Abstract
Blunt abdominal trauma can cause multiple internal injuries. However, these injuries are often difficult to accurately evaluate, particularly in the presence of more obvious external injuries. Computed tomography (CT) imaging is currently used to assess clinically stable patients with blunt abdominal trauma. CT can provide a rapid and accurate appraisal of the abdominal viscera, retroperitoneum and abdominal wall, as well as a limited assessment of the lower thoracic region and bony pelvis. This paper presents examples of various injuries in trauma patients depicted in abdominal CT images. We hope these images provide a resource for radiologists, surgeons and medical officers, as well as a learning tool for medical students.
Keywords: blunt abdominal trauma, computed tomography, injuries, medical sciences
Introduction
The rapid identification of life-threatening injuries and prompt initiation of appropriate care may increase the chance of survival for patients with trauma. However, it is often difficult to accurately clinically evaluate blunt abdominal injuries, which may be masked by other more obvious external injuries. CT imaging is the diagnostic tool of choice for the evaluation of abdominal injury due to blunt trauma in haemodynamically-stable patients (1). CT scans can provide a rapid and accurate appraisal of the abdominal viscera, retroperitoneum and abdominal wall (2). In addition, an abdominal CT scan can assist in the evaluation of coexisting abdominal injuries such as thoracic injuries (3) and unsuspected pelvic and spinal fractures. The ability of CT to perform and produce fast-processing images, such as multiplanar reconstruction (MPR), is important for the accurate interpretation of abnormalities.
A variety of comments, reports and studies on the accuracy and efficacy of CT in the evaluation of blunt abdominal trauma are available in the medical literature; this topic is highly debated and has generated much discussion (4–11). CT has been reported to be valuable for the diagnosis of solid organ injuries and for the detection of active bleeding. The accurate detection of bowel and mesenteric injuries has also improved with the development of thin-section multidetector CT (MDCT) (7). The use of CT to evaluate blunt trauma has influenced current trends in the management of solid organ injuries, prompting a greater focus on non-surgical management (12). Although the decision to surgically intervene is usually based on clinical criteria rather than findings from images (13), CT information often increases diagnostic confidence and decreases rates of unnecessary exploratory laparotomy (14).
In 2008, 92 abdominal CT scans were performed to assess blunt abdominal trauma in a tertiary referral centre (Hospital Tengku Ampuan Afzan (HTAA) in Kuantan, Pahang). In all of these cases, CT scans were performed based on the clinical suspicion of intra-abdominal injury. CT films and each patient’s case notes were followed and retrospectively reviewed. Of these 92 scans, CT images showed injuries involving various organs in 72% of cases; the remaining images did not show any injuries.
All of the scans were performed using a fourrow multislice CT scanner (Somatom Siemens Volume Zoom, Siemens Medical Systems, Erlangen, Germany) with a slice width of 10 mm, a 2.5 mm collimation, a 0.75 s rotation time, a table feed of 15 mm and a 3 mm reconstruction interval. Pre- and post-contrast scans were routinely performed and patients received 2 mL/kg of intravenous contrast medium (Iohexol, 300 mg/mL). Oral contrast was not routinely given. The CT scans were acquired during the portal venous phase approximately 80 seconds after the contrast injection. When necessary, sagittal and coronal images were acquired using the maximum intensity projection (MIP) and MPR techniques. Full thoracic CT scans were not routinely performed when lower thoracic injuries were observed on the abdominal CT.
The various injuries seen on the CT images were grouped and examined based on the injury site and the organs involved.
Haemoperitoneum and the detection of active haemorrhage
CT has high sensitivity and specificity for the detection of blood in the peritoneal cavity (15). Haemoperitoneum starts near the site of injury and spreads along the expected anatomic pathways (16). When the patient is in a supine position, blood from the liver collects in Morison’s pouch and passes down the right paracolic gutter to the pelvis. From the spleen, blood passes via the phrenocolic ligament to the left paracolic gutter and the pelvis (Figure 1a). Blood from a splenic injury also goes to the right upper quadrant (16). Although peritoneal lavage is a sensitive indicator of intraperitoneal haemorrhage, it is unable to detect the source or origin of the bleeding (17). The ‘sentinel clot’ sign indicates adjacent, focal higher attenuation clotted blood as a marker for the organ that is the cause of haemorrhage (16) (Figure 1b). A large amount of blood may collect in the pelvis without much haemoperitoneum seen in the upper abdomen.
