Abstract
INTRODUCTION
Persistent sciatic artery (PSA) is a rare vascular anomaly associated with a higher rate of aneurysm formation or thromboembolic complications causing lower extremity ischemia.
PRESENTATION Of Case
A 15-year-old female patient with bilateral PSA presented with lower extremity ischemia. Considering the age and symptoms of the patient, we did not perform any intervention, but continued surveillance with duplex ultrasonography in case of the high incidence of aneurysmal formation or thromboembolic event.
DISCUSSION
Epidemiology, development, anatomical structure, diagnosis and treatments of PSAs are discussed.
CONCLUSION
PSAs, are prone to early atheromatous degeneration and aneurysm formation. Treatment of a PSA mainly dependent on the symptoms is either by surgical procedures or by endovascular interventions.
Keywords: Sciatic artery, Arterial anomaly, Angiography, Ischemia, Embryology
1. Introduction
Persistent sciatic artery (PSA) is an unusual anatomical anomaly first reported in 18321 and was described angiographically by Cowie2 in 1960. The sciatic artery is a continuation of the internal iliac artery and serves as the major blood supply for the lower limb bulb in the early embryonic stage, and it normally involutes and is replaced by the iliofemoral artery as the fetus develops.3 The failure to regress, sometimes associated with femoral arterial hypoplasia, and therefore becoming the dominant inflow to the lower extremity is called persistent sciatic artery.4–6 PSA is a rare vascular anomaly associated with a higher rate of aneurysm formation or thromboembolic complications causing lower extremity ischemia.7–9 We report a 15-year-old female patient with bilateral PSA suffering from lower extremity ischemia.
2. Presentation of case
A 15-year-old girl was admitted for vascular evaluation because of bilateral calf claudication affecting both legs after 500 m. There was no history of trauma, and physical examination revealed the femoral and popliteal pulses were impalpable, and the posterior tibial and dorsalitis pedis pulses were absent. Her feet were cold with poor capillary refilling. Color duplex sonography suggested poor distal flow in both superficial femoral arteries. Subsequently, angiography (Fig. 1) was undertaken with unexpected results of bilateral persistent sciatic arteries identified. The bilateral internal iliac arteries were larger in caliber than the external iliac arteries and were continuous with persistent sciatic arteries that continued into the posterior aspect of the thigh, and reached the popliteal arteries through the popliteal fossae. The bilateral external iliac, common femoral and proximal superficial femoral arteries were incompletely developed. Considering the age and symptoms of the patient, we did not perform any intervention, but continued surveillance with duplex ultrasonography in view of the high incidence of aneurysmal formation or thromboembolic event.
Fig. 1.
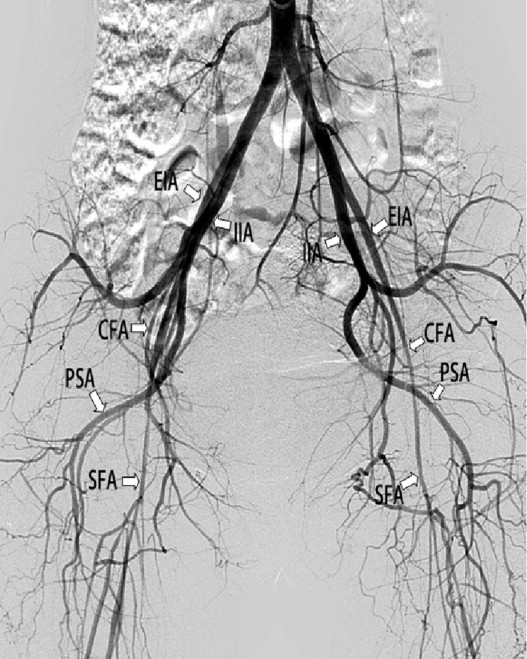
Bilateral external iliac artery (EIA), common femoral artery (CFA) and superficial femoral artery (SFA) are hypoplastic. Bilateral internal iliac artery (IIA) continues as the inferior gluteal artery and persistent sciatic artery (PSA).
3. Discussion
PSA is a rare arterial embryologic anomaly reported in 0.025–0.04% of people.10 It occurs on the right in 50% of cases, on the left in 20%, and bilaterally in 30%.11 It affects both genders equally and can occur at any age after puberty. The average age of symptomatic presentation was approximately 44 years.
The sciatic artery is a branch of the umbilical artery and the principal arterial supply of the developing lower limb during the 6 mm stage of embryonic development. By the third month, the upper portion of the sciatic artery atrophies and is replaced by the femoral artery, which develops from the external iliac artery. Meanwhile, the umbilical artery develops into the internal iliac artery. The only remnants of sciatic artery present at birth are the inferior gluteal artery, the distal popliteal artery, and the peroneal artery3 (Fig. 2).
Fig. 2.
