Abstract
Objective
To profile and compare the health and health services characteristics for children with special health care needs (CSHCN) with and without disabilities, and to determine factors associated with unmet need.
Methods
Secondary data analysis of the 2005-06 National Survey of Children with Special Health Care Needs was conducted. The socio-demographics, health, and health services of CSHCN with and without disabilities were compared. Multivariable logistic regression was employed to examine factors associated with unmet need for health services.
Results
Children from minority racial and ethnic groups and children living in or near poverty were overrepresented among CSHCN with disabilities compared to other CSHCN. Statistically higher percentages of CSHCN with disabilities had behavioral problems (39.6% vs. 25.2%), anxiety/depressed mood (46.1% vs. 24.0%) and trouble making/keeping friends (38.1% vs. 15.6%) compared to other CSHCN. 32% of CSHCN with disabilities received care in a medical home compared to 51% of other CSHCN. CSHCN with disabilities had higher rates of need and unmet need than other CSHCN for specialty care, therapy services, mental health services, home health, assistive devices, medical supplies and durable medical equipment. The adjusted odds of unmet need for CSHCN with disabilities were 71% higher than for other CSHCN.
Conclusion
CSHCN with disabilities had more severe health conditions and more health services need, but they less commonly received care within a medical home and had more unmet need. These health care inequities should be amenable to policy and health service delivery interventions to improve outcomes for CSHCN with disabilities.
What’s New
CSHCN with disabilities are identified as a distinct group of CSHCN because of their sociodemographic, health and health services characteristics. CSHCN with disabilities had more psychosocial problems and health service needs than other CSHCN. We also document inequities in health services by highlighting the rates of unmet need and low percentages of care within a medical home for CSHCN with disabilities.
Keywords: Children with Special Health Care Needs, Disabilities, Medical Home, Unmet Need
INTRODUCTION
Children with special health care needs (CSHCN) are those children with chronic physical, developmental, emotional or behavioral conditions who need or use health and related services of a type or amount beyond that typically required by children.1 A child can qualify as having special health care needs if he/she had a chronic condition that has lasted or is expect to last at least one year and is associated with at least one of five consequences: needing or using prescription medication; needing or using more medical care, mental health or educational services than is usual for most children of the same age; being limited or prevented in any way in his/her ability to do the things most children of the same age can do; needing or receiving special therapy; and/or needing or receiving treatment or counseling for any emotional, developmental or behavioral problem.2 Over 20% of CSHCN qualify because they are limited or prevented in their abilities to do things that most children of the same age can do,3 and thus are considered to be disabled based on the International Classification of Functioning (ICF) framework for understanding disability.4
CSHCN with disabilities are a special and vulnerable subset of CSHCN because the consequences of having a disabling health condition can be profound.5 Children with disabilities are reported to have extensive health care needs, high rates of health services utilization and costs, and poorer access to needed health services.6-8 Furthermore, the consequences related to disability in childhood extend beyond experiences with the health care system and can include difficulties with school and participation in life events.3,9 These consequences can have long-term impacts on health outcomes, life opportunities and participation in adulthood.10 Because of the negative impacts of disability, it is important for pediatric health providers to understand the population of children with disabilities to provide optimal health care and advocate for the services and assistance they need to be successful in life.
Since the operationalization of the definition of the Children with Special Health Care Needs (CSHCN) over a decade ago, fewer health services research studies specifically focus on children with disabilities and only a handful of recent studies have focused on the subgroup of CSHCN with disabilities.8,9,11-13 Instead, most studies have focused on the general population of CSHCN and have identified issues around access, health insurance, quality of medical care, financial impacts on families, and health disparities.12,14-17 Few studies have looked at services specifically related to children with disabilities/functional limitations, such as durable medical equipment and assistive aids, although some studies identify the presence of functional limitations as a risk factor for unmet need and difficulty with health care access.8,9,18,19 Therefore, a gap in the health services literature exists for CSHCN with disabilities. The purpose of this project is to fill the gap in the literature by profiling and comparing CSCHN with disabilities to other CSHCN to identify sociodemographic, health, and health services differences and to determine factors associated with unmet need. We hypothesize that CSHCN with disabilities have more severe and less stable health conditions than other CSHCN and have more extensive health services needs, but have higher rates of unmet needs and less commonly receive care within a medical home than other CSCHN. We further hypothesize that after controlling for health condition severity and sociodemographic characteristics often associated with health care inequities, that CSHCN with disabilities have increased odds of unmet service need.
