Abstract
Adolescents who abuse substances are more likely to engage in health-risking sexual behavior (HRSB) and are at particularly high risk for HIV/AIDS. Thus, substance abuse treatment presents a prime opportunity to target HIV-risk behaviors. The present study evaluated a one-session HIV-risk intervention embedded in a controlled clinical trial for drug-abusing adolescents. The trial was conducted in New Mexico and Oregon with Hispanic and Anglo adolescents. Youths were randomly assigned to individual cognitive behavior therapy (CBT) or to an integrated behavioral and family therapy (IBFT) condition, involving individual and family sessions. The HIV-specific intervention was not associated with change. IBFT and CBT were both efficacious in reducing HIV-risk behaviors from intake to the 18-month follow-up for high-risk adolescents. For low-risk adolescents, CBT (versus IBFT) was more efficacious in suppressing HRSB. These data suggest that drug abuse treatments can have both preventative and intervention effects for adolescents, depending on their relative HIV-risk.
Keywords: Adolescent, Substance-abuse, Treatment, HIV-risk
Introduction
Health-risking sexual behavior (HRSB) among young people is a national research priority. Nearly two-thirds of individuals who acquire sexually transmitted diseases (STDs) in the U.S. are under the age of 25 [1]. Although the estimated number of HIV/AIDS cases decreased among children under age 13 from 2001 to 2004, increases were noted in adolescents and young adults up to age 24 [2]. Nearly half of teens are sexually active and a vast proportion of these contacts are unprotected, as evidenced by extremely low rates of consistent condom use and high rates of STDs, especially among sexually active youth between ages 15–19 [3, 4].
A greater understanding of the etiology and treatment of HRSB among young people are a national research priority that is closely linked to substance use and abuse. As with adults, in whom this relationship has been evident for decades [5, 6], adolescents who abuse substances are more likely to practice sexually risky behaviors [7–11] and thus are at particularly high risk for HIV/AIDS or other STDs. Adult studies [12] found this to be the case for both injection drug users (IDU) and non-IDUs, the latter most likely to occur among adolescents. Increasingly, programs with addiction treatment appear to be one of the best avenues for providing infection-related healthcare [13]. Moreover, a prime route of access to drug treatment is the criminal justice system. Given that the majority of adolescent referrals for drug treatment come from this source [14], adolescent substance abuse treatment, therefore, presents a prime opportunity for intervention on HIV/AIDS risk behaviors [15–17].
Treatment for Adolescent Drug Abuse and HIV-Risk Behaviors
Individual cognitive behavioral model treatments (CBT) and family-based interventions have garnered substantial empirical support in controlled clinical trials evaluating their efficacy for adolescent substance abuse and dependence [18]. Significant reductions in substance use from pre- to post-treatment and follow-up periods, for both approaches across multiple studies have been shown [19, 20]. However, interventions for drug abuse in adolescents have not often examined any potential impact on risky sexual behavior.
Intervention and prevention efforts directed at individual change such as CBT have been shown to reduce the incidence of HRSB in adolescent populations and in a variety of formats [9, 21–24]. Large scale school and community based programs have been offered with at-risk youth populations. These structured, small group programs, based on social learning and cognitive behavioral intervention models, have focused on providing information on HIV-risk and condom use, development of social skills to reduce sexual risk-taking behavior, and general cognitive-behavioral skills such as decision-making and assertive communication. Behavioral findings from these studies demonstrate more frequent condom use, fewer sexual partners [25, 26] and delayed initiation of sexual intercourse [27, 28]. Further, Kirby et al., [29] found that these curriculum-based programs worked across cultures and communities. However, with some exceptions, individual-based programs have not realized long-term maintenance of effects [30] and other more extensive forms of intervention have been recommended [31, 32].
Family-based interventions for risky sexual behavior have been evaluated in several randomized control trials (RCT). Prado et al. [33] showed that the inclusion of the family reduced the incidence of HRSB. Other large scale programs such as PARE [34] and CHAMP [35] were successful family interventions targeting both HIV-risk and early pregnancy prevention with elementary and middle school students by enhancing family communication, family decision-making, parent monitoring, and education about HIV-risk and reproduction. However, programs offered in health care and medical settings focus more on prevention aspects and provide services in the context of addressing other health care needs of adolescents. Other prevention programs occur in the school and community context. Although results have been generally modest [31], significant effects have been noted in increased use of condoms [36] and behaviors related to risky sexual behavior such as parent-adolescent communication [37], parenting behavior [38], and drug use [33]. With few exceptions [33], the interventions have not shown effects on risky sexual behavior, not surprising in prevention studies with somewhat younger populations. Nevertheless, both individual and family-based approaches have the potential for reducing HRSB in adolescent populations.
Theoretically, family-based interventions [39, 40], generally conceptualize alcohol and drug abuse as problems that develop and are maintained in the context of maladaptive family relationships. Consequently, treatment focuses on improving relationships among all family members based on the supposition that such improvements will reduce addictive behaviors and possibly, HRSB as well. Improved relationships should result in increases in parent–adolescent communication, and subsequently in lower levels of drug use. Cognitive-behavioral approaches conceptualize substance abuse and related problems such as HRSB as learned behaviors that are initiated and maintained in the context of environmental factors. Modules often include self-monitoring, avoidance of stimulus cues, altering reinforcement contingencies, and coping-skills training to manage and resist urges to use. In addition, other skills-focused interventions (e.g., drug and alcohol refusal skills, communication, problem solving, assertiveness), mood regulation (e.g., relaxation training, anger management, modifying cognitive distortions), and relapse prevention are incorporated to promote sobriety [41, 42] and foster abstinence or safe sexual practices [9, 25, 43]. Because research on interventions for substance abuse and HIV-risk behavior has demonstrated the effectiveness of training in similar cognitive-behavioral skills (e.g., refusal skills), a combined approach offers an opportunity to treat both problems in a single intervention. For example, studies with adults have shown marked reductions in risky sexual behavior following treatment for drug abuse [5] most likely due to reductions in behaviors that are mediators of HIV-risk such as multiple sex partners, unprotected sex and drug use [44].
Moderators of Treatment Effects: Level of HIV-Risk and Ethnicity
Although prevention and intervention efforts for HIV-risk behaviors have been demonstrated, what is less well understood is the impact of an intervention on different subgroups of individuals, such as those with low versus elevated HRSB, and those in different racial/ethnic groups. For example, several studies have shown that interventions may be more effective for sexually experienced youth as opposed to those less experienced [45, 46], although positive effects have been shown for the latter as well [45]. Thus, interventions that have both preventative (suppressing normal increases in risky sexual behavior) and intervention effects (reducing frequency of these behaviors) could be considered more desirable.
HIV infection rates are especially high for ethnic minorities [15, 47]. Hispanics have the second highest rate of AIDS and Hispanic adolescents account for 18% of those diagnosed with AIDS [2]. Hispanic youth also report higher use of drugs compared to non-Hispanic whites or Anglos [48, 49] increasing the likelihood of problematic sexual behavior. Early sexual initiation, multiple partners and lower condom use have all been shown to be more problematic for Hispanic youth than non-Hispanic whites [2, 50], all of which are significant predictors of STDs and HIV. Yet, with some exceptions [45, 51], there has been a paucity of well-designed interventions to reduce HRSB among Hispanic youth. Villarruel et al. [51] found that a 2-day culturally specific group intervention compared to a health-promotion control condition, did significantly reduce the frequency of sexual intercourse, number of partners, and simultaneously increase the frequency and consistency of condom use during sexual activity over a 12-month follow-up period. However, their intervention, as did most others, occurred within the context of the school and generally did not focus on drug use as a related behavior. Villaruel et al.’s [51] health promotion control condition included a focus on drug use but did not report any effects on drug behavior. Several studies have examined drug abuse interventions or integrated drug abuse and HIV interventions among juvenile offenders [9, 17], but most of these were within residential settings with effects assessed after discharge. More recently, Liddle et al. [52] reported a family-based intervention that moved from detention to the community, but no impact on risky sexual behavior was offered.
