Abstract
The present investigation examines anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations in relation to Coping and Conformity marijuana use motives among a sample of young adult marijuana users (n = 135; 46.7% women; Mage = 20.45, SD = 5.0). After controlling for current marijuana use frequency (past 30 days), daily cigarette smoking rate, average volume of alcohol used over the past year, negative affectivity, and other marijuana use motives, anxiety sensitivity was significantly and uniquely associated with Coping and Conformity motives for marijuana use. Distress tolerance evidenced significant and unique incremental relations to Coping motives, whereas fear reactivity to bodily sensations was unrelated to any marijuana use motive. These results provide novel information related to the role of emotional sensitivity and tolerance factors as they pertain to specific types of motives for marijuana use among young adults.
Keywords: anxiety sensitivity, distress tolerance, marijuana, motives
Marijuana is the most frequently used and abused illicit drug in the United States and many other parts of the world (Office of Applied Studies [OAS], 2004; Substance Abuse and Mental Health Services Administration [SAMHSA], 1998). For example, approximately 25 million people (8.6%) in the United States have used marijuana in the past year (Johnston, O’Malley, Bachman, & Schulenberg, 2005). Marijuana use is particularly prevalent among young adults, with 34% of college students reporting past year use, 19% reporting past month use, and 5% reporting daily use (Johnston et al., 2005; Mohler-Kuo, Lee, & Weschler, 2003). Moreover, recent research has indicated increased rates of marijuana abuse and dependence among young adults in the United States (Compton, Grant, Colliver, Glantz, & Stinson, 2004). These data are alarming from a public health perspective, as regular and heavy users of marijuana are at an increased risk for a variety of problems, including, but not limited to, medical illness (e.g., chronic bronchitis; Bloom, Kaltenborn, Paoletti, Camilli, & Lebowitz, 1987), risk-taking behavior (e.g., unprotected sexual intercourse; McDonald, Schleifer, Richards, & de Wit, 2003), and interpersonal impairment (Stephens, Roffman, & Simpson, 1993).
To forward the scientific study of the nature of marijuana use, researchers are increasingly applying motivational models to understand marijuana use. This work has built from the motivational study of alcohol (Cooper, Frone, Russell, & Mudar, 1995; Cox & Klinger, 1988; Stewart, Zeitlin, & Samoluk, 1996; Stewart, Zvolensky, & Eifert, 2001) and tobacco use (Ikard, Green, & Horn, 1969; Piper et al., 2004; Russell, Peto, & Patel, 1974; Zvolensky, Feldner et al., 2004). Such an approach recognizes that there are a number of distinct motives for using marijuana that can vary both between and within individuals (Cooper, 1994). That is, two individuals may use marijuana for different reasons, and one individual may use for multiple reasons. Motivational models predict that distinct motives may theoretically be related to particular types of problems (Cooper, 1994). For example, specific motives may play unique roles in various aspects of use (e.g., addictive use, withdrawal symptoms, and craving) or problems related to use (e.g., psychological disturbances and risk-taking behavior). Thus, enhancing efforts to empirically explicate marijuana use motives will presumably facilitate, as it has for alcohol and tobacco use (Cooper, 1994; Piper et al., 2004), an under-standing of the nature of marijuana use and its disorders, as well as linkages between marijuana use and its clinically important correlates.
J. Simons, Correia, Carey, and Borsari (1998) developed the Marijuana Motives Measure (MMM) to identify various marijuana use motives. Research using the 25-item MMM measure has thus far indicated that there are distinct, replicable, and internally consistent factors of marijuana use motives (J. Simons, Correia, & Carey, 2000), specifically, Enhancement (e.g., “because it’s exciting”), Conformity (e.g., “to fit in with the Group I like”), Expansion (e.g., “to expand my awareness”), Coping (e.g., “to forget my worries”), and Social motives (e.g., “because it makes social gatherings more fun”; Chabrol, Duconge, Casas, Roura, & Carey, 2005; J. Simons et al., 1998; Zvolensky et al., 2007). Specific marijuana use motives have shown explanatory relevance in a variety of ways. For example, Coping motives for marijuana use mediate the relation between social anxiety and marijuana use problems (Buckner, Bonn-Miller, Zvolensky, & Schmidt, 2007) as well as the relation between negative affect regulation expectancies and marijuana use problems (J. S. Simons, Gaher, Correia, Hansen, & Christopher, 2005). Other work indicates that Enhancement, Expansion, Coping, and Social motives have been related to greater frequency of marijuana use (Bonn-Miller, Vujanovic, Feldner, Bernstein, & Zvolensky, 2007; Bonn-Miller, Zvolensky, & Bernstein, 2007; Buckner et al., 2007; J. Simons et al., 1998). Overall, by better understanding the nature of marijuana use motives, it will be possible to build more integrated and comprehensive models of marijuana use behavior. Such knowledge can ultimately contribute to the development and refinement of intervention approaches for marijuana use and its disorders.
One line of inquiry in regard to the study of marijuana use motives has focused on relations between emotional vulnerability factors and coping-oriented marijuana use (e.g., Bonn-Miller, Vujanovic, & Zvolensky, 2008; Comeau, Stewart, & Loba, 2001). This work has been influenced by the recognition that anxiety and depressive symptoms and their disorders co-occur with frequent (e.g., daily) and problematic marijuana use (Agosti, Nunes, & Levin, 2002; Bovasso, 2001; Brook, Brook, Zhang, Cohen, & Whiteman, 2002; Dannon, Lowengrub, Amiaz, Grunhaus, & Kotler, 2004; Grant, 1995; Weller & Halikas, 1985; Zvolensky, 2006; Zvolensky, Lewinsohn et al., 2008). Anxiety sensitivity is one possible contributing factor for these observed linkages between anxiety and marijuana use problems. Anxiety sensitivity reflects individual differences in the fear of anxiety and arousal-related sensations (McNally, 2002; Taylor, 1999). When anxious, individuals high in anxiety sensitivity become acutely fearful because of beliefs that these interoceptive sensations have harmful physical, psychological, or social consequences (Taylor et al., 2007). Over time, elevated levels of anxiety sensitivity predict greater risk for anxiety and, to a lesser extent, depressive symptoms and disorders (Feldner, Zvolensky, Schmidt, & Smith, 2008; Hayward, Killen, Kraemer, & Taylor, 2000; Li & Zinbarg, 2007; Maller & Reiss, 1992; Schmidt, Lerew, & Jackson, 1997, 1999; Schmidt, Zvolensky, & Maner, 2006). Anxiety sensitivity has been shown to be significantly related to coping-oriented marijuana use motives among adolescents (Comeau et al., 2001) and adults (Bonn-Miller, Zvolensky et al., 2007; Mitchell, Zvolensky, Marshall, Bonn-Miller, & Vujanovic, 2007). To the extent that anxiety sensitivity is associated with increased risk for anxiety and depressive symptoms, persons with high levels of this factor in comparison with low levels may desire to use drugs such as marijuana to cope with such distressing symptoms. In this sense, this emotional sensitivity factor may be important for understanding the putative linkages between marijuana use problems and anxiety and depressive emotional disturbances.