METHODS
Dataset
The National Survey of Children with Special Health Care Needs, 2005-06 (NS-CSHCN) is a nationally representative sample of CSHCN that was conducted by National Center for Health Statistics (NCHS), the Maternal and Child Health Bureau (MCHB) and the Centers for Disease Control and Prevention (CDC) between April 2005 and February 2007.20 The NS-CSHCN offers a special opportunity to evaluate CSHCN with disabilities because it is the most extensive and up- to-date version of these periodic surveys of CSHCN.21 The State and Local Area Integrated Telephone Survey mechanism was used to randomly identify 4 million household phone numbers. A computer assisted telephone interview system was used to screen households for eligible children and to administer the CSHCN survey. From the 192,083 households with children, 364,481 children were screened for having special health care needs via the CSHCN Screener and 42,332 (11.6%) qualified. If a household had more than one identified child with special health care needs, one child was randomly chosen to be included in the sample.22 For these children, full interviews were conducted with the adult in the household most familiar with the child’s special health care needs (usually the mother), with a completion rate of 96.2%.22
Conceptualizing Disability and Health Services
To frame our research we used two conceptual models. The first model, the International Classification of Functioning, Disability and Health (ICF) provided a framework for classifying CSHCN as having disabilities or not. Individuals who are limited in their ability to do what people are typically able to do can be considered to have disabilities at one or more of the following levels: bodily impairments, activity limitations or participation restrictions.23 This robust framework is well-aligned with the CSHCN Screener, which identifies CSHCN who are considered by their caregiver to be limited in their ability to do the things that most children of the same age can do because of a medical, behavioral, emotional or developmental condition that has lasted or is expected to last at least one year.2 Based on these Screener questions, we dichotomized CSHCN into those with disabilities and those without. We note that the ICF framework for disability relates health conditions to functioning but does not require the identification of a specific etiology nor does it require a minimum amount of time for the condition to be present.23 Because disability among CSHCN is more narrowly defined than in the ICF framework, the NS-CSHCN population estimates may subsequently be lower than other reports.
The second model, the behavioral model of health services use, framed our analyses of health utilization and unmet need. This model frames health service use and access to health services based on predisposing characteristics and enabling resources.24 Individuals with the need for health services may have those needs met through realized access or might have unmet needs and experience health care inequities.25 For example, the presence of a mobility limitation might predispose an individual to need durable medical equipment (DME) and their insurance might act as an enabling factor. There are certainly other factors that hinder or enable access. Therefore, we used this model to guide us in determining which factors should be included in our multivariable logistic regression analysis of presence of unmet need. Using these two frameworks -the ICF and the behavioral model of health services use, we examined factors that relate to the experience of disability in childhood.
Socio-Demographic, Health and Psychosocial Characteristics
The socio-demographic variables of interest for this study include gender, age, race/ethnicity, income, insurance status, household composition, and highest educational attainment in the household. Age was categorized into the following groups: 0-4 years old (pre-school aged), 5- 13 years old (school aged) and 14-17 years old (high school aged). Race/ethnicity was categorized into four groups: White Non-Hispanic, Black Non-Hispanic, Hispanic, and Other. Income was divided into 3 categories by using the Federal Poverty Level (FPL) criteria: less than 200% FPL, 200-399% FPL, and 400% or greater of the FPL. Insurance status was categorized into the following categories: full year private insurance, full year public insurance, full year private and public coverage, full year other comprehensive insurance, and uninsured at the time of the interview. Household composition included the following categories: single mother, two- parent, and other type of household composition. The highest educational attainment in the household was defined as less than high school, graduated from high school, and more than high school.
We identified two questions from the Survey to describe the health status of CSHCN with and without disabilities. Parents/Caregivers reported the severity of their child’s health conditions/problems (no severity, mild, moderate and severe) and how stable the child’s health was (changed all the time, changed once in a while or was usually stable). In addition, we compared the percentages of CSHCN with and without disabilities whose parents reported that their child felt anxious or depressed; had behavior problems; and/or had trouble keeping and making friends. As a measure of health impact, we report the percentage of CSHCN with and without disabilities who missed 20 or more days of school because of their health problems.
Health Services: The Medical Home, Service Need and Unmet Need
To evaluate health services, we measured care within a medical home, and need and unmet need for a variety of services. The presence of a medical home was operationalized using the five Maternal and Child Health Bureau (MCHB) criteria - having a personal doctor or nurse, having a usual source of care, receiving family-centered care, having no problem with getting referrals when needed, and receiving effective care coordination when needed,26,27 For our analysis, having a usual source of care, having a personal doctor or nurse and having family- centered care were dichotomized as present or not. The criterion of having no problems with referrals was measured as yes, no, and did not require; therefore, the percentage of children getting the service when needed was calculated as a fraction of those who reported needing it. The criterion for care coordination was calculated in the same way as having no problems with referrals. Therefore, both the referral outcome and care coordination outcome were considered met if individuals did not have a need, or when need was reported, it was also reported met. We also created a composite measure to classify children as receiving care in a medical home when all five criteria were met. To address need, we identified whether the sample child used specialty care, prescription medication, physical/occupational/speech therapy, mental health care, home health care, mobility aids, communication aids, medical supplies, durable medical equipment (DME), and/or respite care in the 12 months preceding the Survey. When one of the aforementioned items/services were needed but not received in the 12 months preceding the Survey, the need was considered unmet. Additionally, we created a composite measure of unmet need as the presence of one or more of the aforementioned types of unmet need for our multivariable analysis.
Statistical Analysis
We performed univariate and bivariate analyses to evaluate the differences between CSHCN with and without disabilities. Survey weights provided by the NCHS20, 28 were used to obtain population-level estimates. Multivariable logistic regression was conducted to identify factors associated with unmet need for services based on the behavioral model of health services use. We used the multiple imputation files available from the NCHS to account for the 9% missing income values, 29 and did not otherwise impute values of missing covariates. Instead, we compared the fit of models that included and excluded missing covariate values, and we found negligible differences between parameter estimates or confidence intervals for any covariate. We performed a Hosmer-Lemenshow goodness of fit test designed to take into account the complex survey design and found that our model had a good fit, with a p=0.44. The adjusted estimated prevalences of unmet need among CSHCN were calculated from the regression model. All analyses were conducted using STATA 11 (StataCorp; College Station, TX) to account for the complex nature of the survey design and to appropriately weight the estimates. The Committee on Human Research at the University of California San Francisco approved this study in the Exempt category.