The Current Study
The present study evaluated an HIV-risk intervention that was imbedded in a large-scale RCT for drug abusing adolescents. A 1-session HIV-risk module was provided during the latter part of the drug intervention. The trial was conducted in both New Mexico and Oregon with both Hispanic and Anglo adolescents who had been referred for drug abuse and/or dependence. Two types of interventions were conducted for drug abuse, an individual CBT [20] and an integrated model that combined aspects of both family therapy and individual CBT. In the Integrative Behavioral and Family Therapy (IBFT) [18, 53] model, the family-based sessions followed Functional Family Therapy (FFT) [39, 54], a widely disseminated, highly effective intervention for youth presenting with a variety of problems that has been shown to be efficacious for drug-abusing youth [20]. Core individual CBT sessions (e.g., coping with urges and cravings, substance refusal skills) were included in the course of IBFT. Prior research has supported combining family and individual CBT strategies [55, 56]. The HIV-risk module was implemented near the end of treatment for adolescents in both conditions. However, not all participants received the module because of attrition or an incomplete course of therapy. It was hypothesized that adolescents receiving the HIV-risk module would show significant reductions on a range of risky sexual behaviors following substance abuse treatment.
Methods
Sample Characteristics and Recruitment Procedures
Adolescents were referred to our clinics for outpatient substance abuse treatment. Primary referral sources included the juvenile justice system, the public school system, community-based service providers (e.g., hospitals, clinics, youth and family social services) and local advertisements. Eligibility criteria for adolescent participant in the study were (a) ages 13–19, (b) DSM-IV diagnostic criteria for substance abuse or dependence, and (c) residing with at least one parent or legal guardian willing to participate in the clinical and research procedures. Adolescents excluded from the study were referred elsewhere for treatment given evidence of (a) a psychotic disorder or condition, or (b) the need for more restrictive or intensive services. Of the 263 adolescents enrolled in the clinical trial, the sample for the current study (n = 225) included only adolescents who received at least a minimal dose of four treatment sessions, had complete data on at least one of the post-treatment assessments and were of either Anglo or Hispanic ethnicity.
Sixty percent of the study sample was recruited from greater Albuquerque, NM with the remaining 40% from Salem, Woodburn and Portland, Oregon. The adolescent sample was 83% male (consistent with most treatment studies of drug abuse), ranged in age from 13 to 19 years (M = 15.8; SD = 1.21), with 51% of Hispanic ethnicity and the remainder White non-Hispanic or Anglos. None of the Hispanic adolescents was monolingual Spanish speaking; however, nearly half of the Hispanic parents preferred or spoke Spanish, and were provided with questionnaires, interviews, and therapy sessions in Spanish.
Adolescents accepted into the study reported substance use (other than tobacco) an average of 46.0 % (SD = 30.5) of the previous 90 days. The most frequently used substances were marijuana (M = 41.6%, SD = 32.3) and alcohol (M = 7.6%, SD = 10.1). With respect to other problem behaviors, 62.7% of the sample scored at or above the clinical threshold for delinquent behavior problems on the Achenbach Child Behavior Checklist (CBCL) [57], and 39.6% scored at or above the threshold for mild-to-moderate clinical depression on the Beck Depression Inventory (BDI) [58]. In terms of sexual behavior, 69.3% of the adolescents reported at least one lifetime incident of sexual intercourse. The mean age of first sexual intercourse was 14.1 years (SD = 1.7), and the number of lifetime sexual partners ranged from 1 to 40 (M = 5.0, SD = 5.9, median = 3, mode = 1). In the 90-day period prior to entry into the study, 48.0% of the adolescents reported having had sexual intercourse at least once with the number of partners ranging from 1 to 15 (M = 1.8, SD = 1.9, median = 1, mode = 1).
Treatment Conditions
Participants were randomly assigned to either CBT or IBFT. Given the range of risky sexual behaviors commonly reported among drug abusing adolescents, the CBT and IBFT drug interventions were augmented with a brief 1-session HIV-risk education and behavioral skills training intervention. Each treatment consisted of approximately 14 weekly sessions averaging 60 min in length. All therapy sessions were video recorded for purposes of clinical supervision and therapist adherence monitoring.
The CBT intervention utilized in the study was a cognitive-behavioral skills training program designed to teach individual adolescents psychosocial and behavioral self-management and coping skills for reducing drug use [59, 60]. CBT consisted of three distinct clinical phases: motivational enhancement, skills training, and relapse prevention. The supplemental HIV module was embedded within the skill-building phase of treatment. Specific objectives and tasks during CBT included: (a) identifying and recognizing high-risk behaviors and situations, (b) coping with urges and cravings, (c) learning effective communication and problem-solving skills, (d) managing anger and depression, (e) acquiring and practicing drug refusal skills, and (f) setting goals for educational and vocational achievement. During the relapse prevention phase of CBT [41], the focus was on consolidating newly acquired skills, practicing alternatives to substance use, and strengthening attachments with non-substance using peers.
The IBFT treatment integrated components from individual CBT and family-based models within a unitary intervention. The family-focused sessions in IBFT were adapted from the FFT model, a behaviorally oriented approach developed for high-risk youth and their families [39, 61]. The IBFT condition included a mix of individual and family therapy sessions. The first four were family therapy sessions designed to engage and motivate all family members to participate in treatment. The following 10 sessions were behavioral skill-building sessions that were conducted with the adolescent alone or with the family. Family skill building sessions focused on communication and relationship quality between family members, problem solving, and affect regulation. The individual CBT sessions included a functional analysis of drug use behavior and an individually selected set of core CBT skills such as coping with urges and cravings and relapse prevention. As with CBT, the supplemental HIV module was embedded within the skill-building phase of treatment.
The HIV module focused on providing knowledge and skills for identifying and avoiding high-risk sexual behaviors and activities [62]. Although sexual abstinence is the most obvious method of preventing sexual transmission of HIV, a substantial proportion of adults and adolescents fail to adopt this strategy [63–65]. Thus, for most people who are not celibate, appropriate and consistent use of condoms represents the most effective strategy to reduce risk of exposure to HIV [66, 67]. Risk was conceptualized along a continuum from activities very high in risk (unprotected intercourse) to those that pose lesser risk (condom-protected intercourse) to those in which neither partner is at risk (hugging, massage).
The HIV education plus skills training module was adapted from the program used by Kamb et al. [68] for Project RESPECT, a RCT for risk reduction of HIV and other STDs. As part of the HIV education session, the therapist conducts a risk assessment individually tailored to the clients’ HRSB, similar to a functional analysis of high-risk drug behaviors. By combining the risk assessment with information about HIV-risk and adolescents’ beliefs about reducing risk, the therapist is able to identify cues that increase risk for HIV and target the positive and negative consequences of risky behavior. The therapist also identifies HIV preventive behaviors and explores strategies for adoption. Once the situations and problems associated with risky behaviors are identified, whether substance use or HIV, coping strategies and other skills needed to manage high risk situations or promote healthier choices can be targeted for skill training and performance in each of the individual skill training modules of the two interventions wherever appropriate.
Therapist Characteristics
Therapists consisted of six women and two men, two of whom were Hispanic. All were fluent in English and four also fluent in Spanish. Therapists either had a masters or PhD degree in clinical or counseling psychology and all received cultural sensitivity training to work with families from Hispanic and Anglo cultures.