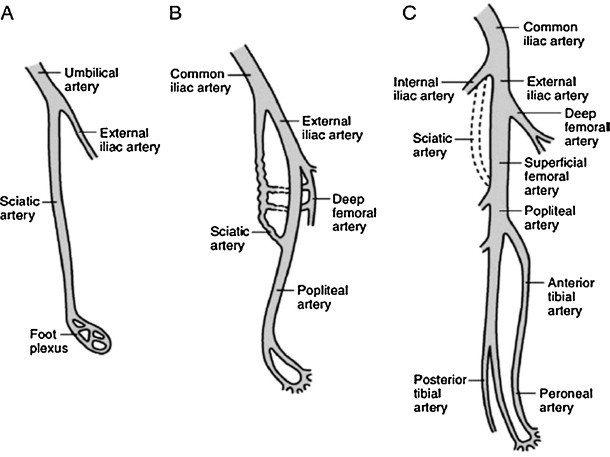
Arterial supply to the left lower extremity. (A) Sciatic artery forming as a branch of the umbilical artery initially supplies the entire leg. (B) The sciatic artery regresses, and the external artery develop into the common femoral artery to supply the thigh. Note that the sciatic artery communicates with the popliteal artery just above the knee. (C) The sciatic artery disappears, although small portions remain to form the popliteal and peroneal arteries.3
When the sciatic artery persists, it is usually a tortuous and enlarged vessel. Commonly, the internal iliac artery has a larger diameter than the external iliac artery, supplying blood to the lower leg through the PSA. And the superficial femoral artery may be normal in diameter, hypoplastic, or absent. PSA is classified as complete or incomplete. In incomplete persistent sciatic arteries, as in our patient, no continuous connection exists between iliac artery and the popliteal artery, but rather, the sciatic artery connects to the distal popliteal system via collateral connections. A complete persistent sciatic artery is directly contiguous from the internal iliac to the anterior tibial, posterior tibial, and peroneal artery trifurcation.3,4,6,12
The sciatic artery starts at the internal iliac artery and runs through the greater sciatic foramen, from where its course is close to the sciatic nerve. In some cases, the sciatic artery actually lies inside the sciatic nerve sheath. Distally, the artery lies deep in the major gluteal muscle and follows a course along the adductor magnus muscle. Finally, the sciatic artery reaches the popliteal artery running through the popliteal fossae, lateral to the insertion of the adductor magnus muscle.
PSA is often asymptomatic until a complication develops, and the diagnosis of PSA relies on patient presentation and physical examination. Patients present with claudication, lower extremity ischemia caused by thrombosis or distal embolization, painful pulsatile buttock mass, and sciatic neuropathy caused by sciatic nerve compression. The presence of Cowie's sign suggests persistent sciatic artery, which is the absence of a femoral pulse but the presence of distal pulses. Some of the cases were found incidentally by radiologic or autopsy findings. In our case, the normal size of bilateral common femoral arteries and the tapering change of the superficial femoral arteries further misled us to have an initial impression of acute obstruction at the lower level of the left superficial femoral artery with chronic atherosclerotic change. In our case, so it was neglected initially.
Contrast angiography, the most frequently used diagnostic tool to detect PSA, would provide information about the classification and outflow of the PSA, and it is essential for determining the pattern of the existing vasculature and providing appropriate treatment. CTA and magnetic resonance imaging angiography have been demonstrated to be useful in determining the presence and size of an aneurysm, the relationship of the local vascular structures to the bony landmarks, the course of the PSA, and progression after treatment.13 Other diagnostic tools such as color duplex scanning was helpful in demonstrating that the femoropopliteal system was probably developmentally normal but secondarily occluded by an old embolic event or, less likely, atherosclerosis. Color duplex scanning via a posterior approach also allowed identification of the persistent sciatic artery and its collateralization of the above-knee popliteal artery.
Although most asymptomatic PSAs are not discovered, persistent sciatic arteries, unlike the fully developed femoral arteries, are prone to early atheromatous degeneration and aneurysm formation. Generally, the aneurysm develops in the buttocks between the pyriform muscle and the posterior aspect of the greater trochanter of the femur – the site where the PSA has a slight S-shaped curve.14 The exact reason why an aneurysm is frequently seen in a PSA is unknown. Hypoplasia of the elastic components and the primitive arterial wall may be a factor in these pathological changes. The incidence of persistent sciatic artery aneurysm formation is reported to occur with 15–40%, resulting in aneurysm thrombosis, embolization, rupture and radicular pain of the involved limb,15 while stenosis and occlusions of the PSA are also frequently reported with an incidence of 7% and 9%, respectively. These complications may lead to an amputation in 8% of the cases.16
Treatment of a PSA is mainly dependent on the symptoms, the vascular anatomy of the sciatic artery and the iliofemoral system, the presence of concurrent vascular occlusive disease, and the presence or absence of aneurysm. Treatment is either by surgical procedures or by endovascular interventions. PSA aneurysm can be obliterated via ligation, resection, embolization, or endovascular stent graft. Vascular reconstruction can be performed by femoral–popliteal bypass, iliopopliteal transobturator bypass or interposition bypass.17 End-to-end graft reconstruction after aneurysmectomy using autologous venous graft and/or prosthetic graft is another option. PSA without aneurysmal formation in an asymptomatic patient does not require any intervention; however, continued surveillance, usually with duplex ultrasonography, is required because of the high incidence of aneurysmal formation or thromboembolic event.