Figure 1a:
CT coronal MPR in 18-year-old boy whose motorbike skidded. He had a Grade V splenic injury (images not shown). Splenectomy was performed and about 2 litres of haemoperitoneum was noted intraoperatively. This image demonstrate the possible pathway of blood flow, from the splenic injury to perihepatic (single arrow) regions and passes down the right paracolic gutter (double arrows) to the pelvic cavity (long arrow).
Figure 1b:
CT scan showing haemoperitoneum from liver injury in a 23-year-old man who was involved in a motor vehicle accident (MVA). The ‘sentinel clot’ sign is seen as a high-attenuation collection adjacent to the liver surface (arrow). Liver injury was confirmed surgically with estimated blood loss of 3 litres.
Active haemorrhage can appear as a region of extravasated contrast material and is indicated on a CT scan by an area of high attenuation, with values ranging from 85 to 350 Hounsfield units (HU) (Figure 1c) (18). The site of contrast extravasations noted on CT scans corresponds to the site of bleeding seen on angiography (19).
Figure 1c:
CT scan demonstrating active haemorrhage in a 20-year-old man following MVA. CT shows contrast extravasation (long arrows) and pooling of the extravasated contrast in the dependant area (short arrows). This patient died 2 days after surgery from excessive blood loss.
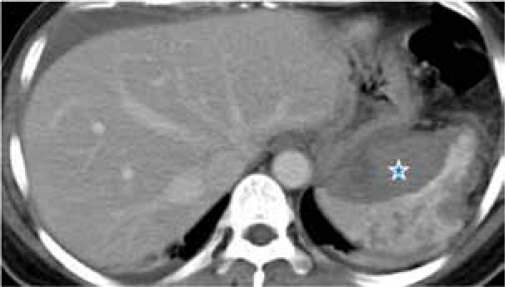
Splenic injury
The spleen is the most frequently injured abdominal organ during blunt abdominal trauma and accounts for up to 45% of all visceral injuries (20). A CT scan following the power injection of intravenous contrast is highly accurate (98%) in diagnosing acute splenic injuries (21). CT scans can detect a variety of splenic injuries, including laceration, a non-perfused region, intra-parenchymal haematoma and subcapcular haematoma (22) (Figures 2a, 2b and 2c). Several CT grading scales for splenic injury are available, but these grading scales have become less clinically important with the increasing popularity of non-surgical management of splenic injury (23–24). These scales are now most important for research and database use.
Figure 2a:
CT scan of a 32-year-old man following MVA showing splenic injury. Subcapsular haematoma (star) appears as a region of low attenuation that compresses the normal splenic parenchyma. Note also multiple lacerations of the spleen. Splenectomy was performed in this patient.
Figure 2b:
CT scan showing splenic laceration in a 13-year-old boy, a pillion rider of a skidded motorbike. Splenic laceration is seen as irregular, linear region of low attenuation (arrows). A 4-cm laceration was identified at the tip of the spleen during surgery and splenectomy was performed.
Figure 2c:
CT scan demonstrating a shattered spleen in a 21-year-old male motorcyclist following MVA. Multiple hypodense areas that connect to the visceral surfaces are shown. This patient had failed conservative treatment and splenectomy was performed 2 days following the trauma which confirmed the CT findings of shattered spleen.
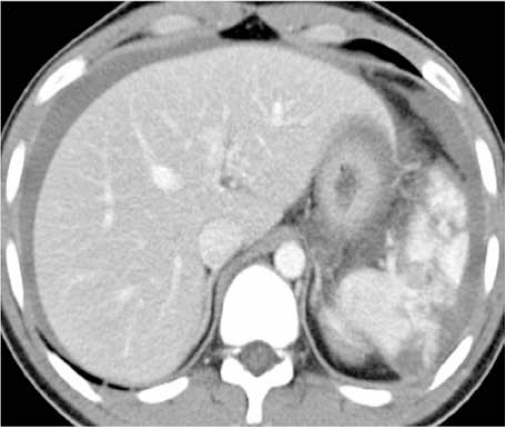
Liver injury
The liver is the second most frequently injured intra-abdominal viscus (2). The worldwide incidence of liver injuries is not known (9), although penetrating injuries (gunshots and stab wounds) account for the majority of liver injuries in North America and South Africa while blunt injuries cause the majority of liver injuries in Europe and Australasia (8).