Research Procedures
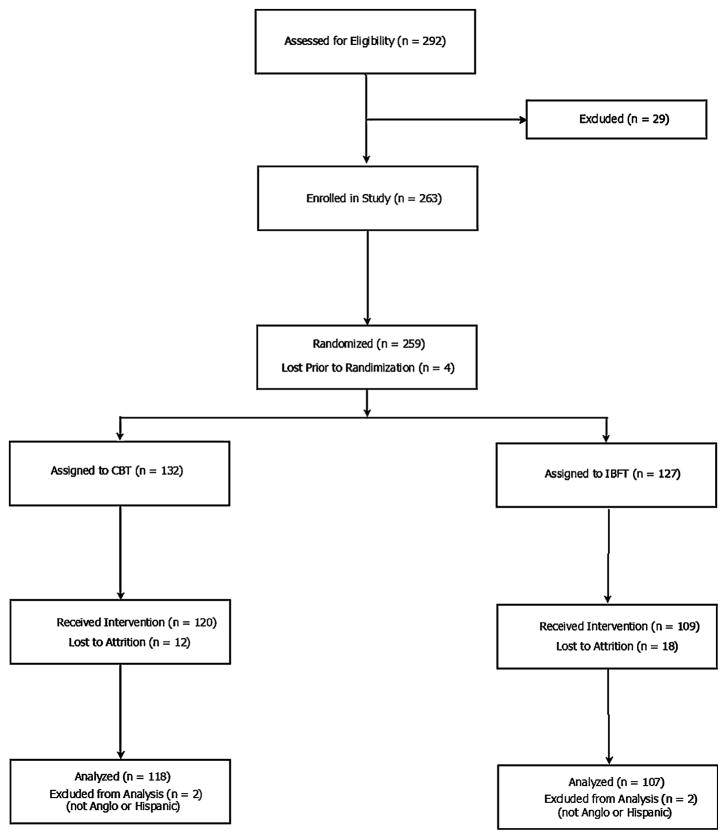
Upon receiving informed consent/assent from each parent/adolescent pairing, adolescents were randomly assigned to the CBT or IBFT condition. Assessments were conducted at intake and at 5, 8, and 18 months after treatment initiation. Assessments included the adolescent, both parents and one sibling over the age of 13, when available. All clinical and research procedures were approved by the Oregon Research Institute’s institutional review board. Figure 1 illustrates the study design and flow of participants through the study.
Fig. 1.
Flow chart of participants through phases of randomized clinical trial
Measure of HIV-Risk Behavior
Involvement in HIV-risk behavior was assessed using a modified version of a screening instrument developed by a National Institute on Drug Abuse (NIDA) workgroup [69] as a supplement to the Problem-Oriented Screening Instrument for Teenagers (POSIT) [70–72]. We obtained a 27-item version of the POSIT HIV scale from the instrument’s developer (E. Rahdert, written communication, June 28, 2000). From this version, we trimmed five items assessing risk factors not directly pertaining to sexual behavior or drug use by needle injection including alcohol use, emotional problems, and family support. The version of the POSIT HIV-risk scale administered to participants contained 22 items assessing whether and in some cases the extent to which adolescents engaged in an array of behaviors elevating one’s risk of exposure to HIV and other STDs over one’s lifetime and/or over the past 90 days. However, only items that could assess change over time (i.e., could occur in the past 90 days) were used in the analysis, resulting in a final set of 17 items. At pretreatment, the scale’s Cronbach’s alpha coefficient was 0.81.
The POSIT HIV-risk scale has been used primarily in studies relating adolescent drug use or abuse to HIV-risk behaviors. Singer et al. [73] found that adolescents currently using MDMA (ecstasy) were significantly more likely to engage in a variety of POSIT HIV-risk behaviors compared to non-MDMA users. Similarly, adolescents in juvenile detention, at high risk for HIV reported significantly higher levels of delinquent behavior and substance use compared to adolescents classified at low risk [74]. Finally, an unpublished 11-item version of the scale was tested on a multi-site sample of 1,418 adolescents from community and clinical settings [75]. The reduced version was found to correlate significantly with measures of substance use and impulsivity among a sample of older adolescents with histories of early behavioral problems.
Analysis Plan
We examined change in the probability of engaging in each HIV-risk behavior using piecewise logistic growth curve (PLGC) models (see Supplementary materials for complete description of the PLGC modeling procedure). In the PLGC analysis, we tested differences in the mean change of the probability of each HIV-risk behavior during and after treatment between each of the following groups, separately, (a) adolescents who did and did not receive the HIV-risk module, (b) the IBFT and the CBT treatment conditions, and (c) Anglo and Hispanic adolescents. Differences between groups were modeled by adding indicator variables for group membership as independent predictors within the PLGC model.
Prior to conducting the PLGC analysis, we partitioned the sample into two subgroups representing distinct levels of risk for HIV at treatment entry [74]. This subgroup classification was performed by means of a latent class analysis (LCA) of the POSIT HIV-risk indicators at the pre-treatment assessment. Briefly, LCA is a semi-parametric statistical procedure for modeling unobserved or latent class membership based on a set of observed variables [76–78]. Upon completing the LCA, the PLGC modeling portion of the analysis was executed separately within each HIV-risk latent class.
Results
Pretreatment HIV-Risk Behavior
\We examined the percentage of the sample that provided a “yes” response at pre-treatment to the 17 items from the POSIT HIV-risk scale assessing the occurrence of high-risk behavior over the past 90 days. Response rates for 11 of the 17 items were less than 10%. We regarded the six highly endorsed items, (a) vaginal sex, 48.0%, (b) oral sex, 40.0%, (c) close friends have sex, 46.2%, (d) sex without a condom, 32.1%, (e) sex while high on drugs or alcohol, 26.3%, and (f) multiple sex partners, 19.7%, as representing the primary profile or repertoire of HIV-risk behaviors characterizing the substance-abusing adolescents in the sample. (Response rates for all 17 items are displayed in Supplement Table S1). Accordingly, with one exception (see “Latent class analysis” below), statistical analyses focused on this primary subset of six items.
Missing Data
Among the 225 adolescent participants in the study, 52.4% had complete data across all four assessments whereas 47.6% had missing data on at least one assessment. Overall, the percentage of cases with completely missing data at the intake, 5-, 8-, and 18-month assessments were 1.3, 19.1, 20.9, and 25.4%, respectively. We addressed missing data using multiple imputation (MI; see Supplementary materials for MI procedure and results).
Latent Class Analysis
Inspection of the response patterns across the six primary POSIT HIV-risk items revealed that 61 of the 225 adolescents (27.1%) did not endorse any items at treatment entry whereas the remaining 164 adolescents (72.9%) endorsed at least one. We hypothesized that (a) the 61 adolescents in the former group represented a distinct subgroup exhibiting inordinately low levels of risk for HIV relative to those endorsing at least one of the six HIV-risk indicators, and (b) adolescents entering treatment at exceptionally low levels of risk for HIV might exhibit qualitatively different responses to treatment than those entering treatment at higher levels of risk. This hypothesis is consistent with numerous clinical studies of adolescent problem behavior in which different patterns and levels of response to treatment have been observed between subgroups entering treatment at distinct levels of risk or problem severity [79, 80].
To investigate the possibility of subgroups exhibiting distinct levels of HIV-risk at treatment entry, we fit a series of LCA models to selected POSIT HIV-risk items at the pre-treatment assessment (see Supplementary materials for full description of the LCA procedure and results). Results indicated that a 2-class LCA model provided the best fit to the data, with the majority of adolescents being classified as low-risk for HIV (n = 153) and a smaller subgroup being classified as high-risk (n = 72).