4. Conclusions
Persistent sciatic artery is a rare arterial embryologic anomaly, and PSAs are prone to early atheromatous degeneration and aneurysm formation. Treatment of a PSA is mainly dependent on the symptoms either by surgical procedures or by endovascular interventions.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author's contributions
Bin Wang contributed in writing, data collection, and literature review.
Zhenjie Liu contributed in writing, data collection, and literature review.
Laigen Shen contributed in study design, manuscript editing and supervision.
References
- 1.Green P. On a new variety of the femoral artery. Lancet. 1832:1730–1732. [Google Scholar]
- 2.Cowie T.N., Mckellar N.J., McLean N., Smith G. Unilateral congenital absence of the external iliac and femoral arteries. Br J Radiol. 1960;33:520–522. doi: 10.1259/0007-1285-33-392-520. [DOI] [PubMed] [Google Scholar]
- 3.Sidway A.N. Embryology of the vascular system. In: Rutherford R.B., editor. Vascular surgery. 6th ed. Elsevier; Philadelphia: 2005. pp. 53–63. [Google Scholar]
- 4.Kritsch D., Hutter H.P., Hirschl M., Katzenschlager R. Persistent sciatic artery: an uncommon cause of intermittent claudication. Int Angiol. 2006;25(3):327–329. [PubMed] [Google Scholar]
- 5.Patel S.N., Reilly J.P. Persistent sciatic artery – a curious vascular anomaly. Catheter Cardiovasc Interv. 2007;70(2):252–255. doi: 10.1002/ccd.21205. [DOI] [PubMed] [Google Scholar]
- 6.Brancaccio G., Falco E., Pera M., Celoria G., Stefanini T., Puccianti F. Symptomatic persistent sciatic artery. J Am Coll Surg. 2004;198(1):158. doi: 10.1016/j.jamcollsurg.2003.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Hiki T., Okada Y., Wake K., Fujiwara A., Kaji Y. Embolization for a bleeding pelvic fracture in a patient with persistent sciatic artery. Emerg Radiol. 2007;14(1):55–57. doi: 10.1007/s10140-006-0569-6. [DOI] [PubMed] [Google Scholar]
- 8.Littler P., Blair S.D., Lea S. Angioplasty via retrograde popliteal approach in a stenosed persistent sciatic artery. Eur J Vasc Endovasc Surg. 2007;34(6):719–722. doi: 10.1016/j.ejvs.2007.04.026. [DOI] [PubMed] [Google Scholar]
- 9.Shiwan K.S., Nghi B.P., Snehal D., Richardson C.J. Symptomatic persistent sciatic artery in a newborn. J Pediatr Surg. 2008;43(9):1741–1744. doi: 10.1016/j.jpedsurg.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 10.Donovn D.L., Sharp W.V. Persistent sciatic artery: two cases reports with emphasis on embryologic development. Surgery. 1984;95(3):363–366. [PubMed] [Google Scholar]
- 11.SreeKumar K.P., Prabhu N.K., Moorthy S. Bilateral persistent sciatic artery: demonstration of the anomaly and its complications with intra arterial contrast enhanced spiral CT. Indian J Radiol Imaging. 2004;14:205–207. [Google Scholar]
- 12.Como J.J., Cooper C., Mirvis S.E., Scalea T.M. Penetrating trauma to a persistent sciatic artery. J Trauma. 2005;59(1):246–248. doi: 10.1097/01.ta.0000174368.40268.75. [DOI] [PubMed] [Google Scholar]
- 13.Michel C., Marcus C., Clement C., Wejroch P., Devy-Michel A., Menanteau B. Persistent sciatic artery: findings using spiral CT. J Radiol. 2002;83:1847–1849. [PubMed] [Google Scholar]
- 14.Paraskevas G., Papaziogas B., Gigis J., Mylonas A., Gigis P. The persistent of the sciatic artery. Folia Morhol. 2004;63(4):515–518. [PubMed] [Google Scholar]
- 15.Ertuk S.M., Tatli S. Persistent sciatic artery aneurysm. J Vasc Interv Radiol. 2005;16(10):1407–1408. doi: 10.1097/01.RVI.0000175323.74112.FC. [DOI] [PubMed] [Google Scholar]
- 16.Van Hooft I.M., Zeebregts C.J., van Sterkenburg S.M., de Vries W.R., Reijnen M.M. The persistent sciatic artery. Eur J Vasc Endovasc Surg. 2009;37(5):585–591. doi: 10.1016/j.ejvs.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 17.Batchelor T.J., Vowden P. A persistent sciatic artery aneurysm with an associated internal iliac artery aneurysm. Eur J Vasc Endovasc Surg. 2000;20(4):400–402. doi: 10.1053/ejvs.2000.1182. [DOI] [PubMed] [Google Scholar]


