Abstract
By creating mutations in the Burkholderia mallei ATCC 23344 animal pathogen-like type III secretion system (TTSS), this study analyzes the correlation between type III secretion and the pathogenicity of ATCC 23344 in vivo. Mutagenesis demonstrated that a functional TTSS was required for the full pathogenicity of ATCC 23344 in the BALB/c mouse and Syrian hamster models of infection. However, vaccination with each mutant failed to elicit a protective immunity against challenge with wild-type ATCC 23344.
Burkholderia mallei, the causative agent of glanders disease, is a gram-negative, oxidase-positive, nonmotile bacillus that normally infects equines (horses, mules, and donkeys). B. mallei is an obligate animal pathogen that can infect various solipeds, mice, guinea pigs, rabbits, monkeys, hamsters, and even lions and dogs that consume contaminated meat (2, 6, 8). Humans are considered an incidental host for B. mallei, and individuals whose occupation subjects them to contact with B. mallei, particularly laboratory workers, are at high risk for contracting glanders disease (2). Occupational infection with B. mallei can occur via the cutaneous and inhalation routes.
Numerous gram-negative bacteria, including both animal and plant pathogens, encode specialized type III secretion systems (TTSS) that deliver bacterial proteins (effector molecules) into the plasma membrane and cytoplasm of eukaryotic cells (4). Several investigations recently identified the presence of animal and plant pathogen-like TTSS in Burkholderia pseudomallei (9, 13, 15). Of particular interest, and the scope of this investigation, is the animal pathogen-like TTSS encoded by B. mallei ATCC 23344. To evaluate the role of TTS in the virulence of ATCC 23344, specific mutations were created within the bsaQ and bsaZ alleles, which are homologues of the Salmonella enterica serovar Typhimurium invA and spaS genes and have been shown to encode proteins required for bacterial pathogenicity both in vivo and in vitro (4). In B. pseudomallei, mutation of the bsaZ (strain RD02 in this study) gene caused a drastic reduction in intracellular replication within J774.2 murine macrophages, failure of endocytic vacuole escape, and inhibition of actin polymerization (13). Considering the history and highly infective nature of B. mallei, as well as the potential for weaponization, there is a significant need to identify virulence determinants encoded by this bacterium.
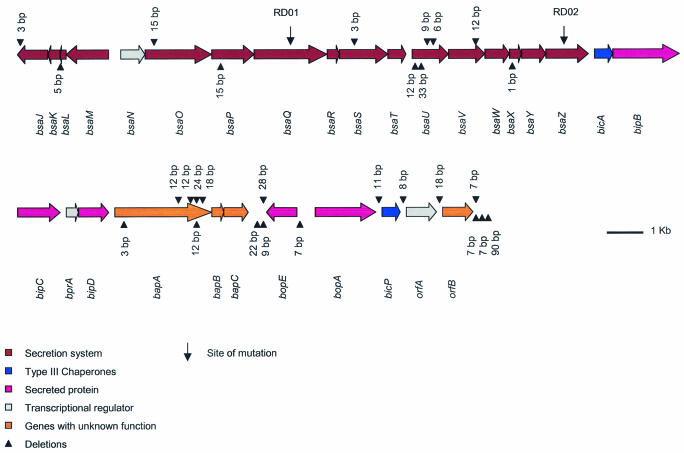
Analysis of the ATCC 23344 genome (http://www.tigr.org/) revealed the presence of a TTSS genetically similar (Fig. 1) to the B. pseudomallei animal pathogen-like TTSS locus reported by Stevens et al. (13). The ATCC 23344 TTSS encodes 30 open reading frames (ORFs) and shares genetic similarity to the Salmonella inv/spa/prg and Shigella ipa/mxi/spa systems (thoroughly reviewed in reference 4). Interestingly, multiple sequence gaps ranging from 1 to 90 bp were identified when the B. pseudomallei K96243 (http://www.sanger.ac.uk/) and ATCC 23344 TTSS loci were aligned with each other and compared at the nucleotide level (Fig. 1). Many of the sequence gaps are flanked by simple sequence repeats, which may provide a mechanism for the addition or removal of amino acids from the encoded proteins. A majority of the sequence gaps (99%) occurring within putative ORFs did not induce frameshift mutations because they occurred in multiples of 3 bp. In contrast, sequence gaps not divisible by 3, which generate frameshifts, were primarily present within intergenic regions. However, located in the 5′ region of the bsaX allele (Fig. 1), a 1-bp deletion was identified, which conceivably causes a frameshift resulting in a truncated protein in B. mallei. These results suggest the BsaX protein may not be an essential component of the Burkholderia TTSS.
