cancer that metastasize to the GI tract. Remissions are observed in 32–53% of patients.18 Survival after diagnosis of GI metastases from a breast primary is poor with few patients surviving beyond two years, although survival up to nine years has been reported.19,20
4. Conclusion
We present one of the first reports of metastatic lobular breast cancer presenting as a synchronous rectal and gastric tumors. Metastatic lobular carcinoma of the breast is a rare entity with a wide range of clinical presentations. A high level of suspicion, repetition of endoscopic procedures, and a detailed pathological analysis is necessary for early diagnosis, which might help to avoid surgical treatment due to incorrect diagnosis. Patients with a history of breast cancer who present with new gastrointestinal lesions should have these lesions evaluated for evidence of metastasis through histopathologic evaluation and immunohistochemical analysis. Differentiating between a primary GI lesion and metastatic breast cancer will allow initiation of appropriate treatment and help prevent unnecessary operations.
Conflict of interest statement
None
Funding
None
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author's contributions
R.A. was involved in drafting the manuscript and revising it critically for important intellectual content. Has given final approval of the version to be published. P.P. was involved in drafting the manuscript and revising it critically for important intellectual content. Has given final approval of the version to be published. H.J. was involved in revising it critically for important intellectual content. Has given final approval of the version to be published. J.F. was involved in revising it critically for important intellectual content. Has given final approval of the version to be published.
References
- 1.Sastre-Garau X., Jouve M., Asselain B., Vincent-Salomon A., Beuzeboc P., Dorval T. Infiltrating lobular carcinoma of the breast: clinicopathological analysis of 975 cases with reference to data on conservative therapy and metastatic patterns. Cancer. 1996;77:113–120. doi: 10.1002/(SICI)1097-0142(19960101)77:1<113::AID-CNCR19>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 2.Rakha E.A., El-Sayed M.E., Menon S., Lee A.H., Ellis I.O. Histologic grading is an independent prognostic factor in invasive lobular carcinoma of the breast. Breast Cancer Res Treat. 2008;111:121–127. doi: 10.1007/s10549-007-9768-4. [DOI] [PubMed] [Google Scholar]
- 3.Li C.I., Anderson B.O., Daling J.R., Moe R.E. Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA. 2003;289:1421–1424. doi: 10.1001/jama.289.11.1421. [DOI] [PubMed] [Google Scholar]
- 4.Bamias A., Baltayiannis G., Kaminam S., Fatouros M., Lymperopoulos E., Agnanti N. Rectal metastases from lobular carcinoma of the breast: report of a case and literature review. Ann Oncol. 2001;12:715–718. doi: 10.1023/a:1011192827710. [DOI] [PubMed] [Google Scholar]
- 5.Santini D., Altomare A., Vincenzi B., Perrone G., Bianchi A., Rabitti C. An increase of CA 19.9 as the first clinical sign of ileocecal valve metastasis from breast cancer. In Vivo. 2006;20:165–168. [PubMed] [Google Scholar]
- 6.Aurello P., D’Angelo F., Cosenza G., Petrocca S., Stoppacciaro A., Ramacciato G. Gastric metastasis 14 years after mastectomy for breast lobular carcinoma: a case report and literature review. Am J Surg. 2006;72:456–460. [PubMed] [Google Scholar]
- 7.Ayantunde A.A., Agrawal A., Parsons S.L., Welch N.T. Esophagogastric cancers secondary to a breast primary tumor do not require resection. World J Surg. 2007;31:1597–1601. doi: 10.1007/s00268-007-9099-y. [DOI] [PubMed] [Google Scholar]
- 8.Cervi G., Vettoreto N., Vinco A., Cervi E., Villanacci V., Grigolato P. Rectal localization of metastatic lobular breast cancer. Dis Colon Rectum. 2001;44:453–455. doi: 10.1007/BF02234749. [DOI] [PubMed] [Google Scholar]
- 9.Jemal A., Siegel R., Ward E., Hao Y., Xu J., Murray T. Cancer statistics 2008. CA Cancer J Clin. 2008;58:71. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 10.Washington K., McDonagh D. Secondary tumours of the gastrointestinal tract: surgical pathologic findings and comparison with autopsy series. Mod Pathol. 1995;8(4):427–433. [PubMed] [Google Scholar]
- 11.Harris M., Howell A., Chrissohou M., Swindell R.I., Hudson M., Sellwood R.A. A comparison of the metastatic pattern of infiltrating lobular carcinoma and infiltrating ductal carcinoma of the breast. Br J Cancer. 1984;50:23–30. doi: 10.1038/bjc.1984.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamovec J., Bracko M. Metastatic pattern of infiltrating lobular carcinoma of the breast: an autopsy study. J Surg Oncol. 1991;48:28–33. doi: 10.1002/jso.2930480106. [DOI] [PubMed] [Google Scholar]
- 13.Schwarz R., Klimstra D., Turnbull A. Metastatic breast cancer masquerading as gastrointestinal primary. Am J Gastroenterol. 1998;93:111–114. doi: 10.1111/j.1572-0241.1998.111_c.x. [DOI] [PubMed] [Google Scholar]
- 14.Clavien P.A., Laffer U., Torhost J., Harder F. Gastro-intestinal metastases as first clinical manifestation of the dissemination of a breast cancer. Eur J Surg Oncol. 1990;16:121–126. [PubMed] [Google Scholar]
- 15.Benfiguig A., Anciaux M.L., Eugene Cl., Benkémoun G., Etienne J.C. Gastric metastasis of breast cancer occurring after a cancer-free interval of 30 years. Ann Gastroentetol Hepatol. 1992;28:175–177. [PubMed] [Google Scholar]
- 16.Van Halteren H.K., Peters H., Gerlag P.G.G. Large bowel mucosal metastases from breast cancer. J Clin Oncol. 1998:16-3711–16-3713. doi: 10.1200/JCO.1998.16.11.3711. [DOI] [PubMed] [Google Scholar]
- 17.Tokunaga A., Nishi K., Matsukura N., Tanaka N., Onda M., Shirota A. Estrogen and progesterone receptors in gastric cancer. Cancer. 1986;57:1376–1379. doi: 10.1002/1097-0142(19860401)57:7<1376::aid-cncr2820570722>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 18.Deogracias M., Jaime L., Camisón I., Zamacola I., Murillo Guibert J., Suescun García R. Rectal metastasis from lobular breast carcinoma 15 years after primary diagnosis. Clin Transl Oncol. 2010;12:150–153. doi: 10.1007/S12094-010-0481-0. [DOI] [PubMed] [Google Scholar]
- 19.Taal B.G., den Hartog Jager F.C.A., Steinmetz R., Peterse H. The spectrum of gastrointestinal metastases of breast carcinoma. Gastrointest Endosc. 1992;38:136–141. doi: 10.1016/s0016-5107(92)70378-2. [DOI] [PubMed] [Google Scholar]
- 20.Bamias A., Baltayiannis G., Kamina S. Rectal metastases from lobular carcinoma of the breast: report of a case and literature review. Ann Oncol. 2001;12:715–718. doi: 10.1023/a:1011192827710. [DOI] [PubMed] [Google Scholar]


