Abstract
Objective
Intimate partner violence (IPV) against women is a significant health issue in the United States and worldwide. The majority of studies on IPV have been conducted in urban populations. The objectives of this study are to determine if prevalence, frequency, and severity of IPV differ by rurality and to identify variance in geographic access to IPV resources.
Methods
A cross-sectional clinic-based survey of 1478 women was conducted to measure the 1-year prevalence of physical, sexual, and psychologic IPV. IPV intervention programs in the state were inventoried and mapped, and the distance to the closest program was estimated for each participant based on an innovative algorithm developed for use when only ZIP code location is available.
Results
Women in small rural and isolated areas reported the highest prevalence of IPV (22.5% and 17.9%, respectively) compared to 15.5% for urban women. Rural women reported significantly higher severity of physical abuse than their urban counterparts. The mean distance to the nearest IPV resource was three times greater for rural women than for urban women, and rural IPV programs served more counties and had fewer on-site shelter services. Over 25% of women in small rural and isolated areas lived >40 miles from the closest program, compared with <1% of women living in urban areas.
Conclusions
Rural women experience higher rates of IPV and greater frequency and severity of physical abuse yet live much farther away from available resources. More IPV resources and interventions targeting rural women are needed.
Introduction
The frequency of intimate partner violence (IPV) against women has been well documented, as have the many negative physical and mental health consequences among its victims.1–5 Few studies have examined prevalence rates of IPV by rurality, but the available literature indicates that it is as prevalent or more prevalent in rural than in urban populations.6–9
In the United States, Domestic Violence Intervention Programs (DVIP) have been established to provide services for victims of IPV and are the main resource for intervention. Services include emergency shelter, transitional housing, individual and group IPV counseling, resource referral, and advocacy.10 State DVIP programs are funded through a variety of federal legislative acts, including the Family Violence Services Act, the Victims of Crime Act, and the Violence Against Women Act. On any given day, however, an estimated 5200 women in the United States are turned away from DVIP services because of lack of space or funding.10
Access to health, prevention, and protection services in the United States is disparate based on population density: rural women have less access than urban women to domestic violence shelters, physical and mental health professionals, law enforcement, and judicial personnel.11–14 Rural women are also nearly twice as likely to be turned away from services because of the insufficient number of programs and inadequate staffing of community-based health programs; they also face barriers to accessing services because of geographic distance and isolation.7,10,15
This study examined a sample of women seeking elective abortions. IPV is more prevalent among women with unintended pregnancies than in the general population.16–20 Women seeking elective terminations of their pregnancies have substantially increased rates of IPV compared with other pregnant women.21 This high-risk population may also be an important focus for intervention efforts because their need for clinical services provides an opportunity for early screening and linkage with intervention services and primary healthcare.5 The objectives of this study were to first determine if IPV prevalence varies among women seeking elective abortion services according to rurality of residence and then to identify disparities in the location and types of DVIP services by rurality.
Materials and Methods
Population, design, and setting
This cross-sectional study was conducted from November 1, 2007, through July 18, 2008, in a large family planning clinic that provides aspiration and medication abortion. Eligibility criteria included attendance for elective abortion, Iowa residency, and English or Spanish proficiency. After clinic intake, education staff introduced the study to eligible patients in a private room. Participants who provided informed, voluntary consent completed a 10-minute, anonymous, self-administered, computer-based questionnaire (available in English or Spanish) to estimate the 12-month prevalence of physical, sexual, and psychologic abuse. This study was approved by the institutional review boards of the University of Iowa and the National Planned Parenthood Federation of America. IPV prevalence in this study population has been published previously.21
Study variables
IPV was defined as physical or sexual abuse by a current or former intimate partner or psychologic abuse by a current intimate partner during the prior 12 months. Physical and sexual abuse were measured using a modified version of the Abuse Assessment Screen (AAS).22,23 The AAS identifies the frequency and severity of physical abuse (defined as being hit, slapped, kicked, or otherwise physically hurt) and sexual abuse (forced to have sex or engage in a sex act against her will). Psychologic abuse was assessed using the Women's Experience with Battering (WEB) scale. The WEB measures women's experience with chronic, nonphysical psychologic abuse by a current intimate partner.24,25 Subjects used a 6-point Likert-type scale to rate their agreement or disagreement with 10 items; a total score of ≥20 indicated psychologic abuse.24,25
Because this was an anonymous survey, we could not ask for participants' addresses; instead, subjects provided their five-digit ZIP code. Women were identified as living in an urban, suburban, large rural town, small rural town, or isolated rural area based on 2004 Rural Urban Commuting Area (RUCA) codes (www.ers.usda.gov/Data/RuralUrbanCommutingAreaCodes/); categories were based on RUCA code definitions version 2.0 (depts.washington.edu/uwruca/ruca-codes.php). RUCA codes examine rurality on a continuum of population density considering influence of population density, in neighboring ZIP codes. RUCA codes for urban include 1.0, 1.1; suburban include 2.0, 2.1, 3.0, 4.1, 5.1, 8.1, 10.1; large rural towns include 4.0, 4.2, 5.0, 5.2, 6.0, 6.1; small rural towns include 7.0, 7.2, 7.3, 7.4, 8.0, 8.2, 8.3, 8.4, 9.0, 9.1, 9.2; and isolated areas include 10.0, 10.2, 10.3, 10.4, 10.5, 10.6. The suburban category was combined with urban because only 88 women in total and only 9 with any abuse were classified as suburban.