Although promising, extant work on anxiety sensitivity and marijuana use motives has been limited in a number of substantive respects. First, there is evidence that anxiety sensitivity is a lower-order factor, along with distress tolerance (the perceived ability to experience and endure negative emotional states; Simons & Gaher, 2005), of a common higher-order emotional sensitivity and tolerance construct (Bernstein, Zvolensky, Vujanovic, & Moos, in press). Thus, anxiety sensitivity and distress tolerance are related, but distinct, constructs, showing differential relations to a number of psychologically based criterion variables (Bernstein, Zvolensky, et al., in press). Work on distress tolerance and Coping and other marijuana use motives is highly limited. One study found that distress tolerance, as measured by the Distress Tolerance Scale (DTS; J. S. Simons & Gaher, 2005), was negatively related to Coping motives (r = −.20) for marijuana use among undergraduate marijuana users (J. S. Simons & Gaher, 2005). In other words, individuals who were less able to tolerate negative emotional states reported greater motivation to smoke to cope with such emotional states. Given that anxiety sensitivity and distress tolerance are related, but theoretically and empirically distinct (lower-order factors of a common higher-order latent construct; Bernstein et al., in press), it is necessary to evaluate the relations between these factors and Coping motives for marijuana use in one overarching model (i.e., in the context of one another). Here, it is possible that both sensitivity to (anxiety sensitivity) and tolerance for (distress tolerance) negative emotional states are important explanatory constructs for understanding Coping motives for marijuana use. For example, a marijuana user fearful of expected negative consequences of anxiety symptoms (anxiety sensitivity) may desire to use marijuana to regulate his or her anticipatory anxiety, and a person with lower levels of distress tolerance may be motivated to use marijuana to cope with his or her limited ability to tolerate noxious emotional states.
Second, emerging work has identified an association between more frequent (e.g., daily use) and problematic (e.g., dependent) marijuana use and increased risk for panic attacks and panic disorder (Zvolensky, Bernstein et al., 2006; Zvolensky et al., 2008). This work indicates that heavy marijuana use may be related to high levels of fear reactivity, reflecting the degree of emotional responsivity to internal cues (e.g., bodily sensations, often measured, as in the present study, via reactivity to biological challenge; Zvo-lensky & Eifert, 2000); we use the terms panic attacks and fear reactivity interchangeably throughout this article (Barlow, 2002). It is therefore possible that fear reactivity (indexed by the tendency to have a panic attack; Barlow, 2002), which is related to anxiety sensitivity and distress tolerance (Bernstein, Zvolensky, Marshall, & Schmidt, in press), reflects an emotional reactivity variable that also could be related to coping-oriented marijuana use. As such, the previously noted relations between anxiety sensitivity and distress tolerance and coping-oriented marijuana use motives could possibly be better accounted for by shared variance with fear reactivity to interoceptive cues. Alternatively, the examination of these three related factors may reveal both shared and unique relations with coping-oriented marijuana use motives and, thereby, a more ecologically valid model of emotional vulnerability in regard to motivation to use marijuana.
Third, there is limited study in general about the role of emotional sensitivity, tolerance, and fear reactivity variables in relation to marijuana use motives other than coping motives. Such study is important to determine the specificity of these emotional vulnerability factors in regard to marijuana use motives. Among adolescents, anxiety sensitivity has been found to be related to Conformity motives for marijuana use (Comeau et al., 2001). Thus, adolescent youth who are sensitive to the expected negative consequences of anxiety symptoms may be more motivated to use marijuana to conform to perceived peer pressure for such drug use. It is unknown whether a similar effect is evident for adults.
Finally, past work on anxiety sensitivity, as well as distress tolerance, has not taken into account the shared variance among marijuana use motives. This limitation is problematic, because marijuana use motives are strongly correlated with one another (Chabrol et al., 2005; J. Simons et al., 1998; Zvolensky et al., 2007). Thus, it is unclear whether emotional sensitivity (anxiety sensitivity), tolerance (distress tolerance), or fear reactivity factors are uniquely related to only certain marijuana use motives (i.e., coping motives) but not other marijuana use motives, after accounting for their shared variance.
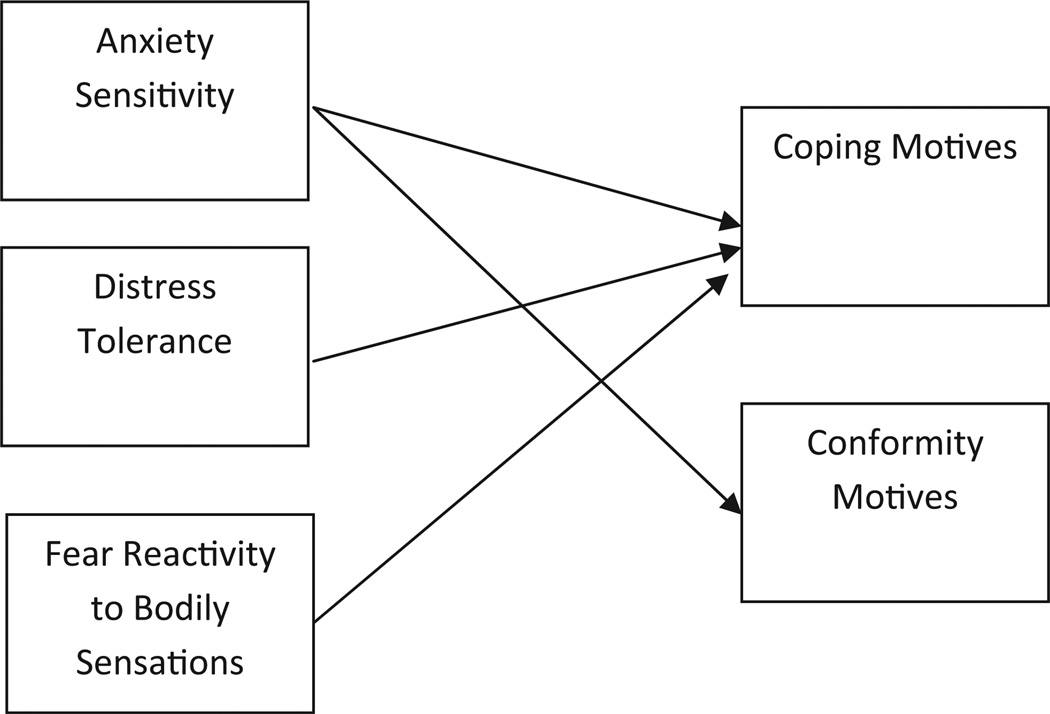
The present investigation sought to address key limitations of past work by comprehensively evaluating anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations in regard to motives for marijuana use among a community-recruited young adult sample of current marijuana users. Although past work on affective vulnerability for marijuana use and its disorders has largely thus far been atheoretical, the current study attempted to study three putative vulnerability constructs of possible relevance in one overarching model. In this sense, the study helps generate as well as test, in an overarching model risk, candidates for certain types of marijuana motivation for use. It was hypothesized that anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations would each make unique explanatory contributions to Coping motives for marijuana use (see Figure 1). These effects were expected to be evident above and beyond the variance accounted for by concurrent substance use (current marijuana, tobacco, and alcohol use), a broad-based tendency to experience negative affect (negative affectivity), and shared variance with other marijuana use motives. Additionally, it was hypothesized, on the basis of past work with adolescents (Comeau et al., 2001), that anxiety sensitivity, but not distress tolerance or fear reactivity to bodily sensations, would be incrementally related to Conformity motives for marijuana use (see Figure 1).
Figure 1.
Anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations in relation to coping and conformity motives for marijuana use.
Method
Participants
The present sample consisted of 135 community-recruited young adult (46.7% women; Mage = 20.45, SD = 5.0) current marijuana smokers. Generally consistent with the racial distribution of Vermont (Vermont Department of Health, 2007), 95% of participants identified as Caucasian, 0.7% African American, 0.7% Asian, 0.7% Hispanic, 0.7% bi- or multiracial, 1.5% other, and 0.7% did not provide ethnic data. Sixty-seven percent of the sample smoked marijuana at least once per week, and 24.4% smoked more than once per day. The mean age for first-time marijuana use was 14.96 (SD = 2.2) years, and the mean age of onset for regular marijuana use was 15.4 (SD = 4.89) years. Thirty-one percent of the sample met diagnostic criteria for marijuana abuse, while 29% met criteria for marijuana dependence. The remaining 40% of the sample were marijuana users who did not meet diagnostic criteria for a marijuana use disorder.
