Abstract
In type 2 diabetes, insulin resistance is the main problem that is associated with a cluster of conditions such as obesity and hyperlipidemia. The present study was designed with the objective to evaluate the role of Mehamudgara vati (MMV), which was expected to work at the level of Medodhatwagni due to its Medohara properties, to have an effective control on type 2 diabetes. To fulfill the objective, known patients of type 2 diabetes attending the OPD and IPD of Kayachikitsa Department, IPGT and RA, were selected and were divided in two groups. In Group A, MMV was given 3 tab. thrice a day with lukewarm water for 3 months and in Group B, the patients who were already taking modern antidiabetic treatment, although their blood sugar level was not well under control, were additionally given MMV in the same manner. The formulation has shown a highly significant decrease in the fasting and post-prandial blood sugar level. The formulation has also shown a synergistic action when combined with the modern antidiabetic drugs due to its known hypolipidemic, hypocholesterolemic, hepatoprotective, antihyperglycemic, antistress, antioxidant and immunomodulatory activities.
Keywords: Agni, antihyperglycemic, antihyperlipidemic, dosha, dushya, stress, type 2 diabetes
Introduction
The syndrome of diabetes mellitus (DM) is largely covered under the broad heading of Prameha. However, Apathyanimittaja Prameha (Sushruta), Sthula Pramehi (Charaka) and Avaranjanya Madhumeha described in the Ayurvedic literature have similarity with type-2 non-insulin-dependent diabetes mellitus (NIDDM).
DM is a chronic disease marked by elevated blood glucose levels. It affects 5-6% of the global adult population. Its prevalence is rising at alarming rates worldwide because of increased urbanization, high prevalence of obesity, sedentary lifestyle and stress, among other factors. The summary published by the “World Diabetes Congress” on 14th Nov., 2009, “World Diabetes Day,” represents that diabetes affects 246 million people worldwide and is expected to affect some 380 million by 2025. More than 90% of all diabetes patients are of type 2 diabetes. Gujarat is the epicenter of India, accounting for close to 10 million cases alone. In Gujarat, a high dependence of milk products and oily foods coupled with genetic factors are responsible for this dubirious distribution.
The approach in treating diabetes has been to reduce the sugar intake i.e. excluding carbohydrate intake; but the real problem is the fat deposition in the cells leading to stoppage of insulin from doing its work. Insulin resistance, a primary defect in pathogenesis of type 2 diabetes, is the condition whereby the effectiveness of insulin in transporting glucose into cells is diminished. Insulin resistance is closely associated with cluster of conditions such as obesity, hypertension and hyperlipidaemia which is collectively known as Syndrome ‘X’ or Metabolic syndrome. Fat cells are more insulin resistant than muscle cells; therefore, one important cause of insulin resistance is obesity.
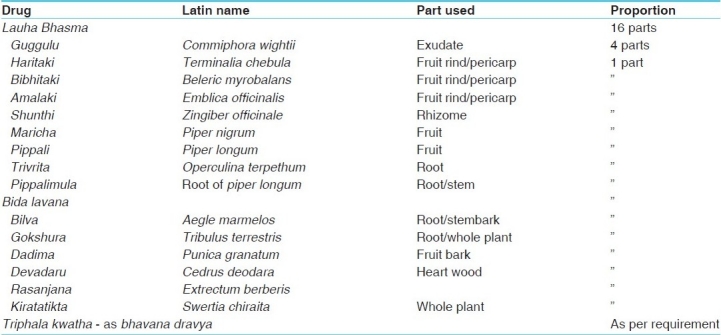
Though Prameha is Tridoshaja vyadhi, Acharyas have mainly emphasized on vitiation of Kapha dosha and medodhatwagnimandya. Meda has been described to be the anchor seat (important dooshya) of this disease. So the goal to prevent or control this disease cannot be achieved without modifying the diet and lifestyle. Further, for disintegrating the Samprapti, a formulation, which not only has antihyperglycemic/hypoglycemic effect, but also would work at the level of Dhatwagni to counteract Kapha Dosha and Medodhatu for correcting the fat and carbohydrate metabolism and insulin resistance is needed. The Mehamudgara vati (MMV) – a herbo mineral formulation comprises herbs [Table 1] with properties which can be helpful to break the etiopathogenesis of this disease.
Table 1.
Ingredients of Mehamudgara vati
Aims and objectives
To assess the antihyperglycemic, antihyperlipidemic and insulin-releasing effect of “Mehamudgaravati” on Medodushti in the patients of type 2 diabetes.
To assess the synergistic effect of MMV when added with modern antihyperglycemic drugs.
Materials and Methods
A total of 94 patients of type 2 diabetes, attending the out patient/in patient department of Institute for Post Graduate Teaching and Research in Ayurveda Hospital, Gujarat Ayurved University, Jamnagar, were selected irrespective of their sex, caste etc. and divided into two groups taking into consideration the inclusion and exclusion criteria.
Inclusion criteria
Patients of type 2 diabetes fulfilling the standard diagnostic criteria of the World Health Organization (WHO) for DM: Symptoms of DM plus random blood glucose >200 mg/dl or fasting blood glucose >126 mg/dl or 2-h blood glucose >200 mg/dl during an oral glucose tolerance test.
