Abstract
Amavata (Rheumatoid Arthritis) has been a challenging problem to the medical field. Various treatment protocols are applied in this disease with partial success. In present clinical study, 12 patients of clinically proven Amavata (Rheumatoid Arthritis) were treated with Panchamuladi Kaala Basti to evaluate its efficacy. All clinical Ayurvediya nidanadi parameters and American Rheumatism Association guidelines for Rheumatoid Arthritis were followed. Before treatment and after treatment, analysis was done and results were calculated statistically using paired ‘t’ test. Results obtained are encouraging and indicate the efficacy of Panchamuladi Kaala Basti over Amavata (Rheumatoid arthritis), exploring many aspects of this clinical entity.
Keywords: Amavata, Panchamuladi Kaala Basti, Rheumatoid Arthritis
Introduction
In Ayurveda, it is explained that Samprapti (pathogenesis) of almost all the diseases begins with the Agnimandya[1] which leads to formation of Ama. This Ama is the utmost important causative factor for various diseases. On other hand, Vata Dosha is most powerful among three Doshas and it controls the other two Doshas[2] as well as it is very difficult for treatment. Therefore, when these two factors (Ama and Vata) simulteniously take part in the Samprapti (pathogenesis), then the resultant disease becomes very difficult to treat.
Amavata is one of the most challenging diseases caused by Ama combining with vitiated Vata Dosha. The disease Amavata belongs to Abhyantara as well as Madhyama roga marga. The Samprapti (pathogenesis) starts in the Annavaha Srotasa and then extends through Madhyama roga marga with special inclination for Kapha Sthanas[3] especially Sandhis (joints). In such a condition, patient weeps in agony of pain and reduced functional capacity with severe stiffness and cripling deformity of joints, which make them bed ridden.
Having several features similar to Rheumatoid arthritis, Amavata is generally compared with this disease. Rheumatoid arthritis is an autoimmune polyarthritis of unknown etiology with symmetrical joint involvement and effects many other systems too. There is no definite cure for the disease.
In Ayurveda, many approaches are in practice to treat Amavata but still remain a challenging problem. Many research works have been done on this disease, but still there is a need of an effective, safe, and less-complicated treatment. In present study, Basti Chikitsa was selected for clinical trials as Basti is the major treatment in Ayurveda which directly acts over the Vata Dosha and many a times is called as Ardha Chikitsa or Sarva Chikitsa.[4] Also, Basti, especially Kshara Basti, is main treatment for Amavata.
Aims and objectives
To evaluate the efficacy of Panchamuladi Kaala Basti in Amavata (Rheumatoid Arthritis).
Materials and Methods
Selection of the patients
Patients in between 16 to 60 years of age, of both genders, religion, etc., having classical signs and symptoms of Amavata were selected randomly from the OPD and IPD of Govt. Akhandanand Ayurveda Hospital, Ahmedabad. A total of 12 patients were taken for study, all of them completed the course. However, patients who were suffering from systemic disorders like cardiac disease, Diabetes Mellitus, Hypertension, cancer, Tuberculosis, respiratory diseases, etc., and having chronicity of more than 5 years were excluded.
The patients were mainly diagnosed on classical signs and symptoms of Amavata and American Rheumatism Association (ARA) criteria. An elaborate proforma was filled containing clinical history as well as complete general and physical examination of the patients.
Investigations
Relevant investigations were conducted in every patient, which included routine investigations for blood along with special investigations for Rheumatoid factor, Hemoglobin%, and Erythrocyte sedimentation rate.