Modeling Trajectories of Change in Sexual Behavior
The next phase of the analysis was to estimate trajectories of change for the six highly endorsed POSIT items among adolescents in the high- and low-risk latent classes, independently. As noted previously, change in HRSB was analyzed using a PLGC modeling strategy.
High-Risk Latent Class Analysis
Perhaps the most striking pattern of findings is that the probability of engaging in three of the six risky behaviors decreased between the pretreatment and 5-month assessments. Specifically, significant decreases during treatment were evident in the unconditional models for close friends have sex (γ10 = −1.81, SE = 0.53, P < 0.01), multiple sex partners (γ10 = −0.95, SE = 0.40, P < 0.05), and sex without a condom (γ10 = −0.60, SE = 0.30, P < 0.05). These mean decreases were evident across all adolescents regardless of whether the HIV intervention was received, treatment condition, or ethnicity. No other conditional or unconditional effects were evident during treatment on any POSIT HIV-risk dependent variable.
In contrast to the absence of group-specific effects during treatment, differences between groups were more evident during the post-treatment period. In particular, the probability of engaging in sex while high decreased significantly in the CBT condition (γ21 = −1.84, SE = 0.75, P < 0.05) compared to the IBFT condition in which the corresponding trajectory was relatively flat (γ20 = 0.58, SE = 0.40). Additionally, significant differences between ethnic groups were evident during the post-treatment period for the probability of engaging in oral sex (γ21 = 1.32, SE = 0.62, P < 0.05) and close friends have sex (γ21 = 0.78, SE = 0.37, P < 0.05). Both of these findings indicate a significant increase among Hispanic compared to Anglo adolescents, for whom the probability of engaging in each behavior remained relatively stable (γ20 = −0.78, SE = 0.49, and γ20 = −0.22, SE = 0.27, respectively). No other conditional or unconditional effects were evident during the post-treatment period on any POSIT HIV-risk dependent variable. Table 1 presents the predicted mean trajectories of change in the probability of engaging in each of the HIV-risk behaviors for which significant results were obtained in the PLGM. The mean probabilities, expressed on a log-odds scale, were computed by exponentiating the PLGM estimates.
Table 1.
Mean predicted probabilities of engaging in HIV-risk behaviors at each assessment based on the results of the PLGCMs among adolescents at high risk for HIV
| HIV risk behavior | Group | Predicted mean probabilities
|
|||
|---|---|---|---|---|---|
| Pre-treatment | 5 months | 8 months | 18 months | ||
| Vaginal sex | All youth | 0.91 | 0.95 | 0.94 | 0.94 |
| Oral sex | Anglo | 0.89 | 0.96 | 0.91 | 0.83 |
| Hispanic | 0.84 | 0.88 | 0.93 | 0.96 | |
| Sex while high | CBT | 0.85 | 0.95 | 0.62 | 0.13 |
| IBFT | 0.72 | 0.77 | 0.65 | 0.52 | |
| Close friends have sex | Anglo | 0.94 | 0.81 | 0.78 | 0.74 |
| Hispanic | 0.85 | 0.58 | 0.70 | 0.81 | |
| Multiple sex partners | All youth | 0.58 | 0.35 | 0.28 | 0.23 |
| Sex without a condom | All youth | 0.58 | 0.44 | 0.48 | 0.52 |
Low-Risk Latent Class Analysis
The most noteworthy pattern of findings for the low-risk group is the beneficial effect of CBT compared to IBFT in delaying or preventing increases in several risky behaviors. Specifically, significant increases were observed during treatment for IBFT in the probability of vaginal sex (γ10 = 2.20, SE = 0.49, P < 0.001) and multiple sex partners (γ10 = 3.76, SE = 0.96, P < 0.001). In contrast, in CBT these mean increases were largely negated (γ11 = −1.58, SE = 0.64, P < 0.05 for vaginal sex, and γ11 = −2.45, SE = 1.16, P < 0.05 for multiple sex partners).
In addition to these treatment condition effects, significant overall increases in the probability of engaging in oral sex (γ10 = 1.31, SE = 0.33, P < 0.001) and sex while high (γ10 = 2.31, SE = 0.76, P < 0.01) were found between the pretreatment and 5-month assessments. These increases were unrelated to whether or not the HIV intervention was received, treatment condition, or adolescent ethnicity. No other conditional or unconditional effects were evident during treatment on any POSIT HIV-risk dependent variable.
Similar to the during-treatment results, a preventative effect of CBT was evident during the post-treatment period. Specifically, the probability of engaging in sex without a condom decreased significantly in CBT (γ11 = −0.86, SE = 0.41, P < 0.05) relative to IBFT in which the probability remained relatively stable (γ10 = 0.48, SE = 0.28). Contrary to this result, however, the preventative effect of CBT on change in the probability of vaginal sex, evident during treatment, appeared to erode during the post-treatment period (γ11 = 0.82, SE = 0.32, P < 0.05) relative to IBFT in which the probability remained flat (γ10 = −0.06, SE = 0.24).
In addition to these treatment condition effects, a significant difference between ethnic groups was evident during the post-treatment period for the probability of engaging in sex without a condom which showed a significant increase among Hispanics (γ21 = 0.86, SE = 0.41, P < 0.05) relative to Anglos among whom the probability remained relatively stable (γ20 = −0.43, SE = 0.36). In addition, an overall significant increase in the mean probability of close friends have sex was obtained between the pretreatment and 5-month assessments (γ21 = 0.62, SE = 0.23, P < 0.05). No other conditional or unconditional effects were evident during treatment on any POSIT HIV-risk dependent variable. Table 2 presents the predicted mean trajectories of change in the probability of engaging in each of the HIV-risk behaviors for which significant results were obtained in the PLGM among adolescents entering treatment at low risk for HIV.
Table 2.
Mean predicted probabilities of engaging in HIV-risk behaviors at each assessment based on the results of the PLGCMs among adolescents at low risk for HIV
| HIV risk behavior | Group | Predicted mean probabilities
|
|||
|---|---|---|---|---|---|
| Pre-treatment | 5 months | 8 months | 18 months | ||
| Vaginal sex | CBT | 0.05 | 0.40 | 0.59 | 0.75 |
| IBFT | 0.22 | 0.72 | 0.70 | 0.69 | |
| Oral sex | All youth | 0.15 | 0.39 | 0.45 | 0.50 |
| Sex while high | All youth | 0.01 | 0.13 | 0.15 | 0.18 |
| Close friends have sex | All youth | 0.20 | 0.11 | 0.18 | 0.29 |
| Multiple sex partners | CBT | 0.00 | 0.06 | 0.07 | 0.09 |
| IBFT | 0.01 | 0.18 | 0.16 | 0.15 | |
| Sex without a condom | Anglo | 0.11 | 0.15 | 0.11 | 0.08 |
| Hispanic | 0.07 | 0.13 | 0.18 | 0.26 | |
| CBT | 0.15 | 0.15 | 0.11 | 0.08 | |
| IBFT | 0.13 | 0.13 | 0.20 | 0.29 | |
Discussion
The current study compared the effectiveness of two adolescent drug abuse treatments (CBT and IBFT) on HIV-risk behaviors, and in a quasi-experimental design, examined the additional impact of a brief HIV-risk module embedded within each of the primary interventions. Despite the absence of any effect of the HIV-specific intervention module, significant effects were noted for both of the interventions on HIV-risk behavior with effects dependent upon whether participants were (a) in the high versus low-risk groups, or (b) members of the Anglo versus Hispanic ethnic groupings. Specifically, the results indicated that CBT was more efficacious than IBFT in suppressing HIV-risk behaviors among both high- and low-risk participants. Among high-risk youth, however, both interventions were associated with signification reductions in three risk behaviors, sex without a condom, close friends have sex and multiple sex partners from pre to post-treatment with sustained effects up to the 18-month assessment for the first two. CBT also showed superior effects compared to IBFT for having sex while high but only in the post-treatment follow-up period. However, the long-term decrease in sex under the influence of drugs showed a significant decrease for both conditions although a greater reduction was found for CBT.