Sixty-three percent of the participants smoked cigarettes on a daily basis, averaging 8.24 (SD = 12.63) cigarettes per day. Cigarette smoking status was verified for all participants by carbon monoxide (CO) analysis at 10 ppm cutoff (Cocores, 1993). Participants in the present sample reported smoking their first cigarette at 13.83 years of age (SD = 3.56), and smoking daily at 16.2 years of age (SD = 3.75). Participants scored an average of 2.98 (SD = 1.85) on the Fagerstrom Test for Nicotine Dependence (FTND; Heatherton, Koz-lowski, Frecker, & Fagerstrom, 1991), indicating low levels of nicotine dependence. On average, participants reported drinking alcohol an average of 2–3 days per week and consuming an average of 5–6 drinks per occasion. Additionally, participants scored an average of 11.85 on the Alcohol Use Disorders Identification Test (AUDIT; Babor, De La Fuente, Saunders, & Grant, 1992; SD = 5.47), with 65.7% of participants meeting criteria for at least moderate alcohol problems.
Participants were deemed eligible for enrollment in the present study if they endorsed marijuana use within the past 30 days and were between the ages of 18 and 65 years. Participants were excluded on the basis of the following criteria: (a) current Axis I psychopathology excluding substance use disorders; (b) current use of psychotropic medication; (c) current suicidality or homicidality; (d) current or past chronic cardiopulmonary illness (e.g., chronic obstructive pulmonary disease or severe asthma); (e) current acute respiratory illness (e.g., bronchitis), (f) seizure disorder, cardiac dysfunction, or other serious medical illness (e.g., history of seizures or emphysema); (g) pregnancy (women); and (h) limited mental competency or inability to give informed, written consent. Overall, these exclusionary criteria (a) helped to ensure the safety of participants during the biological challenge wherein fear reactivity to bodily sensations was tested and (b) ruled out alternative explanations to any observed effects. For example, if individuals with current Axis I conditions were included, it is possible that psychopathology status, rather than any of the studied emotional vulnerability factors, could account for observed relations with marijuana use motives because of the relations between psychopathology and anxiety sensitivity, distress tolerance, and panic attacks (Schmidt et al., 2006; J. S. Simons & Gaher, 2005).
Measures
The Structured Clinical Interview—Non-Patient Version (SCID–N/P; First, Spitzer, Gibbon, & Williams, 1994) for the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994) was administered as a screener in order to rule out psychopathology and assess current suicidal ideation (see exclusionary criteria). In addition, current marijuana abuse and dependence (with the inclusion of substance withdrawal criteria as defined by the DSM–IV for other drugs and as assessed by the SCID–N/P for other drug classes) was determined using the SCID–N/P. Although the SCID–N/P has high rates of reliability in terms of interrater agreement (First et al., 1994), we did not compute such reliability ratings in the current study because just the screening aspect of the measure was used.
Marijuana smoking history was assessed with the Marijuana Smoking History Questionnaire (MSHQ; Bonn-Miller & Zvolensky, 2005). The MSHQ is a self-report instrument that assesses marijuana smoking rate (lifetime and past 30 days), age of onset at initiation, years of being a regular marijuana smoker, and other descriptive information (e.g., number of attempts to discontinue using marijuana). The MSHQ has been used successfully in the past as a descriptive measure of marijuana use history and pattern (Bonn-Miller, Zvolensky, Leen-Feldner, Feldner, & Yartz, 2005; Zvolensky, Bonn-Miller et al., 2006).
Marijuana motives for use were assessed with the Marijuana Motives Measure (MMM; J. Simons et al., 1998). The MMM is a 25-item measure in which respondents indicate on a 5-point Likert-type scale (1 = almost never/never to 5 = almost always/always) the degree to which they have smoked marijuana for a variety of possible reasons (e.g., “to be sociable”). Factor analysis of the scale indicates that it has five first-order factors entitled Enhancement (e.g., “because it’s exciting”), Conformity (e.g., “to fit in with the group I like”), Expansion (e.g., “to expand my awareness”), Coping (e.g., “to forget my worries”), and Social (e.g., “because it makes social gatherings more fun”; J. Simons et al., 1998; Zvolensky et al., 2007). The MMM has high levels of internal consistency for each of the five factors (range of alpha coefficients: .72 to .92) and has been successfully used in the past to measure motivation for using marijuana (Chabrol et al., 2005). In the present study, only the Coping and Conformity marijuana use motives were studied as criterion variables because of their theoretical relevance to the study objectives.
The Smoking History Questionnaire (SHQ; Brown, Lejuez, Kahler, & Strong, 2002) is a self-report questionnaire used to assess cigarette smoking history and pattern. The SHQ includes items pertaining to smoking rate, age of onset of smoking initiation, and years of being a daily smoker. The SHQ also assesses information regarding quit attempts, including problematic symptoms experienced during such attempts. The SHQ has been successfully used in previous studies as a measure of smoking history, pattern, and symptom problems during quitting (Zvolensky, Lejuez, Kahler, & Brown, 2004). The current investigation utilized the SHQ to determine rate of cigarette smoking.
The Fagerström Test for Nicotine Dependence (FTND; Heatherton et al., 1991) is a 6-item scale designed to assess gradations in tobacco dependence (Heatherton et al., 1991). The FTND has shown good internal consistency, positive relations with key cigarette smoking variables (e.g., saliva cotinine; Heatherton et al., 1991; Payne, Smith, McCracken, McSherry, & Antony, 1994), and high degrees of test–retest reliability (Pomerleau, Carton, Lutzke, Flessland, & Pomerleau, 1994).
Biochemical verification of cigarette smoking history was completed by carbon monoxide (CO) analysis of breath samples (10 ppm cutoff; Cocores, 1993). Expired air CO levels were assessed using a CO carbon monoxide monitor (Model 3110; Spirometrics, Inc., Gray, Maine). CO analysis of breath samples was used to verify cigarette smoking status (abstinence/smoking) at baseline.
The Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 1992) is a 10-item self-report screening measure developed by the World Health Organization to identify individuals with alcohol problems (Babor et al., 1992). There is a large body of literature attesting to the reliability and validity of the AUDIT (e.g., Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). In the present study, the frequency and quantity items from the AUDIT were used to index current alcohol consumption (an average frequency-by-quantity composite score; Stewart et al., 2001). Additionally, the AUDIT total score was utilized to identify current difficulties with alcohol use (Babor et al., 1992).
The Positive Affect Negative Affect Scale (PANAS; Watson, Clark, & Tellegen, 1988) is a 20-item measure in which respondents indicate, on a 5-point Likert-type scale (1 = very slightly or not at all to 5 = extremely), the extent to which they generally feel different feelings and emotions (e.g., “hostile”). The PANAS is a well-established mood measure commonly used in psychopathology research (Watson et al., 1988), and factor analysis indicates that the PANAS assesses the global dimension of negative affect (PANAS–NA). The PANAS–NA subscale has demonstrated good convergent and discriminant validity (Watson, 2000). Additionally, the negative affect scale demonstrated high levels of internal consistency in the current sample (Cronbach’s alpha = .82).
The Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986) is a 16-item measure in which respondents indicate, on a 5-point Likert-type scale (0 = very little to 4 = very much) the degree to which they are concerned about possible negative consequences of anxiety symptoms (e.g., “It scares me when I feel shaky”). The ASI has high levels of internal consistency for the global score (Cronbach’s alpha = .84 in the current sample). The ASI is unique from, and demonstrates incremental validity in relation to, trait anxiety (Rapee & Medoro, 1994) as well as negative affectivity (Zvolensky, Kotov, Antipova, & Schmidt, 2005). In the present investigation, the total ASI score was used, because it represents the global-order AS factor and therefore takes into consideration different types of fears, including fears of anxiety-related somatic, cognitive, and social cues.
