Abstract
The authors describe a unique presentation of celiac disease as multiple non-traumatic fractures in a young male without gastrointestinal complaints. A 29-year-old man presented with back pain and was found to have a non-traumatic compression fracture of the lumbar and thoracic spine on plain X-ray. Dual-energy x-ray absorptiometry (DXA) confirmed osteoporosis at the L3/L4 vertebral bodies. Parathyroid hormone (PTH), calcium, and vitamin D levels were normal. He had no gastrointestinal complaints, but serologic studies were positive to include an elevated gliadin IgA Ab, gliadin IgG Ab, and an elevated tissue transglutaminase IgA Ab. He was treated with a gluten-free diet, calcium, and vitamin D supplementation as well as teriparatide. Follow up bone density showed improvement and has no further fractures to date. Primary care physicians, gastroenterologists, and endocrinologists must have a high index of clinical suspicion for celiac disease in any patient who presents with low bone density regardless of the serum 25-OH vitamin D levels or presence of gastrointestinal complaints.
Overview
Celiac disease is a common gastrointestinal disease that affects up to 1% of the population of European descent.1,2 It is often diagnosed in patients with chronic diarrhea, weight loss, and fatigue; however some recent demographic studies have shown that less than 50% will have any of those symptoms and 25% of patients do not have any of these classic symptoms.3 This inconsistent presentation leads to a majority of patients being undiagnosed and more patients presenting later in life as 50% of adults are diagnosed over age 50.2,4,5
The non-classic symptoms include iron deficiency anemia, osteoporosis or low bone density, and dermatitis herpetiformis.6 We describe a unique case in which a young male without any of the classical celiac symptoms presented with back pain and no history of trauma but with several vertebral fractures. Low bone density was found on Dual energy x-ray absorptiometry scan prompting further evaluation leading to a diagnosis of celiac disease.
Case Report
A 29-year-old thin Caucasian male with a history of several traumatic childhood fractures presented with a 6-month history of back pain. He denied precipitating events or trauma. He awoke from sleep with severe, non-radiating pain in his lower back, thought it was muscle strain and treated it with ibuprofen and acetaminophen. At the time of presentation he had had three similar episodes. After each incident he described acute pain lasting 2 days to 2 weeks, subsiding to a dull, chronic pain with rest. Past medical history was significant for multiple bone fractures as a child and a fibular stress fracture associated with excessive running. Review of systems was otherwise unremarkable. Physical exam was notable only for kyphosis of the thoracic spine, which the patient stated was stable since childhood.
Plain X-rays of the thoracic and lumbar spine were obtained and revealed anterior wedge compression fractures of the T4, T6, L1, L2, and L4 vertebral bodies (Figure 1). Dual energy X-ray absorptiometry (DXA) showed low bone density with a T-score of −3.5 and a Z-score of −3.2.
Figure 1.
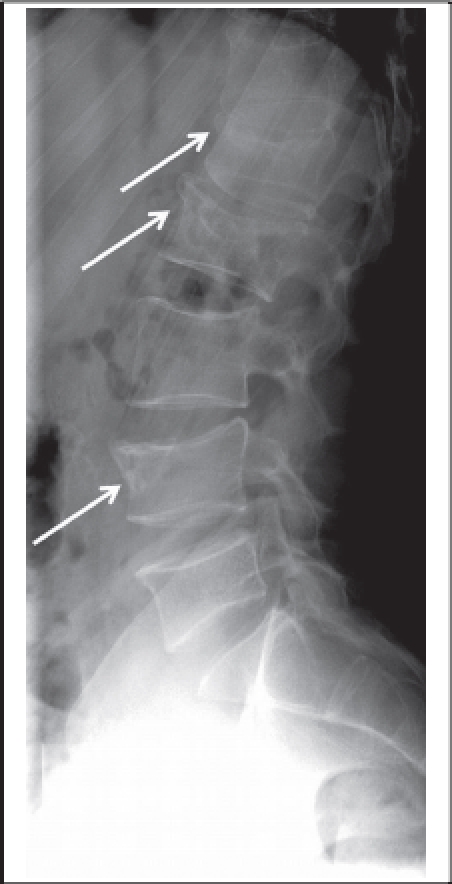
Lateral lumbar spine radiograph with anterior wedge compression fractures of the L1, L2, and L4 vertebral bodies.