Among the low-risk participants, in general, increases in four of the six risk behaviors were found consistent with expected developmental patterns. However, despite increases in vaginal sex to about 70%, sex without a condom remained quite low and under 30%. Moreover, CBT appeared to suppress effects of the increases in vaginal sex and multiple sex partners observed in the IBFT condition from pre to post treatment, although these effects appear to be short-lived. CBT also showed post treatment effects for sex without a condom. Overall, despite significant increases in vaginal sex to near 80%, sex without a condom never rose above 30% suggesting the interventions did have some long-term impact on the low-risk adolescents.
The pattern of findings has several important implications for both treatment and prevention activities. For example, an HIV-specific intervention may not be necessary to target specific risky sexual behaviors among high-or low-risk adolescents. Rather, the results suggest that some evidence-based treatments designed to target drug use and associated risk factors more generally may be sufficient to reduce or prevent the expected increase in HRSBs among drug-abusing adolescents. This implication is consistent with the notion that drug abuse and risky sexual behaviors are represented within a constellation of problem behaviors among youth [7]. A number of investigators have suggested that adolescent problems such as drug abuse, HIV-risk behaviors, and other conduct problems may not constitute independent disorders or problems but may represent deviant behaviors that are part of a known developmental trajectory [81]. Many adolescents with these disorders have common behavioral skill deficits, as in poor problem solving, limited coping strategies, low motivation for change or low self-efficacy. The focus on changing these skill deficits, especially via the CBT intervention, may act to reduce related behavioral problems such as those associated with drug abuse and HIV-risk. Consequently, drug abuse treatments with demonstrated efficacy [18] may in fact be affecting a host of risk and protective factors associated with risky behaviors, including those associated with HIV infection and other STDs during a critical developmental period. Moreover, the effects of the interventions appear to be maintained up to 18 months after intake or approximately 1 year after treatment ended. The durability of the changes observed for HIV-risk reductions is similar to the maintenance of drug use reductions over time [18]. Further, the data show that interventions for drug abuse can have both preventative and intervention effects for adolescents who are less and more sexually active, respectively. Such effects have the potential for informing similar treatment programs for drug-abusing adolescents.
Earlier, we noted that mediators of reductions in HIV-risk behaviors could be improved relationships within the family as a function of family therapeutic approaches or skill building via CBT. Another important mediator of reductions in risky sexual behavior is the use or abuse of drugs. Adolescent and adult studies show that drug use interferes with cognitive processes such as decision-making and increases impulsivity, both of which act to increase the likelihood of high-risk sexual practices. Whether these mediators performed as predicted in the current study will be the focus of future analyses.
The differential effects for low-risk and high-risk adolescents are particularly interesting and are similar to the results of several other studies that have targeted HIV-risk behaviors. Both Kirby et al. [45] and Jemmott et al. [46] found that their interventions had greater effects for more sexually experienced youth. The population of drug-abusing adolescents served here appeared to consist of two distinct populations, those who were more sexually active and also at higher current risk for HIV and other STDs, and those who were less sexually active. For the former, significant decreases in three behaviors, frequently found to be associated with a host of sexually transmitted diseases were found from pre to posttreatment. Further, multiple sex partners continued to decline while sex while high, although not showing an immediate intervention effect, dropped considerably by the 18-month assessment. These two behaviors showed significant decreases of 35 and 46%, respectively, 18 months after intake. While other programs have demonstrated similar or greater increases [45, 51], neither of these studies examined drug-abusing populations considered at higher risk for HIV or STD infections or had interventions that were directed at related behaviors, not HIV-risk per se.
The effects for the low-risk or less sexually experienced adolescents did not show significant reductions in HRSB, in part due to their lower baseline levels and greater variability. However, despite significant increases in both vaginal and oral sex, we did not see similar increases in the other risky behaviors from post-treatment to the 18-month follow-up as might be expected developmentally. For example, despite nearly 70% of the participants reporting vaginal intercourse, less than 30% reported having sex without a condom. Further, differential treatment effects were noted for this group with CBT showing more suppressive effects compared to IBFT for multiple partners and sex without a condom. Perhaps, the different social contexts of the treatments accounted, in part, for the stronger CBT effects. For example, although the HIV-risk module was an individual session in both CBT and IBFT, IBFT involved relatively few individual sessions, with the majority of sessions held conjointly with the family. The exclusive individual focus of CBT and the greater number of individual sessions may have led adolescents in CBT to develop a stronger therapeutic bond that made discussing sexually related behaviors or other concerns more comfortable. Alternatively, the greater focus on skill building in the CBT sessions may have led to increased coping skills in adolescents compared to youth in IBFT, and the increased skills provided a foundation for change in a variety of HSRBs. Possibly, the strengths of the therapeutic relationship and skill acquisition are particularly important for low-risk youth and may have accounted for the suppression of HIV-risk behaviors in this group.
The single behavior that showed differential results for the low-risk group in favor of Anglos was somewhat surprising. Guzman et al. [82] noted that discussions of sexual behavior in Hispanic families may be more difficult given different cultural norms. However, no family discussions of sexual behavior were planned and other studies of family involvement in HIV-risk prevention have occurred with positive results [33]. Further, condom use among Hispanics is generally higher than among whites [83]. Interventions may have to focus on different negotiation strategies for Latinos compared to non-Hispanic whites [84]. Thus, explanation of the results here will require further exploration.
The similarity of HIV-risk outcomes for both Hispanic and Anglo adolescents among the high-risk youth is noteworthy. Although there were differences between Hispanic and Anglos in oral sex, both were quite high even after intervention. Similarly, Anglos responded more positively to the intervention in terms of having sexually involved friends but this too dissipated by the 18-month assessment. Cultural differences did not appear to play a role in treatment responding. These data are similar to the results of other studies that compared the effects of an intervention on different cultural/ethnic/racial groupings. For example, Kirby et al. [45] showed that although Hispanics improved more than nonHispanic Whites with respect to delaying initiation into sex, both Hispanics and White students showed significantly greater increases in their condom use at last sex compared to Blacks. The power of interventions to effect change across cultural/ethnic groupings may be due to their focus on common cross-ethnicity variables. Further research will be necessary to demonstrate whether this is so. Clearly, the development of prevention programs and treatments that are efficacious across ethnic cultural groupings is more efficient than the development of a wide array of culturally specific interventions [51]. Each new culturally specific treatment requires independent evaluations to establish an empirical foundation, whereas existing evidence-based practices can be tailored or implemented in a culturally sensitive manner without sacrificing treatment fidelity [85, 86]. Lending support to this idea, sessions in the current study were conducted in Spanish for all youth and families who preferred therapy to be conducted in their native language by therapists who had received cultural sensitivity training as part of the clinical trial protocol. Thus, both evidence-based practices were tailored to participants’ ethnic culture without modifying the elements of the treatment models themselves. Because so few studies have been conducted examining treatment outcomes across racial/ethnic groups the question of culturally specific versus culturally sensitive interventions has not been resolved. The current findings are promising, however, suggesting that some interventions for HSRBs may be efficacious across ethnic groups.