RESULTS
Socio-demographics, Health and Psychosocial Characteristics
We estimate that in 2005-2006 13.9% of children in the United States had special health care needs. Of these children, 21.5% qualified as having disabilities in this study because they had at least one functional limitation, as shown in Table 1. This equates to 2.2 million children with disabilities associated with chronic conditions and 8 million other CSHCN. Boys, minority children, children living near or in poverty, uninsured and publicly insured children, children living in households headed by a single mother, and children living in homes in which the highest educational attainment was high school or less were over-represented in the sample of CSHCN with disabilities compared to CSHCN without disabilities. For example, 52.2% CI (50.3- 54.1) of CSHCN with disabilities live in homes with incomes below 200% of the FPL compared to 37.9% CI (36.9-38.9) of CSHCN without disabilities.
Table 1.
Distributions of Socio-demographic and Child Health and Related Characteristics of CSHCN by Disability
| CSHCN with Disabilities | CSHCN without Disabilities | |||
|---|---|---|---|---|
| Sample Distribution N=8,739 % (95% CI) |
Estimated Population (in millions) |
Sample Distribution N=31,984 % (95% CI) |
Estimated Population (in millions) |
|
| All: | 21.5% (20.8-22.1) | 2.2 | 78.5% (77.9-79.2) | 8.0 |
|
| ||||
| Gender:* | ||||
| Boys | 61.8% (60.0-63.5) | 1.4 | 58.7% (57.8-59.6) | 4.7 |
| Girls | 38.2% (36.5-40.0) | 0.8 | 41.3% (40.4-42.2) | 3.3 |
|
| ||||
| Age: | ||||
| 0-4 | 15.5% (14.3-16.9) | 0.3 | 16.3% (15.5-17.0) | 1.3 |
| 5-13 | 55.4% (53.7-57.2) | 1.2 | 56.1% (55.1-57.0) | 4.5 |
| 14-17 | 29.0% (27.4-30.7) | 0.6 | 27.7% (26.9-28.5) | 2.2 |
|
| ||||
| Race/Ethnicity:* | ||||
| White Non-Hispanic | 62.2% (60.4-64.0) | 1.4 | 66.2% (65.2-67.1) | 5.3 |
| Black Non-Hispanic | 17.9% (16.5-19.4) | 0.4 | 15.8% (15.1-16.6) | 1.3 |
| Hispanic | 12.7% (11.4-14.1) | 0.3 | 11.5% (10.9-12.2) | 0.9 |
| Other | 7.2% (6.4-8.2) | 0.2 | 6.5% (6.1-7.0) | 0.5 |
|
| ||||
| Income:* | ||||
| <200% FPL | 52.2% (50.3-54.1) | 1.1 | 37.9% (36.9-38.9) | 2.8 |
| 200-399% FPL | 27.0% (25.4-28.7) | 0.54 | 31.0% (30.1-31.9) | 2.3 |
| >/=400% FPL | 20.8% (19.4-22.3) | 0.42 | 31.1% (30.3-32.0) | 2.3 |
|
| ||||
| Insurance Status:* | ||||
| Private | 45.5% (43.7-47.2) | 1.0 | 62.9% (61.9-63.8) | 5.0 |
| Public | 36.7% (35.0-38.5) | 0.8 | 25.7% (24.8-26.6) | 2.1 |
| Private + Public | 11.7% (10.7-12.9) | 0.3 | 6.2% (5.7-6.6) | 0.5 |
| Other Insurance | 1.9% (1.5-2.3) | 0.04 | 2.0% (1.8-2.3) | 0.2 |
| Uninsured | 4.2% (3.9-5.0) | 0.09 | 3.3% (3.0-3.6) | 0.3 |
|
| ||||
| Household Composition:* | ||||
| Two-Parent | 59.5% (57.7-61.3) | 1.3 | 66.4% (65.5-67.3) | 5.1 |
| Single Mother | 35.3% (33.5-37.1) | 0.7 | 28.4% (27.5-29.3) | 2.2 |
| Other | 5.2% (4.6-6.0) | 0.1 | 5.2% (4.8-5.6) | 0.4 |
|
| ||||
| Highest Educational Attainment in the Home:* |
||||
| <High School | 8.7% (7.6-9.8) | 0.2 | 6.3% (5.8-6.9) | 0.5 |
| High School | 27.7% (26.0-29.4) | 0.6 | 21.8% (21.0-22.7) | 1.8 |
| >High School | 63.7% (61.9-65.4) | 1.4 | 71.8% (70.9-72.7) | 5.8 |
|
| ||||
| Condition Severity* | ||||
| None/Not Applicable | 2.4% (2.0-3.0) | 0.05 | 18.5% (17.8-19.2) | 1.5 |
| Minor | 18.7% (17.4-20.0) | 0.4 | 50.1% (49.2-51.1) | 4.0 |
| Moderate | 53.2% (51.4-55.0) | 1.2 | 27.6% (26.7-28.4) | 2.2 |
| Severe | 25.7% (24.2-27.3) | 0.6 | 3.9% (3.5-4.3) | 0.3 |
|
| ||||
| Condition Stability- Health care needs* | ||||
| Were usually stable | 48.9% (47.1-50.7) | 1.1 | 70.5% (69.6-71.4) | 5.6 |
| Changed once in a while | 35.6% (34.0-37.3) | 0.8 | 25.8% (25.0-26.7) | 2.1 |
| Changed all the time | 15.5% (14.2-16.8) | 0.3 | 3.7% (3.2-4.1) | 0.3 |
|
| ||||
| Missed >/= 20 days of school* | 12.0% (10.9-13.3) | 0.2 | 3.3% (3.0-3.8) | 0.2 |
|
| ||||
| Feels anxious or depressed* | 46.1% (44.3-47.9) | 1.0 | 24.0% (23.2-24.8) | 1.9 |
|
| ||||
| Has behavioral problems* | 39.6% (37.8-41.4) | 0.8 | 25.2% (24.4-26.0) | 2.0 |
|
| ||||
| Has trouble making or keeping friends* | 38.1% (36.3-39.9) | 0.8 | 15.6% (14.9-16.3) | 1.2 |
Chi-squared and t-tests were used to identify statistically significant differences (p<0.01) between CSHCN with and without disabilities.