Although elevated transaminase levels are 100% sensitive and 92.3% specific in predicting hepatic injuries (25), CT is currently the diagnostic modality of choice. CT scans can be used to accurately diagnose parenchymal injuries and exclude surgical lesions such as bowel or pancreatic injuries (26) (Figures 3a and 3b). CT grading criteria have been proposed for liver injuries, but, as with splenic injury, these criteria do no correlate well with the need for surgical intervention or risk of subsequent complications. Surgical analyses have shown that up to 80% of liver injuries in adults and up to 97% of liver injuries in children can be treated without surgery (27).
Figure 3a:
CT scan of liver injury in a 48-year-old man with MVA. CT demonstrates a subcapsular haematoma that appears as a hypodense collection, compressing on the underlying liver parenchyma (arrows).
Figure 3b:
CT scan of liver injury in a 23-year-old man with MVA. Liver laceration is shown on CT as a non-enhancing irregular, linear low attenuation area (arrow) with associated intraparenchymal haematoma (star), which appears as a region of decrease attenuation compared to the rest of the enhanced liver parenchyma. He was managed surgically.
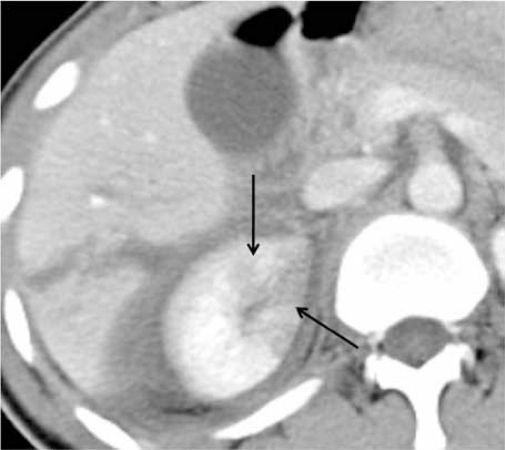
Urinary tract injury
Renal injury occurs in about 10% of cases of abdominal injury and the majority of renal injuries (80% to 90%) result from blunt trauma (28). CT can provide a precise delineation of renal laceration, haematoma and perinephric collection (29); in addition, CT scans can be used to differentiate trivial injuries from those requiring intervention (28) (Figures 4a, 4b and 4c).
Figure 4a:
CT scan of renal injury in a 20-year-old man with MVA. A right contusion that appears as a focal patchy area of decreased enhancement (arrows) was observed on CT. A liver laceration is present adjacent to the kidney. He was managed conservatively with an uneventful recovery.
Figure 4b:
CT of renal laceration in a 32-year-old man with MVA. The right renal lacerations are shown as iregular, linear low attenuation areas within the parenchyma (arrow), which does not involve the collecting systems. He was managed conservatively with an uneventful recovery.
Figure 4c:
CT scan of renal injury in a 17-year-old girl with MVA. Subcapsular haematoma of the right kidney (arrows) appears on CT as a superficial, crescentic, low attnuation area that compresses the adjacent renal parenchyma. She was managed conservatively with uneventful recovery.
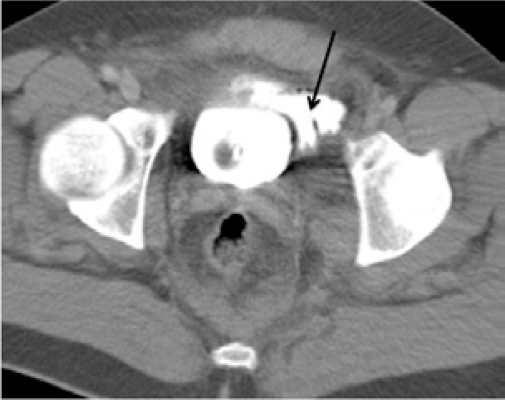
To evaluate bladder injuries, CT cystography with retrograde bladder filling can be added to the routine CT abdominal examination (30). Bladder injuries have characteristic CT cystographic features that can be used to accurately classify injuries and plan treatment (Figures 5a, 5b and 5c). CT differentiates between extraperitoneal and intraperitoneal bladder ruptures and helps determine the management of these injuries.