Limitations
Adolescents were randomly assigned to CBT or IBFT but not to different HIV-risk reduction interventions. Thus, we recognize that we cannot directly attribute changes to the clinical treatments since some non-experimental factor may have produced changes in both conditions. However, our analyses by level of risk were similar to those contained in other studies with similar outcomes. We also used a brief HIV-intervention that was coordinated with the drug abuse treatments. A more comprehensive HIV-risk component might have produced stronger effects than those reported here. In addition, we found only one significant predictor of receiving the HIV-risk module in each risk group, which did not appear to account for possible differences in outcome. Further research will be required that randomly assign participants on the basis of HIV-risk behaviors to specific treatments.
It is also possible that substantial decreases among the high-risk group and similar increases among the low-risk group are simply regression to the mean effects. However, the changes noted in the current study were not all in the direction that would be predicted by regression effects. Some differences were noted as a function of the type of intervention with CBT showing greater suppression effects than IBFT. Further, not all variables showed dramatic increases among the low-risk group. As noted above, although oral and vaginal sex showed increases that were 2–3 times that of pretreatment, the other variables remained relatively low and differential treatment effects noted there as well.
Finally, the current analysis examined change in six HIV-risk items separately within two latent classes of adolescents. Consequently, a large number of statistical tests were performed which elevates the risk of Type-I error (i.e., obtaining significant findings by chance). For this reason, the findings reported here should be interpreted cautiously, especially those at the P < 0.05 level of significance. Specific results that appear to form a pattern across items, however, are substantially less likely to be due to random chance. As discussed previously, in the current analysis several relatively stable patterns of findings emerged including the overall reduction in the probability of engaging in HIV-risk behaviors over time among adolescents in the high-risk latent class, as well as the general superiority of CBT over IBFT in reducing the probability of HIV-risk behavior over time among adolescents in the low-risk latent class.
Despite these limitations, this was the first study conducted in outpatient treatment for drug abusing adolescents with a focus on HIV-risk behaviors. Even though the specific treatment directed at risky sexual behaviors did not prove to be efficacious, this does not detract sufficiently from the general outcome showing that drug abuse treatment itself can be effective for reducing or preventing HIV-risk behaviors in drug-abusing adolescents.
Supplementary Material
Acknowledgments
We gratefully acknowledge the contributions of Gael Johnson in the preparation of this article, the many families that participated in this research, and the therapists and research assistants who made this work possible. This manuscript was supported by National Institute on Drug Research Grants R01DA13350, R01DA13354.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s10461-011-0019-7) contains supplementary material, which is available to authorized users.
Contributor Information
Hyman Hops, Email: hy@ori.org, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403-1983, USA.
Timothy J. Ozechowski, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403-1983, USA
Holly B. Waldron, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403-1983, USA
Betsy Davis, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403-1983, USA.
Charles W. Turner, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403-1983, USA
Janet L. Brody, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403-1983, USA
Manuel Barrera, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403-1983, USA. Psychology Department, Arizona State University, Box 871104, Tempe, AZ 85287-1104, USA.
References
- 1.Institute of Medicine, Committee on Prevention and Control of Sexually Transmitted Diseases. The hidden epidemic: confronting sexually transmitted diseases. Washington DC: National Academy Press; 1997. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Morbidity and Mortality weekly report 53. SS-2. 2004. Surveillance summaries. [Google Scholar]
- 3.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: incidence and prevalence estimates. Perspect Sex Reprod Health. 2004;36(1):6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 4.Sayegh MA, Fortenberry JD, Anderson J, Orr DP. Relationship quality, coital frequency, and condom use as predictors of incident genital Chlamydia trachomatis infection among adolescent women. J Adolesc Health. 2005;37:163. doi: 10.1016/j.jadohealth.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 5.Metzger DS, Woody GE, O’Brien CP. Drug treatment as HIV Prevention: a research update. J Acquir Immune Defic Syndr. 2010;55(Supp1):S32–6. doi: 10.1097/QAI.0b013e3181f9c10b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woody GE, VanEtten-Lee ML, McKirnan D, et al. Substance use among men who have sex with men: comparison with a national household survey. J Acquir Immune Defic Syndr. 2001;27:86–90. doi: 10.1097/00126334-200105010-00015. [DOI] [PubMed] [Google Scholar]
- 7.Ary DV, Duncan TE, Duncan SC, Hops H. Adolescent problem behavior: the influence of parents and peers. Behav Res Ther. 1999;37:217–30. doi: 10.1016/s0005-7967(98)00133-8. [DOI] [PubMed] [Google Scholar]
- 8.Kirby D. Antecedents of adolescent initiation of sex, contraceptive use and pregnancy. Am J Health Behav. 2002;26:473–85. doi: 10.5993/ajhb.26.6.8. [DOI] [PubMed] [Google Scholar]
- 9.St Lawrence JS, Crosby RA, Brasfield TL, O’Bannon RE., III Reducing STD and HIV risk behavior of substance-dependent adolescents: a randomized controlled trial. J Consult Clin Psychol. 2002;70:1010–21. [PubMed] [Google Scholar]
- 10.Tildesley EA, Hops H, Ary D, Andrews JA. Multitrait-multi-method model of adolescent deviance, drug use, academic, and sexual behaviors. J Psychopathol Behav Assess. 1995;17:185–215. [Google Scholar]
- 11.Capaldi DM, Stoolmiller M, Clark S, Owen LD. Heterosexual risk behaviors in at-risk young men from early adolescence to young adulthood: prevalence, prediction, and STD contraction. Dev Psychol. 2002;38:394–406. doi: 10.1037//0012-1649.38.3.394. [DOI] [PubMed] [Google Scholar]
- 12.Walkup J, Blank MB, Gonzalez JS, et al. The impact of mental health and substance abuse factors on HIV prevention and treatment. J Acquir Immune Defic Syndr. 2008;47(Supp1):S15–9. doi: 10.1097/QAI.0b013e3181605b26. [DOI] [PubMed] [Google Scholar]
- 13.Brown LS, Jr, Kritz S, Muhammad A, et al. Disparities in health services for HIV/AIDS, Hepatitus C virus, and sexually transmitted infections: role of substance abuse treatment programs. J Addict Med. 2009;3(2):95–102. doi: 10.1097/ADM.0b013e318190f0e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ozechowski TJ, Waldron HB. Assertive outreach strategies for narrowing the adolescent substance abuse treatment gap: implications for research, practice, and policy. J Behav Health Serv Res. 2010;37(1):40–63. doi: 10.1007/s11414-008-9136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peterson JL, Marin G. Issues in the prevention of AIDS among Black and Hispanic men. Am Psychol. 1988;43:871–7. doi: 10.1037//0003-066x.43.11.871. [DOI] [PubMed] [Google Scholar]