Demographic information collected included age, race, ethnicity, education, employment status, type of health insurance, and presence of children <18 living in the home. These were examined as covariates potentially associated with rurality and IPV prevalence.
Domestic Violence Intervention Program geocoding and service inventory
DVIPs in the State of Iowa were identified through a resource directory maintained by Children and Families of Iowa Family Violence Center.26 The list included 43 center locations operating during the study period: 22 included complete addresses, 18 included only P.O. boxes with ZIP codes, and 1 did not contain location information. The address list was verified using ArcMap software to ensure the accuracy of the geocoding process.
Each of the DVIP programs serve designated counties within the state. We examined the types of services provided based on the rurality of counties served. To designate rurality, we used U.S. Department of Agriculture (USDA) Urban Influence Codes (UIC), which, unlike RUCA codes, are assigned at the county level. UICs assign counties to categories based on their population size and distance to counties with larger populations. UIC categories included urban, suburban, rural, and remote rural counties using the most recently available county data from 2003 (www.ers.usda.gov/data/urbaninfluencecodes/). UIC codes of 1 or 2 were considered urban, 3–7 were considered suburban, 8–10 were rural, and >10 was remote rural. For all 99 Iowa counties grouped by UICs, we examined the average number of DVIP programs providing services per county, average number of counties served by each DVIP program; number of counties that do not have a program located in that county, availability of shelter beds, average number of shelter beds per county and per 100,000 population, and availability of transportation services. If the number of beds was not available, three beds per room were assumed. This analysis focused on the 28 DVIP programs that serve a general population; programs that served only the deaf or a specific ethnic group were excluded because we do not know the base populations for these specific populations.
Calculation of survey participant distance to IPV services
We used a probabilistic sampling method (PSM) we developed for this study.27,28 This method is appropriate when the only street address component known is the ZIP code, as is often the case with protected data. Although many studies use ZIP codes for geocoding, their tacit assumption is that the location is in the geometric center (centroid) of the ZIP code, which may not be accurate. Using PSM, we first created a sample of Census blocks within ZIP codes using Monte Carlo methods. We used Census blocks because adequate demographic data exist at this geographic level (e.g., age, gender distribution). We then weighted these Census blocks by the number of residents in the same age and gender (female) group as the study participants. Sample Census blocks that resulted in a distribution of 30 distance estimates representative of age and gender for each participant location were selected, and the median distance from this distribution was defined the most likely distance traveled to the nearest DVIP location. We computed 95% confidence intervals (CI) to identify the likely range of distances. Locations were geocoded using the street network (which includes gravel-top roads) obtained from the Department of Natural Resources/Iowa Geological Survey GIS Library (www.igsb.uiowa.edu/nrgislibx/).
Analysis
We examined participant demographic and IPV variables by rurality, based on the participant's ZIP code; differences were assessed using chi-square tests. Adjusted odds ratios (OR) controlling for age, race, insurance status, employment, and presence of children in the household were calculated using multiple logistic regression methods to estimate the association of rurality with IPV prevalence. These variables were chosen for model inclusion based on previously identified risk factors, and estimates are not presented for this analysis.21 Confidence limits (95%) that do not include the value of 1.0 were considered statistically significant. Likelihood ratio tests were insignificant, indicating an acceptable model fit, although R2 values were <0.10. Distances to IPV resources were compared by rurality for all women and women reporting IPV using a box and whiskers plot. This plot portrays the mean, median, range represented as minimum and maximum values, and the 1st and 3rd quartiles.