Exclusion criteria
Patients of Sahaja Prameha (type I diabetes), patients of Madhumeha suffering from bala and dhatukshaya (IDDM), complicated with any major heart disease like Congestive Cardiac Failure (CCF), any renal impairment like nephropathy, patients suffering from tuberculosis, carcinoma and human immunodeficiency virus-positive patients were also excluded from the present study. Patients suffering from endocrinal disorders like, thyrotoxicosis, Cushing syndrome etc. were also excluded.
Laboratory investigation
Blood for Hb%, total leucocyte count, deferential leucocyte count, erythrocyte sedimentation rate, urine for routine and microscopic examination and biochemical investigations (fasting blood sugar, post-prandial blood sugar, blood urea, serum creatinine, lipid profile and serum insulin [in selected patients]) was performed.
Ethical approval
The research protocol was approved by the “Institutional Ethics Committee,” I.P.G.T. and R.A., Jamnagar.
Treatment protocol
-
Group A: Mehamudgara vati group:
Mild to moderate cases of type 2 diabetes were administered MMV along with pathyapalana.
-
Group B: Integrative group:
Known patients of type 2 diabetes already taking modern antidiabetic drug but with diabetes not well under control were administered MMV additionally along with pathyapalana.
Drug, dose and duration
Drug:- Mehamudgara Vati[1]
Dose:- 3 tab. thrice a day (each tab. of 250 mg: After breakfast, lunch and dinner).
Anupana:- Luke warm water.
Duration:- 3 months.
Patients of both the groups were advised to follow the Pathyapathya as follows:
Pathya: Yava (barley), green gram, bengal gram, Samo (Panicum frumentaceum)
Fruits: Orange, sweet lemon, pomegranate
Vegetables: Cabbage, cucumber, radish, bitter gourd, drum sticks, bottle guard, ridge gourd, parval, kankoda, methi (fenugreek leaves)
Dal: Chana dal, moong dal, tuvar dal (adhaki)
Apathya: Milk and milk products like curd, butter, cheese, ghee etc., oily fried food, sweets, dried fruits, chocolates, bakery products, fermented items, potatoes, sugar, ice cream, fast foods etc. Patients were also advised to avoid sleeping during the day.
Exercise: Thirty minutes brisk walking in fresh air in the morning and evening.
First of all, Triphala kwath was made and then Guggulu and Rasanjana were melted in it. All the herbal ingredients were mixed properly with Lauha bhasma. After proper mixing of all the ingredients, they were given lavigation of Triphala kwatha in an end runner and granules were made from the lavigated material. After drying of the granules, these were made to a tablet form.
Criteria for assessment of the overall effect of therapy
The overall effect was assessed on the basis of relief in chief and associated complaints, improvement on “Brief Psychiatry Rating Scale,” relief in Medovaha Srotodushti lakshana, decrease in Fasting Blood Sugar (FBS) and Post Prandial Blood Sugar (PPBS) decrease in urine sugar and decrease in serum cholesterol and serum triglyceride and increase in the serum high-density lipoprotein (HDL) level.
The overall effect of therapy was assessed on the basis of following criteria
Complete remission: 100%
Marked improvement: >75% to <100% improvement
Moderately improved: >50% to <75% improvement
Improved: >25 to <50% improvement
Unchanged: <25% improvement
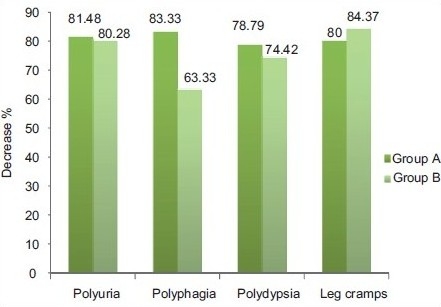
Statistical analysis
The Wilcoxon signed rank method[2] was used to check the significance of the subjective criteria and Paired “t” test[3] was used for objective criteria in a single group and to compare the effect of therapy of the two groups. Chi square (χ2)-test[4] was carried out for subjective criteria and unpaired “t” test[5] for objective criteria. The obtained results were interpreted as follows:
Follow-up
Patients were advised to visit the hospital every week during the treatment and for 1 month after the treatment as follow-up.
Observations and Results
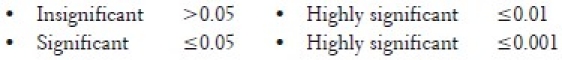
In Group A, a total 46 patients were registered, among which 34 patients had completed the treatment whereas 12 were dropped out. In Group B, a total 48 patients were registered, among which 35 had completed the treatment whereas 13 were dropped out. The data of general observation of the occurrence of chief complaints, associated complaints and the most prevalent factors in brief psychiatry rating scale is shown in Table 2.
Table 2.
Chief complaints, associated complaints and brief psychiatry rating scale wise distribution (n = 94)
In Group A, maximum patients (58.82%) had chronicity of ≤1 year whereas in Group B, maximum patients (40%) had chronicity of 5-10 years. A total of 70.21% among the 22.34% patients in Group A and 47.87% patients in Group B were obese (body mass index [BMI] > 25).