The Distress Tolerance Scale (DTS; J. S. Simons & Gaher, 2005) is a 14-item self-report measure in which respondents indicate, on a 5-point Likert-type scale (1 = strongly agree to 5 = strongly disagree), the extent to which they can experience and withstand distressing psychological states (J. S. Simons & Gaher, 2005). The DTS encompasses four types of emotional distress items including perceived ability to tolerate emotional distress (e.g., I can’t handle feeling distressed or upset), subjective appraisal of distress (e.g., My feelings of distress or being upset are not acceptable), attention being absorbed by negative emotions (e.g., When I feel distressed or upset, I cannot help but concentrate on how bad the distress actually feels), and regulation efforts to alleviate distress (e.g., When I feel distressed or upset I must do something about it immediately; J. S. Simons & Gaher, 2005). High levels of distress tolerance are indicated by higher scores on the DTS (J. S. Simons & Gaher, 2005). In the present sample, the DTS demonstrated high levels of internal consistency (Cronbach’s alpha =.86). We used the total DTS score in the current study (a) to facilitate comparability to past research (e.g., J. S. Simons & Gaher, 2005) and (b) because the hypotheses being evaluated pertained to a global distress tolerance construct.
Laboratory assessment
The Diagnostic Sensations Questionnaire (DSQ; Sanderson, Rapee, & Barlow, 1988, 1989) was used to assess DSM–IV panic attack symptoms immediately postchallenge. This measure is frequently used in challenge work (Forsyth, Eifert, & Canna, 2000; Schmidt, Forsyth, Santiago, & Trakowski, 2002; Zvolensky, Lejuez, & Eifert, 1998). Ratings for the DSQ are made on a 9-point Likert-type scale (0 = not at all to 8 = very strongly felt). The DSQ lists DSM–IV panic symptoms and, as in past studies (Sanderson et al., 1989; Zvolensky et al., 1998), was used to measure fear reactivity to bodily sensations (Sanderson et al., 1989). In the present investigation, as in past work (Abrams et al., 2008; Bernstein, Zvolensky, Marshall et al., in press), a panic attack was defined as the endorsement of at least three physical symptoms, one cognitive symptom, and the item indicative of “panic sensations,” at a minimum severity rating of 4 (on a 0 to 8 scale). We use the terms panic attacks and fear reactivity, in response to the biological challenge, interchangeably (Sanderson et al., 1989).
Physiologic stimulus and gas delivery
The physiologic stimulus was 10% CO2-enriched air (10% CO2, 21% O2, 69% NO2). Participants were equipped with a continuous positive pressure Downs C-Pap Mask (Model No. 9000; Vital Signs Inc., Totowa, New Jersey). For a comprehensive description of the automated apparatus, see Lejuez, Forsyth, and Eifert (1998). Participants were administered one 4-min CO2 presentation, a dose that pilot testing suggested was sufficient to produce acute anxious arousal and panic symptoms among nonclinical participants.
Procedure
Participants were recruited from the Burlington, Vermont, community for participation in a laboratory study via placement of study flyers throughout various community settings and posting of printed advertisements in local newspapers. Interested participants who contacted the research team about the study were given a detailed description of the investigation via telephone and scheduled for an initial laboratory visit. Upon arrival, participants completed a written informed consent, which explained study protocol and lab procedures involving exposure to 10% CO2-enriched air. Additionally, participants were administered the SCID–N/P (First et al., 1994) by trained interviewers to assess for current Axis I psychopathology. If deemed eligible, participants then completed a battery of self-report measures prior to engaging in the biological challenge procedure.
The laboratory challenge consisted of two phases. The first phase involved a 10-min baseline adaptation period during which participants sat quietly in the testing room breathing regular room air. Phase 2 consisted of the automated delivery of one 4-min 10% CO2-enriched air presentation. Participants completed the DSQ immediately after completing the 4-min challenge exposure. At the completion of the study, participants were debriefed and compensated $20 for their time and effort.
Data Analytic Strategy
Hierarchical multiple regression analyses were conducted to determine the relations between the emotion vulnerability variables and marijuana use motives. Specifically, cigarettes smoked per day, marijuana use frequency (past month), average alcohol use volume over the past year, and negative affectivity (NA) were entered at Level 1 of the regression; the noncriterion marijuana use motives were entered at Level 2 (i.e., all other motives with the exception of the one being used as the dependent variable); and the ASI, DSQ-measured panic attacks during the CO2-enriched air challenge (yes/no), and DTS total were entered at Level 3. Criterion variables were the MMQ subscales of Conformity and Coping motives. This hierarchical model tests the incremental main effects of each set of the variables, independent of the other use motives and covariates, in relation to each of the criterion marijuana use motive indices (Haynes & Lench, 2003).
Results
Descriptive Data and Correlations Among Theoretically Relevant Variables
See Table 1 for descriptive data and zero-order (or bivariate) correlations among studied variables. It should be noted from the outset that Table 1 includes nicotine dependence and alcohol use problems in addition to cigarette smoking rate and volume of alcohol consumed per occasion for comparative purposes. Results of the zero-order correlations indicated that ASI scores were significantly correlated with Conformity (r = .39, p < .001) and Coping motives (r = .41, p < .001). DTS scores were significantly negatively related to Conformity (r = −.24, p < .01) and Coping motives (r = −.33, p < .001). Fear reactivity (PA) was not significantly related to the two MMQ subscales (range of observed rs = .10 to .13).
Table 1.
Zero-Order Correlations Among Theoretically Relevant Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Mean or percentage (SD) |
Observed range |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Cigarettes/daya | 1 | .75** | .00 | .04 | .03 | .27* | .06 | −.08 | −.02 | .02 | . 06 | .28* | .05 | .30** | 8.24 (12.63) | 0–120 |
| 2. | FTND | 1 | −.14 | .20 | −.18 | .11 | .16 | .11 | .24 | −.06 | −.10 | −.01 | −.13 | −.05 | 2.98 (1.85) | 0–6 | |
| 3. | Alcoholb | 1 | .68** | .27* | −.16 | .00 | .09 | −.06 | .15 | .10 | −.01 | .25* | .08 | 2.73 (.91) | 0–4 | ||
| 4. | AUDIT | 1 | .27* | −.07 | .10 | −.02 | −.12 | .15 | .05 | −.09 | .26* | .16*** | 11.85 (5.47) | 0–31 | |||
| 5. | MJ | 1 | .01 | .04 | −.05 | .08 | .51** | .38** | −.04 | .41** | .39** | 4.84 (2.48) | 1–8 | ||||
| 6. | NA | 1 | .40** | −.35** | .16 | −.06 | .06 | .29** | .04 | .33** | 17.27 (4.97) | 10–36 | |||||
| 7. | ASI | 1 | −.46** | .24* | .07 | .17*** | .36** | .15 | .41** | 15.73 (8.07) | 0–44 | ||||||
| 8. | DTS | 1 | −.18*** | .12 | −.03 | −.24* | −.01 | −.33** | 3.65 (.74) | 1.93–5.00 | |||||||
| 9. | PA (% yes) | 1 | −.03 | .07 | .13 | .04 | .10 | 22.9% | |||||||||
| 10. | MMM–Enhancement | 1 | .55** | −.01 | .45** | .37** | 3.76 (.99) | 1–5 | |||||||||
| 11. | MMM–Social | 1 | .30** | .45** | .38** | 2.50 (.97) | 0.2–4.6 | ||||||||||
| 12. | MMM–Conformity | 1 | .14 | .22 | 1.40 (.58) | 0.4–4.0 | |||||||||||
| 13. | MMM–Expansion | 1 | .38** | 2.19 (1.16) | 0–5 | ||||||||||||
| 14. | MMM–Coping | 1 | 2.00 (.95) | 1–5 |
Note. FTND = Fagerstrom Test for Nicotine Dependence (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991); AUDIT = Alcohol Use Disorders Identification Test (Babor, de la Fuente, Saunders, & Grant, 1992); MJ = frequency of marijuana use; NA = Negative Affectivity subscale of the Positive Affect Negative Affect Scale (Watson, Clark, & Tellegen, 1988); ASI = Anxiety Sensitivity Index total (Reiss, Peterson, Gursky, & McNally, 1986); DTS = Distress Tolerance Scale total (J. S. Simons & Gaher, 2005); PA = panic attack during carbon dioxide–enriched air challenge (yes/no); MMM = Marijuana Motives Measure; Enhancement, Social, Conformity, Expansion, and Coping are subscales of the MMM (J. Simons, Correia, Carey, & Borsari, 1998).