CSHCN with disabilities had conditions that ‘changed all the time’ four times as frequently as other CSHCN and their conditions were rated as ‘severe’ seven times as frequently (Table 1). Feeling anxious and/or depressed was twice as commonly reported for CSHCN with disabilities than other CSHCN (46% versus 24%, p<0.001). Additionally, nearly 40% of CSHCN with disabilities had behavioral problems compared to only 25% of other CSHCN, p<0.001. Similarly, 38% of CSHCN with disabilities had trouble making or keeping friends compared to only 16% of other CSHCN, p<0.001. Of CSHCN with disabilities, 12% missed more than 3 weeks of school compared to 3.3% of CSHCN without disabilities, p<0.001.
Health Services: The Medical Home, Service Need and Unmet Need
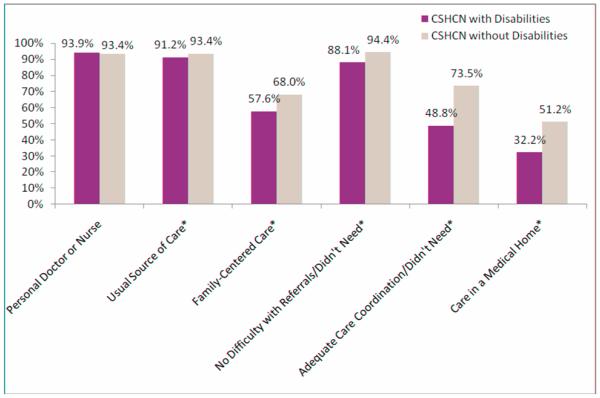
When the medical home was measured as a composite, only 31.8% of CSCHN with disabilities were receiving care within a medical home, compared to over half of other CSHCN (Figure 1). Over 93% of CSHCN reported having a personal doctor or nurse, regardless of disability status. On all other components of the medical home, statistically significant differences were noted such that CSHCN with disabilities less commonly reported meeting the component criteria. Most notably, only 48.8% of CSHCN with disabilities reported adequate care coordination compared to 73.5% of other CSHCN.
Figure 1.
Percentages of CSHCN with and without Disabilities Who Meet Medical Home Criteria
*statistically significant difference, p-value<0.01
As shown in Table 2, CSHCN with disabilities needed fewer prescription medications but statistically significantly more of every other item/service studied. Overall 94.9% of CSHCN without disabilities and 96.7% of CSHCN with disabilities had an identified need for at least one item/service. As a composite measure of unmet need, 22.8% CI (21.3-24.3) of CSHCN with disabilities had an unmet need for at least one of the aforementioned items/services compared to 7.4% CI (6.9-7.9) of other CSHCN. The unadjusted odds of having at least one unmet need for the aforementioned items/services was 3.71 CI (3.30-4.16) for CSHCN with disabilities compared to other CSHCN. CSHCN with disabilities has statistically higher odds of unmet need for the following services: prescription medication, specialty care, mental health services, physical/occupational/speech therapy, medical supplies, durable medical equipment, and communication aids.
Table 2.
