Abstract
Low back pain (LBP) is a major health issue with significant socioeconomic implications in most Western countries. Many forms of treatment have been proposed and investigated in the past, with exercise being a commonly prescribed intervention. Within allied health, in particular physiotherapy, there has been a growing movement that recognizes the role of the McKenzie method in treating LBP. Within the McKenzie framework, directional preference (DP) exercises are one such intervention, with preliminary data demonstrating its effectiveness in the management of LBP. In this paper, we aim to integrate the evidence from current research, identified using a systematic review, and utilize a practical real-life case scenario to outline how evidence from the literature can be implemented in clinical practice. The findings from the systematic review indicate that DP exercises may have positive effects in the management of LBP. While the body of evidence to support this is limited (only four studies) and therefore modest at best, it does provide some emerging evidence to support the use of DP exercises in clinical practice. Despite this, gaps also persist in the literature on DP exercises, and this relates to the exercise parameters and the compliance rates. Recognizing this dichotomy (modest evidence in some areas and evidence gaps in other areas), which is likely to confront health practitioners, using a practical approach with a real-life clinical scenario, we outline how the evidence from the systematic review can be implemented in clinical practice. This approach builds on the philosophy of evidence-based practice of integrating research evidence with clinical expertise and patient values.
Keywords: low back pain, McKenzie method, directional preference exercises
Introduction
Low back pain (LBP) is a major health issue with significant socioeconomic implications in many Western countries.1 Prevalence reports vary considerably, but it has been estimated that 60%–80% of people will experience an episode of LBP during their lives.2 With increasing costs, both in terms of health care and loss in productivity, there is a clear need for effective and timely management which will ensure recovery and avoid chronicity.1 Several treatment strategies, for instance, joint mobilization and manipulation, soft tissue massage techniques, electrotherapy, acupuncture, and traction, are currently utilized in clinical practice by a range of practitioners, with varying degrees of effectiveness.3–6 Exercises are commonly prescribed for LBP by physiotherapists, but only seem to be supported as an intervention by evidence for patients with chronic LBP.7,8 While current evidence supports the role of exercise for LBP, clinical application of this intervention is varied, especially in terms of exercise prescription.1,4,8 Core stability exercises are particularly popular in the clinical setting and have been extensively researched.9,10
Historically, classification of LBP, particularly for research purposes, has been determined by the chronicity of the condition, eg, “acute”, “subacute”, and “chronic”.4,11 While this classification takes into account symptom duration, it fails to capture the complexities associated with a patient’s actual symptoms and the response of their symptoms to movement. Recognizing this, an alternative classification system based on identifying a patient’s preferred direction of movement (ie, directional preference, DP), has been suggested in the literature.4,12,13
The McKenzie method of mechanical diagnosis and therapy is one clinical approach which uses the DP system. In the McKenzie method, repeated movements in specific directions are used to determine the direction of movement which positively or negatively affects the patient’s symptoms.14 The McKenzie method has good evidence to support its validity, reliability, and generalizability amongst skilled practitioners, who are trained in assessment and treatment techniques.14,15 Using this method, once the preferred direction of movement for a patient is determined, it informs individual patient management.16,17
Worldwide, best practice clinical guidelines for the management of LBP almost unanimously identify exercise as a key treatment option, particularly for chronic LBP.18–20 Despite this, LBP continues to be poorly managed across the health care spectrum. In a systematic review,4 physiotherapist-prescribed DP exercises were identified as possibly being superior to other forms of exercise for patients with LBP. Anecdotal evidence indicates that those who have training in the McKenzie method or other forms of DP exercise, such as clinical pilates, use DP exercises to great effect in LBP patients.
The aim of this research was two-fold. Firstly, we summarized the current research evidence for DP exercises, as applied under the McKenzie method, in the treatment of mechanical LBP using a systematic review approach. Secondly, we operationalized findings from this review using a real-life case scenario, to demonstrate how evidence from the literature can be integrated into clinical practice.
Materials and methods
In order to gain an overview of the effectiveness of McKenzie-based DP exercises for mechanical LBP, a systematic review of the literature was conducted. Studies were included if the subjects were over 18 years of age, had LBP assessed prior to entering the study as being directional in nature (as per a McKenzie assessment), and received treatment in the form of DP exercises only. For further clarity of the inclusion criteria, the population, intervention, comparison, and outcomes (PICO) format was utilized because it provides a framework for deconstructing review parameters into distinct categories. No limits to the duration of symptoms were set. All lower limb referral and/or neurological deficit presentations were considered. All randomized controlled trials and randomized clinical trials (Level 2 evidence) were included in this review, as outlined by the Australian National Health and Medical Research Council hierarchy of evidence.23 Studies were excluded if no DP was demonstrated on baseline assessment or generic McKenzie treatment was performed, or if other manual treatment, such as massage or mobilizations, were performed as a cointervention. Education and/or use of a lumbar roll were accepted because they are common cointerventions and reflect typical clinical practice. Other exclusion criteria included LBP of neurological origin or LBP with an underlying cause, eg, spinal fractures, postoperative lumbar surgery LBP (recent or past), pregnancy, and underlying medical conditions, eg, severe osteoporosis, inflammatory or infectious conditions, diabetes, and angina.