Drugs
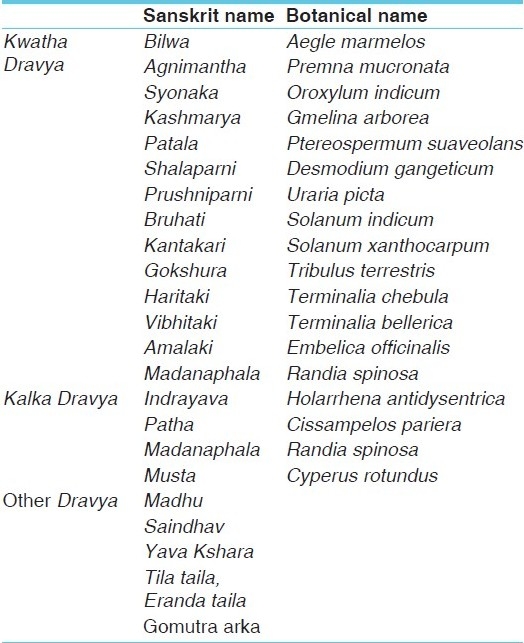
Following table shows ingredients of Panchamuladi Kaala Basti [Table 1].
Table 1.
Ingredients of Panchamuladi Kaala Basti
Method of preperation
Asthapana Basti
Each Asthapana Basti was prepared with classical method which is as follows.
First of all, the kwatha is prepared as per classical method and kept ready.The Saindhava (rock salt) and Yava kshara are taken in a mortar to which honey is added. Both are mixed well by triturating. When it is properly mixed, the Tila taila (oil) is added and levigating is further continued. To this mixture, Kalka Dravya is then added and is mixed well. When these ingredients are emulsified properly by levigating, the kashaya Dravya is added and at last Gomutra is added, levigating is continued till they get properly mixed.
Anuvasana Basti
Panchamuladi taila was prepared using drugs of Panchamuladi Basti as per classical method of Taila preparation. For Taila preparation, Eranda taila was used in place of Tila taila.
Dose
Asthapana Basti: Each Basti was administered in a dose of 480 ml.
Anuvasana Basti: The 80 ml of Panchamuladi Taila was administered in each Basti.
Management and duration
Total duration of treatment was 21 days which included Langhan for 3 days, deepan-pachan for 3 days and kaala basti for 15 days.
All the 12 patients taken for the study were kept on langhana (fasting) for first 3 days. During this period, they were advised to consume Mudgayusha only. Complete fasting was avoided as it may aggrevate the Vata Dosha. However, Deepana pachana was done from day 4 to day 6 with Trikatu churna 10 g in 3 divided doses every day along with Ushnodaka (luke warm water) as Anupana and patients were advised to consume Mudga dal and rice during this period. After that, Kaala Basti was performed from 7th day onward for 15 days. Patients were kept on normal hospital diet during this period. The sequence of Kaala Basti was as per Astanga Hrudaya, that is, a total of 15 Bastis with Anuvasana Basti 10 and Asthapana Basti 5 were administered. The Anuvasana Basti and Asthapana Basti were administered in sequence of 2 Anuvasana Basti in the beginning and then 5 Asthapana Basti and 5 Anuvasana Basti on alternate days, and 3 Anuvasana Basti in the end.
Method of administration of Basti
The procedure of administration of Basti was divided into 3 stages.
Purva karma: The patients were advised to consume little quantity of light diet before every Anuvasana Basti, while every Asthapana Basti was administered in empty stomach.
Before administering every Basti, local Abhyanga with lukewarm Tila taila was done on abdomen, thighs, and buttocks for 5 to 10 minutes and after Abhyanga, the Nadi Swedana was done on abdomen, thighs, and buttocks for 5 to 10 minutes.
On the day of every Asthapana Basti, Basti was prepared by mixing all the ingredients in their sequence and kept ready.
Pradhana Karma
The patient was advised to lie down on left lateral position on Basti (enema) table with right lower extrimity flexed on knee and hip joint and left lower extremity straight. The patient was asked to keep his left hand below the head. Oil was applied on anus with cotton dipped in oil.
Anuvasana Basti
The 80 ml of lukewarm Panchamuladi taila was filled in enema syringe. Rubber catheter oleated with oil was attached to enema syringe and air was removed. Rubber catheter was introduced into anus of patient up to length of 4 inches. The taila was pushed inside leaving little quantity within syringe in order to avoid entrance of vayu.