Reported Need and Unmet Need for Services for CSHCN with and without Disabilities*
| Percentage with Service Need Present | Percentage with Unmet Need for Services | |||||
|---|---|---|---|---|---|---|
| CSHCN with disabilities n=8,719 |
CSHCN without disabilities n=32,004 |
Unadjusted Odds Ratio (Confidence Intervals) CSHCN with disabilities compared to other CSHCN |
CSHCN with disabilities |
CSHCN without disabilities |
Unadjusted Odds Ratio (Confidence Intervals) CSHCN with disabilities compared to other CSHCN |
|
| Prescription Medication N=35,179 |
84.5% | 86.9% | 0.82 (0.74-0.92) | 3.6% | 1.4% | 2.62 (1.97-3.47) |
| Specialty Care N=21,064 |
67.6% | 47.4% | 2.32 (2.13-2.52) | 8.6% | 4.1% | 2.25 (1.81-2.79) |
| Mental Health N=10,171 |
33.7% | 22.6% | 1.74 (1.59-1.90) | 17.9% | 13.8% | 1.36 (1.11-1.68) |
| PT/OT/Speech Therapy N=9,305 |
51.3% | 15.1% | 5.92 (5.43-6.48) | 16.6% | 10.9% | 1.63 (1.30-2.05) |
| Medical Supplies N=7,588 |
29.4% | 15.7% | 2.24 (2.04-2.46) | 3.9% | 1.8% | 2.26 (1.39-3.67) |
| Durable Medical Equipment N=4,662 |
20.8% | 8.9% | 2.70 (2.41-3.02) | 6.5% | 2.2% | 3.03 (1.71-5.38) |
| Respite Care N=1,855 |
14.3% | 1.9% | 8.69 (7.19-10.50) | 50.5% | 43.0% | 1.35 (0.93-1.95) |
| Home Health N=1,826 |
11.4% | 2.6% | 4.82 (4.06-5.73) | 12.9% | 8.0% | 1.71 (1.00-2.91) |
| Mobility Aids N=1,823 |
11.0% | 2.7% | 4.53 (3.82-5.37) | 9.8% | 4.2% | 2.48 (1.00-6.15) |
| Communication Aids N=898 |
8.1% | 0.6% | 14.99 (11.18-20.09) | 26.4% | 14.6% | 2.09 (1.08-4.03) |
| At least one of the listed identified N= 39,020 |
96.7% | 94.9% | 1.60 (1.31-1.95) | 22.8% | 7.4% | 3.71 (3.30-4.16) |
If need was identified as present, the survey asked if that need had been met. Unmet need represents when the service was identified as needed and not met.
The adjusted odds of having at least one unmet need was 1.68 CI (1.45-1.94) for CSHCN with disabilities compared to other CSHCN (see Table 3). Other child level predictors of unmet need included the ‘other’ race designation, living below 400% of the FPL, increased condition severity levels, and having health care needs that were not usually stable. The family level predictors of unmet need were living in a home headed by a single mother and living in a home where the highest educational attainment level was less than high school. The health systems factors of being uninsured and not receiving care within a medical home were associated with increased adjusted odds of unmet need, 3.03 (2.33-3.95) and 3.40 (2.87-4.03), respectively. The adjusted estimated prevalences of having at least one unmet need were highest among CSHCN with severe health conditions (32.0%), CSHCN with conditions that were unstable (24.3%), CSHCN who were uninsured (25.4%), and CSCHN with disabilities (18.6%); as shown in Table 3.
Table 3.
Adjusted Estimated Prevalences and Adjusted Odds Ratios of Unmet Need for At Least One Health Service/Item
| Adjusted Estimated Prevalences* of Unmet Need (95% Confidence Interval) |
Adjusted Odds* of Unmet Need (95% Confidence Interval) |
|
|---|---|---|
| Presence of Disability | ||
| No | 4.5% (4.0-5.2) | REF |
| Yes | 18.6% (17.0-20.3) | 1.68 (1.45-1.94) |
|
| ||
| Gender: | ||
| Girls | 5.7% (5.0-6.7) | REF |
| Boys | 6.5% (5.8-7.4) | 0.98 (0.85-1.13) |
|
| ||
| Age: | ||
| 0-4 | 4.8% (3.9-6.0) | REF |
| 5-13 | 6.3% (5.6-7.2) | 1.14 (0.92-1.41) |
| 14-17 | 6.7% (5.8-7.8) | 1.26 (1.00-1.58) |
|
| ||
| Race/Ethnicity: | ||
| White Non-Hispanic | 5.5% (4.9-6.3) | REF |
| Black Non-Hispanic | 7.2% (6.0-8.7) | 0.73 (0.60-0.91) |
| Hispanic | 8.8% (7.3-10.6) | 0.92 (0.75-1.14) |
| Other | 9.8% (7.8-12.2) | 1.34 (1.05-1.72) |
|
| ||
| Income: | ||
| <200% FPL | 12.0% (10.8-13.2) | 2.19 (1.73-2.77) |
| 200-399% FPL | 5.6% (4.8-6.5) | 1.43 (1.15-1.77) |
| >/=400% FPL | 3.3% (2.7-4.0) | REF |
|
| ||
| Insurance Status: | ||
| Private | 4.4% (3.8-5.1) | REF |
| Public | 10.7% (9.6-12.1) | 0.98 (0.80-1.20) |
| Private + Public | 12.7% (10.5-15.4) | 1.10 (0.85-1.41) |
| Other Insurance | 5.4% (3.6-8.1) | 1.01 (0.66-1.55) |
| Uninsured | 25.4% (21.3-30.0) | 3.03 (2.33-3.95) |
|
| ||
| Household Composition: | ||
| Two-Parent | 5.0% (4.4-5.8) | REF |
| Single Mother | 10.4% (9.2-11.6) | 1.23 (1.05-1.44) |
| Other | 7.6% (5.9-9.6) | 1.08 (0.83-1.42) |
|
| ||
| Highest Educational Attainment in the Home: | ||
| <High School | 10.5% (8.2-13.5) | 1.47 (1.09-1.98) |
| High School | 7.6% (6.5-8.8) | 1.05 (0.77-1.44) |
| >High School | 5.8% (5.1-6.6) | REF |
|
| ||
| Condition Severity | ||
| None/Not Applicable | 1.5% (0.9-2.5) | REF |
| Minor | 4.2% (3.6-4.9) | 2.12 (1.28-3.50) |
| Moderate | 13.6% (12.5-14.8) | 4.35 (2.67-7.08) |
| Severe | 32.0% (28.9-35.3) | 8.37 (5.01-13.97) |
|
| ||
| Condition Stability- Health care needs | ||
| Were usually stable | 4.4% (3.8-5.1) | REF |
| Changed once in a while | 10.9% (9.7-12.1) | 1.42 (1.22-1.65) |
| Changed all the time | 24.3% (20.7-28.3) | 1.62 (1.27-2.07) |
|
| ||
| Care within the Medical Home | ||
| Presence | 2.6% (2.2-3.2) | REF |
| Absence | 13.6% (12.5-14.8) | 3.40 (2.87-4.03) |
Adjusted for all other variables in the model. REF=referent group
DISCUSSION