Results
Demographic characteristics of sample
A total of 2610 abortion clients were seen at the clinic during the study period; among these, 2230 met eligibility criteria, and 2209 were invited to participate. A total of 1498 women agreed to participate, and 1494 completed the questionnaire, yielding an overall participation rate of 66.9% (1494/2230) and a cooperation rate of 73.6% (1494/2029). A previous study compared participants with the overall clinic population and found participants to be a representative sample.21 We excluded 16 women who did not provide a ZIP code or residence, or the ZIP code provided did not match an existing Iowa ZIP code.
Among the 1478 women, 72.7% lived in urban or suburban areas (referred to hereafter as urban), 10.9% in large rural towns, 9.9% in small rural towns, and 6.6% in isolated rural areas (demographics not tabled). Urban women were more likely than rural women to be nonwhite (21.3%) or of Hispanic ethnicity (8.8%). A slightly higher proportion of women in large rural towns reported not working (32.9%) than women residing in other areas. Approximately a third of women in each area reported having no insurance, whereas women in large and small rural areas had a higher proportion of public insurance coverage (26.7% and 21.9%, respectively) than women in urban areas.
Relationship status, depressive symptoms, and alcohol consumption did not differ appreciably by rurality, although a higher proportion of isolated rural women engaged in binge drinking. Women in large and small rural areas were significantly more likely than urban women to have children in the home.
IPV prevalence by rurality
Overall, 16.1% of women reported any IPV in the last year (Table 1). Women in urban (15.5%) and large rural towns (13.5%) reported the lowest prevalence of any IPV, whereas women in small rural towns reported the highest prevalence (22.5%), followed by women in isolated rural areas (17.9%). Women in small rural towns had an increased overall IPV prevalence OR of 1.61 (95% CI 1.03-2.52) compared with urban women. Women in large rural towns had a slightly reduced and nonsignificant odds of IPV, and women in isolated rural areas had a 20% increased but nonsignificant odds. The odds of physical or sexual violence prevalence by rurality showed a trend similar to that for any IPV. Prevalence ORs of psychologic abuse did not differ appreciably by rurality, although psychologic abuse by a current partner was most prevalent among urban women (9.3%), followed by women in isolated rural areas (8.5%).
Table 1.
Prevalence and Odds of Intimate Partner Violence by Type of Abuse and Rurality Among Abortion Clients Screened for Intimate Partner Violence, Iowa, November 2006–July 2008 (n=1478)
| |
|
Any IPVa |
Physical and/or sexual IPV |
Battering (current partner only)b |
|||
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | ORc(95% CI) | n (%) | ORc(95% CI) | n (%) | ORc(95% CI) | |
| All women | 1478 | 233 (16.1) | 180 (12.5) | 97 (9.0) | |||
| Urban/suburban | 1074 (72.7) | 163 (15.5) | 1.0 (referent) | 121 (11.6) | 1.0 (referent) | 72 (9.3) | 1.0 (referent) |
| Large rural town | 161 (10.9) | 21 (13.3) | 0.9 (0.5-1.4) | 17 (10.6) | 0.9 (0.5-1.6) | 10 (8.2) | 1.0 (0.5-2.0) |
| Small rural town | 146 (9.9) | 32 (22.5) | 1.6 (1.03-2.5) | 27 (18.8) | 1.8 (1.1-3.0) | 9 (8.0) | 0.8 (0.4-1.8) |
| Isolated | 97 (6.7) | 17 (17.5) | 1.2 (0.7-2.1) | 15 (15.6) | 1.4 (0.8-2.5) | 6 (8.5) | 0.8 (0.3-2.2) |
Includes physical or sexual violence by a former or current partner and battering by a current partner.
Denominator for this analysis=1081.
Controls for age, race (white/nonwhite), health insurance (private, public, none), employment (yes/no), age (18–20, 21–24, 25–29, 30–34), and children <18 in the household (yes/no).