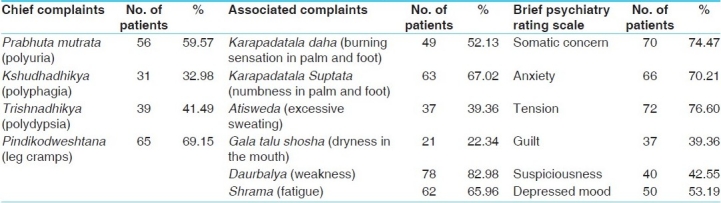
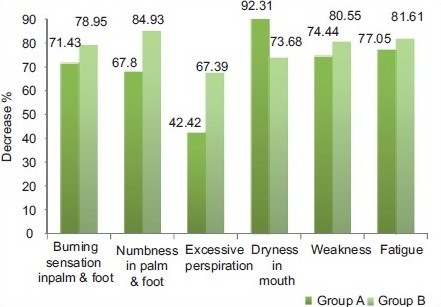
Both the groups have shown a highly significant relief in most of the chief complaints, associated complaints and brief psychiatry rating scale [Graphs 1–3]. On suspiciousness and on Gala talu shosha, both the groups have shown significant relief. On comparison by Chi square test, both the groups were equally effective in reliving all the chief complaints, associated complaints and brief psychiatry rating scale. The effect of MMV on srotodushti is shown in Graph 4.
Graph 1.
Effect on chief complaints
Graph 3.
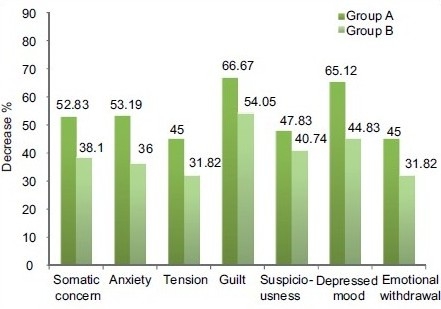
Effect on brief psychiatry rating scale
Graph 4.

Effect on Srotodushti
Graph 2.
Effect on associated complaints
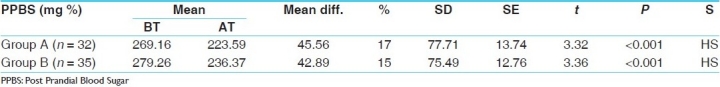
Both Group A and Group B have shown a highly significant (P < 0.001) decrease in FBS by 9.24% and 15%, respectively [Table 3], and in PPBS by 17% and 15%, respectively [Table 4]. On comparison with the test of significance, both Chi square and unpaired “t” tests showed insignificant results, indicating that both the groups are equally effective in decreasing the blood sugar level.
Table 3.
Effect on FBS
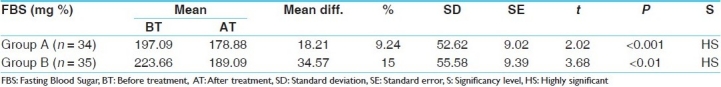
Table 4.
Effect on PPBS
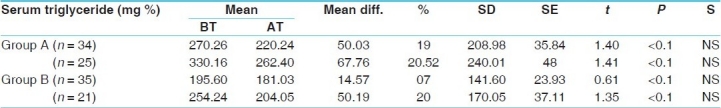
MMV has shown a highly significant decrease in the serum cholesterol level by 10%, serum triglyceride level by 19% and serum HDL level by 7%. However, when these patients were split depending upon serum cholesterol >200 mg%, serum triglyceride >150 mg% and serum HDL <40 mg%, the results were better. The percentage decrease was highly significant by 15.13% and 20.52% in the serum cholesterol and serum triglyceride levels, respectively, and 5.08% increase in the serum HDL level. The integrative group has shown a 3% decrease in the serum cholesterol level, 7% decrease in serum triglyceride and 3% increase in serum HDL. However, when these patients were split depending upon serum cholesterol >200 mg%, serum triglyceride >150 mg% and serum HDL <40 mg%, the results were better. The percentage decrease was 9% and 20% in the serum cholesterol and serum triglyceride levels, respectively, and 14% increase in serum HDL [Tables 5–7]. On comparison with the test of significance, by the unpaired “t” test, Group A was significantly (P < 0.05) better than Group B.
Table 5.
Effect on serum cholesterol
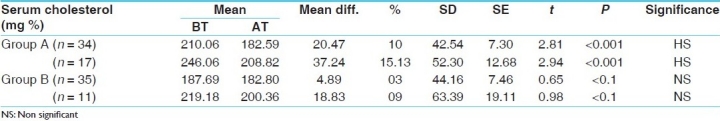
Table 7.
Effect on serum high density lipoprotein
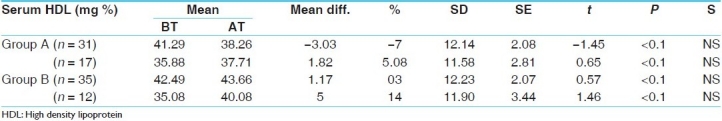
Table 6.
Effect on serum triglyceride
The effect of MMV on Urine sugar, Fasting serum Insulin and post prandial serum insulin is shown in the Tables 8–10 respectively.
Table 8.
Effect on urine sugar
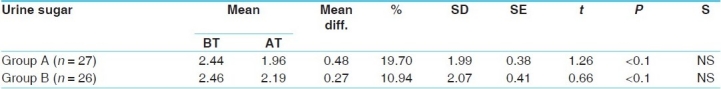
Table 10.