The differential diagnosis of osteoporosis in men is broad and includes endocrine disease, hematologic disorders, connective tissue diseases, drug ingestion, and gastrointestinal disease. Testosterone, luteinizing hormone, follicle stimulating hormone, dehydroepiandrosterone sulfate (DHEA), morning cortisol, and thyroid stimulating hormone were normal. Parathyroid hormone (PTH) (33.1pg/ml), calcium (9.2mg/dL) and 25-hydroxy vitamin D level (35ng/ml) were also normal. Complete blood count, differential, erythrocyte sedimentation rate, C-reactive protein, HIV, serum protein electrophoresis, urine protein electrophoresis, rheumatoid factor, and nuclear antibody screen were unremarkable. He had a bone scan that revealed healing vertebral fractures noted above, old fractures of the right fibula and left fifth rib, and a new fracture of the T7 vertebral body (Figure 2). He was not consuming any medications, illicit drugs, and only rarely consumed alcohol. He had no gastrointestinal complaints, but serologic studies were positive for an elevated gliadin IgA Ab at 115 units/ml (>17 is positive), gliadin IgG Ab at 45 units/ml (>17 is positive), and tissue transglutaminase IgA Ab at 198 units/ml (>8 is positive). Upper endoscopy was performed and a duodenal biopsy showed focal villous blunting and atrophy with mildly expanded lamina propria with lymphocytes and plasma cells, consistent with Celiac disease.
Figure 2.
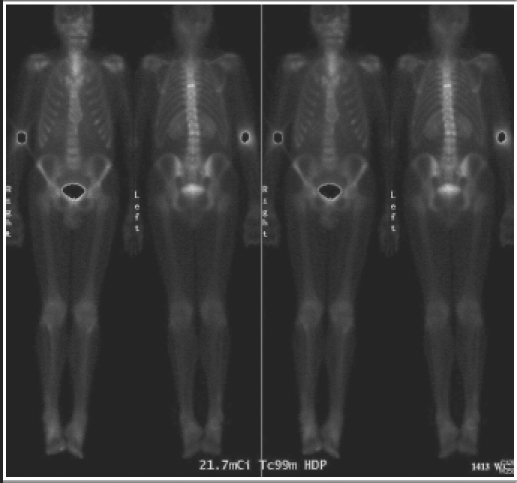
Bone scan revealed healing vertebral fractures at T4, T6, L1, L2, and L4, old fractures of the right fibula and left fifth rib, and a recent fracture of the T7 vertebral body.
He was started on treatment with a gluten-free diet, calcium and vitamin D supplementation as well as teriperatide 20mcg daily for a planned 2-year course. He immediately gained weight and follow up DXA done 8 months after starting treatment showed improvement with a Z-score of −2.7. He has been compliant with treatment and has not had any more fractures through 16 months of follow up.
Discussion
Celiac disease is most commonly found in patients presenting with diarrhea, weight loss and other gastrointestinal symptoms, however that typical presentation is now the atypical presentation as less than 50% of patients diagnosed have diarrhea.6 The next most common presenting symptoms are iron deficiency anemia, apthous ulcers, dermatitis herpetiformis, and low bone mineral density.
These “silent” or atypical presentations are becoming more and more common due to increased physician awareness and the availability of accurate serologic studies. Celiac disease is often a cause of low bone density and patients with celiac disease have an increased fracture risk, a hazard ratio of 1.43 or 43% increased risk when compared to age-matched healthy populations.4 This is thought to be due to lack of absorption of vitamin D and calcium causing a secondary hyperparathyroidism.7,8 On presentation, vitamin D levels are often lower and PTH levels are higher than controls.9
As seen in our patient this is not always the case, as his vitamin D level was 35ng/ml. There are other contributing factors to this poor bone density. In experimental models gut inflammation is shown to activate inflammatory cytokines that are members of the TNF-alpha family called receptor activator of nuclear factor kappa B (RANK) and its ligand (RANK-L).8,10 Gut inflammation also has a direct inhibitory effect on the usual inhibitor of this pathway, osteoprotegrin (OPG).10 Through this RANK/RANK-L/OPG pathway gut inflammation can have a direct negative effect on bone mineral density (BMD), that is independent of vitamin D absorption and could explain the degree of low BMD out of proportion to PTH and vitamin D levels. The level of gut inflammation was significant as is demonstrated by the significantly elevated level of anti-tissue transglutaminase ab, which is directly tied to severity of disease, but not always gastrointestinal symptoms.1,7
Screening for celiac disease during the evaluation of all patients with osteoporosis is not recommended by all. Previously it was thought that celiac disease would present early in life and usually did not overlap with the expected age range of osteoporosis. However 50% of diagnoses of celiac disease are in patients over the age of 50.5 In 2005 an article by Stenson et al, comprehensively reviewed screening for celiac disease in all osteoporotic patients. In this study the incidence of celiac disease in patients without gastrointestinal complaints who had osteoporosis was 3.4% compared to 0.2% of the general population. This study concluded that all patients with osteoporosis should be screened for celiac disease as treatment with a gluten-free diet would be integral to treating their bone disease as well as the many other known complications of untreated celiac disease. It was estimated this would have a cost of $1500 to identify one patient with celiac disease.