FIG. 1.
Schematic organization of the genes encoding the B. mallei ATCC 23344 animal pathogen-like TTS apparatus. The nomenclature of the putative ORFs has been kept consistent with that of the B. pseudomallei TTSS. The B. mallei TTS locus is approximately 32,000 bp, has a relative G+C content of 69.9%, which is consistent with the ATCC 23344 genome, and is located on chromosome 2 beginning at nucleotide 1,201,133 and ending at nucleotide 1,233,132. Inverted triangles (▾) located above the ORFs represent sequence gaps present in the B. pseudomallei K96243 TTSS, while triangles (▴) depict sequence gaps identified in the ATCC 23344 TTSS. Mutation sites are indicated with arrows.
Bacterial strains, plasmids, and PCR primers used in this study are listed in Table 1. Primers for the bsaQ and bsaZ (13) genes were designed in silico using the nucleotide sequence of the B. mallei ATCC 23344 TTSS. Disruption of these alleles, which are essential components of the secretion apparatus, would likely exert a polar effect on the ATCC 23344 TTSS and disrupt effector molecule secretion. Genomic DNA for PCR amplification was purified using the MasterPure DNA purification kit according to the manufacturer's instructions (Epicentre Technologies, Madison, Wis.). Internal gene fragments for creating disruption cassettes were PCR amplified using the following conditions: one cycle at 94°C for 5 min; 30 cycles at 94°C for 30 s, 56°C for 30 s, and 72°C for 30 s; followed by a final 7-min extension at 72°C. Internal gene amplicons were subcloned into pCR2.1-TOPO (Invitrogen, Carlsbad, Calif.) and transformed into One Shot chemically competent Escherichia coli cells (Invitrogen). Integration cassettes were made by digesting pCR2.1-TOPO containing the bsaQ and bsaZ internal gene amplicons with EcoRI (New England Biolabs, Beverly, Mass.) followed by subcloning (Fast-Link DNA ligation kit; Epicentre Technologies) into the suicide vector pTSV3 digested with EcoRI. Ligations were electroporated into E. coli SM10 (11) and mobilized into ATCC 23344 using methods described by DeShazer et al. (3). To confirm site-specific integration (single-crossover mutants), PCR parameters modified from those described above, specifically increasing the extension to 4 min, were employed using gene-specific primers flanking the bsaQ and bsaZ alleles (Table 1). To confirm the stability of our merodiploids in vitro, organ extracts 30 days postexposure were plated on Luria-Bertani plates (Fisher Scientific, Pittsburgh, Pa.) containing 4% glycerol (vol/vol) (LBG) with and without antibiotic. Whole-body aerosol exposures of 6- to 8-week-old female BALB/c mice (National Cancer Institute, Frederick, Md.) using ATCC 23344, RD01 (bsaQ::pTSV3), and RD02 (bsaZ::pTSV3) were performed as described by Jeddeloh et al. (5). A relative dose of 1.0 × 104 CFU was targeted for each strain, representing approximately 10 times the 50% lethal dose (LD50) (5).
TABLE 1.