Effect on serum insulin (post-prandial – 2 h)
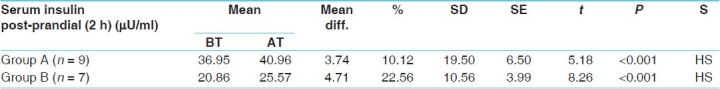
Table 9.
Effect on serum insulin (fasting)
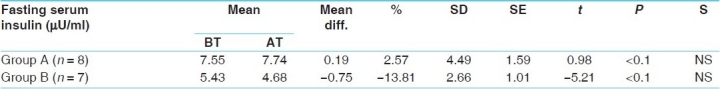
After 3 months of administration of MMV, the fasting serum insulin level was increased in 68.75% of the patients. Among them, the serum insulin level was increased with the effect of decreased fasting blood sugar level in 31.25% of the patients and in 37.50% of the patients, although the serum insulin level was increased, FBS was not decreased (rather, it was increased) and in 31.25% of the patients, although the serum insulin level was decreased, FBS was also decreased. The post-prandial serum insulin level was however increased in 62.50% of the patients. Among them, the serum insulin level was increased with the effect of decreased post-prandial blood sugar level in 31.25% of the patients and in 18.75% of the patients, although the serum insulin level was increased, PPBS was not decreased (rather, it was increased) and in 37.5% of the patients, although the serum insulin level was decreased, PPBS was also decreased [Figure 1]. The effect of therapy on body mas index is shown in Graph 5 and the overall effect of therapy is shown in Graph 6.
Figure 1.
Effect of therapy on serum insulin
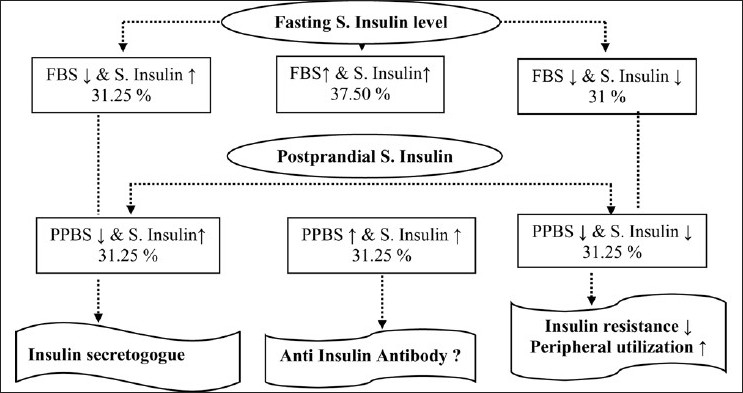
Graph 5.
Effect on body mass index
Graph 6.
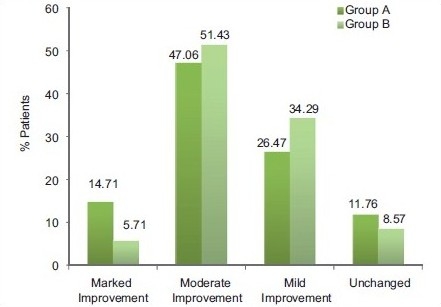
Overall effect of therapy
Follow-up
It is not ethical to follow-up patients of diabetes without giving any drug. Therefore, after completing the course of the trial drug, all the patients were shifted to routine OPD Ayurvedic antidiabetic treatment. And, it was observed that none of the patients aggravated their symptoms or blood sugar level. Although Lauha bhasma was present in a higher proportion in the formulation, even during the follow-up period, none of the patients reported increased serum creatinine and blood urea levels.
Discussion
Prabhuta mutrata (Polyuria) – the main symptoms of Prameha are caused by an excess of vitiated Kleda, which gets converted into mutra. From the modern point of view, due to a lack of the action of insulin, glucose is not utilized, causing a high blood glucose level. When it crosses the renal threshold (180 mg/ dl), blood glucose starts to excrete through the urine. Thus, in diabetic patients, increased frequency of urine is seen commonly. MMV is dominant in Tikta (bitter) – Kashaya (astringent) rasa and Ruksha (dry) guna among which Tikta (bitter) rasa is said to be “kleda upashoshana” while Kashaya (astringent) rasa to be “sharira kledasya upayokta.”[6] The word Ruksha itself indicates dryness, which in turn means lack or decrease of Kleda. Thus, all the three dominant properties show a Kleda-reducing effect. Bahu drava Shleshma is the dosha vishesha and Kleda is one of the dushya vishesha in Samprapti of Prameha; thus, the dominating three properties directly affect both the dosha and the dushya vishesha and hence effectively counteract the Samprapti.
Because of sedentary lifestyle and excessive intake of foods, which increases Kapha, the end product of digestion becomes abnormally sweet, which in turn causes an increase of medas (fat). This obstructs the nutrient channel of the remaining tissue, depriving them of nutrition. Therefore, only fat accumulates in large quantities in the body, making the person incapable of all activities. The channels of Vata become obstructed by the increased fat inside the abdomen; Vata then begins to act fast inside the abdomen, increasing the digestive capacity, making for voracious hunger and craving for large quantity of food,[7] which is presented as Kshudhadhikya (polyphagia). Kshudhadhikya (polyphagia) occurs due to tikshna and ushna guna of Pitta. In the pathophysiology of NIDDM, due to lack of insulin utilization, glucose consumption in muscle tissues is reduced, which is an essential requirement for energy. When muscle tissue does not get glucose and it demands for glucose, this is represented as polyphagia in patients. Due to Dipana and Pachana properties of the drugs present in MMV, like Triphala, Trikatu, Dadima,[8] Bidalavana, Kiratatikta[9] etc., it might have improved the digestive process by correcting Dhatvagnimandya, resulting in prevention of further medo vriddhi and by Vatashamaka property of Guggulu,[10] Haritaki[11] etc. it alleviates the Vata dosha responsible for atiagnisandhukshana. If Kshudhadhikya has occurred due to tikshna and ushna guna of Pitta, MMV may act by pacifying it with the help of its Sheeta veerya.