- 16.Rounds-Bryant JL, Staab J. Patient characteristics and treatment outcomes for African American, Hispanic, and White adolescents in DATOS-A. J Adolesc Res. 2001;16(6):624–41. [Google Scholar]
- 17.Marvel F, Rowe CL, Colon-Perez L, DiClemente RJ, Liddle HA. Multidimensional family therapy HIV/STD risk-reduction intervention: an integrative family-based model for drug-involved juvenile offenders. Fam Process. 2009;48(1):69–84. doi: 10.1111/j.1545-5300.2009.01268.x. [DOI] [PubMed] [Google Scholar]
- 18.Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. J Clin Child Adolesc Psychol. 2008;37(1):238–61. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- 19.Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27(3):197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. J Consult Clin Psychol. 2001;69:802–13. [PubMed] [Google Scholar]
- 21.DiClemente RJ, Wingood GM, Harrington KF, et al. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. J Am Med Assoc. 2004;292:171–9. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- 22.Jemmott JB, Jemmott LS, Fong GT, McCaffree K. Reducing HIV risk-associated sexual behavior among African American adolescents: testing the generality of intervention effects. Am J Community Psychol. 1999;7:161–87. doi: 10.1007/BF02503158. [DOI] [PubMed] [Google Scholar]
- 23.Slonim-Nevo V. The effect of HIV/AIDS prevention intervention for Israeli adolescents in residential centers: results at 12-month follow-up. Soc Work Res. 2001;25(2):71–88. [Google Scholar]
- 24.Villarruel AM, Jemmott JB, Jemmott LS, Ronis DL. Predictors of sexual intercourse and condom use intentions among Spanish-dominant Latino youth. Nurs Res. 2004;53(3):172–81. doi: 10.1097/00006199-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Jemmott JB, Jemmott LS, Fong GT. Reductions in HIV risk-associated sexual behaviors among Black male adolescents: effects of an AIDS prevention intervention. Am J Public Health. 1992;82(3):372–7. doi: 10.2105/ajph.82.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Main DS, Iverson DC, McGloin J, Banspach SW. Preventing HIV infection among adolescents: evaluation of a school-based education program. Prev Med. 1994;23(4):409–17. doi: 10.1006/pmed.1994.1056. [DOI] [PubMed] [Google Scholar]
- 27.Kirby D, Barth RP, Leland N, Fetro JV. Reducing the risk: impact of a new curriculum on sexual risk-taking. Fam Plann Perspect. 1991;23(6):253–63. [PubMed] [Google Scholar]
- 28.St Lawrence JS, Brasfield TL, Jefferson KW, Alleyne E, O’Bannon RE, Shirley A. Cognitive-behavioral intervention to reduce African-American adolescents’ risk for HIV infection. J Consult Clin Psychol. 1995;63(2):221–37. doi: 10.1037//0022-006x.63.2.221. [DOI] [PubMed] [Google Scholar]
- 29.Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: their impact on sexual behaviors of young people throughout the world. J Adolesc Health. 2007;40:206–17. doi: 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- 30.Coyle KK, Kirby DB, Robin LE, Banspach SW, Baumler E, Glassman JR., Jr ALL4YOU! A randomized trial of an HIV, other STDs, and pregnancy prevention intervention for alternative school students. AIDS Educ Prev. 2006;18:187–203. doi: 10.1521/aeap.2006.18.3.187. [DOI] [PubMed] [Google Scholar]
- 31.DiClemente RJ, Salazar LF, Crosby RA. A review of STD/HIV preventive interventions for adolescents: sustaining effects using an ecological approach. J Pediatr Psychol. 2007;2(8):888–906. doi: 10.1093/jpepsy/jsm056. [DOI] [PubMed] [Google Scholar]
- 32.Donenberg GR, Paikoff R, Pequegnat W. Introduction to the special section on families, youth and HIV: family-based interventional studies. J Pediatr Psychol. 2006;31(9):869–73. doi: 10.1093/jpepsy/jsj102. [DOI] [PubMed] [Google Scholar]
- 33.Prado G, Pantin H, Briones E, et al. A randomized controlled trial of a parent-centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. J Consult Clin Psychol. 2007;75(6):914–26. doi: 10.1037/0022-006X.75.6.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lederman RP, Mian TS. The parent-adolescent relationship education (PARE) program: a curriculum for prevention of STDs and pregnancy in middle school youth. Behav Med. 2003;29(1):33–41. doi: 10.1080/08964280309596173. [DOI] [PubMed] [Google Scholar]
- 35.Sperber E, McKay MM, Bell CC, Petersen I, Bhana A, Paikoff R. Adapting and disseminating a community-collaborative evidence-based HIV/AIDS prevention programme: lessons from the history of CHAMP. Vulnerable Child Youth Stud. 2008;3:150–8. doi: 10.1080/17450120701867561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DiIorio C, McCarty F, Resnicow K, Lehr S, Denzmore S. REAL Men: a group-randomized trial of an HIV prevention intervention for adolescent boys. Res Pract. 2007;97(6):1084–9. doi: 10.2105/AJPH.2005.073411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tapia MI, Schwartz SJ, Prado G, Lopez B, Pantin H. Parent-Centered Intervention: a practical approach for preventing drug abuse in Hispanic adolescents. Res Soc Work Pract. 2006;16(2):146–65. [Google Scholar]
- 38.Murry VM, Berkel C, Brody GH, Gibbons M, Gibbons FX. The strong African American families program: longitudinal pathways to sexual risk reduction. J Adolesc Health. 2007;41:333–42. doi: 10.1016/j.jadohealth.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 39.Alexander JF, Parsons BV. Functional family therapy: principles and procedures. Carmel: Brooks/Cole; 1982. [Google Scholar]
- 40.Liddle HA, Rowe CL, Dakof GA, Ungaro RA, Henderson CE. Early intervention for adolescent substance abuse: pretreatment to posttreatment outcomes of a randomized clinical trial comparing multidimensional family therapy and peer group treatment. J Psychoact Drugs. 2004;36:49–63. doi: 10.1080/02791072.2004.10399723. [DOI] [PubMed] [Google Scholar]
- 41.Marlatt BA, Gordon JR. Relapse prevention. New York: Guilford Press; 1985. [Google Scholar]
- 42.Monti PM, Rohsenow DJ, Rubonis AV, et al. Cue exposure with coping skills treatment for Male alcoholics: a preliminary investigation. J Consult Clin Psychol. 1993;61:1011–9. doi: 10.1037//0022-006x.61.6.1011. [DOI] [PubMed] [Google Scholar]
- 43.Rotheram-Borus MJ. Testimony at hearing; The risky business of adolescence: how to help teens stay safe. Washington, DC: Select Committee on Children, Youth and Families. U. S. House of Representatives; 1991. [Google Scholar]
- 44.Woody GE. Research findings on psychotherapy of addictive disorders. Am J Addict. 2003;12:S19–26. [PubMed] [Google Scholar]
- 45.Kirby DB, Baumler E, Coyle KK, et al. The “Safer Choices” intervention: its impact on the sexual behaviors of different subgroups of high school students. J Adolesc Health. 2004;35:442–52. doi: 10.1016/j.jadohealth.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 46.Jemmott JB, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: a randomized controlled trial. J Am Med Assoc. 1998;279:1529–36. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- 47.Walter HJ, Vaughan RD, Ragin DF, Cohall AT, Kasen S, Fuli-love RE. Prevalence and correlates of AIDS-risk behaviors among urban minority high school students. Prev Med. 1993;22:813–24. doi: 10.1006/pmed.1993.1074. [DOI] [PubMed] [Google Scholar]
- 48.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Overview of key findings 2008. Bethesda: National Institute on Drug Abuse; 2009. Monitoring the future: national results on adolescent drug use. [Google Scholar]
- 49.Substance Abuse and Mental Health Services Administration (SAHMSA) NSDUH Series H-32, DHHS Publication No. SMA 07–4293. Rockville: Office of Applied Studies; 2007. Results from the 2006 national survey on drug use and health: national findings. [Google Scholar]