CI, confidence interval; IPV, intimate partner violence; OR, odds ratio.
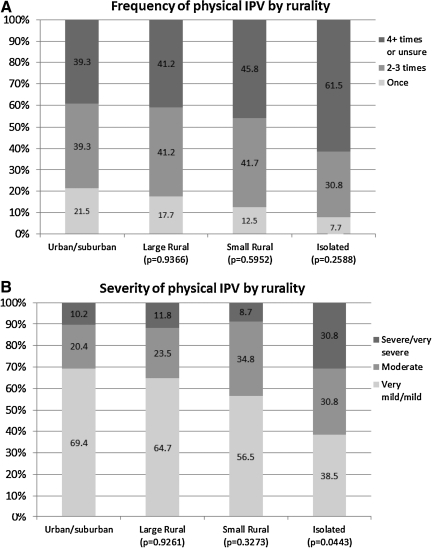
IPV frequency and severity by rurality
Among women who reported physical IPV, the frequency and severity increased with increasing rurality. In particular, subjects living in isolated rural areas reported a higher frequency and much higher severity of abuse than did their urban counterparts (Fig. 1). For example, 61.5% of isolated rural women reported four or more events of physical violence in the past year compared with 39.3% of urban women. More than 30% of isolated rural women reported severe to very severe physical violence compared with 10% of urban women.
FIG. 1.
(A) Frequency and (B) severity of physical intimate partner violence (IPV) by rurality.
IPV services by rurality
Iowa had a total of 28 independent DVIP that served the general population (Table 2). Urban counties had 13 DVIP for an average of 0.62 programs per county in the 21 urban counties. In contrast, rural counties had 10 DVIP for an average of 0.31 programs per county in the 32 rural counties. Urban DVIP provided services to an average of 2.8 counties, whereas rural DVIP served an average of 5.6 counties, and remote rural DVIP served an average of 5.0 counties. A third of urban counties did not have a DVIP based in the county, and approximately 80% of suburban, rural, and remote rural counties did not have a DVIP.
Table 2.
Domestic Violence Intervention Services Available in Iowa Counties, by County Urban Influence, 2008
| All counties (n=99) | Urban counties (n=21) | Suburban counties (n=37) | Rural counties (n=32) | Remote rural counties (n=9) | |
|---|---|---|---|---|---|
| Total number of DVIP | 28 | 13 | 17 | 10 | 6 |
| Average number of counties served by each DVIP | 3.7 | 2.8 | 3.5 | 5.6 | 5.0 |
| Number (%) of counties that do not have a program in that county (but are served by a program in another county) | 71 (71.7) | 7 (33.3) | 31 (83.8) | 25 (78.1) | 8 (88.9) |
| Number of programs that provide on-site shelter | 82 (82.8) | 16 (76.2) | 31 (83.8) | 31 (96.9) | 4 (44.4) |
| Number of programs that provide shelter through a safe house, motel, hotel | 17 (17.2) | 5 (23.8) | 6 (17.2) | 1 (3.1) | 5 (55.6) |
| Average number of shelter beds per county | 6.2 | 13.8 | 4.2 | 4.7 | 3.3 |
| Average number of shelter beds per 100,000 population | 20.9 | 18.0 | 23.8 | 27.4 | 26.5 |
| Serve Spanish speakers | 90 (90.9) | 20 (95.2) | 33 (89.1) | 28 (87.5) | 9 (100.0) |
| Transportation services | 75 (75.8) | 11 (52.3) | 24 (64.9) | 32 (100.0) | 8 (88.9) |
Iowa counties were classified by Urban Influence Codes using standard classification categories.
DVIP, Domestic Violence Intervention Programs.
DVIP provided shelter to women and their families either through direct shelter services at the DVIP site or through arrangements with safe houses and motels. Shelter services were available in only 44% of the remote rural county DVIP compared with >75% in less rural counties. Urban counties had an average of 13.8 shelter beds per county, compared with 4.2 for suburban, 4.7 for rural, and 3.3 for remote rural counties. Transportation was provided by 52.3% of DVIP serving urban counties, 64.9% of those serving suburban counties, 100% of those serving rural counties, and 88.9% of those serving remote rural counties.