Our analysis demonstrates that CSHCN are a distinct subset of CSHCN. Because of their higher rates of severe health conditions, psychosocial issues and unmet need, CSHCN with disabilities could benefit from focused attention to address their needs in the health and social realms. We found that CSCHN with disabilities differ from other CSHCN in many ways. Among CSHCN with disabilities, there is an over-representation of boys, Blacks, children covered by public insurance, uninsured children and those living in relative poverty. These differences are even more alarming considering the known sociodemographic disparities between CSHCN and children without special health care needs.6,28-31 We also observed that CSHCN with disabilities had more severe and less stable health conditions than other CSHCN. Bramlett et al. categorized CSHCN by functional status and also found differences between CSHCN with functional limitations and those without in terms of health status, and health complexity.8 This is not unexpected because as conditions such as asthma or cystic fibrosis become more severe, they more likely will limit children’s activities. Conversely, though, a child with mild cerebral palsy might be considered to be very healthy and stable but have disabilities in multiple functional domains. Therefore, practitioners should consider how factors that lead to disability can be mitigated and if stabilizing the child’s health condition might improve functional outcomes.
In addition to the relationships between disability status and condition severity and stability, we found that CSHCN with disabilities more commonly had psychosocial issues compared to other CSHCN. CSHCN with disabilities had more problems with behavior, feeling anxious or depressed and trouble making or keeping friends. These findings have important practice implications. With the knowledge that CSHCN with disabilities more commonly experience psychosocial problems, health care providers can screen those with disabilities more closely to identify and make recommendations to address psychosocial issues as needed. Addressing psychosocial issues early may help lessen the long-term effects on mental health and well-being.32 There is also a need to study more closely the factors that contribute to the differential experience of psychosocial problems between CSHCN with disabilities and other CSHCN in order to intervene on behalf of children in terms of their psychosocial well-being.
We also found that CSHCN with disabilities also experience health care inequities when compared to other CSHCN. Despite having increased need for health services, CSHCN with disabilities had more unmet need and were less commonly receiving care within a medical home. The lack of assistance with care coordination was especially notable. Bramlett et al also found that CSHCN with functional limitations experienced health care inequities in terms of insurance adequacy.8 According to the behavioral model of health service use, a multitude of factors may contribute to health care inequities.24,25,33 Our multivariable model points to condition severity as being the most strongly associated with unmet need. But even when controlling for condition severity, disability status was a predictor of unmet need and a significantly higher percentage of CSHCN with disabilities had at least one unmet need than other CSHCN. This indicates that while attending to severity is important, examining health factors beyond the condition itself is important for understanding health inequities. Both excess needs and excess unmet needs should be considered when tailoring programs and interventions to maximize the health and well-being of CSHCN with disabilities. Policies and practices that address unmet need are particularly relevant to CSHCN with disabilities because of the long-term potential impacts of unrealized access to care that could negatively impact health outcomes and participation in life events. Additionally, we found that the family characteristics of living in or near poverty, having lower educational attainment levels in the home and living in single mother households increased the odds of unmet need. Practitioners should be cognizant of these risk factors because these families are often disadvantaged in a multitude of ways that may limit their success in their interactions with the health care system. Conversely, the enabling factors of having care within a medical home and having health insurance were associated with decreased odds of unmet need. These associations were expected and have been shown in the literature previously for CSHCN.34,35 Thus, our findings add credence to the national call to address health insurance adequacy and care within a medical home for CSHCN with and without disabilities.
Limitations
In this study we used a screening tool through which parents/guardians identified children who had limitations in their ability to do the things that other children of the same age can do. The CSHCN Screener may not capture all children with disabilities, especially children with relatively mild functional limitations. Furthermore, by limiting our sample to children with special health care needs we might have underestimated the number of children with disabilities. We note that the national estimates of disability in childhood vary substantially. Using 2000 Medical Expenditures Panel Survey (MEPS) data, Newacheck and colleagues estimated that 7.3% of children have disabilities when disability is defined as a social role limitation or based on the receipt of special services.36 Nageswaran, Silver and Stein found that 60% of the estimated 12.8% CSHCN in the United States have functional limitations using the NS-CSHCN 2001.9 These differences indicate that defining and measuring disability in childhood likely requires refinement and consensus building for improved uniformity. And lastly, we used a cross-sectional survey for our analyses, thus we are limited in our ability to draw conclusions from the data because we are only able to identify associations. Further research is necessary to identify causal relationships between child, family and health systems factors and health care inequities for CSHCN with disabilities.