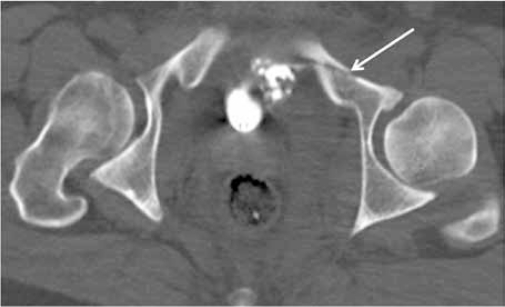
Figure 5a:
CT cystogram of urinary bladder trauma in a 28-year-old man following MVA. There is extravasation of contrast (arrow) in the perivesical fat indicating an extraperitoneal bladder rupture.
Figure 5b:
CT scan showing fracture of the pelvic bone. A lower scan of the same patient in Figure 5a shows the pelvic fracture (arrow). He was managed conservatively with uneventful recovery.
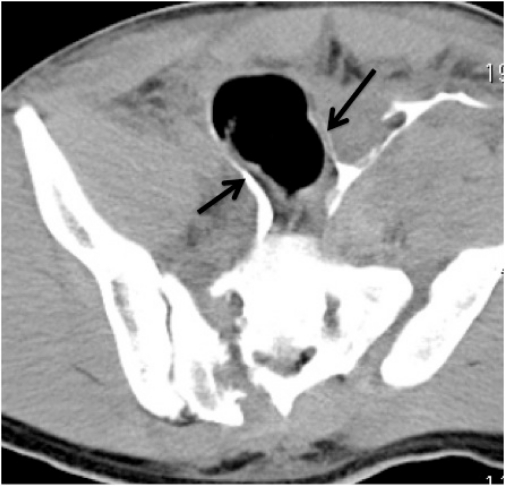
Figure 5c:
CT scan of urinary bladder injury in a 26-year-old man with industrial accident. He fell and was run over by a tractor. This image shows extravasation of contrast from a urinary bladder injury, which outline the bowel loops (arrows). This indicates an intraperitoneal bladder rupture. Note fracture on the right side of the sacrum and diasthesis of left sacroilliac joint. Urinary bladder perforation at 2 sites with about 1 litre of haemoperitoneum was confirmed at surgery.
Pancreatic injury
Pancreatic injury is encountered in only 3% to 12% of all abdominal injuries (31). Pancreatic injury is more common in children and young adults, possibly because these individuals have less retroperitoneal fat to act as a protective buffer (2). The identification of blunt pancreatic injury may be difficult because image findings are often subtle (32). Initial CT findings may be normal, even with pancreatic transaction, because the elastic pancreatic parenchyma resumes its normal contour (33). A repeated CT abdominal scan at 24 to 48 hours can help reveal evolving injuries (2). A delay in diagnosis can often result in recurrent pancreatitis, pseudocyst, fistula or abscess formation (27)(Figure 6).
Figure 6:
CT scan of pancreatic transection in a 9-year-old girl with ‘bicycle-handle’ injury. Diagnosis was delayed and CT scan performed 2 days after the incident showed a total transection of the body of pancreas (arrow). This was later complicated by a pseudocyst formation that required a percutaneous drainage.
Bowel and mesenteric injury
The sensitivity of CT to traumatic bowel injury varies from 69% to 92% and CT is 94%–100% specific for the diagnosis of bowel and mesenteric injuries (10, 34–35). CT findings can include focal bowel wall thickening, mesenteric infiltration, free air, the presence of intraperitoneal fluid without solid organ injuries and extravasated contrast material (10,11,34,36) (Figures 7a and 7b). CT images must be carefully examined to detect injuries and close attention should be paid to scanning techniques and optimal bowel contrast (37).
Figure 7a:
CT scan of perforated bowel in a 26-year-old man with MVA. Note subtle extraluminal air (single white arrows) with focal bowel wall thickening (double white arrows) at the rectosigmoid region that was missed on initial review of the CT images. Also note air pockets in the urinary bladder (black arrows). Urinary bladder perforation and transection at the rectosigmoid junction were detected intraoperatively.
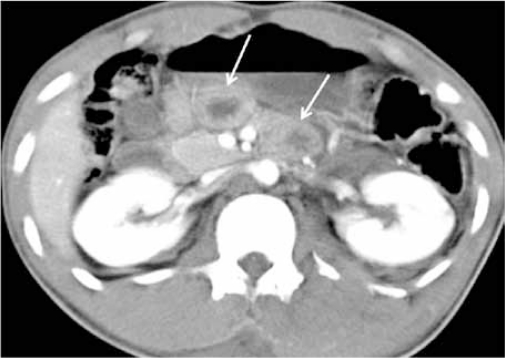
Figure 7b:
CT scan of bowel injury in a 23-year-old lorry driver with MVA. CT scan showed focal small bowel thickening (arrows) but no free air was identified. Small bowel perforation was found intraoperatively.