Cigarettes/day = average number of cigarettes smoked per day.
Alcohol = frequency of alcohol use (from AUDIT item).
p < .01.
p < .001.
p < .05.
ASI scores were significantly related to both DTS scores (r = −.46, p < .001; 21% shared variance) and PA (r = .24, p < .01; 5% shared variance). DTS scores also were significantly negatively related to PA (r = −.18, p < .01; 3% shared variance). None of the emotional vulnerability factors were significantly related to marijuana use in the past 30 days (see Table 1).
The interrelation between daily cigarette smoking level and marijuana use (current) was minimal (r = .03), whereas alcohol use (volume typically consumed per occasion) was significantly associated with marijuana use in the past 30 days (r = .27). Also, marijuana use (past 30 days) was significantly related to Coping motives (r = .39) but not to Conformity motives (r = −.04; see Table 1). Daily cigarette smoking rate was significantly related to Coping (r = .30) and Conformity (r = .28) marijuana use motives (see Table 1), whereas current alcohol use (volume typically consumed per occasion) was not (see Table 1).
Marijuana Motive Regression Analyses1,2
Overall, the model predicted 45.5% of variance in Coping motives, F(11, 130) = 9.05, p < .001. Step 1 of the model predicted a significant 27.7% of variance, with marijuana use frequency (t = 4.55, β = .36, p < .001), cigarettes per day (t = 2.14,β = .17, p < .05), and negative affectivity (t = 3.13, β = .24, p < .01) being significant, independent effects. Step 2 predicted a significant 9.0% of variance, with Enhancement motives being the only significant, independent effect (t = 2.01,β = .20, p < .05). As was hypothesized, Step 3 accounted for a significant 8.9% of variance, with ASI (t = 2.69, β = .22, p < .01) and DTS (t = −2.3,β = −.19, p < .05) each being significant, independent effects (see Table 2).
Table 2.
Hierarchical Regression Analyses: Coping Motives
| Variable | ΔR2 | t | β | sr2 | p |
|---|---|---|---|---|---|
| Step 1 | .28 | <.001 | |||
| Cigarettes/daya | 2.14 | .17 | .04 | <.05 | |
| Alcoholb | 1.03 | .08 | .01 | ns | |
| MJ | 4.55 | .37 | .14 | <.001 | |
| NA | 3.13 | .24 | .07 | <.01 | |
| Step 2 | .09 | <.01 | |||
| MMM–Enhancement | 2.01 | .20 | .03 | <.05 | |
| MMM–Social | 1.14 | .11 | .01 | ns | |
| MMM–Conformity | 1.19 | .09 | .01 | ns | |
| MMM–Expansion | 1.17 | .10 | .01 | ns | |
| Step 3 | .09 | <.001 | |||
| PA | −.74 | −.05 | .00 | ns | |
| DTS | −2.31 | −.19 | .04 | <.05 | |
| ASI | 2.69 | .22 | .06 | <.01 |
Note. F(11, 130) = 9.05, p < .001. MJ = frequency of marijuana use; NA = Negative Affectivity subscale of the Positive Affect Negative Affect Scale (Watson, Clark, & Tellegen, 1988); MMM = Marijuana Motives Measure (J. Simons, Correia, Carey, & Borsari, 1998); PA = panic attack during carbon dioxide–enriched air challenge (yes/no); DTS = Distress Tolerance Scale total (J. S. Simons & Gaher, 2005); ASI = Anxiety Sensitivity Index total (Reiss, Peterson, Gursky, & McNally, 1986).
Cigarettes/day = average number of cigarettes smoked per day.
Alcohol = frequency of alcohol use.
The model predicted 20.7% of variance in Conformity motives, F(11, 130) = 2.82, p < .01. Step 1 of the model predicted a significant 8.6% of variance, with alcohol volume of use per occasion (t = 2.27, β = .21, p < .05) and negative affectivity (t = 2.10, β = .18, p < .05) being significant, independent effects. Step 2 was not significant; no other marijuana use motive accounted for unique variance in Conformity motives beyond Step 1 covariates. As expected, Step 3 predicted a significant 5.7% of variance, with ASI the only significant, independent effect (t = 2.37, β = .24, p < .05; see Table 3).
Table 3.
Hierarchical Regression Analyses: Conformity Motives
| Variable | ΔR2 | t | β | sr2 | p |
|---|---|---|---|---|---|
| Step 1 | .09 | <.05 | |||
| Cigarettes/day | −1.29 | −.11 | .01 | ns | |
| Alcohol | 2.27 | .21 | .04 | <.05 | |
| MJ | −1.74 | −.16 | .02 | ns | |
| NA | 2.10 | .18 | .03 | <.05 | |
| Step 2 | .06 | ns | |||
| MMM–Enhancement | −1.49 | −.17 | .02 | ns | |
| MMM–Social | 2.28 | .25 | .04 | <.05 | |
| MMM–Expansion | .46 | .05 | .00 | ns | |
| MMM–Coping | 1.19 | .12 | .01 | ns | |
| Step 3 | .06 | <.05 | |||
| PA | .52 | .05 | .00 | ns | |
| DTS | −.55 | −.06 | .00 | ns | |
| ASI | 2.37 | .24 | .04 | <.05 |
Note. F(11, 130) = 2.82, p < .01. MJ = frequency of marijuana use; NA = Negative Affectivity subscale of the Positive Affect Negative Affect Scale (Watson, Clark, & Tellegen, 1988); MMM = Marijuana Motives Measure (J. Simons, Correia, Carey, & Borsari, 1998); PA = panic attack during carbon dioxide–enriched air challenge (yes/no); DTS = Distress Tolerance Scale total (J. S. Simons & Gaher, 2005); ASI = Anxiety Sensitivity Index total (Reiss, Peterson, Gursky, & McNally, 1986).
Cigarettes/day = Average number of cigarettes smoked per day.
Alcohol = frequency of alcohol use.
Discussion
The present study evaluated the role of anxiety sensitivity, distress tolerance, and fear reactivity to somatic perturbation, above and beyond concurrent substance use and negative affectivity, in regard to Coping and Conformity marijuana use motives among a young adult marijuana-using population. Consistent with prediction, anxiety sensitivity was significantly and uniquely related to Coping motives. This effect represented approximately 6% of unique variance and was apparent after controlling for the significant variance accounted for by marijuana use, daily cigarette smoking, and negative affectivity (Level 1) as well as Enhancement motives for marijuana use (Step 2). The anxiety sensitivity effect also was unique from the shared variance with distress tolerance, which also demonstrated, as hypothesized and consistent with past work (J. S. Simons et al., 2005), a significant incremental negative relation with Coping motives for marijuana use (4% of unique variance). In contrast, there was no evidence that fear reactivity to the CO2-enriched air provocation was related to Coping motives for marijuana use. Overall, the size of the observed effects for anxiety sensitivity and distress tolerance were theoretically and practically meaningful (see Table 2; Cohen, 1988). Indeed, 37% of total variance in the regression model was accounted for by the covariates at the first two levels in the hierarchical model. Given the magnitude of variance accounted for at Steps 1 and 2 in the model—in conjunction with the significant relationship between anxiety sensitivity, distress tolerance, and fear reactivity (see Table 1)—it is noteworthy that anxiety sensitivity and distress tolerance enhanced the model’s predictive power (Abelson, 1985). Indeed, this is potentially clinically important and empirically documents the importance of considering both anxiety sensitivity and distress tolerance in efforts to understand coping-oriented marijuana use.