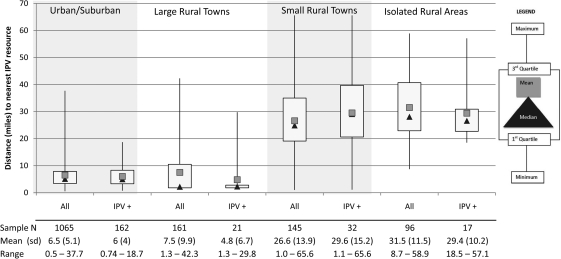
Distance to IPV resources
Figure 2 shows the estimated distances to the closest DVIP resource, by rurality, for the overall study sample and respondents who reported IPV. Women residing in urban counties lived an average of 6.5 miles from the closest resource, with a maximum distance of 37.7 miles. The average distance to the closest program among IPV victims was 6 miles, with a maximum of 18.7. Differences were not statistically different for IPV victims compared with all women or for women in urban vs. large rural towns.
FIG. 2.
Box and whiskers plot of distance, in miles, between participant residence and closest IPV resources for all subjects and the subset who are IPV victims.
The mean distance to the closest DVIP resource was three times farther for women residing in small rural or isolated areas than for women in urban or large rural towns. More than 25% of IPV victims in small rural and isolated areas had to travel a distance of >40 miles to the nearest services; in comparison, no women in urban and large rural towns were >40 miles from the nearest services. The average distance for IPV victims in small rural areas was 29.6 miles and for women in isolated rural areas was 29.4 miles.
Discussion
In this sample of women seeking elective abortions, the prevalence, frequency, and severity of physical and sexual IPV was higher among women living in small or isolated rural areas than in urban or large rural towns. Psychologic abuse prevalence did not vary by rurality. The few previous studies that have examined IPV prevalence by rurality in general populations of women also suggest that rates among rural women are commensurate with or higher than those among nonrural women.6,8 Reasons for the high prevalence of IPV in rural areas have not been adequately studied. It is suggested that hiding violence may be easier in isolated areas,8,15 leading to a self-selection of perpetrators in violent relationships to preferentially reside in or relocate to isolated areas. Higher prevalence could also be due to a disparity in access to services to help intervene against or prevent the violence.
DVIP in rural or remote rural counties covered considerably more counties per program, had fewer on-site shelter services, and had far fewer total shelter beds available per county. Reduced access to DVIP is exacerbated by lack of access to general and specialized healthcare in rural areas.29 Rural areas have significantly fewer primary care physicians and obstetrics/gynecology specialists, and residents have far less access to acute care hospitals than urban residents.29 Emergency departments and obstetrics/gynecology clinics are the most common medical settings to have integrated IPV screening, and these clinics can serve as resource liaisons for victims of IPV.
In addition to the lack of health and DVIP resources in many rural counties, the distance to these services for rural women represents a barrier to access. Women in urban, suburban, or large rural towns had an average drive of <10 miles to the closest DVIP resources, whereas women in small or isolated rural areas faced distances averaging >25 miles. The USDA reports that rural residents are more likely than urban residents to delay seeking or not seek medical care.29 Chan et al.30 examined access to medical services based on a 30-minute travel standard. For rural residents, >25% of the residents had travel times that exceeded the standard, and for emergency care, the travel time exceeded 75 minutes for one quarter of rural residents. Burstrom and Hunter31 examined factors affecting use of free mammogram services and found that patients who needed to travel >20 miles did not use the services provided. Three of four small rural and isolated rural women were >20 miles from the nearest DVIP resource, compared to one of five women in more urban areas. This distance represents a significant hardship for rural women to access resources, which is especially important considering they are victims of more frequent and severe IPV.
This study has several notable strengths, including the ability to detect high rates of IPV and to classify prevalence by IPV subtypes. This was among the first and the largest studies to examine IPV among the high-risk population of women seeking elective abortion and the first to examine access to services by rurality. We found that rural women tend to be as or more likely to experience abuse and more likely to suffer frequent and severe abuse, yet they have less access to DVIP services and must travel a much greater distance to reach existing services.
This study was also subject to some limitations. Our data are representative of women of reproductive age with unintended pregnancies in a largely rural state, that is, Iowa. Because this was an anonymous survey, we did not have addresses of participants available for precise geocoding. Distance to IPV resource calculations relied on ZIP codes, and new methods to best approximate these distances were employed.27,28 Although we collected information about the severity and frequency of abuse, we were not able to collect information about the context or bidirectionality of abuse or the timing of the abuse over the 12-month reporting period. Even though we had a large sample size, the number of women in isolated rural areas is low. This low number is most likely due to a lower population of isolated rural women but could also be due to barriers in seeking care that made these women underrepresented in our sample.