Bacterial strains, plasmids, and primers used in this study
| Strain, plasmid, or primer | Descriptionc | Reference or source |
|---|---|---|
| E. coli strains | ||
| TOP10 | Used for cloning and blue-white screening | Invitrogen |
| SM10 | Mobilizing strain, RP4 chromosomally integrated, Kmr | 12 |
| B. mallei strains | ||
| ATCC 23344 | Human isolate | USAMRIID |
| RD01 | ATCC 23344 derivative, bsaQ::pTSV3, Tpr | This study |
| RD02 | ATCC 23344 derivative, bsaZ::pTSV3, Tpr | This study |
| Plasmids | ||
| pPCR2.1-TOPO | TA cloning vector, Kmr Apr | Invitrogen |
| pTSV3 | pTnMod-OTp lacking the 1.5-kb BglII tnp fragment; mobilizable Tpr suicide vector | This study |
| pRD01 | Contains a 489-bp PCR amplicon from the ATCC 23344 bsaQ gene; Tpr | This study |
| pRD02 | Contains a 313-bp PCR amplicon from the ATCC 23344 bsaZ gene; Tpr | This study |
| pTnMod-OTp | Modular mini-transposon; pMB1 oriR, Tpr | 1 |
| Primers | ||
| bsaQiFa | 5′-ACGCGATGCCCGGCAAGCAGATGA-3′ | This study |
| bsaQiR | 5′-GCGCGAGCGCGATCAGCAGGAAGA-3′ | This study |
| bsaQgFb | 5′-CGCTCGGCGGCGTGCTGCTCA-3′ | This study |
| bsaQgR | 5′-AGCGGGGTCATCGCATGGCTCCTG-3′ | This study |
| bsaZiF | 5′-GATGAATCTCGCGCCGCTTGCTCT-3′ | This study |
| bsaZiR | 5′-GACGCGGTGAAGGCGCTGCTCTAT-3′ | This study |
| bsaZgF | 5′-CGCCGCCGCCATTTCCTG-3′ | This study |
| bsaZgR | 5′-GCGCCGTTCGTGAGCCTGTTCTAT-3′ | This study |
Within the primer nomenclature, i specifies internal gene primers.
Gene-specific primers are designated with the letter g.
Kmr, kanamycin resistance; Tpr, trimethoprim resistance; Apr, ampicillin resistance.
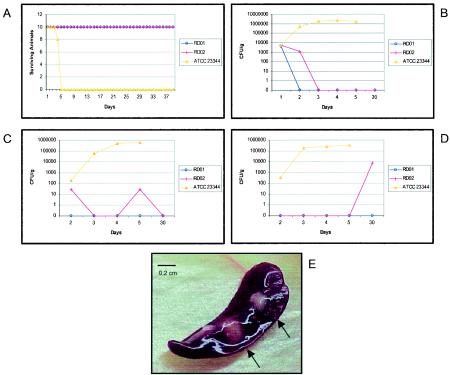
Figure 2A depicts the survival pattern of BALB/c mice (10 mice for each bacterial strain) infected via aerosol with ATCC 23344, RD01, or RD02. Mice infected with approximately 1.2 × 104 CFU of ATCC 23344 began to die at day 4, and the remaining animals died at day 5. All mice exposed to RD01 and RD02 survived an aerosol challenge of 1.8 × 104 and 1.5 × 104 CFU, respectively, and exhibited no clinical symptoms 42 days postexposure.
FIG. 2.
Mutations in the B. mallei ATCC 23344 TTSS locus drastically reduce virulence in a BALB/c animal model. (A) Survival of BALB/c mice exposed to ATCC 23344, RD01 (bsaQ::pTSV3), and RD02 (bsaZ::pTSV3). (B to D) Relative bacterial loads within the lungs, liver, and spleen of BALB/c mice challenged via aerosol with ATCC 23344, RD01, and RD02. (E) Multiple splenic abscesses (arrows) observed after 30 days postexposure to RD02.
To analyze the pathogenicity of ATCC 23344, RD01, and RD02, bacterial loads within the spleen, liver, and lungs of BALB/c mice challenged with each strain (doses were identical to those previously described) were assayed over a 5-day period postexposure. Briefly, one mouse from each experimental group was euthanized (CO2 chamber) on each of days 1 to 5, and the organs were extracted, homogenized in sterile phosphate-buffered saline, serially diluted, and plated on LBG. In addition, to determine if animals were chronically infected with RD01 and RD02, a single animal was euthanized 30 days postchallenge and organs were processed as described above. Figure 2B shows the bacterial loads of ATCC 23344, RD01, and RD02 within the lungs of BALB/c mice. Bacterial counts for ATCC 23344 progressively increased over the 5-day course of analysis and peaked at day 4, with an average load of 2.4 × 106 CFU/g of homogenized tissue. Organ loads within the liver and spleen spiked at day 5 with an enumerated concentration of 5.8 × 105 and 3.5 × 105 CFU/g of organ, respectively (Fig. 2C and D). Due to the animal mortality of groups infected with wild-type ATCC 23344, organ assays were not possible at day 30. In comparison, recovery of RD01 and RD02 within the lungs of challenged mice was markedly reduced in contrast to that of ATCC 23344 (Fig. 2B). Both RD01 and RD02 were cleared from the lungs at days 2 and 3 postexposure, respectively. Interestingly, animals challenged with RD01 contained no recoverable organisms from the liver or spleen at days 2 to 30 (Fig. 2C and D). In contrast, at days 2 and 5, the livers of the experimental group receiving RD02 contained 2.9 × 101 CFU/g of organ tissue. Unlike ATCC 23344 and RD01, RD02 caused a biphasic course of infection and trophism for the liver and spleen was observed. At days 3 and 30, the livers of mice infected with RD02 were sterile compared to the spleen, which contained 7.3 × 103 CFU/g of homogenized tissue at day 30 (Fig. 2D). The stability of each merodiploid was analyzed from lung, liver, and spleen samples (30 days postexposure) by plating extracts on nonselective LBG. As anticipated, vector integration in vivo was stable without the presence of trimethoprim (data not shown).