Asthapana Basti
The 480 ml of lukewarm Basti dravya was filled in enema can. Rubber catheter oleated with oil was attached to enema can and air was removed. Rubber catheter was introduced into anus of patient up to length of 4 inches. The Basti dravya was allowed to move inside leaving little quantity within enema can in order to avoid entrance of vayu.
While introduction of catheter and drug, the patient was asked to take deep breath and not to shake his body.
Pashchat karma
After administration of Basti, the patient was advised to lie in supine position with hand and legs freely spread over the table. Thereafter, patient's both legs were raised for few minutes so as to raise the waist and gently tapped over the hips. Patient was advised to void the urge of stool whenever he feels so. Basti Pratyagamana Kaala was noted after every Basti.
Follow-up: All the patients were followed up for 1 month after completion of Basti Chikitsa.
Pathyapathya
All the patients were strictly advised to follow the Pathya as mentioned in the context of Amavata in Ayurveda classics.
Criteria for assessment: The results of therapy were assessed on the basis of clinical signs and symptoms mentioned in Ayurveda classics. Functional capacity of patients was also assessed and laboratory investigations were repeated at the end of the treatment schedule. All the signs and symptoms were given scoring pattern depending upon severity as below.
Cardinal symptoms
-
Sandhi ruja (joint pain)
-
(1)No pain - 0
-
(2)Mild pain of bearable nature comes occasionally - 1
-
(3)Moderate pain but no difficulty in joint movements and requires some upashaya measures for relief - 2
-
(4)Slight difficulty in joint movement due to pain and requires some medication and remains throughout the day - 3
-
(5)More difficulty in the joint movements and pain is severe, disturbing sleep and requires strong Analgesic - 4
-
(1)
-
Sandhi shotha (joint swelling)
-
(1)No swelling - 0
-
(2)Mild swelling - 1
-
(3)Moderate swelling and present in more than 2 affected joints - 2
-
(4)Excessive swelling over the all affected joints - 3
-
(1)
-
Stabdhata (stiffness)
-
(1)No stiffness or stiffness lasting for 10 to 20 minutes - 0
-
(2)Stiffness lasting for 20 minutes to 2 hours - 1
-
(3)Stiffness lasting for 2 to 5 hours - 2
-
(4)Stiffness lasting for 5 to 8 hours - 3
-
(5)Stiffness lasting for more than 8 hours - 4
-
(1)
-
Ushnata (heat over the affected joints)
-
(1)Raised temperature when compared with normal body surface - 02
-
(2)Fall in local warmth - 01
-
(3)Normal temperature - 00
-
(4)No change after the treatment - 02
-
(1)
-
Sparshasahyata (tenderness about the joints)
-
(1)No tenderness - 0
-
(2)Subjective experience of tenderness - 1
-
(3)Wincing of face on pressure - 2
-
(4)Wincing of face with withdrawal of affected part on pressure - 3
-
(5)Resist touching - 4
-
(1)
General symptoms
-
(1)
Symptoms observed before treatment - 2
-
(2)
Some relief after treatment - 1
-
(3)
Complete relief after treatment - 0
-
(4)
No improvement after treatment - -2
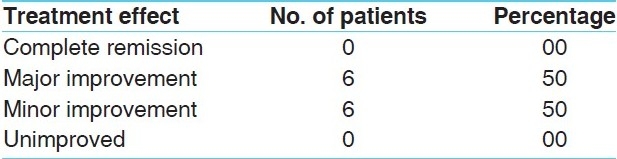
Overall assessment of the therapy
To assess the overall effect of the therapy, the criteria laid down by ARA were adopted. Results are classified into four groups as listed below:
-
(1)
Complete remission
-
(2)
Major improvement
-
(3)
Minor improvement
-
(4)
Unimproved
Statistical analysis
Mean, percentage, SD, SE, ‘t,’ and P value were calculated. Paired ‘t’ test was used for calculating ‘t’ value.