Conclusions
Isolation is a complex barrier to help seeking among rural victims of IPV.7,15 The isolation may contribute to increased severity and frequency of violence, perhaps because fewer people are around to witness the events. The isolation also secludes women from services, which could also contribute to high prevalence and high frequency through lack of intervention. IPV victims often have barriers to transportation because their partners do not allow them access to the car and track carefully when they leave the home and where they are going.7 Women living in rural areas rarely have access to public transportation, may have to travel long distances to services, and thus have significant barriers to accessing available domestic violence resources. Heath disparities among rural populations have been well documented, and an increased focus on access to preventive services, including DVIP resources, is critically needed.29
Acknowledgments
This work was supported by University of Iowa Social Research Center, the University of Iowa Injury Prevention Research Center (CDC R49 CCR703640), and the National Institutes of Health (R21 HD053850). We acknowledge Hind Beydoun for contributions to the survey instrument, Fiona Tubmen-Scovack for facilitating data collection, Sherry Sperlich for supporting the field operations, and Gerard Rushton for contributions to developing the distance estimation approach.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359:1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 2.Neggers Y. Goldenberg R. Cliver S. Hauth J. Effects of domestic violence on preterm birth and low birth weight. Acta Obstet Gynecol Scand. 2004;83:455–460. doi: 10.1111/j.0001-6349.2004.00458.x. [DOI] [PubMed] [Google Scholar]
- 3.Coker A. Davis KE. Arias I, et al. Physical and mental health effets of intimate partner violence for men and women. Am J Prev Med. 2002;23:260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 4.Staggs SL. Riger S. Effects of intimate partner violence on low-income women's health and employment. Am J Community Psychol. 2005;36:133–145. doi: 10.1007/s10464-005-6238-1. [DOI] [PubMed] [Google Scholar]
- 5.Wathen CN. MacMillan HL. Interventions for violence against women: Scientific review. JAMA. 2003;289:589–600. doi: 10.1001/jama.289.5.589. [DOI] [PubMed] [Google Scholar]
- 6.Breiding MJ. Ziembroski JS. Black MC. Prevalence of rural intimate partner violence in 16 U.S. states, 2005. J Rural Health. 2009;25:240–246. doi: 10.1111/j.1748-0361.2009.00225.x. [DOI] [PubMed] [Google Scholar]
- 7.Lanier C. Maume MO. Intimate partner violence and social isolation across the rural/urban divide. Violence Against Women. 2009;15:1311–1330. doi: 10.1177/1077801209346711. [DOI] [PubMed] [Google Scholar]
- 8.Murty SA. Peek-Asa C. Zwerling C. Stromquist AM. Burmeister LF. Merchant JA. Physical and emotional partner abuse reported by men and women in a rural community. Am J Public Health. 2003;93:1073–1075. doi: 10.2105/ajph.93.7.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Hightower NR. Gorton J. Domestic violence among patients at two rural health care clinics: Prevalence and social correlates. Public Health Nurs. 1998;15:355–362. doi: 10.1111/j.1525-1446.1998.tb00360.x. [DOI] [PubMed] [Google Scholar]
- 10.Iyengar R. Sabik L. The dangerous shortage of domestic violence services. Health Aff. 2009;28:1052–1065. doi: 10.1377/hlthaff.28.6.w1052. [DOI] [PubMed] [Google Scholar]
- 11.Lohmann N. Lohmann RA. Rural social work practice. NewYork: Columbia University Press; 2005. [Google Scholar]
- 12.Merwin E. Hinton I. Dembling B. Stern S. Shortages of rural mental health professionals. Arch Psychiatr Nurs. 2003;17:42–51. doi: 10.1053/apnu.2003.1. [DOI] [PubMed] [Google Scholar]