The PICO format was used to evaluate the suitability of articles for inclusion, as outlined in Table 1.
Table 1.
Population, Intervention, Comparison and Outcomes (PICO) assessment
| Population | Adults (>18 years) presenting with mechanical low back pain, of any duration, with a directional preference* |
| Intervention | McKenzie-based, directional preference exercises |
| Comparison | All types of comparison groups were included (either control, other conservative or surgical based intervention) |
| Outcomes | All pain and functional outcomes were considered. Pain measures could include but were not limited to visual analog scale and pain medication intake. Functional outcomes could include but were not limited to the Oswestry Disability Index, Roland Morris Disability Questionnaire |
Note: Directional preference determined by McKenzie assessment.
Search strategy
A literature search was conducted on the following electronic databases: CINAHL, AMED, MEDLINE, PUBMED, EMBASE, Cochrane Library, Google Scholar, and PEDro. The following key words were used: McKenzie OR “mechanical diagnosis and therapy” OR “mechanical diagnosis” AND “low back pain” OR “spinal pain” OR “back pain” AND “exercise” OR “directional preference”. Truncation symbols were utilized as appropriate across the different databases.
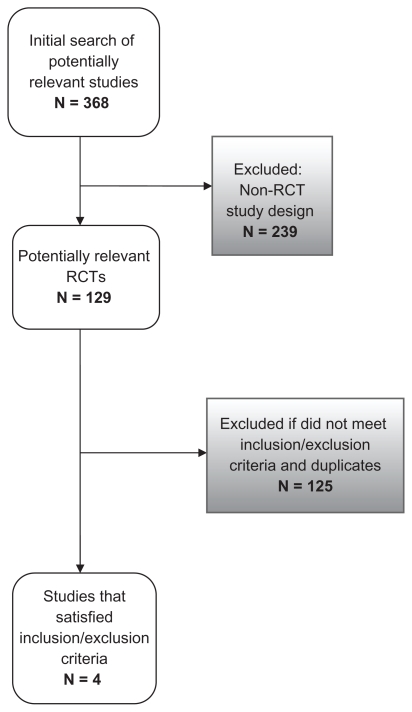
The search was limited to studies published in the English language in peer-reviewed journals from 1995 to February 2010. Date limitations reflect the increasing use of direction-specific exercises as a treatment tool for LBP in Western countries, particularly since the 1990s, and the growing body of evidence in this field from this time onwards.22 Abstracts of potentially relevant studies were reviewed and inclusion/exclusion criteria applied. Two independent researchers (AD, SC) determined eligibility for inclusion and then sought full text copies. Pearling of references was conducted to identify further eligible studies. Identified duplicates were removed to create a master list. Figure 1 provides an overview of the included and excluded studies.
Figure 1.
Consort diagram.
Critical appraisal of methodological quality
Selected studies were assessed for methodological quality by using the 11-point PEDro (Physiotherapy Evidence Database) scale.24 Two independent assessors (AD, SC) appraised each study to ensure rigor in the critical appraisal process. PEDro is a reliable scale commonly used to assess the methodological quality of randomized controlled trials. The first criterion assesses external validity and is excluded in the overall score.25 Criteria 2–11 assess internal validity and hence the score is usually given out of 10.26 Any disagreements in critical appraisal scores were resolved by discussion until consensus was reached.
Data extraction
Data was extracted by two reviewers (AD, SC). Data relating to study characteristics such as sample size, age of subjects, and duration of symptoms were collected to gain an overview of the included studies. To gain an understanding of the individual results of the studies, data relating to pain and function outcomes were collected. Results were deemed to be significant where statistical analysis reported a P value less than 0.05. In addition to significant results, treatment effect sizes were sought, and if not stated, were calculated where sufficient data were presented. Effect sizes greater than 0.6 were deemed large, between 0.06 and 0.3 moderate, and below 0.3 small. Exercise prescription parameters were identified to satisfy the secondary aim of this review.