Observations
Maximum numbers of patients (41.66%) were in the age group of 41 to 50 years. Maximum numbers of patients (83.33%) were female, were house wives (50%), and belonged to lower middle class (41.66%). Maximum numbers of patients were of Vata-Pitta Prakriti (75%), had Rajasa-Tamasa Prakriti (58.33%). All the patients (100%) had Avara Vyayama shakti, Abhyavaharana shakti, and Jarana shakti. Maximum numbers of patients had Mandagni (83.33%) and Krura Koshtha (75%). Fifty percent of patients were RA positive, (50%) had chronicity below 1 year, (58.33%) had gradual onset, and (33.33%) got the disease in 4th decade.
Maximum numbers of patients (58.33%) had Vata Kapha Doshanubandha, were indulging in Virudhaahara, Abhishyandi ahara, and Snigdhaahara (91.66%), were consuming Guru and Madhura Ahara (83.33%), were indulging in Vishmashana and Adhyashana (58.33%), and were indulging in Bhojanottara Vyayama and Divaswapna (58.33%).
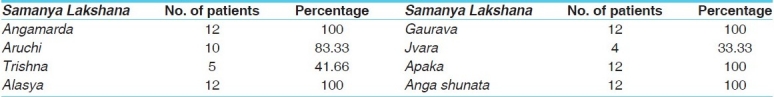
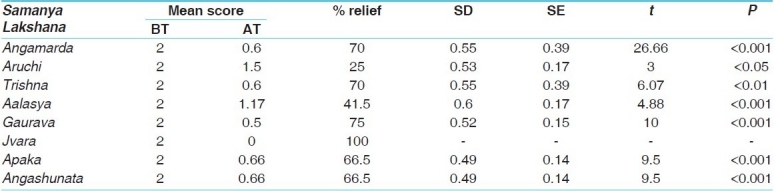
All (100%) patients gave the history of Sandhi Ruja (joint pain), Sandhi Shotha (joint swelling), Sandhi Stabdhata (Joint stiffness), and 83.33% of patients gave history of Ushnata (heat over joint) and Sparsha asahatva (tenderness) [Table 2]. All (100%) patients showed the features Angamarda, Alasya, Gaurava, Apaka, and Anga shunata. Aruchi in 83.33% of patients, Trishna in 41.66% of patients, and Jvara in 33.33% of patients were seen [Table 3]. Proximal interphalangeal and metacarpo phalangeal joints, joints were affected in all (100%) of patients taken for study, knee joints in 83.33%, wrist and ankle joints in 75% of patients, shoulder joints in 66.66% of patients, metatarso phalangeal joints in 25% of patients, and elbow joints in 16.66% of patients were affected.
Table 2.
Distribution of 12 patients of Amavata as per cardinal symptoms
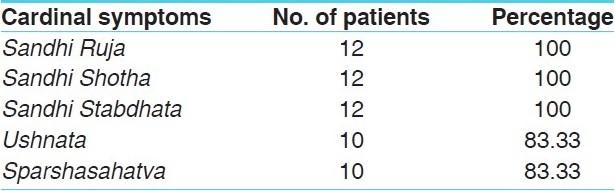
Table 3.
Distribution of 12 patients of Amavata as per Samanya Lakshana
Results
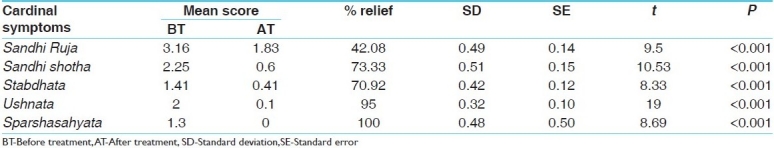
Highly significant results (P < 0.001) were obtained in all the cardinal symptoms Sandhi Ruja (42.08%), Shotha (73.3%), Stabdhata (70.09%), Ushnata (95%), Sparshasahyata (100%) [Table 4].
Table 4.