- 13.Merwin E. Snyder A. Katz E. Differential access to quality rural healthcare—Professional and policy challenges. Fam Community Health. 2006;29:186–194. doi: 10.1097/00003727-200607000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Mueller KJ. MacKinney AC. Care across the continuum: Access to health care services in rural America. J Rural Health. 2006;22:43–49. doi: 10.1111/j.1748-0361.2006.00010.x. [DOI] [PubMed] [Google Scholar]
- 15.Riddell T. Ford-Gilboe M. Leipert B. Strategies used by rural women to stop, avoid, or escape from intimate partner violence. Health Care Women Int. 2009;30:134–159. doi: 10.1080/07399330802523774. [DOI] [PubMed] [Google Scholar]
- 16.Woo J. Fine P. Goetzl L. Abortion disclosure and the association with domestic violence. Obstet Gynecol. 2005;105:1329–1334. doi: 10.1097/01.AOG.0000159576.88624.d2. [DOI] [PubMed] [Google Scholar]
- 17.Kaye D. Domestic violence among women seeking post-abortion care. Int J Gynecol Obstet. 2001;75:323–325. doi: 10.1016/s0020-7292(01)00484-2. [DOI] [PubMed] [Google Scholar]
- 18.Evins G. Chescheir N. Prevalence of domestic violence among women seeking abortion services. Womens Health Issues. 2006;6:204–210. doi: 10.1016/1049-3867(95)00012-7. [DOI] [PubMed] [Google Scholar]
- 19.Castro RP. Peek-Asa C. Garcia L. Ruiz A. Kraus JF. Risks for abuse against pregnant Hispanic women. Morelos, Mexico and Los Angeles County, California. Am J Prev Med. 2003;25:325–332. doi: 10.1016/s0749-3797(03)00211-3. [DOI] [PubMed] [Google Scholar]
- 20.Guo SF. Wu JL. Qu CY. Yan RY. Physical and sexual abuse of women before, during, and after pregnancy. Int J Gynaecol Obstet. 2004;84:281–286. doi: 10.1016/j.ijgo.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 21.Saftlas AF. Wallis AB. Shochet T. Harland KK. Dickey P. Peek-Asa C. Prevalence of intimate partner violence among an abortion clinic population. Am J Public Health. 2010;100:1412–1415. doi: 10.2105/AJPH.2009.178947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coker AL. Pope BO. Smith PH. Sanderson M. Hussey JR. Assessment of clinical partner violence screening tools. J Am Med Womens Assoc. 2001;56:19–23. [PubMed] [Google Scholar]
- 23.McFarlane J. Parker B. Soeken K. Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267:3176–3178. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- 24.Smith PH. Earp JA. DeVellis R. Measuring battering: Development of the Women's Experience with Battering (WEB) Scale. Womens Health. 1995;1:273–288. [PubMed] [Google Scholar]
- 25.Coker AL. Smith PH. McKeown RE. King MJ. Frequency and correlates of intimate partner violence by type: Physical, sexual, and psychological battering. Am J Public Health. 2000;90:553–559. doi: 10.2105/ajph.90.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Children and Families of Iowa. Family Violence Center Services. 2005. www.cfiowa.org/asp/news/news.asp?t=7&m=45&i=1 www.cfiowa.org/asp/news/news.asp?t=7&m=45&i=1
- 27.Beyer K. Schultz AJ. Rushton G. Using ZIP codes as geocodes in cancer research. In: Rushton G, editor; Armstrong MP, editor; Gittler J, et al., editors. Geocoding health data: The use of geographic codes in cancer prevention and control, research and practice. Boca Raton: CRC Press; 2007. [Google Scholar]
- 28.Beyer KM. Saftlas A. Wallis AB. Peek-Asa C. Rushton G. A probabilistic sampling method (PSM) for estimating geographic distance to health services when only the region of residence is known. Intl J Health Geogr. 2011;10:4–12. doi: 10.1186/1476-072X-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones CA. Parker TS. Ahearn M. Mishra AK. Variyam JN Health status and health care access of farm and rural populations. Economic Information Bulletin No. 57. United States Department of Agriculture, Economic Research Service. 2009.
- 30.Chan LL. Hart G. Goodman D. Geographical access to health care for rural medicare beneficiaries. J Rural Health. 2006;22:140–146. doi: 10.1111/j.1748-0361.2006.00022.x. [DOI] [PubMed] [Google Scholar]
- 31.Burstrom JE. Hunter DC. Going the distance: How far will women travel to undergo free mammography? Mil Med. 2001;166:347–349. [PubMed] [Google Scholar]