The present study also found that anxiety sensitivity, but not distress tolerance or fear reactivity to bodily sensations, was significantly and incrementally related to Conformity marijuana use motives. This significant effect (4% of unique variance), consistent with past work with adolescents (Comeau et al., 2001) and young adults (Bonn-Miller, Zvolensky et al., 2007), was evident above and beyond the 9% of variance accounted for by the Step 1 effects and the 6% of variance explained by the other covarying marijuana use motives at Step 2. It is possible that marijuana users high in anxiety sensitivity experience elevated fears about the perceived negative effects of publicly observable anxiety symptoms (e.g., sweating) and therefore may be more motivated to use marijuana in public, group-oriented settings to conform with the drug-using actions of other peers. This type of account would be broadly consistent with an anxiety sensitivity-driven social anxiety perspective of conformity-oriented marijuana use (Buckner et al., 2007). Yet, given Conformity-oriented marijuana use motives, as found in past work (Bonn-Miller, Zvolensky et al., 2007), were not related to marijuana use (past 30 days), the ultimate relevance of this relation to actual marijuana use behavior and its treatment deserves further investigation.
The present investigation yields other important and novel insights into the nature of the studied variables among adult marijuana users in a number of other ways. First, there was no significant explanatory effect for fear reactivity for either of the two studied marijuana use motives (see Tables 2 and 3). The lack of the hypothesized fear reactivity effect may be at least partially attributable to shared variance between this variable and anxiety sensitivity and distress tolerance (see subsequent paragraph; see also Table 1). However, it should be noted that relation between fear reactivity and Coping and Conformity motives for marijuana use was minimal (r = .10 and r = .13, respectively). It is difficult to fully explicate this finding. These data may suggest that fear reactivity is not related uniquely to marijuana Coping or Conformity motives per se. It is possible that participants who did not meet the fear reactivity criterion in the present study were nonetheless meaningfully emotionally reactive to the employed panic provocation tactic but were subthreshold for meeting formal panic attack criteria. This latter interpretation may therefore by a by-product of the manner in which we coded for fear reactivity in the current study (i.e., categorically rather than dimensionally). Consistent with this perspective, in follow-up analyses, there were no significant differences between the mean level of Coping (1.3[.63] vs. 1.4[.65]) and Conformity (1.7[.93] vs. 1.9 [1.0]) motives among those who did and did not meet panic attack criteria during the challenge, respectively. Future research in this domain is clearly warranted. For example, research could use an alternative operational definition of fear reactivity than that used in the current study in terms of marijuana use motives. Also, research could usefully examine the relation between fear reactivity and other process variables related to marijuana use behavior (e.g., marijuana withdrawal symptoms and quit success).
Second, anxiety sensitivity was significantly related to both distress tolerance and fear reactivity to bodily sensations (see Table 1); a pattern of findings consistent with past work focused on non-marijuana-using populations (Bernstein et al., in press; Rapee & Medero, 1994). Yet, anxiety sensitivity also was empirically distinguishable from distress tolerance and fear reactivity to bodily sensations, sharing 21% and 5% of variance with these variables, respectively. Likewise, distress tolerance shared only 3% of variance with fear reactivity. Thus, although related to one another, the current findings suggest that these affective vulnerability factors (anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations, respectively) are empirically distinguishable. These findings are consistent with recently forwarded hierarchical conceptualizations of emotional sensitivity and tolerance (Bernstein et al., in press). On the basis of the present findings, in conjunction with those on non-marijuana-using populations (Bernstein et al., in press), it would perhaps be useful to incorporate a hierarchical model of emotional sensitivity and tolerance in future work on marijuana use and its disorders.
Third, it is noteworthy that the interrelation between marijuana use (past 30 days) and cigarette smoking (daily rate) was minimal (r = .03), whereas it was markedly higher for volume of alcohol use typically consumed per occasion (r = .27). Although marijuana use often is related to both daily cigarette smoking and alcohol use and problems (Amos, Wiltshire, Bostock, Haw, & McNeill, 2004), the current findings suggest that this pattern of results may not always be the case. In the current study, participants without Axis I disorders were purposively studied. As has been reported in other work, it is possible that stronger relations between marijuana use and cigarette smoking rate would have been evident if persons with psychopathology were sampled (Zvolensky, Lewinsohn, et al., 2008). At the same time, marijuana use (past 30 days) was significantly related to each of the studied marijuana use motives except Conformity motives (see Table 1). In contrast, daily cigarette smoking was significantly related to only Coping and Conformity marijuana use motives, and current alcohol use was significantly associated only with Expansion motives. At a minimum, these data collectively indicate that not all forms of substance use uniformly relate in the same manner to marijuana use motives. This is an important observation in efforts to advance ecologically valid motivational models of substance use that recognize polysubstance use as well as the unique and shared motivational underpinnings of such co-occurring substance use problems. Given the robust patterns of polysubstance use observed across many drug-using populations (e.g., Amos et al., 2004), it would be useful for future work to more rigorously evaluate these unique and shared motivational underpinnings of co-occurring substance use problems (i.e., cigarette smoking, marijuana, and alcohol) by, for example, evaluating use motives for multiple substances in single-substance and polysubstance users. This type of work points to the clinically promising approach of applying motivational models to better understand the nature of marijuana use and its co-occurrence with other forms of substance use behavior (J. Simons et al., 1998).
Overall, the results of the current study broadly highlight the importance of anxiety sensitivity and distress tolerance in terms of better understanding marijuana use motives. For instance, the present findings, along with others (J. S. Simons et al., 2005), suggest that focusing greater attention on linkages between emotional vulnerability factors such as anxiety sensitivity and distress tolerance in regard to marijuana use motives will be useful in terms of identifying, and perhaps clinically assisting, young adults, and presumably others, at risk for certain types of marijuana use patterns (e.g., coping-oriented marijuana use). These effects were observed after accounting for other theoretically relevant factors common to such a population, including concurrent substance use and tendency to experience negative affect states (negative affectivity). Thus, it is possible that in order to activate change in certain marijuana use domains (e.g., marijuana use aimed at coping or conformity motives), which are associated with marijuana use levels, it may be necessary to understand and clinically address the roles of anxiety sensitivity and distress tolerance. For example, intervention approaches aimed at reducing anxiety sensitivity and increasing distress tolerance may facilitate the ability to alter the use of marijuana for coping-oriented reasons.
The present study has a number of limitations and related future directions that warrant comment. First, the studied participants were not a representative sample of the population as a whole but ratherwere a demographically homogenous, agelimited, self-selected sample from the community. Thus, it may be fruitful to build from the present research and replicate and extend the current results to independent, more diverse populations from distinct developmental age ranges (e.g., adolescents and older adults) and clinical service centers. Second, the present study utilized a cross-sectional design. Although such a methodological strategy was useful for testing the current study hypotheses, it cannot shed light on processes over time or isolate causal relations between variables. Thus, the study results are best construed as a cross-sectional “snapshot” of the relations between emotional sensitivity and tolerance factors and marijuana use motives. Third, although the current study used multimethod assessment tools, it may prove helpful to continue to further expand the measurement approach in future work for certain variables. For example, distress tolerance has been assessed in some work using laboratory methodologies (e.g., Brown et al., 2002; Marshall et al., in press). Inclusion of these assessment tactics would be helpful in further elucidating the relative consistency of the observed self-report findings to other methodologies. Similarly, as an early test in this domain of scientific work, we did not include a range of marijuana outcome variables such as success in quitting or severity of withdrawal symptoms. These types of dependent variables represent exciting avenues for future study.