Results
The review identified 368 studies eligible for inclusion, with 129 randomized controlled trials accepted as potentially relevant. After reviewing the studies, and applying the inclusion/exclusion criteria, four randomized controlled trials were accepted for inclusion in this review.12,13,21,22 The main reason for exclusion was the use of matched DP exercises in combination with other treatment, such as massage or spinal joint mobilization. Practicing such adjunctive treatments acts as a confounding variable to the results and prevents useful clinical conclusions from being drawn about the primary intervention. One case series article was identified26 which was a follow-up to one of the included randomized controlled trials.12 A meta-analysis of the included studies could not be undertaken due to heterogeneity.
Table 2 outlines the key characteristics of each of the included studies. Sample sizes across the four studies ranged from 25 to 321. A range of chronicity states was included. All studies included a subacute population. Two studies12,21 also included acute populations and two studies12,22 included chronic populations. All but one study22 included subjects/ patients with referred lower limb symptoms. Two studies12,22 included subjects/patients with nonsevere neurological signs, whereas two studies chose to exclude these subjects/ patients.13,21
Table 2.
Characteristics of studies
| Study | Country | Sample age (years) | Patients (n) | Presentation (acute, subacute, chronic) | Included sample |
|---|---|---|---|---|---|
| Long et al12 | Canada | 312 (18–65) | G1: DP (80) | Acute | +lower limb referral |
| US | G2: Opposite exercises to DP (69) | Subacute | +neurological signs (not severe) | ||
| Germany | G3: Multidirectional exercises (80) | Chronic | |||
| UK | |||||
| Kuwait | |||||
| Mayer et al21 | US | 100 (18–55) | G1: DP (25) | Acute | +lower limb referral (above knee) |
| G2: Heat (25) | Subacute | No neurological signs | |||
| G3: DP + heat (24) | |||||
| G4: Control, education (26) | |||||
| Schenk et al13 | US | 25 (21–76) | G1: DP (15) | Subacute | +lower limb referral |
| G2: Mobilization (10) | No neurological signs | ||||
| Cherkin et al22 | US | 321 (20–64) | G1: DP (133) | Subacute | No lower limb referral |
| G2: Chiropractic (122) | Chronic | +neurological signs (not severe) | |||
| G3: Control, education (66) |
Abbreviations: G, group; DP, directional preference.
Methodological quality of selected studies
All included studies had a score of ≥5 out of 10 (range 5–8) on the PEDro critical appraisal tool. All included studies outlined their eligibility criteria, randomly allocated their groups, had similar groups at baseline, had less than 15% dropout rates, included between-group statistical comparisons for at least one key outcome, and provided point and variability measures. One study12 blinded subjects/patients to intervention, one randomized controlled trial21 did not blind the measurer to group allocation, no study blinded the therapist to intervention, and one study22 blinded the measurer to intervention. The individual results for each criterion are displayed in Table 3.
Table 3.
PEDro results
| Study | PEDro criterion | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Long et al12 | √ | √ | √ | √ | √ | x | x | √ | √ | √ | √ | 8/10 |
| Mayer et al21 | √ | √ | x | √ | x | x | x | √ | √ | √ | √ | 6/10 |
| Schenk et al13 | √ | √ | x | √ | x | x | x | √ | x | √ | √ | 5/10 |
| Cherkin et al22 | √ | √ | √ | √ | x | x | √ | √ | √ | √ | √ | 8/10 |
Notes: √, satisfied criteria; x, did not satisfy criteria.
The four studies were all of good quality, with the main methodological flaw being a lack of subject blinding, something which is challenging in therapy intervention studies of this nature. Subject selection, allocation, and management were of a high standard in all studies, but only one study22 provided long-term follow-up data. This study reported no difference in DP exercises over time, but subject compliance and exercise progression were not reported and these factors may have affected the long-term outcomes of the exercise intervention.22 As previously mentioned, limited reporting of treatment effects (eg, effect size, confidence intervals, standard deviations) has negative implications on all study results and conclusions, because the size of the differences in effect between groups are unknown.
The individual statistical results for each study are displayed in Table 4. Only one study13 supplied enough statistical data to calculate effect sizes. In this study, the effect of DP exercises compared with mobilization as an intervention was moderate for both pain and functional outcomes, with effect sizes of 0.50 and 0.39, respectively.
Table 4.