Conclusion
Our study highlights that the health and social challenges faced by CSHCN are more problematic for those with disabilities than those without. Furthermore, despite having more health services needs, CSHCN with disabilities have more unmet need and are not commonly receiving care within a medical home. Pediatric health providers should be cognizant of these findings and work to address the differences in health and health care delivery in their practices and community settings. Based on the differences noted between CSHCN with and without disabilities, we conclude that special attention needs to be given to those with disabilities to ensure that their health is maximized and the negative impacts of disability are minimized. Our findings also point to the need for continued research on this population to evaluate disparities and identify areas of intervention that successfully ameliorate the negative health and social consequences associated with disabilities and improve health services delivery and access.
Acknowledgments
Amy Houtrow, MD, MPH is funded on a Rehabilitation Medicine Scientist Training Program K12 through the NICHD 2K12H001097-12
Megumi Okumura, MD is funded on an AHRQ K-08 1K08HS017716
Footnotes
The authors have no conflicts of interest or corporate sponsorship.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Amy J Houtrow, Department of Pediatrics, University of California San Francisco, San Francisco, CA.
Megumi J Okumura, Department of Pediatrics, University of California San Francisco, San Francisco, CA.
Joan F Hilton, Department of Biostatistics, University of California San Francisco, San Francisco, CA.
Roberta S Rehm, Department of Family Health Care Nursing, University of California San Francisco, San Francisco, CA.
REFERENCES
- 1.Newacheck, Strickland B, Shonkoff JP, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998 Jul;102(1 Pt 1):117–123. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]
- 2.Bethell CD, Read D, Stein REK, Blumberg SJ, Wells N, Newacheck PW. Identifying Children With Special Health Care Needs: Development and Evaluation of a Short Screening Instrument. Ambulatory Pediatrics. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services . The National Survey of Children with Special Health Care Needs Chartbook 2005-2006. Rockville, MD: 2007. [Google Scholar]
- 4.Lollar DJ, Simeonsson RJ. Diagnosis to Function: Classification of Children and Youths. Developmental and Behavioral Pediatrics. 2005 August;26(4):323–330. doi: 10.1097/00004703-200508000-00012. 2005. [DOI] [PubMed] [Google Scholar]
- 5.Eddy LL, Engel JM. The impact of child disability type on the family. Rehabil Nurs. 2008 May-Jun;33(3):98–103. doi: 10.1002/j.2048-7940.2008.tb00212.x. [DOI] [PubMed] [Google Scholar]
- 6.Benedict RE. Disparities in Use of and Unmet Need for Therapeutic and Supportive Services among School-Age Children with Functional Limitations: A Comparison across Settings. Health Services Research. 2006;41(1):103–124. doi: 10.1111/j.1475-6773.2005.00468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hogan DP, Rogers ML, Msall ME. Functional limitations and key indicators of well-being in children with disability. Arch Pediatr Adolesc Med. 2000 Oct;154(10):1042–1048. doi: 10.1001/archpedi.154.10.1042. [DOI] [PubMed] [Google Scholar]
- 8.Bramlett MD, Read D, Bethell C, Blumberg SJ. Differentiating subgroups of children with special health care needs by health status and complexity of health care needs. Matern Child Health J. 2009 Mar;13(2):151–163. doi: 10.1007/s10995-008-0339-z. [DOI] [PubMed] [Google Scholar]
- 9.Nageswaran S, Silver EJ, Stein RE. Association of functional limitation with health care needs and experiences of children with special health care needs. Pediatrics. 2008 May;121(5):994–1001. doi: 10.1542/peds.2007-1795. [DOI] [PubMed] [Google Scholar]
- 10.King G, Tucker MA, Baldwin P, Lowry K, LaPorta J, Martens L. A life needs model of pediatric service delivery: services to support community participation and quality of life for children and youth with disabilities. Phys Occup Ther Pediatr. 2002;22(2):53–77. [PubMed] [Google Scholar]
- 11.Stein REK, Silver EJ. Are Rates of Functional Limitations Associated with Access to Care? A State-Level Analysis of the National Survey of Children with Special Health Care Needs. Maternal and Child Health Journal. 2005;9(0):S33–S39. doi: 10.1007/s10995-005-3856-z. [DOI] [PubMed] [Google Scholar]
- 12.Bethell C, Read D, Blumberg S, Newacheck P. What is the Prevalence of Children with Special Health Care Needs? Toward an Understanding of Variations in Findings and Methods Across Three National Surveys. Maternal and Child Health Journal. 2008;12(1):1–14. doi: 10.1007/s10995-007-0220-5. [DOI] [PubMed] [Google Scholar]