Trishnadhikya (polydypsia) and Gala talu shosha (dryness in mouth) occur due to Pitta vriddhi and udaka kshaya, which may be pacified by Tikta (astringent), Madhura (sweet) and Kashaya (astringent) rasa of the MMV that affects the condition by correcting Pitta dosha or due to the trishna nigrahana effect of Kiratatikta,[9] Dadima[8] and Devadaru.[12] Polyuria is commonly found in diabetics. Through polyuria, a lot of body fluid is excreted. Therefore, to compensate for this loss, the body demands for liquid, and this is called polydypsia. Because MMV significantly reduces polyuria, it in turn mechanically also reduces polydypsia. In same manner, it also shows an effect on Gala talu shosha (dryness in mouth).
Karapadatala Daha and Karapadatala Suptata (burning sensation and numbness in the palm and foot) are both common neurological complications of diabetes described in the Ayurvedic literature as Purvarupa of Prameha. They reflect one′s glycemic control. Therefore, when hyperglycemia is corrected with hypoglycemic activity of Amalaki,[13] Shunthi,[14] Pippali,[15] Kiratatikta,[9] Devadaru,[12] Dadima,[8] Rasanjana,[16] Bilva[17] etc. ingredients of MMV, relief was obtained in these neuropathic complications like Karapadatala daha and Karapadatala Suptata (burning sensation and numbness in palm and foot). Amalaki,[13] Haritaki,[11] Shunthi,[14] Maricha[18] and Guggulu[10] are said to be Nadibalya, and are thus beneficial in neurological symptoms.
Karapadatala Daha (burning sensation in palm and foot) is due to Pitta by provocation of Ushna quality or may be due to loss of Udaka, which might have been pacified by Sheeta quality of MMV. Karapadatala suptata (numbness in palm and foot) is due to Vata – decrease in Chala guna of Vyana vayu that might have been compensated by Sara guna of MMV.
Daurbalya (weakness), Pindikodweshtana (leg cramps) and Shrama (fatigue) conditions were found in many of diabetic patients because of less glucose uptake by muscle tissue for energy due to an insulin antagonist effect.[19] In the etiopathogenesis of Prameha, the Dhatus get vitiated and vitiated apyamsha of dhatus get converted into Sharira kleda and is excreted through urine.[20] As a result, Dhatukshaya takes place with manifestation of Daurbalya, Shrama and Pindikodveshtana. Therefore, significant results were obtained by the Rasayana effect of Triphala[21] and shunthi. But, this samprapti can be true in IDDM patients, whereas in NIDDM patients, obesity (Sthaulya) may be the cause for manifestation of these symptoms as, due to Medodhatvagnimandya, only fat accumulates in large quantities in the body making the person incapable of all activities. MMV, through its tikta-kashaya (bitter – astringent) rasa and ruksha (dry) guna does shoshana of the abaddha medas and through the Dipana and Pachana properties present in its ingredients like Triphala, Trikatu, Dadima,[8] Bidalavana, Devadaru[12] etc. may have corrected digestive process resulting in correction of medodhtvagni and reducing the baddha meda. The ingredients like Lauha bhasma,[22] Guggulu, Maricha, Devadaru etc. present in MMV have Medohara properties, which may help in reducing excessive meda and, thereby, relieving these complaints.
Atisweda (excessive sweating) is the symptom that arises due to medo mala vriddhi. The MMV due to its ruksha (dry) guna, Kashaya (astringent) rasa, Tikta (bitter) rasa has medohara property due to which it decreases meda and, ultimately, its mala, i.e. sweda. These properties directly, also, contribute to the adsorption of sweda.