Results of included studies
| Study | Outcome measures | Statistical significance (P < 0.05) | |
|---|---|---|---|
| Pain | Function | ||
| Long et al12 | VAS (back pain intensity) VAS (leg pain intensity) Medication (taking medication/s yes/no; amount/day) |
RMDQ | Significantly greater improvements in all outcomes for the DP group compared with comparison groups (opposite direction, multidirectional) directly post intervention #P values ranged from 0.016 to <0.001 |
| Mayer et al21 | VAS (pain relief) | RMDQ RPC-S |
Pain relief scores: Day 4* HDP > control (P = 0.000) FU (2 days) HDP > DP (P = 0.007) HDP > control (P < 0.0001) RMDQ: Day 4* HDP > control (P = 0.007) FU (2 days) HDP > H (P = 0.0267) HDP > DP (P = 0.007) HDP > control (P = 0.000) RPC-S: Day 4* HDP > DP (P = 0.018) HDP > control (P = 0.002) FU (2 days) HDP > H (P = 0.001) HDP > DP (P = 0.000) HDP > control (P < 0.0001) |
| Schenk et al13 | VAS (presenting symptoms) | OLBPDQ | Compared with the mobilization intervention group, significant results were found on both the presenting symptoms scale (P = 0.037) and OLBPDQ (P = 0.047) directly post intervention |
| Cherkin et al22 | VAS (symptoms bothersome) | RMDQ | No significant differences between DP and comparison groups pre and post intervention and at 1-year follow-up |
Notes: Data analysis performed on day 4 of a 5-day intervention;
as stated by study.
Abbreviations: VAS, 11-point visual analog scale; RMDQ, Roland Morris Disability Questionnaire; DP, directional preference exercise group; RPC-S, Rating of Perceived Capacity-Spine; FU, follow-up; HDP, heat wrap combined with DP intervention group; H, heat wrap intervention group; OLBPDQ, Oswestry low back pain disability questionnaire.
Literature summary
DP exercises were shown to be an effective form of treatment for LBP in adults in all four included studies. Three studies12,13,21 demonstrated that immediately post intervention, DP exercises were significantly better for pain and functional outcomes compared with joint mobilizations, educational control groups, and directionally opposite and multidirectional exercises. DP exercises had a positive effect on outcome when compared with baseline, and this effect was independent of symptom duration (chronicity), with subjects in each study showing improvements.
Long et al12 compared matched DP exercises with other types of exercise, and demonstrated that there was a significant difference in pain and function in favor of DP exercises compared with exercises in the opposite direction or compared with common multidirectional evidence-based exercises. Two studies compared DP exercises with education only in the form of a booklet.21,22 Mayer et al21 found that DP exercises demonstrated significant improvement when combined with a heat wrap, in both pain (pain relief visual analog scale [VAS]) and functional (Roland Morris Disability Questionnaire, Rating of Perceived Capacity-Spine) outcomes directly when practiced post intervention and at 2-day follow-up periods. Cherkin et al22 showed a trend towards significance in favor of a matched DP exercise group compared with an education only group at 4 weeks for pain (using an 11-point “bothersome” scale) outcomes. However, by 12 weeks, this trend was no longer evident, thus demonstrating no significant differences for functional outcomes between groups over time (up to 1 year of follow-up). Overall, the four studies showed positive within-group changes for those subjects undertaking DP exercises for management of their LBP.
Three studies compared matched DP exercises with other types of treatments, which included heat wrap therapy, joint mobilizations, and chiropractic treatment.13,21,22 No statistically significant differences were reported when DP exercises were compared with heat wrap therapy.21 However, when DP exercises were combined with heat wrap therapy and compared with heat wrap therapy alone, statistical differences were found for functional outcomes (Roland Morris Disability Questionnaire, Rating of Perceived Capacity-Spine) at 2-day follow-up, with no differences in pain outcomes. This finding may highlight that combinations of treatments may be better than just DP exercises in isolation. When compared with joint mobilizations, Schenk et al13 found a significant positive difference for pain and function (VAS, Oswestry Disability Index) outcomes for pre-post measures using DP exercises. No significant differences were found when DP exercises were compared with chiropractic treatment, but both intervention groups demonstrated improvements from baseline directly post intervention and at 1-year follow-up.22 Overall, the between-group changes for subjects undertaking DP exercises compared with other forms of therapy were not significant.
All studies reported different exercise parameters for the prescription of matched DP exercises.12,13,21,22 Across the four studies, there was no consistency in intensity, frequency, or duration of exercises performed.12,13,21,22 Intensity of exercises was reported in two studies13,21 and ranged from one to five sets of 10–20 repetitions. Frequency of performing exercises was not reported in the same way across all studies. All studies employed visits supervised by a trained McKenzie therapist, with a minimum of three visits over the duration of the intervention.12,13,21,22 Overall duration of exercise intervention ranged from 5 days to 1 month across the studies. No study reported the duration of a single exercise session. Description of the actual exercises was both poorly described and often omitted. Consequently, recommendations regarding best-practice prescription were not possible. Table 5 provides an overview of the exercise prescription parameters used in each study.