To determine if RD01 and RD02 provided protection against wild-type ATCC 23344, experimental groups exposed to RD01 and RD02 were rechallenged by aerosol with each corresponding mutant at day 21. Following this booster, on day 42 mice were aerosolized with 1.7 × 105 CFU of ATCC 23344 (100 times the LD50). Unfortunately, neither RD01 nor RD02 conferred protection against challenge with wild-type ATCC 23344. These results could have been the consequence of the dose of ATCC 23344 delivered. For RD01, these findings were consistent with the observed rapid clearance from the lungs of infected animals (Fig. 2B). However, these results were surprising for RD02, which persisted in the liver for several days postchallenge at concentrations conceivably sufficient to generate an adequate immunological response (Fig. 2C).
Clinical manifestations, such as fur ruffling and animal huddling, of mice challenged with ATCC 23344 began 2 days postexposure. Animals receiving RD01 and RD02 did not exhibit any clinical symptoms throughout the 42-day course of infection. However, gross pathological analysis of spleen extracts from animals challenged with RD02 (30 days after exposure) revealed extensive splenic abscesses (Fig. 2E), indicating a chronic form of infection.
Previous investigations demonstrated the extreme sensitivity (<10 CFU) of Syrian golden hamsters to ATCC 23344 (3), which makes this animal model ideal for analyzing the pathogenicity of mutant derivatives of B. mallei. Using the methods described by DeShazer et al. (3), male Syrian golden hamsters were infected intraperitoneally with 1.0 × 101 to 1.0 × 103 CFU of ATCC 23344, 1.0 × 101 to 1.0 × 106 CFU of RD01, or 1.0 × 101 to 1.0 × 105 CFU of RD02. Five animals for each 10-fold dilution series were used, and the LD50 was determined at day 4 as described by Reed and Muench (10). The relative LD50 for ATCC 23344 was <13 CFU, in contrast to >106 CFU and >105 CFU for RD01 and RD02, respectively. These findings definitively illustrate that TTS is crucial for the pathogenicity of ATCC 23344.
In addition to analyzing the organ loads of infected animals and determining the LD50s, the immunoglobulin G (IgG) titer against RD01 and RD02 was assayed 30 days postchallenge. IgG titers for each strain, in one animal from the ATCC 23344, RD01, and RD02 groups used for organ load analysis, were determined using an enzyme-linked immunosorbent assay-based technique described by Waag et al. (14). Positive control ATCC 23344 antigen was prepared by harvesting an overnight culture of ATCC 23344 grown in glycerol (4% [vol/vol])-tryptone broth (Fisher Scientific). The cellular pellet was resuspended in Hanks balanced salt solution, irradiated at 2.1 Mrads, washed three times in Hanks balanced salt solution, and resuspended in sterile water to yield a 1-mg/ml stock. An assayable immunological response, expressed as the reciprocal of the highest dilution yielding a positive reaction, was observed for RD02 (800) and the ATCC 23344 positive control (12,500). However, the IgG titer of animals infected with RD01 was undetectable. These results are consistent with the observed rapid clearance, 48 h postexposure, of RD01 from the lungs (Fig. 2B) of infected mice.
The only virulence factor definitively shown to be essential for the pathogenicity of B. mallei is an extracellular capsule (3). Mutational analysis of the B. pseudomallei animal pathogen-like TTSS, using in vitro techniques, demonstrated that the TTSS is required for intracellular replication within murine macrophage-like cells (J774.2), escape from endocytic vacuoles, and actin polymerization (13). By creating specific mutations located within the bsaQ and bsaZ genes (Salmonella invA and spaS homologues), this investigation, despite only being able to analyze the organ loads from a single animal for each time point, suggests that TTS plays an essential role in the virulence of B. mallei ATCC 23344 in vivo. Further studies will be needed to identify putative effector molecules and decipher the complex molecular mechanisms associated with this animal pathogen-like TTSS.