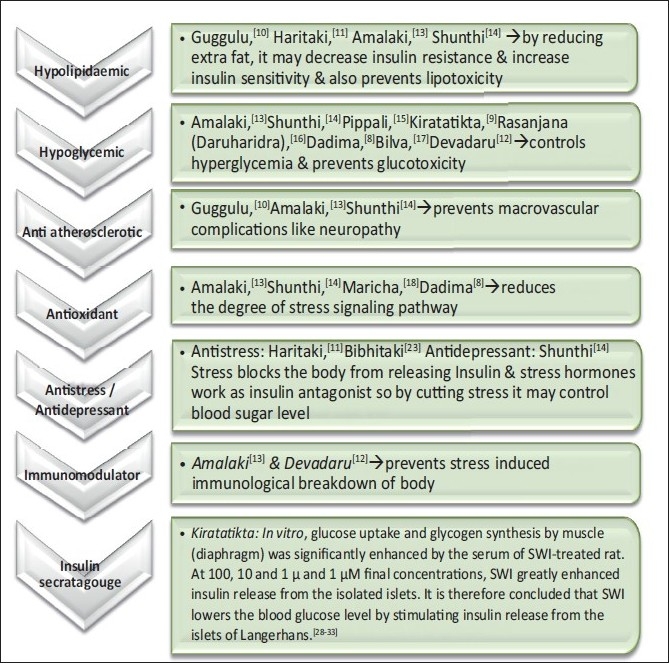
Stress blocks the body from releasing insulin in people with type 2 diabetes; therefore, cutting stress is very essential for effective control of the blood sugar level. The ingredients present in the formulation MMV have different properties that may be helpful in minimizing the stress response or cutting stress. As Haritaki and Bibhitaki[23] are antistress agents and Shunthi is an antidepressant, they might have been cutting the stress directly. Rasayana effect of Lauha bhasma,[22] Haritaki,[11] Amalaki[13] and Pippali,[15] antioxidant properties of Amalaki,[13] Shunthi,[14] Maricha[18] and Dadima[8] and immunomodulatory properties of Amalaki[13] and Devadaru[12] might have helped in minimizing the stress response, and in the manner controlling the disease.
High blood sugar is the main characteristic and diagnostic feature of diabetes. The MMV decreased this elevated blood glucose level, which may be by its ingredients such as Amalaki,[13] Shunthi,[14] Pippali,[15] Kiratatikta,[9] Daruharidra (Rasanjana),[16] Dadima,[8] Bilva[17] and Devadaru,[12] which are proven hypoglycemic agents, whereas Lauha bhasma,[22] Guggulu,[10] Amalaki,[13] Devadaru,[12] Gokshura[24] and Haritaki[11] have Pramehahara properties. Oral administration of the extracts of Triphala significantly reduced the blood sugar level in normal and in alloxan diabetic rats. It may decrease the effect of inflammatory cytokine release in diabetics, which in turn might reduce the insulin resistance. Interestingly, the authors note that traditional medications used to treat diabetes also have significant antioxidant effects.[25]
When glucose and FFA increase, they cause oxidative stress-sensitive signaling pathways. Activation of these pathways, in turn, worsens both insulin action and secretion, leading to overt type 2 diabetes.[26] Furthermore, insulin-resistant patients, with and without type 2 diabetes, are at an increased risk for developing metabolic syndrome, a major cause of heart disease, hypertension and dyslipidemia.[27] Thus, treatment aimed at reducing the degree of oxidative stress signaling pathways might appear to warrant consideration for inclusion as part of the treatment program for patients with type 2 diabetes. Some of the drugs like Amalaki,[13] Shunthi,[14] Maricha[18] and Dadima[8] present in MMV are proven antioxidants and Lauha bhasma,[22] Haritaki,[11] Amalaki[13] and Pippali,[15] due to their Rasayana properties, might have reduced the degree of oxidative stress signaling pathways and, by that, preventing insulin resistance and Beta cell dysfunction and, ultimately, controlling the blood sugar level.
The contents of MMV – Lauha bhasma,[22] Guggulu,[10] Maricha[18] and Devadaru,[12] have Medohara effect, and Guggulu,[10] Haritaki,[11] Amalaki[13] and Shunthi[14] have a proven hypolipidemic effect due to which they may have decreased the high lipid level and BMI [Graph 5].
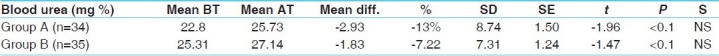
Group A has shown 3.15% decrease in S. creatinine whereas Group B has decreased S. creatinine significantly by 5.33%. Blood Urea was decreased in Group A by 2.93% whereas it was increased by 1.83%. [Tables 11–12]. Even during the follow-up period, they have not gone beyond the normal limit. The patients having abnormally high serum creatinine and blood urea levels were excluded from the study. Thus, decrease and increase in the physiological value of serum creatinine has no value, but not going beyond the normal limit after administration of MMV for 3 months, it certainly gives the safety profile of the drug as Lauha bhasma is the main ingredient of this formulation.
Table 11.
Effect on serum creatinine
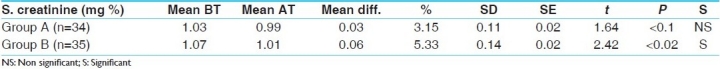
Table 12.
Effect on blood urea
When the blood sugar level crosses the renal threshold, i.e. 180 mg/dl, then it starts its excretion through the urine to decrease the load of blood sugar. Although by MMV, the blood sugar level was found to have decreased, it could not come within the normal limit in all the patients; thus, urine sugar also was not found to be nil in all the patients. Therefore, on examination, urine sugar is found to be present in these patients also after the treatment.
An increased level of serum insulin gives the indication toward an insulin-secretagaug effect of the ingredients of the trial formulation – MMV. An increased level of serum insulin with a decreased blood sugar level gives the idea that the drug has worked through its insulin-secretagauge effect. Where the blood sugar level is decreased and serum insulin is also decreased, it shows that MMV might have decreased insulin resistance and increased peripheral utilization or increased insulin sensitivity. Where the blood sugar level is increased although the serum insulin level is also increased, the role of anti-insulin antibody can be thought of in the etiopathogenesis of the disease, which is not counteracted by this formulation.