Fourth, we sampled for nonclinical persons (without Axis I disorders with the exception of substance use disorders). This methodological strategy was designed to rule out possible explanatory confounds between psychopathology and the studied emotional sensitivity and tolerance variables. That is, because each of these emotional vulnerability factors covaries with psychopathology, the inclusion of participants with psychopathology could obfuscate pinpointing the relations between emotional vulnerability factors—specifically, anxiety sensitivity, distress tolerance, and fear reactivity—and marijuana use motives. Although this emphasis on internal validity is a strength of the study, it would also be beneficial to replicate and extend the results to a clinical sample of marijuana users. Fifth, because of the theoretical focus on drug-based motivational processes, the measurement strategy focused on marijuana use motives. However, it is possible that anxiety sensitivity and distress tolerance may play key explanatory roles in other aspects of marijuana use behavior. Thus, it may be useful to extend future work on these vulnerability factors to the nature of quit success, withdrawal symptoms, and self-efficacy for quitting. This type of work would continue to build the empirical knowledge base about emotional vulnerability, broadly defined, and a variety of clinically relevant factors related to marijuana use and its disorders. Finally, extant work on marijuana and its disorders, including motivational processes for use, has largely been atheoretical in nature. In many respects, this characteristic simply reflects the early developmental stage of the work on psychological and emotional vulnerability and co-occurring marijuana use. Although the current study was not informed by an overarching theoretical model, it did evaluate in one model three putative vulnerability factors for certain types of motivation for marijuana use. Using this type of multirisk factor approach, it will be possible to gain clearer insight into the enigmas of the motivational bases of marijuana use and to utilize such knowledge to develop and ultimately test treatment models targeting multiple facets of emotional vulnerability.
Overall, the present study provides novel empirical information concerning anxiety sensitivity, along with distress tolerance and fear reactivity to bodily sensations, in terms of their relation to marijuana use motives among young adult marijuana users. Results indicated that anxiety sensitivity was significantly and uniquely associated with Coping and Conformity motives for marijuana use; effects were evident above and beyond concurrent substance use and other marijuana use motives, as well as distress tolerance and fear reactivity to somatic perturbation. Distress tolerance evidenced significant and unique relations to Coping motives. These results provide novel information related to the role of anxiety sensitivity and distress tolerance as they pertain to motives for marijuana use among young adults.
Footnotes
Analyses were conducted with nicotine dependence and alcohol use problems as covariates instead of cigarette smoking rate per day and average volume of alcohol consumed per occasion. The results did not differ in pattern, and all effects were evident. These supplementary analyses can be obtained by contacting Michael J. Zvolensky.
We used a self-reported index of fear reactivity. It should be noted, however, that supplementary analyses were conducted in an exploratory fashion with an alternative physiological reactivity index (i.e., change in heart rate and skin conductance). This physiological index of somatic reactivity was not significantly related to marijuana use motives. These supplementary analyses can be obtained by contacting Michael J. Zvolensky.
Contributor Information
Michael J. Zvolensky, Department of Psychology, University of Vermont, Burlington
Erin C. Marshall, Department of Psychology, University of Vermont, Burlington
Kirsten Johnson, Department of Psychology, University of Vermont, Burlington.
Julianna Hogan, Department of Psychology, University of Vermont, Burlington.
Amit Bernstein, Department of Psychology, University of Haifa, Mount Carmel, Haifa, Israel.
Marcel O. Bonn-Miller, Center for Health Care Evaluation, Veterans Affairs, Palo Alto Health Care System, Palo Alto, California, and Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Palo Alto, California
References
- Abelson RP. A variance explanation paradox: When a little is a lot. Psychological Bulletin. 1985;97:129–133. [Google Scholar]
- Abrams K, Zvolensky MJ, Dorflinger L, Galatis A, Blank M, Eissenberg T. Fear reactivity to bodily sensations among heavy smokers and non-smokers. Experimental and Clinical Psychopharmacology. 2008;16:230–239. doi: 10.1037/1064-1297.16.3.230. [DOI] [PubMed] [Google Scholar]
- Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. American Journal of Drug and Alcohol Abuse. 2002;28:643–652. doi: 10.1081/ada-120015873. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Amos A, Wiltshire S, Bostock Y, Haw S, McNeill A. You can’t go without a fag…you need it for your hash—A qualitative exploration of smoking, cannabis, and young people. Addiction. 2004;99:77–81. doi: 10.1111/j.1360-0443.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: The alcohol use disorders identification test: Guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- Bloom JW, Kaltenborn WT, Paoletti P, Camilli A, Lebowitz MD. Respiratory effects of non-tobacco cigarettes. British Medical Journal. 1987;12:1516–1518. doi: 10.1136/bmj.295.6612.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Feldner MT, Bernstein A, Zvolensky MJ. Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event–exposed marijuana users. Journal of Traumatic Stress. 2007;20:577–586. doi: 10.1002/jts.20243. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Zvolensky MJ. Emotional dysregulation: Association with coping-oriented marijuana use motives among current marijuana users. Substance Use and Misuse. 2008;43:1656–1668. doi: 10.1080/10826080802241292. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ. The Marijuana Smoking History Questionnaire. Burlington: Anxiety and Health Research Laboratory, University of Vermont; 2005. Unpublished manuscript, (Available from M. J. Zvolensky Author upon request) [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Bernstein A. Marijuana use motives: Concurrent relations to frequency of past 30-day use and anxiety sensitivity among young adult marijuana smokers. Addictive Behaviors. 2007;32:49–62. doi: 10.1016/j.addbeh.2006.03.018. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Leen-Feldner EW, Feldner MT, Yartz AR. Marijuana use among daily tobacco smokers: Relationship to anxiety-related factors. Journal of Psychopathology and Behavioral Assessment. 2005;27:279–289. [Google Scholar]
- Bovasso GB. Cannabis abuse as a risk factor for depressive symptoms. American Journal of Psychiatry. 2001;158:2033–2037. doi: 10.1176/appi.ajp.158.12.2033. [DOI] [PubMed] [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Archives of General Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111:180–185. [PubMed] [Google Scholar]
- Buckner JD, Bonn-Miller MO, Zvolensky MJ, Schmidt NB. Marijuana use motives and social anxiety among marijuana-using young adults. Addictive Behaviors. 2007;32:2238–2252. doi: 10.1016/j.addbeh.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabrol H, Duconge E, Casas C, Roura C, Carey KB. Relations between cannabis use and dependence, motives, for cannabis use and anxious, depressive and borderline symptomatology. Addictive Behaviors. 2005;30:829–840. doi: 10.1016/j.addbeh.2004.08.027. [DOI] [PubMed] [Google Scholar]
- Cocores J. Nicotine dependence: Diagnosis and treatment. Psychiatry Clinics of North America. 1993;16:49–60. [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Comeau N, Stewart SH, Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors. 2001;26:803–825. doi: 10.1016/s0306-4603(01)00238-6. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. Journal of the American Medical Association. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cox WM, Klinger E. A motivational model of alcohol use. Journal of Abnormal Psychology. 1988;97:168–180. doi: 10.1037//0021-843x.97.2.168. [DOI] [PubMed] [Google Scholar]
- Dannon PN, Lowengrub K, Amiaz R, Grunhaus L, Kotler M. Comorbid cannabis use and panic disorder: Short term and long term follow-up study. Human Psychopharmacology. 2004;19:97–101. doi: 10.1002/hup.560. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Schmidt NB, Smith RC. A prospective test of anxiety sensitivity as a moderator of the evaluation between gender and posttraumatic symptom maintenance among high anxiety sensitive young adults. Depression and Anxiety. 2008;22:78–87. doi: 10.1002/da.20281. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV patient edition. New York: Biometrics Research Department; 1994. (SCID-N/P, Version 2.0) [Google Scholar]
- Forsyth JP, Eifert GH, Canna MA. Evoking analogue subtypes of panic attacks in a nonclinical population using carbon dioxide–enriched air. Behaviour Research and Therapy. 2000;38:559–572. doi: 10.1016/s0005-7967(99)00074-1. [DOI] [PubMed] [Google Scholar]