Effect of Panchamuladi Kaala Basti on cardinal symptoms
Among general symptoms, highly significant results (P < 0.001) were obtained in Gaurava (75%), Angamarda (70%), Apaka and Angashunata (66.5%), and Alasya (41.5%). Significant results (P < 0.01) in Trishna (70%), improvement (P < 0.05) in Aruchi (25%), and 100% results were observed in Jvara [Table 5].
Table 5.
Effect of Panchamuladi Kaala Basti on associated symptoms
Fifty percent of patients showed minor improvement and equal percentage of patients showed major improvement. None of the patients showed complete remission and no one remained unimproved [Table 6].
Table 6.
Overall effect of Panchamuladi Kaala Basti
Discussion
As per age-wise distribution, maximum numbers of patients (41.66%) in this study were in the age group of 41 to 50 years. This is the age wherein Hani (deterioration) of Dhatus starts.[5] This leads to reduced Vyadhikshamatva (immunity) during this age. Increased responsibility towards parents, children, and work lead to faulty dietary habits and increased stress during this age. All these factors contribute towards increased incidence of Amavata during this age.
In this study, maximum numbers of patients (83.33%) were females and among them, 50% were house wives. The female and male ratio was 5 : 1. Increased responsibility towards house works and day-to-day family stress may induce Vata prakopa and Agnimandya and thus results in Amavata in females. As per modern medical science, the female: male ratio in Rheumatoid arthritis is 3 : 1 and below 45 years of age the ratio is 6 : 1.[6]
Data show that 50% of patients had chronicity below 1 year, whereas 25% of patients were between 1 and 3 years, and remaining 25% of patients were between 3 and 5 years. These data signify that people are getting aware regarding importance of Ayurveda Chikitsa in this disease, so that they approached early to Ayurveda Hospital.
The present study revealed that 91.66% of patients were consuming Virudhaahara, Abhishyandi ahara, and Snigdhaahara, while 58.33% of patients were indulged in Bhojnottara Vyayama and 33.33% of patients were indulged in Divaswapna and Nishchalatva. All these Nidanas are specific to Amavata.
In all (100%) of patients, the joints were symmetrically involved. PIP and MCP joints were affected in all patients followed by knee joints in 83.33% and wrist and ankle joints in 75% of patients. Arthritis of hand joints (PIP, MCP) and symmetrical joint involvement are among the diagnostic criteria of rheumatoid arthritis laid down by ARA.
All (100%) of the patients gave the history of Sandhi Ruja, Sandhi Shotha, Sandhi Stabdhata and 83.33% of the patients gave history of Ushnata and Sparshasahatva. Sandhi Ruja and Stabdhata are mainly due to Vata dosha, whereas Shotha, Sparshasahatva, and Ushnata suggest presence of Ama. Above data prove role of Ama and Vata as chief pathological factors in Amavata.
Highly significant results (P < 0.001) in all the cardinal symptoms—Sandhi ruja (42.08%), Shotha (73.3%), Stabdhata(70.09%), Ushnata (95%), Sparshasahyata (100%)prove that Panchamuladi Basti is effective in Amavata. Shula and Stabdhata are mainly due to Vata Dosha and above data prove that Panchamuladi Basti controls Vata Dosha and relieves these symptoms. Shotha, Sparshasahyata, and Ushnata suggest presence of Ama. Above data proves that Kshara property of Panchamuladi Basti help in Ama pachana, and thus relieves these symptoms.
Probable mode of action of Basti
Panchamuladi Basti in general: Basti chikitsa is the prime treatment modality of Ayurveda. Basti in general and Kshara Basti in specific are told as best Chikitsa in Amavata.[7] Panchamuladi Basti administered through Pakvashaya spreads all over the body (head to foot) with its Virya[8] and digests Ama with its Kshara property and at the same time expels the vitiated Vata by targeting it in its pradhan sthana, that is, Pakvashaya.[9] The control gained over Ama and Vata leads to Samprapti vighatana of Amavata.