Probable mode of action of Mehamudgara vati
Probable Rasapanchaka of MMV according to cumulative properties
Rasa: Tikta (bitter) (29.41%), Madhura (sweet) (27.06%), Kashaya (astringent) (24.7%)
Guna: Ruksha (dry) (22.05%), Guru (20.47%) (heavy), Sara (14.17%), Sheeta (cold) (12.60%)
Veerya: Sheeta (cold) (51.52%)
Vipaka: Katu (pungent) (76.47%)
Doshaghnata: Kaphapittashamaka (51.43%)
The active principle of MMV can also be divided into two parts: Acting part and defensive part.
Acting part: Rasa: Tikta (bitter), Kashaya (astringent); Guna: Ruksha.
Defending part: Rasa: Madhura (sweet); Guna: Guru (heavy); Veerya: Sheeta (cold) (Otherwise, the acting part can lead to Dhatukshaya, Vata prakopaka, Vatanubandha, Upadrava etc.).
Role of the defending part
Madhura (sweet) rasa
MMV contains the highest amount of Lauha bhasma, which has Madhura rasa. Here, the purpose of using Lauha bhasma in such a great proportion is getting the Lekhana effect. That is why it can be thought that Lauha bhasma will do Lekhana and thus reduce Meda and Shleshma more effectively by its Lekhana karma rather than by increasing them by Madhura rasa. Madhura rasa prevents Dhatukshaya and Vata Prakopa. Moreover, it may show a shamana effect on Pitta and Vata in Pittanubandhaja and Vatanubandhaja Kaphaja Prameha, respectively.
Guru (heavy) guna
It can be deduced that Guru guna acts as Aviruddha vishesha and thus prevents dhatu kshaya and vata vriddhi. As MMV is dominant in Ruksha and Sheeta guna, if it would be laghu, it would certainly increase vata and cause dhatukshaya, which will further progress to Prameha.
Sheeta (cold) veerya
As Dosha vishesha in pathogenesis of this disease is Bahu drava shleshma and Dushya vishesha is bahu and abaddha meda, including other dushyas involved, i.e., Ap pradhana. If more heat energy would be provided, then, by liquefaction of dosha, it will cause more Prakopa of the already present drava shleshma. Therefore, to prevent this doshic calamity, the drugs having sheeta veerya may be combined as a remedy for Prameha.
Role of the acting part
Tikta (bitter) rasa:
Kashaya (Astringent) rasa:
It seems that both Tikta and Kashaya (bitter and astringent) rasa play both acting and defending roles. By the virtue of Ruksha (dry) property, they especially do Kleda shoshana and Kledopayoga, which is one of the prime dushya in pathogenesis of Prameha. Whereas by Sheeta (cold) property, they prevents liquefaction of the already drava shleshma, abaddha meda and other Ap pradhana dushyas involved in the pathogenesis hence also participating in a defending phenomenon.
Ruksha (dry) guna:
In Samprapti of Prameha, Bahu drava shleshma is important among the dosha and Abaddha meda among the dushyas. Other dushyas involved are either Bahu or Bahu and Abaddha, indicating excessive Ap dhatu in the body and main line of treatment for excessive fluid is their shoshana, which is done by Ruksha (dry) guna. Thus, directly or indirectly, Ruksha guna plays a very important role in Samprapti vighatana starting from the very initial stage, i.e. first kriyakala of Sanchaya.
The mode of action of the ingredients of MMV on the basis of pharmacological activity is shown in Figure 2.
Figure 2.
Mode of action of MMV in type 2 diabetes on the basis of pharmacological activity
Conclusion
Group A and Group B have shown almost the same effect. Of course, Group B shows the synergistic action when MMV is combined with modern antidiabetic drugs. Most of the ingredients of MMV have known hypolipidemic, hypocholesterolemic, hepatoprotective, antihyperglycemic, antistress, antioxidant and immunomodulatory activities. The data also reveals the insulin-releasing effect of MMV, as it was increased in 68% of the patients in a fasting state whereas in the post-prandial state, it was increased in 49% of the patients, which can be taken as an indicator of the drug having complex activities like both insulin secretagaug and peripheral utilization.
Healthy dietetics and healthy lifestyle with the use of Ayurvedic antidiabetic drugs singularly or in combination with modern drugs, depending upon the need, will contribute significantly to achieve the goal of improvement in the quality of life in patients of diabetes.
References
- 1.Das Sen Kaviraja Govind. edited with Siddhiprada Hindi Commentry by Prof. Siddhinandan Mishra. 64 – 68. Vol. 37. Siddhinandan Mishra, Varanasi: Chaukhambha Sanskrit Sansthan; 2007. Bhaishajya Ratnavali; p. 703. [Google Scholar]
- 2.Laurence D.R, Bacharach A.L, editors. Chap. 3- Design, Statistical analysis and interpretation, by Rumke and H. De. Jonge. Vol. 1. London & New York: Academic Press; 1964. Evaluation of Drug Activities: Pharmacometrics; pp. 70–73. [Google Scholar]
- 3.Mahajan BK. Methods in Biostatistics for medical students and research workers. 6th ed. New Delhi: J P Brothers medical publishers limited; 2006. pp. 147–50. [Google Scholar]
- 4.Ibid, Mahajan BK, Methods in Biostatistics for medical students and research workers. pp. 168–85.