- 50.Grunbaum JA, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2003 (Abridged) J Sch Health. 2004;74:307–24. doi: 10.1111/j.1746-1561.2004.tb06620.x. [DOI] [PubMed] [Google Scholar]
- 51.Villarruel AM, Jemmott JB, III, Jemmott LS. A randomized controlled trial testing an HIV prevention intervention for Latino youth. Arch Pediatr Adolesc Med. 2006;160:772–7. doi: 10.1001/archpedi.160.8.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liddle HA, Dakof GA, Henderson C, Rowe C. Implementation outcomes of Multidimensional Family Therapy-Detention to community. Int J Offender Ther Comp Criminol. doi: 10.1177/0306624X10366960. [DOI] [PubMed] [Google Scholar]
- 53.Waldron HB, Brody JL, Slesnick N. Integrative behavioral and family therapy for adolescent substance abuse. In: Monti PM, Colby SM, O’Leary TA, editors. Adolescents, alcohol, and substance abuse: reaching teens through brief interventions. New York: Guilford Press; 2001. pp. 216–43. [Google Scholar]
- 54.Alexander JF, Parsons BV, Pugh C. Blueprints for violence prevention. Colorado: Venture; 1998. [Google Scholar]
- 55.Azrin NH, Donohue B, Besalel VA, Kogan ES, Acierno R. Youth drug abuse treatment: a controlled study. J Child Adolesc Subst Abuse. 1994;3:1–16. [Google Scholar]
- 56.Brown SA, Meyers MG, Mott MA, Vik PW. Correlates of success following treatment for adolescent substance abuse. Appl Prev Psychol. 1994;3:61–73. [Google Scholar]
- 57.Achenbach TM. Manual for the child behavior checklist and the 1991 profile. Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 58.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 59.Monti PM, Abrams DB, Kadden RM, Cooney NL. Treating alcohol dependence. London: Gilford Press; 1989. [Google Scholar]
- 60.Kadden RM, Cooney NL, Getter H, Litt MD. Matching alcoholics to coping skills or interactional therapies: posttreatment results. J Consult Clin Psychol. 1989;57(6):698–704. doi: 10.1037//0022-006x.57.6.698. [DOI] [PubMed] [Google Scholar]
- 61.Barton C, Alexander JF. Functional family therapy. In: Gurman AS, Kniskern DP, editors. Handbook of family therapy. New York: Brunner/Mazel; 1981. pp. 403–43. [Google Scholar]
- 62.DiClemente RJ, Peterson JL, editors. Preventing AIDS: theories and methods of behavioral interventions. New York: Plenum Press; 1994. [Google Scholar]
- 63.Anderson JE, Kann L, Holtzman D, Arday S, Truman B, Kolbe L. HIV/AIDS knowledge and sexual behavior among high school students. Fam Plann Perspect. 1990;22:252–5. [PubMed] [Google Scholar]
- 64.Catania JA, Coates TJ, Stall R, et al. Prevalence of AIDS-related risk factors and condom use in the United States. Science. 1992;258:1101–6. doi: 10.1126/science.1439818. [DOI] [PubMed] [Google Scholar]
- 65.DiClemente RJ. Adolescents and AIDS: current research, prevention strategies, and policy implications. In: Temoshok L, Baum A, editors. Psychosocial perspectives on AIDS: etiology, prevention, and treatment. Hillsdale: Lawrence Erlbaum Associates, Inc; 1990. [Google Scholar]
- 66.Cates W, Jr, Stone KM. Family planning, sexually transmitted diseases and contraceptive choice: a literature update—Part I. Fam Plann Perspect. 1992;24:75–84. [PubMed] [Google Scholar]
- 67.Van de Perre P, Jacobs D, Sprecher-Goldberger S. The latex condom, an efficient barrier against sexual transmission of AIDS-related viruses. AIDS. 1987;1:49–52. [PubMed] [Google Scholar]
- 68.Kamb ML, Fishbein M, Douglas JM, et al. Efficacy of risk-reduction counseling to prevent Human Immunodeficiency Virus and sexually transmitted diseases. J Am Med Assoc. 1998;280(13):1161–7. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- 69.Rahdert E. DHHS Publication ADM-91-1735. Rockville: National Institute on Drug Abuse; 1991. The adolescent assessment and referral manual. [Google Scholar]
- 70.Latimer WW, O’Brien MS, McDouall J, Toussova O, Floyd LJ, Vazquez M. Screening for “substance abuse” among school-based youth in Mexico using the Problem Oriented Screening Instrument for Teenagers (POSIT) Subst Use Misuse. 2004;39:307–29. doi: 10.1081/ja-120028492. [DOI] [PubMed] [Google Scholar]
- 71.Leccese M, Waldron HB. Assessing adolescent substance use: a critique of current measurement instruments. J Subst Abuse Treat. 1994;11:553–63. doi: 10.1016/0740-5472(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 72.Santisteban DA, Tejeda M, Dominicis C, Szapocznik J. An efficient tool for maladaptive family functioning in adolescent drug abusers: the problem oriented screening instrument for teenagers. Am J Drug Alcohol Abuse. 1999;25:197–206. doi: 10.1081/ada-100101855. [DOI] [PubMed] [Google Scholar]
- 73.Singer LT, Linares TJ, Ntiri S, Henry R, Minnes S. Psychosocial profiles of older adolescent MDMA users. Drug Alcohol Depend. 2004;74:245–52. doi: 10.1016/j.drugalcdep.2003.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rowe CL, Wang W, Greenbaum P, Liddle HA. Predicting HIV/STD risk level and substance use disorders among incarcerated adolescents. J Psychoact Drugs. 2008;40:503–12. doi: 10.1080/02791072.2008.10400656. [DOI] [PubMed] [Google Scholar]
- 75.Winters KC, Botzet AM, Fahnhorst T, Baumel L, Lee S. Impulsivity and its relationship to risky sexual behaviors and drug abuse. J Child Adolesc Subst Abuse. 2009;18:43–56. doi: 10.1080/15470650802541095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Clogg CC. Latent class models. In: Arminger G, Clogg CC, Sobell ME, editors. Handbook of statistical modeling for the social and behavioral sciences. New York: Plenum Press; 1995. pp. 311–59. [Google Scholar]
- 77.McLachlan G, Peel D. Finite mixture models. New York: Wiley; 2000. [Google Scholar]
- 78.Skrondal A, Rabe-Hesketh S. Generalized latent variable modeling: multilevel, longitudinal, and structural equation models. New York: Chapman & Hall/CRC; 2004. [Google Scholar]
- 79.Godley SH, Dennis ML, Godley MD, Funk RR. Thirty-month relapse trajectory cluster groups among adolescents discharged from outpatient treatment. Addiction. 2004;99(2):129–39. doi: 10.1111/j.1360-0443.2004.00860.x. [DOI] [PubMed] [Google Scholar]
- 80.Latimer WW, Winters KC, Stinchfield R, Traver RE. Demographic, individual, and interpersonal predictors of adolescent alcohol and marijuana use following treatment. Psychol Addict Behav. 2000;14:162–73. doi: 10.1037//0893-164x.14.2.162. [DOI] [PubMed] [Google Scholar]
- 81.Patterson GR, DeGarmo DS, Knutson N. Hyperactive and antisocial behaviors: comorbid or two points in the same process? Dev Psychopathol. 2000;12:91–106. doi: 10.1017/s0954579400001061. [DOI] [PubMed] [Google Scholar]
- 82.Guzman BL, Schlehofer-Sutton MM, Villanueva CM, Stritto MED, Casad BJ, Feria A. Let’s talk about sex: how comfortable discussions about sex impact teen sexual behavior. J Health Commun. 2003;8(6):583–98. doi: 10.1080/716100416. [DOI] [PubMed] [Google Scholar]
- 83.Eaton DK, Kann L, Kinchen S, et al. Centers for Disease Control, Prevention (CDC) Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ. 2008;57(4):1–131. [PubMed] [Google Scholar]
- 84.Tschann JM, Flores E, de Groat SL, Deardorff J, Wibbelsman CJ. Condom negotiation strategies and actual condom use among Latino youth. J Adolesc Health. 2010;47:254–62. doi: 10.1016/j.jadohealth.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Castro FG, Barrera M, Martinez CR. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci. 2004;5(1):41–5. doi: 10.1023/b:prev.0000013980.12412.cd. [DOI] [PubMed] [Google Scholar]
- 86.Whaley AL, Davis KE. Cultural competence and evidence-based practice in mental health services: a complementary perspective. Am Psychol. 2007;62(6):563–74. doi: 10.1037/0003-066X.62.6.563. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.