Drugs of Panchamuladi Basti: Drugs of Dashmula mainly control Vata Dosha along with Kapha Dosha and also aid in Ama pachana.[10] Yava kshara and Gomutra along with other drugs like Musta and Indrayava mainly perform Ama pachana action. Eranda taila in Panchamuladi taila also aid in breaking the Samprapti[11] by controlling Vata Dosha.
Fifty percent of the patients showed major improvement and equal percentage of patients showed minor improvement. Amavata is a Kricchrasadhya Vyadhi and also the duration of treatment was shorter. This could be the probable reason that none of the patients showed complete remission.
Conclusion
Panchamuladi Kaala Basti is proved to be an effective therapy in Amavata. By combating Vata Dosha and Ama (the chief pathological factors), it lead to Samprapti vighatana of Amavata and hence, highly significant results were achieved in all the cardinal symptoms. Fifty percent of patients showed major improvement and 50% showed minor improvement. Due to limitation of number of cases and duration of the trial, there is a need to conduct further study in this regard on larger sample and for a longer duration to improve this preliminary study.
References
- 1.Shastri Pandit Hari Sadashiva., editor. Nidana Sthana. 1. Vol. 12. Varanasi: Chaukhambha Prakashan; 2007. Vagbhata, Ashtanga Hrudaya; p. 513. [Google Scholar]
- 2.Tripathi Brahmanand., editor. Purva Khanda. Reprint ed. 43. Vol. 5. Varanasi: Chaukhambha Surbharti; 2008. Pandit Sarangdhara, Sarangdhara Samhita; p. 60. with Deepika hindi commentary. [Google Scholar]
- 3.Upadhyaya Yadunandana., Pro, editor. Reprint ed. 2. Vol. 25. Varanasi: Chaukhambha Prakashana; 2009. Acharya Madhavakara; p. 508. Madhava Nidana with Madhukosha commentary and Vidyotini Hindi Tika by Shri Sudarshana Shashtri revised. [Google Scholar]
- 4.Acharya Jadavaji Trikamaji., editor. Siddhi Sthana. 40. Vol. 1. Varanasi: Chaukhambha Prakashan; 2008. Agnivesha, Charaka Samhita; p. 683. [Google Scholar]
- 5.Acharya Jadavaji Trikamaji., editor. Sutra Sthana. Reprint ed. 29. Vol. 35. Varanasi: Chaukhambha Prakashan; 2009. Acharya Sushruta, Sushruta Samhita; p. 155. [Google Scholar]
- 6.Davidson . Davidson principle and practice of medicine. In: John A, editor. A. hunter. 19th ed. Philadelphia: Churchill living stone; p. 1002. [Google Scholar]
- 7.Dwivedi R, editor. Reprint ed. Vol. 25. Varanasi: Chaukhambha Sanskrita Sansthana; 2005. Shri Chakrapanidutta, Chakradatta with Vidyotini Hindi commentary, by Indradeva Tripathi; p. 166. [Google Scholar]
- 8.Acharya Jadavaji Trikamaji., editor. Siddhi Sthana. 64. Vol. 7. Varanasi: Chaukhambha Prakashan; 2008. Agnivesha, Charaka Samhita; p. 712. [Google Scholar]
- 9.Acharya Jadavaji Trikamaji., editor. Sutra Sthana. 13. Vol. 20. Varanasi: Chaukhambha Prakashan; 2008. Agnivesha, Charaka Samhita; p. 114. [Google Scholar]
- 10.Acharya Jadavaji Trikamaji., editor. Sutra Sthana. 71. Vol. 38. Varanasi: Chaukhambha Prakashan; 2008. Acharya Sushruta, Sushruta Samhita; p. 169. [Google Scholar]
- 11.Tripathi I. Varanasi: Choukhambha Krishnadas Academy; 2007. Yogaratnakara with vaidyaprabha hindi commentary. Amavata Chikitsa Verse no. 65; p. 457. [Google Scholar]