Acknowledgments
We thank Melanie Ulrich, William Day, and Katheryn Kenyon for critically reviewing the manuscript; Marilyn England and David Waag for determining the IgG titers; the USAMRIID Aerobiology Division for directing the aerosol challenges; and Lynda Miller, Jennifer and Anthony Bassett, and Ron Lind for their technical assistance.
All research was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals and experiments involving animals and adhered to principles stated in the Guide for the Care and Use of Laboratory Animals (National Research Council [7]). The facility where this research was conducted is fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care International.
Editor: V. J. DiRita
REFERENCES
- 1.Dennis, J. J., and G. J. Zylstra. 1998. Plasposons: modular self-cloning minitransposon derivatives for rapid genetic analysis of gram-negative bacterial genomes. Appl. Environ. Microbiol. 64:2710-2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeShazer, D., and D. M. Waag. New insights into an old disease. In L. Lindler, F. Lebeda, and G. W. Korch (ed.), Biological weapons defense: principles and mechanisms for infectious diseases counter-bioterrorism. The Humana Press, Inc., Totowa, N.J., in press.
- 3.DeShazer, D., D. M. Waag, D. L. Fritz, and D. E. Woods. 2001. Identification of a Burkholderia mallei polysaccharide gene cluster by subtractive hybridization and demonstration that the encoded capsule is an essential virulence determinant. Microb. Pathog. 30:253-269. [DOI] [PubMed] [Google Scholar]
- 4.Hueck, C. J. 1998. Type III protein secretion systems in bacterial pathogens of animals and plants. Microbiol. Mol. Biol. Rev. 62:379-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeddeloh, J. A., D. L. Fritz, D. M. Waag, J. M. Hartings, and G. P. Andrews. 2003. Biodefense-driven murine model of pneumonic melioidosis. Infect. Immun. 71:584-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller, W. R., L. Pannell, L. Cravitz, W. A. Tanner, and T. Rosebury. 1948. Studies on certain biological characteristics of Malleomyces mallei and Malleomyces pseudomallei. II. Virulence and infectivity for animals. J. Bacteriol. 55:127-135. [PMC free article] [PubMed] [Google Scholar]
- 7.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, D.C.
- 8.Parker, M. 1990. Glanders and melioidosis, p. 392-394. In M. T. Parker and L. H. Collier (ed.), Topley & Wilson's principles of bacteriology, virology and immunity, 8th ed. B.C. Decker, Philadelphia, Pa.
- 9.Rainbow, L., C. A. Hart, and C. Winstanley. 2002. Distribution of type III secretion gene clusters in Burkholderia pseudomallei, B. thailandensis and B. mallei. J. Med. Microbiol. 51:374-384. [DOI] [PubMed] [Google Scholar]
- 10.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 11.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 12.Simon, R., U. Priefer, and A. Pühler. 1983. A broad host range mobilization system for in vivo genetic engineering: transposon mutagenesis in gram-negative bacteria. BioTechniques 1:784-791. [Google Scholar]
- 13.Stevens, M. P., M. W. Wood, L. A. Taylor, P. Monaghan, P. Haws, P. W. Jones, T. S. Wallis, and E. E. Galyov. 2002. An Inv/Mxi-Spa-like type III protein secretion system in Burkholderia pseudomallei modulates intracellular behaviour of the pathogen. Mol. Microbiol. 46:649-659. [DOI] [PubMed] [Google Scholar]
- 14.Waag, D., T. Chulay, M. England, and J. Williams. 1995. Validation of an enzyme immunoassay for serodiagnosis of acute Q fever. Eur. J. Clin. Microbiol. Infect. Dis. 14:421-427. [DOI] [PubMed] [Google Scholar]
- 15.Winstanley, C., and C. A. Hart. 2000. Presence of type III secretion genes in Burkholderia pseudomallei correlates with Ara− phenotypes. J. Clin. Microbiol. 38:883-885. [DOI] [PMC free article] [PubMed] [Google Scholar]