Injury to the retroperitoneum, spine, abdominal wall and lower chest
Before the use of CT, haemorrhage into the retroperitoneal space was difficult to diagnose (1). CT is valuable in the detection of retroperitoneal and abdominal wall injuries (38) (Figures 8a and 8b). In addition, CT scans can reveal various fractures involving the pelvis (Figures 9a and 9b) and spine (Figure 10) and can offer information about significant unsuspected or underestimated thoracic injuries (Figures 11a and 11b) that are common in patients with blunt abdominal trauma (3,39).
Figure 8a:
CT scan of retroperitoneal injury in in a 23-year-old man with MVA. CT shows an anterior displacement of the right kidney by a retroperitoneal haemorrhage. Both kidneys are otherwise intact. He was managed conservatively with uneventful recovery.
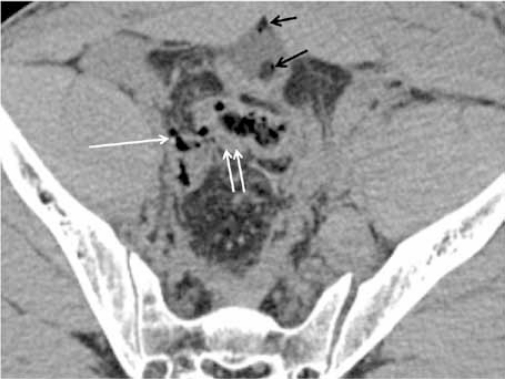
Figure 8b:
CT scan of the same patient in Figure 8a showing the soft tissue injury. There is haematoma and thickening of the abdominal wall (short arrows). The soft tissue injury is extensive involving the right iliopsoas muscle (long arrows) and extends inferiorly to the high region, which compresses the right femoral artery and vein (images are not shown). Note also comminuted fractures of the right iliac bone.
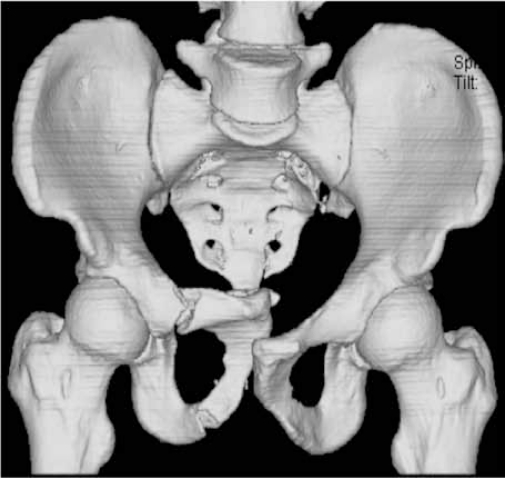
Figure 9a:
CT scan showing fracture of the pelvic bone in a 29-year-old lorry driver following MVA. This volume-rendered CT coronal MPR image clearly depicts fracture of the right public rami with displacement of the fractured fragments.
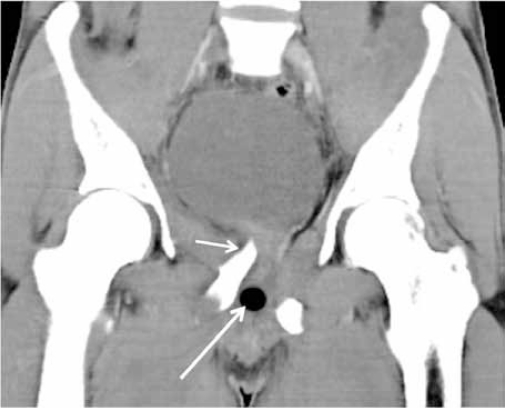
Figure 9b:
CT demonstrating soft tissue injury associated with pelvic fracture. A coronal MPR CT image in soft tissue window of the same patient in Figure 9a showed the fractured fragment (short arrow) compressing at the base of the urinary bladder. Note the mal-positioned Foley’s catheter balloon within the urethra (long arrow). Urethrogram demonstrated a membranous urethral injury.