Table 5.
Parameters of exercises
| Study | Exercise prescription | ||
|---|---|---|---|
| Intensity | Frequency | Duration | |
| Long et al12 | NR | 3–6 visits in total 5 + home exercises/day |
2 weeks |
| Mayer et al21 | 1–2 sets 15–20 reps |
×3 supervised visits home exercises hourly | 5 days |
| Schenk et al13 | 5 sets, 10 reps | 3 visits | NR |
| Cherkin et al22 | NR | Up to 8 visits | 1 month |
Abbreviations: NR, not reported; reps, repetitions.
Cointerventions were utilized across all included studies. All studies included an educational component to their DP exercise programs, which is in line with usual clinical practice using the McKenzie method. Two studies allowed and monitored medication use as an outcome measure related to pain.12,21 One study13 included 20 minutes on the treadmill for each subject as well as education on postural correction. Another study22 provided lumbar rolls to improve posture and symptoms.
Therefore, to summarize, the findings from the systematic review indicate that DP exercises may have positive effects in the management of LBP. While the body of evidence to support this is limited (only four studies) and therefore modest at best, it does provide some emerging evidence to support the use of DP exercises in clinical practice.
Clinical case scenario
Subjective examination
The patient was a 35-year-old mother of three who presented to a McKenzie therapist complaining of a 6-month history of intermittent right-sided LBP (intensity 6/10 on VAS) radiating down her posterolateral right leg (intensity 7/10 VAS) but not extending beyond her right knee. There were no neurological symptoms. She also complained of some intermittent central LBP (intensity 4/10 VAS). The patient had no other symptoms. Overall, her symptoms were unchanged for the past 6 months.
Her symptoms were activity-dependent and were aggravated by bending, sitting for more than 15 minutes, rising from a seated position, and by any lifting activities. Her symptoms were less severe when standing for less than 30 minutes, walking, and lying down. Her symptoms were worse on waking, when she felt stiff and sore for more than 30 minutes. Her symptoms were often worse again by the end of the day. She found it difficult to get to sleep and often woke up when she was moving in bed during the night. She was usually a prone sleeper but was unable to sleep in this position due to pain. Instead, she was sleeping in a supine position on a soft mattress. Overall, she felt better when she moved and worse when she remained still. She had a past history of intermittent central LBP for the last 10 years (more than ten episodes), usually associated with bending and twisting incidents at work. She had never experienced leg pain before. This episode started after she had been gardening for three hours, with regular bending, lifting, and twisting. The next morning, she tried to put on her socks and felt immediate pain in her back, which extended into her leg that afternoon.
The patient has had no previous physiotherapy treatment for her back pain. For the current episode of pain, she has received soft tissue massage and chiropractic treatment, with only short-term relief of her symptoms for up to a maximum of 3 days. She had received ten treatments in the first 2 months, but had no treatment since that time because little improvement had been made. She presented to physiotherapy after reading about McKenzie therapy on the Internet. Her general health was good. She described herself as normally fit and active. Her children were aged 8, 6, and 2 years. Her husband worked full-time, while she normally worked part-time as a clinical aged care nurse. She had been unable to work for the past 6 months due to her symptoms. She did not attribute her symptoms to a specific workplace incident but did feel that her occupation may have contributed to her symptoms over time. She enjoyed exercise, usually going to the gym three times per week and yoga classes once per week. She was unable to do either of these activities in the previous 6 months due to her back pain. In an attempt to keep active, she has persisted with walking for 30 minutes three times per week.
On specific questioning, she was positive for pain on cough/sneeze/strain but had no bladder or gait disturbances. She was taking Nurofen®, Panadol®, and Panadeine Forte® intermittently for pain. She had a computed tomography scan which showed a broad-based central disc protrusion at L4/5 and L5/S1, which extended to the right at L4/5 and could impinge on the exiting L4 nerve root. Her only recent surgery was an elective cesarean for the birth of her third child 2 years earlier. She had no history of significant trauma or accidents, or any significant change in her weight.
Objective examination
The patient had a poor sitting and standing posture with a visibly reduced lumbar lordosis and a relevant lateral shift to the left (contralateral to side of back and leg pain). Correction of her posture resulted in a mild reduction in her leg pain to 5/10 as determined by VAS. Correction of her lateral shift resulted in a further reduction in leg pain to 3/10 VAS. Neither of these corrections changed her LBP. Neurological examination was normal for sensation, power, and reflexes. The patient had a restricted straight leg raise on the right to 60° compared with 80° on the left. She had some pain reproduction on the right side around her knee (3/10 VAS). Resting pain prior to active movement testing was 5/10 VAS at the right lumbar spine and 5/10 VAS at the right leg. Active range of lumbar flexion had a major loss of movement (only able to reach her mid thigh) with significant symptom aggravation (increased back and leg pain to 7/10 VAS). Active range of lumbar extension had a major loss of movement (down to less than 15°), with no increase in resting leg pain but an increase in resting LBP to 7/10 VAS. Side gliding to the right had a major loss of movement (less than 15°) with increased LBP (7/10 VAS) but no increase in leg pain. Side gliding to the left had no loss of movement and no increase in pain.