In contrast, many others suggest that all celiac patients with osteoporosis do not necessarily need to be screened. Some data suggest bone health can be correlated to classic symptoms and their severity.4 Additionally, low levels of disease may not have long term complications.5 Our case argues against a direct correlation of gastrointestinal symptoms to bone health as is supported in other population studies.3 Celiac patients have a hip fracture hazard ratio of 1.3–1.9 compared to the general population which can be reduced by starting a gluten-free diet thus stressing the importance of screening osteoporotic patients for celiac disease.11,12
There is debate on both ends of the spectrum from screening all patients with osteoporosis to screening only those with GI symptoms. However, given the body of literature most authors agree that patients who are either refractory to treatment or do not have classic risk factors (post-menopausal, thin, females) should be screened for celiac disease regardless of the presence of gastrointestinal symptoms.13
This case demonstrates the importance of considering celiac disease in patients without gastrointestinal complaints and the importance of recognizing the disease and treatment. We emphasize considering celiac disease in all patients with idiopathic low bone density even if vitamin D and PTH levels are normal. Furthermore, considering celiac disease in all patients with osteoporosis is reasonable and diagnostic testing is indicated in patients refractory to treatment with calcium and bisphosphanates. The known cases of celiac disease are often described as the tip of the iceberg as there are many undiagnosed patients. Recognition of these patients is important not only for bone health, but also overall health and life expectancy as 10 years in delayed diagnoses has been shown to increase overall mortality.5
Acknowledgements
This work was presented in poster format at the Army American College of Physicians meeting in Washington, DC. in November 2010 and the Hawai‘i Chapter American College of Physicians meeting, Honolulu, HI, January 2011.
Footnotes
The views expressed in this abstract/manuscript are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the US Government.
Declaration of Interest
There are no conflicts of interest.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1.Rodrigo L. Celiac disease. World J Gastroenterol. 2006;12(41):6585–6593. doi: 10.3748/wjg.v12.i41.6585. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez L, Green PH, et al. Extraintestinal Manifestations of celiac disease. Curr Gastroenterol Rep. 2006 Oct;8(5):383–389. doi: 10.1007/s11894-006-0023-7. [DOI] [PubMed] [Google Scholar]
- 3.Jones S, D'Souza C, et al. Patterns of clinical presentation of adult celiac disease in a rural setting. Nutrition Journal. 2006;5:24. doi: 10.1186/1475-2891-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olmos M, Antelo M, et al. Systemic review and meta-analysis of observational studies on the prevalence of fractures in celiac disease. Digestive and Liver Disease. 2008;40:46–53. doi: 10.1016/j.dld.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Goddard CJR, Gillet HR. Complications of celiac disease: are all patients at risk. Postgrad Med J. 2006;82:705–712. doi: 10.1136/pgmj.2006.048876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rampertab SD, Pooran N, Brar P, et al. Trends in presentation of celiac disease. Am J Med. 2006;65:343–357. doi: 10.1016/j.amjmed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 7.Stenson W, Newbery R, Lorenz R, et al. Increased Prevalence of Celiac Disease and Need for Routine Screening Among Patients with Osteoporosis. Arch Intern Med. 2005;165:393–399. doi: 10.1001/archinte.165.4.393. [DOI] [PubMed] [Google Scholar]
- 8.Stanzi A, Trinti B. Risk of osteoporosis in endocrine disorders and celiac disease. Ann Ist Super Sanita. 2007;43(4):430–433. [PubMed] [Google Scholar]
- 9.Corazza GR, Di Sario A, et al. Influence of pattern of clinical presentation and of gluten-free diet on bone mass and metabolism in adult celiac disease. Bone. 1996;18:525–530. doi: 10.1016/8756-3282(96)00071-3. [DOI] [PubMed] [Google Scholar]
- 10.Tilg H, Moschen A R, Kaser A, et al. Gut, inflammation and osteoporosis: basic and clinical concepts. Gut. 2008;57:684–694. doi: 10.1136/gut.2006.117382. [DOI] [PubMed] [Google Scholar]
- 11.West J, Logan RF, et al. Fracture risk in people with celiac disease: a population-based cohort study. Gastroenterology. 2003;123:429–436. doi: 10.1016/s0016-5085(03)00891-6. [DOI] [PubMed] [Google Scholar]
- 12.Vazquez H, Mazure R, et al. Risk of fractures in celiac disease patients: A cross-sectional, case control study. American Journal of Gastroenterology. 2000;95:183–189. doi: 10.1111/j.1572-0241.2000.01682.x. [DOI] [PubMed] [Google Scholar]
- 13.Karakan T, Ozyemisci-Taskiran O, et al. Prevalence of IgA-antiendomysial antibody in a patient cohort with idiopathic low bone mineral density. World J Gastroenterol. 2007;13(21):2978–2982. doi: 10.3748/wjg.v13.i21.2978. [DOI] [PMC free article] [PubMed] [Google Scholar]