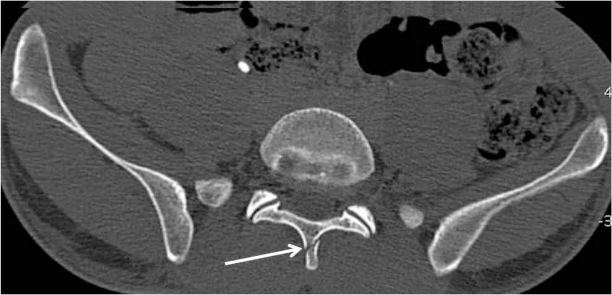
Figure 10:
CT scan of spine fracture in a 29-year-old man who fell from height at the workplace. He complained of pain at the lumbar region. CT scan shows no-intra abdominal injury but demonstrated a subtle of L5 spinous process (arrow), which was missed on the plain radiograph. He was managed conservatively with uneventful recovery.
Figure 11a:
CT of a 15-year-old boy with MVA. The limited evaluation of the lung bases reveals bilateral lung contusions with a left lung laceration (arrow). He sustained a Grade 1 liver injury (not shown) and was managed conservatively.
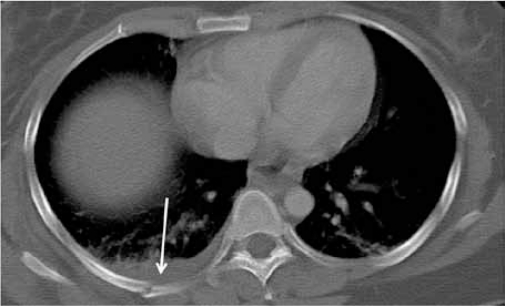
Figure 11b:
CT evaluation of the lower thoracic region in a 25-year-old man with MVA revealed fracture of right posterior rib (arrow) with associated pleural effusion, possibly a haemothorax.
Conclusion
The examination of CT scans is extremely useful for the evaluation of blunt abdominal injuries in haemodynamically-stable patients. CT scans can reveal a wide variety of injuries. In addition, CT examination is fast and widely available. With appropriate scanning protocol, CT can provide good resolution images with MPR.
Acknowledgments
We would like to thank the surgical and radiological staff of HTAA and Kulliyyah of Medicine, IIUM for their continuous effort and assistance in the care and treatment of patients. The data obtained in this pictorial essay is part of a project funded by the IIUM Research Endowment Fund (Type A).
Footnotes
Authors’ contributions
RH and AAA had contributed equally towards drafting and revising the manuscript.
References
- 1.Federle MP, Goldberg HI, Kaiser JA, Moss AA, Jeffrey RB, Mail JC. Evaluation of abdominal trauma by computed tomography. Radiology. 1981;138:637–644. doi: 10.1148/radiology.138.3.6450962. [DOI] [PubMed] [Google Scholar]
- 2.Shuman WP. CT of blunt abdominal trauma. Radiology. 1997;205:297–306. doi: 10.1148/radiology.205.2.9356606. [DOI] [PubMed] [Google Scholar]
- 3.Rhea JT. The frequency and significance of thoracic injuries detected on abdominal CT scans of multiple trauma patients. J Trauma. 1989;29(4):502–505. doi: 10.1097/00005373-198904000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Hoff WS, Holevar M, Nagy KK, Patterson L, Young JS, Arrillaga A, et al. Practice management guidelines for the evaluation of blunt abdominal trauma: the EAST practice management guidelines work group. J Trauma. 2002;53:602–615. doi: 10.1097/00005373-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 5.Ferrada R, Rivera D, Ferrada P. In: Blunt Abdominal Trauma. General Surgery. 2nd ed. Bland KI, Sarr MG, Buchler MW, Csendes A, et al., editors. London: Springer; 2009. pp. 87–96. [Google Scholar]
- 6.Mirvis SE. CT of bowel and mesenteric injury. Nordic Forum Trauma and Emergency Radiology. [Internet]. [updated 2008 May 11; cited 2009 Dec 12]. Available from: www.nordictraumarad.com/Syllabus04/bowelmesentinjury.pdf.