- 5.Ibid, Mahajan BK, Methods in Biostatistics for medical students and research workers. pp. 142–47.
- 6.Acharya Vaidya Yadavji Trikamji., editor. Agnivesha, Charaka samhita, Sutra sthana. Vol. 26. Varanasi: Chaukhambha Surbharati Prakashan; 2008. p. 43. [Google Scholar]
- 7.Madhavakar, Madhava Nidanam, Shrikantha Murthy K. R. Chap. 34, Medo roga Nidanam/1-6. 5 ed. Varanasi: ChaukhambhaOrientalia; 2003. p. 121. [Google Scholar]
- 8.Database on Medicinal plants used in Ayurveda. Vol. 2. New Delhi: Central Council of Research in Ayurveda & Siddha; 2001. Anonymous; p. 177. [Google Scholar]
- 9.Ibid, Database on Medicinal plants used in Ayurveda. 7:226. [Google Scholar]
- 10.Ibid, Database on Medicinal plants used in Ayurveda. 2:223. [Google Scholar]
- 11.Ibid, Database on Medicinal plants used in Ayurveda. 3:282. [Google Scholar]
- 12.Ibid, Database on Medicinal plants used in Ayurveda. 7:72. [Google Scholar]
- 13.Ibid, Database on Medicinal plants used in Ayurveda. 3:11. [Google Scholar]
- 14.Ibid, Database on Medicinal plants used in Ayurveda. 5:315. [Google Scholar]
- 15.Ibid, Database on Medicinal plants used in Ayurveda. 3:472. [Google Scholar]
- 16.Ibid, Database on Medicinal plants used in Ayurveda. 1:120. [Google Scholar]
- 17.Ibid, Database on Medicinal plants used in Ayurveda. 1:79. [Google Scholar]
- 18.Ibid, Database on Medicinal plants used in Ayurveda. 5:187. [Google Scholar]
- 19.Kasper Dennis L, Fauci Anthony S, Longo Dan L, Braunwald Eugene, Hauser Stephen L, Jameson J. Larry., editors. Harrison′s principles of internal medicine. 16th ed. New Delhi: Mcgraw-Hill Medical Publishing Division; p. 2158. [Google Scholar]
- 20.Acharya Vaidya Jadavaji Trikamji., editor. Nidanasthana. 37. Vol. 4. Varanasi: Chaukhambha Surbharati Prakashana; 2000. Agnivesha, Charaka Samhita; p. 215. [Google Scholar]
- 21.Ibid, Charak Samhita, Chikitsasthana. (1-3/64-65, P: 386 and 1-3/30-31, p:385).1-3(6):385. [Google Scholar]
- 22.Acharya Vagbhat. ‘Vijnanabodhini’ Hindi translation & commentary, by Prof. Dattatreya Anant Kulkarni. 5/84. Vol. 1. New Delhi: Meharchand Lachhamandas Publications; 2007. Rasaratna Samuchchyaya; p. 108. [Google Scholar]
- 23.Ibid, Database on Medicinal plants used in Ayurveda. 3:158. [Google Scholar]
- 24.Ibid, Database on Medicinal plants used in Ayurveda. 3:229. [Google Scholar]
- 25. [Last accessed on 2010 7 Feb]. Available from: www.squidoo.com/Triphala_Benefits .
- 26.Evans JL, Goldfine ID, Maddux BA, Grdsky GM. Are oxidative stress – activated signaling pathways mediators of insulin resistance and β – cell dysfunction? Diabetes. 2003;52:1–8. doi: 10.2337/diabetes.52.1.1. [DOI] [PubMed] [Google Scholar]
- 27.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with conventional treatment and risk of complications in patients with Type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 28.Bajpai MB, Asthana RK, Sharma NK, Chatterjee SK, Mukherjee SK. Hypoglycemic effect of Swerchirin from the Hexane fraction of Swertia Chirayita. Planta Med. 1997;57:102–4. doi: 10.1055/s-2006-960041. [DOI] [PubMed] [Google Scholar]
- 29.Mukherjee B, Mukherjee SK, et al. Blood sugar lowering activity of Swertia Chirayita (Buch – Ham) extract. Int J Crude Drugs Res. 1987;25:97–102. [Google Scholar]
- 30.Sekar BC, Mukherjee B, Chakravarti RB, Mukherjee SK. Effect of different fractions of Swertia Chirayita on blood sugar level of Albino Rats. J Ethnopharmaco. 1987;l21:175–81. doi: 10.1016/0378-8741(87)90127-9. [DOI] [PubMed] [Google Scholar]
- 31.Chandrasekar B, Bajpai MB, Mukherjee SK. Hypoglycemic activity of Swertia Chirayita (Roxb exflem) Karst. Indian J Exp Biol. 1990;28:616–8. [PubMed] [Google Scholar]
- 32.Saxena AM, Bajpai MB, Mukherjee SK. Swerchirin induced blood sugar lowering of streptozotocin treated hyperglycemic rats. Indian J Exp Biol. 1991;29:674–5. [PubMed] [Google Scholar]
- 33.Saxena AM, Bajpai MB, Murthy PS, Mukherjee SK. Mechanism of blood sugar lowering by a swerchirin containing hexane fraction (SWI) of Swertia Chirayita. Indian J Exp Biol. 1993;31:178–81. [PubMed] [Google Scholar]