- 13.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002 Jan-Feb;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 14.Chen AY, Newacheck PW. Insurance Coverage and Financial Burden for Families of Children with Special Health Care Needs. Ambulatory Pediatrics. 2006;6(4):204–209. doi: 10.1016/j.ambp.2006.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Houtrow A, Kim S, Newacheck P. Health Care Utilization, Access and Expenditures for Infants and Young Children with Special Health Care Needs. Infants and Young Children. 2008 April/June 21;(2) [Google Scholar]
- 16.Mayer ML, Skinner AC, Slifkin RT. Unmet need for routine and specialty care: data from the National Survey of Children With Special Health Care Needs. Pediatrics. 2004 Feb;113(2):e109–115. doi: 10.1542/peds.113.2.e109. [DOI] [PubMed] [Google Scholar]
- 17.Newacheck PW, McManus M, Fox HB, Hung Y-Y, Halfon N. Access to Health Care for Children With Special Health Care Needs. Pediatrics. 2000 April 1;105(4):760–766. doi: 10.1542/peds.105.4.760. 2000. [DOI] [PubMed] [Google Scholar]
- 18.Dusing SC, Skinner AC, Mayer ML. Unmet Need for Therapy Services, Assistive Devices, and Related Services: Data From the National Survey of Children With Special Health Care Needs. Ambulatory Pediatrics. 2004;4(5):448–454. doi: 10.1367/A03-202R1.1. [DOI] [PubMed] [Google Scholar]
- 19.Strickland BB, van Dyck PC, Kogan MD, et al. Assessing and ensuring a comprehensive system of services for children with special health care needs: a public health approach. Am J Public Health. 2011 Feb;101(2):224–231. doi: 10.2105/AJPH.2009.177915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blumberg SJ, Welch EM, Chowdhury SR, Upchurch HL, Parker EK, Skalland BJ. Design and operation of the National Survey of Children with Special Health Care Needs, 2005-2006. Vital Health Stat 1. 2008 Dec;(45):1–188. [PubMed] [Google Scholar]
- 21.Blumberg SJ, Welch EM, Chowdhury SR, Upchurch HL, Parker EK, Skalland BJ. Design and operation of the national survey of children with special health care needs, 2005-2006. Vital Health Stat 1. 2008 Forthcoming. [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services. Health Resources and Services Administration. Bureau MaCH . The National Survey of Children with Special Health Care Needs Chart Book 2005-2006. US Department of Health and Human Services; Rockville, MD: 2008. [Google Scholar]
- 23.World Health Organization . Summary: World Report on Disability. Geneva: 2011. [PubMed] [Google Scholar]
- 24.Andersen R. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 25.Andersen R, Aday LA. Access to medical care in the U.S.: realized and potential. Med Care. 1978 Jul;16(7):533–546. doi: 10.1097/00005650-197807000-00001. [DOI] [PubMed] [Google Scholar]
- 26.The medical home. Pediatrics. 2002 Jul;110(1 Pt 1):184–186. [PubMed] [Google Scholar]
- 27.Child and Adolescent Health Measurement Initiative . 2005/2006 National Survey of Children with Special Health Care Needs SPSS Codebook. Portland, OR: 2008. [Google Scholar]
- 28.Newacheck PW, Hung YY, Wright KK. Racial and ethnic disparities in access to care for children with special health care needs. Ambul Pediatr. 2002 Jul-Aug;2(4):247–254. doi: 10.1367/1539-4409(2002)002<0247:raedia>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 29.Wong ST, Galbraith A, Kim S, Newacheck PW. Disparities in the Financial Burden of Children’s Healthcare Expenditures. Arch Pediatr Adolesc Med. 2005 November 1;;159(11):1008–1013. doi: 10.1001/archpedi.159.11.1008. 2005. [DOI] [PubMed] [Google Scholar]
- 30.Coker TR, Rodriguez MA, Flores G. Family-Centered Care for US Children With Special Health Care Needs: Who Gets It and Why? Pediatrics. 2010 June 1;125(6):1159–1167. doi: 10.1542/peds.2009-1994. 2010. [DOI] [PubMed] [Google Scholar]
- 31.Raphael JL, Guadagnolo BA, Beal AC, Giardino AP. Racial and ethnic disparities in indicators of a primary care medical home for children. Acad Pediatr. 2009 Jul-Aug;9(4):221–227. doi: 10.1016/j.acap.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 32.Bayer JK, Hiscock H, Ukoumunne OC, Price A, Wake M. Early childhood aetiology of mental health problems: a longitudinal population-based study. Journal of Child Psychology and Psychiatry. 2008;49(11):1166–1174. doi: 10.1111/j.1469-7610.2008.01943.x. [DOI] [PubMed] [Google Scholar]
- 33.Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res. 1983;18(1):49–74. Spring. [PMC free article] [PubMed] [Google Scholar]
- 34.Turchi RM, Gatto M, Antonelli R. Children and youth with special healthcare needs: there is no place like (a medical) home. Curr Opin Pediatr. 2007 Aug;19(4):503–508. doi: 10.1097/MOP.0b013e32825a67b4. [DOI] [PubMed] [Google Scholar]
- 35.Kogan MD, Newacheck PW, Honberg L, Strickland B. Association Between Underinsurance and Access to Care Among Children With Special Health Care Needs in the United States. Pediatrics. 2005 November 1;116(5):1162–1169. doi: 10.1542/peds.2004-2432. 2005. [DOI] [PubMed] [Google Scholar]
- 36.Newacheck PW, Inkelas M, Kim SE. Health Services Use and Health Care Expenditures for Children With Disabilities. Pediatrics. 2004 July 1;114(1):79–85. doi: 10.1542/peds.114.1.79. 2004. [DOI] [PubMed] [Google Scholar]