On repeated movement testing, the following results were observed (resting back and leg pain 5/10 VAS): single extension in standing, increased back pain (7/10 VAS), no worse afterwards; repeated extension in standing ×10, increased back pain during testing (7/10 VAS) and better after testing (4/10 VAS), leg pain unchanged, increased range of extension with increased repetitions; second set of extension in standing ×10, decreased leg pain during testing (4/10), centralizing, increased LBP (6/10 VAS), better after testing, centralized leg pain not abolished; and repeated extension in lying ×10, decreased back and leg pain during testing (3/10 VAS), centralizing, abolished with further repetitions, better after testing, centralized to LBP (3/10 VAS).
Due to the positive response from repeated extension movements, no further testing was conducted after initial assessment. A provisional classification was made of a derangement (likely posterolateral), with symptoms being unilateral, asymmetrical, and above the knee.
Clinical management
The patient was educated about her current symptoms and the underlying pathology within the McKenzie framework. She was informed about the importance of good posture and given a lumbar roll to use during all sitting activities. No mechanical therapy was provided on day 1 to monitor her response to movement-based treatment. She was treated using the extension principle in the first instance, given her positive response to testing. This involved lying prone, repeated extension in prone to elbows and then repeated full range extension in prone. This was complemented by repeated extension in standing. Exercises were completed in sets of 10 repetitions and were to be performed every 2–3 hours during the day, or when she felt her back and leg pain. The patient left her physiotherapy appointment with no leg pain and only a central dull ache in her lumbar spine (3/10 VAS). She had a good understanding of her condition and knew what she needed to do in order to assist herself to get better.
Clinical evidence-based commentary
The case is a common clinical presentation in physiotherapy practice. Patients with longstanding back pain with or without referred leg pain can be a challenging group to treat. One of the key elements in the treatment of this group of patients is establishing the cause of the symptoms, if known, from investigations and clinical testing. The case study is presented in terms of a standard McKenzie assessment, using the standardized McKenzie Institute International Lumbar Spine Assessment form (available via the McKenzie Institute International website http://www.mckenziemdt.org/forms/2006MIIAssessmentFormLumbar.pdf). These forms are used by McKenzie therapists around the world as a standardized means of assessing and treating patients with spinal pain.
The key component to any McKenzie assessment is the establishment of a preferred direction of movement for the patient. This information is gained from both the subjective and objective examination. The activities of sitting, bending, and lifting are all flexion-biased activities for the lumbar spine, whereas standing and walking tend to be more extension-biased activities. In the present case, the patient’s occupation as a nurse was highly flexion-biased and her leisure activities of gym and yoga also tended to involve extended periods of flexion, depending on the activities undertaken. Her regular walks were more of an extension activity. With three children, this also exposed the patient to regular flexion loads on her lumbar spine. Many of our usual daily activities, such as washing dishes, making the bed, and driving a car are flexion-biased as well. Thus, from the subjective information, it is assumed that the patient preferred extension activities (standing and walking) but had to engage in numerous flexion activities as part of her usual life. Her mechanism of injury tended towards a flexion bias in terms of activity, which could be indicative of a need to consider an extension bias in her treatment. In her objective assessment, she demonstrated a reduced range of movement and pain reproduction on flexion, extension, and side gliding to the right, which did not support or negate any preferred direction. However, on repeated movement testing, she demonstrated a clear preference for repeated extension. This direction of movement was chosen for repeated testing based on the subjective examination and the positive (centralizing) response to a single lumbar extension movement.
Her management reflects usual clinical practice for McKenzie therapists treating patients with derangement presentations, a subclassification used by qualified therapists to group patients with particular symptoms together. The use of DP exercises in the management of patients with derangements is standardized between McKenzie therapists. There is no one set formula of exercises which are prescribed to every patient with LBP. In fact, exercise prescription is highly individualized, despite popular opinion which sometimes presents McKenzie therapy as extension-only exercises.