- 7.Fang JF, Wong YC, Lin BC, Hsu YP, Chen MF. Usefulness of Multidetector Computed Tomography for the Initial Assessment of Blunt Abdominal Trauma Patients. World J Surg. 2006;30:176–182. doi: 10.1007/s00268-005-0194-7. [DOI] [PubMed] [Google Scholar]
- 8.Badger SA, Barclay R, Campbell P, Mole DJ, Diamond T. Management of Liver Trauma. World J Surg. 2009;33(12):2522–2537. doi: 10.1007/s00268-009-0215-z. [DOI] [PubMed] [Google Scholar]
- 9.Khan AN, Vadeyar H, MacDonald S, Chandramohan M. Liver. Trauma. [Internet]. [updated 2009 Aug 25; cited 2009 Jun 20]. Available from: www.emedicine.com/radio/topic397.htm.
- 10.Atri M, Hanson JM, Grinblat L, Brofman N, Chughtai T, Tomlinson G. Surgically Importan Bowel and/or Mesenteric Injury in Blunt Trauma: Accuracy of Multidetector CT for Evaluation. Radiology. 2008;249:524–533. doi: 10.1148/radiol.2492072055. [DOI] [PubMed] [Google Scholar]
- 11.Hawkins AE, Mirvis SE. Evaluation of bowel and mesenteric injury: role of multidetector CT. Abdom Imaging. 2003;28:505–514. doi: 10.1007/s00261-002-0079-2. [DOI] [PubMed] [Google Scholar]
- 12.Neish AS, Taylor GA, Lund DP, Atkinson CC. Effect of CT information on the diagnosis and management of acute abdominal injury in children. Radiology. 1998;206:327–331. doi: 10.1148/radiology.206.2.9457182. [DOI] [PubMed] [Google Scholar]
- 13.Ruess L, Sivit CJ, Eichelberger MR, Gotschall CS, Taylor GA. Blunt abdominal trauma in children: impact of CT on operative and nonoperative management. AJR. 1997;169:1011–1014. doi: 10.2214/ajr.169.4.9308453. [DOI] [PubMed] [Google Scholar]
- 14.Taviloglu K, Yanar H. Current Trends in the Management of Blunt Solid Organ Injuries. Eur J Trauma Emerg Surg. 2009;35:90–94. doi: 10.1007/s00068-009-9051-y. [DOI] [PubMed] [Google Scholar]
- 15.Levine CD, Patel UJ, Wachsberg RH, Simmons MZ, Baker SR, Cho KC. CT in patients with blunt abdominal trauma: clinical significance of intraperitoneal fluid detected on a scan with otherwise normal findings. AJR. 1995;164:1381–1385. doi: 10.2214/ajr.164.6.7754877. [DOI] [PubMed] [Google Scholar]
- 16.Lubner M, Menias C, Rucker C. Blood in the Belly: CT Findings of hemoperitoneum. Radiographics. 2007;27:109–125. doi: 10.1148/rg.271065042. [DOI] [PubMed] [Google Scholar]
- 17.Salimi J, Mutamedi M. Detection of intra-abdominal injury in trauma patients: our experience with diagnostic peritoneal lavage. Acta Medica Iranica. 2004;42(2):122–124. [Google Scholar]
- 18.Shanmuganathan K, Mirvis SE, Reanev SM. Pictorial review: CT appearances of contrast medium extravasations associated with injury sustained from blunt abdominal trauma. Clin Radiol. 1995;50:182–187. doi: 10.1016/s0009-9260(05)83054-5. [DOI] [PubMed] [Google Scholar]
- 19.Yao DC, Jeffrey RB, Mirvis SE, Weekes A, Federle MP, Kim C. Using contrast-enhanced helical CT to visualize arterial extravasation after blunt abdominal trauma: incidence and organ distribution. AJR. 2002;178:17–20. doi: 10.2214/ajr.178.1.1780017. [DOI] [PubMed] [Google Scholar]
- 20.Lynn KN, Werder GM, Callaghan RM, Sullivan AN, Jafri ZH, Bloom DA. Pediatric blunt splenic trauma: a comprehensive review. Pediatr Radiol. 2009;39:904–916. doi: 10.1007/s00247-009-1336-0. [DOI] [PubMed] [Google Scholar]
- 21.Brasel KJ, Delisle CM, Olson CJ, Borgstrom DC. Splenic injury: trends in evaluation and management. J Trauma. 1998;4:283–286. doi: 10.1097/00005373-199802000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Jeffrey RB, Laing FC, Federle MP, Goodman PC. Computed tomography of splenic trauma. Radiology. 1981;141:729–732. doi: 10.1148/radiology.141.3.7302229. [DOI] [PubMed] [Google Scholar]