- Grant BF. Comorbidity between DSM–IV drug use disorders and major depression: Results of a national survey of adults. Journal of Substance Abuse. 1995;7:481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- Haynes SN, Lench SC. Incremental validity of new clinical assessment measures. Psychological Assessment. 2003;15:456–466. doi: 10.1037/1040-3590.15.4.456. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Kraemer HC, Taylor CB. Predictors of panic attacks in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:207–214. doi: 10.1097/00004583-200002000-00021. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Ikard FF, Green DE, Horn D. A scale to differentiate between types of smoking as related to the management of affect. International Journal of Addictions. 1969;4:649–659. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future: National results on adolescent drug use. Bethesda, MD: National Institutes of Health; 2005. [Google Scholar]
- Lejuez CW, Forsyth JP, Eifert GH. Devices and methods for administering carbon dioxide–enriched air in experimental and clinical settings. Journal of Behavior Therapy and Experimental Psychiatry. 1998;29:239–248. doi: 10.1016/s0005-7916(98)00018-4. [DOI] [PubMed] [Google Scholar]
- Li W, Zinbarg RE. Anxiety sensitivity and panic attacks: A 1-year longitudinal study. Behavior Modification. 2007;31:145–161. doi: 10.1177/0145445506296969. [DOI] [PubMed] [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders. 1992;6:241–247. [Google Scholar]
- Marshall EC, Zvolensky MJ, Vujanovic AA, Gregor K, Gibson LE, Leyro TM. Panic reactivity to voluntary hyperventilation challenge predicts distress tolerance to bodily sensations among daily cigarette smokers. Experimental and Clinical Psychopharmacology. 2008;16:313–321. doi: 10.1037/a0012752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald J, Schleifer L, Richards JB, de Wit H. Effects of delta9 tetrahydrocannabinol on behavioral measures of impulsivity in humans. Neuropsychopharmacology. 2003;28:1356–1365. doi: 10.1038/sj.npp.1300176. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Mitchell H, Zvolensky MJ, Marshall EC, Bonn-Miller MO, Vujanovic AA. Incremental validity of coping-oriented marijuana use motives in the prediction of affect-based psychological vulnerability. Journal of Psychopathology and Behavioral Assessment. 2007;29:277–288. [Google Scholar]
- Office of Applied Studies (OAS) Summary of findings from the 2003 National Survey on Drug Use & Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2004. [Retrieved September 6, 2008]. (DHHS Publication No. SMA 04–3964, NSDUH Series H-25) from http://www.oas.samhsa.gov/nhsda.htm. [Google Scholar]
- Payne TJ, Smith PO, McCracken LM, McSherry WC, Antony MM. Assessing nicotine dependence: A comparison of the Fagerström Tolerance Questionnaire (FTQ) with the Fagerström Test for Nicotine Dependence (FTND) in a clinical sample. Addictive Behaviors. 1994;19:307–317. doi: 10.1016/0306-4603(94)90032-9. [DOI] [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, et al. A multiple motives approach to tobacco dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) Journal of Consulting and Clinical Psychology. 2004;72:139–154. doi: 10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addictive Behaviors. 1994;19:33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Medoro L. Fear of physical sensations and trait anxiety as mediators of the response to hyperventilation in nonclinical subjects. Journal of Abnormal Psychology. 1994;103:696–699. doi: 10.1037//0021-843x.103.4.693. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky M, McNally RJ. Anxiety, sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Russell MAH, Peto J, Patel UA. The classification of smoking by factorial structure of motives. Journal of the Royal Statistical Society. 1974;137:313–329. [Google Scholar]
- Sanderson WC, Rapee RM, Barlow DH. Panic induction via inhalation of 5.5% CO2 enriched air: A single subject analysis of psychological and physiological effects. Behaviour Research and Therapy. 1988;26:333–335. doi: 10.1016/0005-7967(88)90086-1. [DOI] [PubMed] [Google Scholar]
- Sanderson WC, Rapee RM, Barlow DH. The influence of an illusion of control on panic attacks induced via inhalation of 5.5% carbon dioxide-enriched air. Archives of General Psychiatry. 1989;46:157–162. doi: 10.1001/archpsyc.1989.01810020059010. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the AUDIT: WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Forsyth JP, Santiago HT, Trakowski JH. Classification of panic attack subtypes in patients and normal controls in response to biological challenge: Implications for assessment and treatment. Journal of Anxiety Disorders. 2002;16:625–638. doi: 10.1016/s0887-6185(02)00131-7. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatric Research. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB. A comparison of motives for marijuana and alcohol use among experienced users. Addictive Behaviors. 2000;25:153–160. doi: 10.1016/s0306-4603(98)00104-x. [DOI] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE. Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. Journal of Counseling Psychology. 1998;3:265–273. [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- Simons JS, Gaher RM, Correia CJ, Hansen CL, Christopher MS. An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors. 2005;19:326–334. doi: 10.1037/0893-164X.19.3.326. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Simpson EE. Adult marijuana users seeking treatment. Journal of Consulting and Clinical Psychology. 1993;61:1100–1104. doi: 10.1037//0022-006x.61.6.1100. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Zeitlin SB, Samoluk SB. Examination of a three-dimensional drinking motives questionnaire in a young adult university student sample. Behaviour Research and Therapy. 1996;34:61–71. doi: 10.1016/0005-7967(95)00036-w. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences. 2001;31:157–171. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Services research outcome study. Rockville, MD: Author; 1998. (DHHS Publication No. SMA 98–3177) [Google Scholar]
- Taylor S. Anxiety sensitivity. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley Roth D, et al. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index—3 (ASI-3) Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- [Retrieved June 30, 2007];Vermont Department of Health: Core epidemiologic questions. 2007 from http://www.healthyvermonters.info/
- Watson D. Mood and temperament. New York: Guilford Press; 2000. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scale. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weller RA, Halikas JA. Marijuana use and psychiatric illness: A follow-up study. American Journal of Psychiatry. 1985;142:848–850. doi: 10.1176/ajp.142.7.848. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Marshall EC, Feldner MT. Panic attacks, panic disorder, and agoraphobia: Associations with substance use, abuse, and dependence. Current Psychiatry Reports. 2006;8:279–285. doi: 10.1007/s11920-006-0063-6. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Sachs-Ericsson N, Schmidt NB, Buckner JD, Bonn-Miller MO. Cannabis use, abuse, and dependence and panic attacks in a representative sample. Journal of Psychiatric Research. 2006;40:477–486. doi: 10.1016/j.jpsychires.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bonn-Miller MO, Bernstein A, McLeish AC, Feldner MT, Leen- Feldner EW. Anxiety sensitivity interacts with marijuana use in the prediction of anxiety symptoms and panic-related catastrophic thinking among daily tobacco users. Behaviour Research and Therapy. 2006;44:907–924. doi: 10.1016/j.brat.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Eifert GH. A review of psychological factors/processes affecting anxious responding during voluntary hyperventilation and inhalations of carbon dioxide–enriched air. Clinical Psychology Review. 2000;21:375–400. doi: 10.1016/s0272-7358(99)00053-7. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner E, Bonn-Miller MO, McLeish AC, Gregor K. Evaluating the role of anxiety sensitivity in smoking outcome expectancies among regular smokers. Cognitive Therapy and Research. 2004;28:473–486. [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Diathesis-stress model for panic-related distress: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2005;43:521–532. doi: 10.1016/j.brat.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lejuez CW, Eifert GH. The role of control in anxious responding: An experimental test using repeated administrations of 20% CO2-enriched air. Behavior Therapy. 1998;29:193–209. [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Nonclinical panic attack history and smoking cessation: An initial examination. Addictive Behaviors. 2004;29:825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lewinsohn P, Bernstein A, Schmidt NB, Buckner JD, Seeley J, et al. Prospective associations between cannabis use, abuse, and dependence and panic attacks and disorder. Journal of Psychiatric Research. 2008;42:1017–1023. doi: 10.1016/j.jpsychires.2007.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Bonn-Miller MO, Marshall EC, Leyro T. Marijuana use motives: A confirmatory test and evaluation among young adult marijuana users. Addictive Behaviors, 32,among young adult marijuana users. Addictive Behaviors. 2007;32:3122–3130. doi: 10.1016/j.addbeh.2007.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]