Translating evidence into clinical practice
Evidence from our literature review on the use of DP exercises in the treatment of LBP reveals emerging scientific evidence in support of this form of therapy. Four randomized controlled studies contributed to the body of evidence for the use of DP exercises in the treatment of LBP.12,13,22,27 Although modest, the body of evidence supports the use of DP exercises in reducing pain and improving function in patients with LBP. Specifically, across the four studies, the within-group changes in pain and function were significant for the DP exercise groups. The findings were less marked during between-group comparisons, but a positive trend towards significance was identified and DP exercises were at least as effective as other treatment strategies. In research undertaken by Long et al,12,27 it was demonstrated that patients who were given exercises that correlated with their preferred direction of movement did better than those given exercises in their nonpreferred direction or generalized exercises. Mayer et al21 demonstrated that heat and DP exercises were better than either modality in isolation or no treatment at all. The use of heat is not standardized amongst McKenzie therapists, but is a commonly used adjunct in the treatment of many conditions, and these findings could be applied to LBP patients. Similarly, Schenk et al13 reported positive benefits for pain and function when using DP exercises. Cherkin et al22 also support these findings by reporting that DP exercises were equally beneficial in improving pain and function when compared with chiropractic treatment. These findings collectively hold clinical significance because DP exercises may promote active management, demonstrate cost-effectiveness, and enable patient empowerment through self-management of symptoms.15 For health practitioners who are frequently faced with the difficult decision of which treatment strategy to choose for the best results, these findings may prove helpful.
While collectively the use of DP exercises has been shown to be effective in improving pain and function for patients with LBP, the parameters underpinning the clinical application of DP exercises are inconsistent. All studies used different exercise prescription rationales and this meant that conclusions regarding the most effective prescription (ie, intensity, frequency, duration) for DP exercises could not be identified. The prescription outlined in the case study is recommended by McKenzie therapists, but there is currently a lack of research which specifically validates or justifies these prescription parameters. Cointerventions were commonly used and included heat, medications, treadmill walking, and lumbar roll. The use of the lumbar roll is standard practice amongst McKenzie therapists16,28,29 and this is reflected in the current literature. In the study by Cherkin et al22 lumbar rolls were used to improve posture and symptoms.
Summary
There has been a growing movement in allied health which recognizes the benefit of the McKenzie method in treating LBP. Within the McKenzie framework, DP exercises are commonly utilized in clinical practice for managing LBP. Although underpinned by a modest body of evidence, the findings from this systematic review of the literature support current clinical practice perspectives where DP exercises have been shown to have positive effects in the management of LBP. Because the McKenzie method promotes self-management, the use of DP exercises, in conjunction with other common manual therapy treatments, such as mobilization, manipulation, and general exercise, may present a cost-effective and time-efficient approach to managing LBP. Using a real-life case scenario, we have outlined how the evidence from the literature can be implemented in clinical practice, by building on the established frameworks of evidence-based practice. For health practitioners, this approach can assist in operationalizing the research evidence into an everyday clinical context. While there is emerging evidence for DP exercises, there are persistent evidence gaps. They include variability in the reporting of parameters, compliance, and cost-effectiveness of DP exercises. Future research focusing on broadening the evidence base for DP exercises and addressing these gaps in the literature is required.
Acknowledgments
The authors gratefully acknowledge Zuzana Machotka, Khushnum Pastakia, and Dr Helen Clare for their assistance and feedback during the preparation of this manuscript.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Swinkels A, Cochrane K, Burt A, Johnson L, Lunn T, Rees AS. Exercise interventions for non-specific low back pain: an overview of systematic reviews. Phys Ther Rev. 2009;14(4):247–259. [Google Scholar]
- 2.Truchon M. Determinants of chronic disability related to low back pain: Towards an integrative biopsychosocial model. Disabil Rehabil. 2001;23(17):758–767. doi: 10.1080/09638280110061744. [DOI] [PubMed] [Google Scholar]
- 3.Chou R. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. [DOI] [PubMed] [Google Scholar]
- 4.Cook C, Hegedus EJ, Ramey K. Physical therapy exercise intervention based on classification using the patient response method: a systematic review of the literature. J Man Manip Ther. 2005;13(3):152–162. [Google Scholar]
- 5.Furlan AD, Imamura M, Dryden T, Irvin E. Massage for low back pain. Cochrane Database Syst Rev. 2008;(4):CD001929. doi: 10.1002/14651858.CD001929.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Hilde G, Hagen KB, Jamtvedt G, Winnem M. Advice to stay active as a single treatment for low-back pain and sciatica. Cochrane Database Syst Rev. 2006;(2):CD003632. doi: 10.1002/14651858.CD003632. [DOI] [PubMed] [Google Scholar]
- 7.Pengel LH, Refshuage KM, Maher CG, Nicolas MK, Herbert MK, McNair P. Physiotherapist-directed exercise, advice, or both for subacute low back pain: a randomized trial. Ann Intern Med. 2007;146(11):787–796. doi: 10.7326/0003-4819-146-11-200706050-00007. [DOI] [PubMed] [Google Scholar]
- 8.Slade SC, Keating JL. Unloaded movement facilitation exercise compared to no exercise or alternative therapy on outcomes for people with nonspecific chronic low back pain: a systematic review. J Manipulative Physiol Ther. 2007;30(4):301–311. doi: 10.1016/j.jmpt.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Cairns MC, Foster NE, Wright C. Randomized controlled trial of specific spinal stabilization exercises and conventional physiotherapy for recurrent low back pain. Spine. 2006;31(19):E670–E681. doi: 10.1097/01.brs.0000232787.71938.5d. [DOI] [PubMed] [Google Scholar]
- 10.Richardson CA, Snijders CJ, Hides JA, Damen L, Pas MS, Storm J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine. 2002;27(4):399–405. doi: 10.1097/00007632-200202150-00015. [DOI] [PubMed] [Google Scholar]
- 11.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain. Spine. 2006;31(6):623–631. doi: 10.1097/01.brs.0000202807.72292.a8. [DOI] [PubMed] [Google Scholar]
- 12.Long A, Donelson R, Fung T. Does it matter which exercise? A randomised control trial of exercise for low back pain. Spine. 2004;29(23):2593–2602. doi: 10.1097/01.brs.0000146464.23007.2a. [DOI] [PubMed] [Google Scholar]
- 13.Schenk RJ, Jozefczyk C, Kopf A. A randomized trial comparing interventions in patients with lumbar posterior derangement. J Man Manip Ther. 2003;11(2):95–102. [Google Scholar]
- 14.Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50(4):209–216. doi: 10.1016/s0004-9514(14)60110-0. [DOI] [PubMed] [Google Scholar]
- 15.May S, Donelson R. Evidence-informed management of chronic low back pain with the McKenzie method. Spine J. 2008;8(1):134–141. doi: 10.1016/j.spinee.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 16.Machado LAC, von Sperling de Souza M, Ferreira PH, Ferreira ML. The McKenzie method for low back pain: A systematic review of the literature with a meta-analysis approach. Spine. 2006;31(9):E258–E262. doi: 10.1097/01.brs.0000214884.18502.93. [DOI] [PubMed] [Google Scholar]
- 17.Maguire K. Outcome analysis in those who demonstrated a directional preference from those who did not: Audit of MDT. J Mech Diag Ther. 2005;13(3):21–26. [Google Scholar]
- 18.Accident Compensation Corporation New Zealand. Acute low back pain guide. Wellington, New Zealand: 2004. [Accessed September 27, 2011]. Available at: http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_communications/documents/guide/prd_ctrb112930.pdf. [Google Scholar]
- 19.Airaksinen O, Brox JI, Cedraschi C, et al. European guidelines for the management of chronic non-specific low back pain, 2004. [Accessed September 27, 2011]. Available at: http://www.backpaineurope.org/web/html/wg2_results.html.
- 20.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 21.Mayer JM, Ralph L, Look M, et al. Treating acute low back pain with continuous low-level heat wrap therapy and/or exercise: a randomized controlled trial. Spine J. 2005;5(4):395–403. doi: 10.1016/j.spinee.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339(15):1021–1029. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 23.Evans D. Hierarchy of evidence: a framework for ranking evidence evaluating healthcare interventions. J Clin Nurs. 2003;12(1):77–84. doi: 10.1046/j.1365-2702.2003.00662.x. [DOI] [PubMed] [Google Scholar]
- 24.PEDro. PEDro scale. [Accessed September 26, 2011]. Available at: www.pedro.org.au/wp-content/uploads/PEDro_scale.pdf.
- 25.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 26.Moher D, Cook DJ, Jadad AR. Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses. Health Technol Assess. 1999;3(12):1–98. [PubMed] [Google Scholar]
- 27.Long A, May S, Fung T. Specific directional exercises for patients with low back pain: a case series. Physiother Can. 2008;60(4):307–317. doi: 10.3138/physio.60.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller ER, Schenk RJ, Karnes JL, Rousselle JG. A comparison of the McKenzie approach to a specific spine stabilisation program for chronic low back pain. J Man Manip Ther. 2005;13:103–112. [Google Scholar]
- 29.Underwood MR, Morgan J. The use of a back class teaching extension exercises in the treatment of acute low back pain in primary care. Fam Pract. 1998;15(1):9–15. doi: 10.1093/fampra/15.1.9. [DOI] [PubMed] [Google Scholar]