- 23.Umlas SL, Cronan JJ. Splenic trauma: can CT grading systems enable prediction of successful nonsurgical treatment? Radiology. 1991;178:481–487. doi: 10.1148/radiology.178.2.1987612. [DOI] [PubMed] [Google Scholar]
- 24.Shanmugananthan K, Mirvis SE, Kranis RB, Takada T, Scalea TM. Nonsurgical management of blunt splenic injury: use of CT criteria to select patients for splenic arteriography and potential endovascular therapy. Radiology. 2000;217:75–82. doi: 10.1148/radiology.217.1.r00oc0875. [DOI] [PubMed] [Google Scholar]
- 25.Hennes HM, Smith DS, Schneider K, Hegenbarth MA, Duma MA, Jona JZ. Elevated liver transaminase levels in children with blunt abdominal trauma: a predictor of liver injury. Pediatrics. 1990;86:87–90. [PubMed] [Google Scholar]
- 26.Yoon W, Jeong YY, Kim JK, Seo JJ, Lim HS, Shin SS, et al. CT in blunt liver trauma. RadioGraphics. 2005;25:87–104. doi: 10.1148/rg.251045079. [DOI] [PubMed] [Google Scholar]
- 27.Poletti P, Mirvis SE, Shanmuganathan K, Killeen KL, Coldwell D. CT Criteria for management of blunt liver trauma: Correlation with angiographic and surgical findings. Radiology. 2000;216:418–427. doi: 10.1148/radiology.216.2.r00au44418. [DOI] [PubMed] [Google Scholar]
- 28.Kawashima A, Sandler CM, Corl FM, West OC, Tamm EP, Fishman EK, et al. Imaging of Renal Trauma: A Comprehensive Review. RadioGraphics. 2001;21:557–574. doi: 10.1148/radiographics.21.3.g01ma11557. [DOI] [PubMed] [Google Scholar]
- 29.Harris AC, Zwirewich CV, Lyburn ID, Torreggiani WC, Marchinkow LO. CT findings in blunt renal trauma. RadioGraphics. 2001;21:S201–S214. doi: 10.1148/radiographics.21.suppl_1.g01oc07s201. [DOI] [PubMed] [Google Scholar]
- 30.Vaccaro JP, Brody JM. CT cystography in the evaluation of major bladder trauma. RadioGraphics. 2000;20:1373–1381. doi: 10.1148/radiographics.20.5.g00se111373. [DOI] [PubMed] [Google Scholar]
- 31.Gupta A, Stuhlfaut JW, Fleming KW, Lucey BC, Soto JA. Blunt Trauma of the Pancreas and Biliary Tract: A Multimodality Imaging Approach to Diagnosis. RadioGraphics. 2004;24:1381–1395. doi: 10.1148/rg.245045002. [DOI] [PubMed] [Google Scholar]
- 32.Linsenmaier U, Wirth S, Reiser M, Korner M. Diagnosis and classification of pancreatic and duodenal injuries in emergency radiology. RadioGraphics. 2008;28:1591–1601. doi: 10.1148/rg.286085524. [DOI] [PubMed] [Google Scholar]
- 33.Gross JA, Vaughan MW, Johnston BD, Jurkovich G. Handlebar injury causing pancreatic contusion in a pediatric patient. AJR. 2002;179:222. doi: 10.2214/ajr.179.1.1790222. [DOI] [PubMed] [Google Scholar]
- 34.Brofman N, Atri M, Hanson JM, Grinblat L, Chughtai T, Brenneman F. Evaluation of bowel and mesenteric blunt trauma with multidetector CT. RadioGraphics. 2006;26:1119–1131. doi: 10.1148/rg.264055144. [DOI] [PubMed] [Google Scholar]
- 35.Butela S, Federle MP, Chang PJ, Thaete FL, Peterson MS, Dorvault CJ, et al. Performance of CT in detection of bowel injury. AJR. 2001;176:129–135. doi: 10.2214/ajr.176.1.1760129. [DOI] [PubMed] [Google Scholar]
- 36.Strouse PJ, Close BJ, Marshall KW, Cywes R. CT of bowel and mesenteric trauma in children. RadioGraphics. 1999;19:1237–1250. doi: 10.1148/radiographics.19.5.g99se071237. [DOI] [PubMed] [Google Scholar]
- 37.Stuhlfaut JW, Soto JA, Lucey BC, Ulrich A, Rathlev NK, Burke PA. Blunt abdominal trauma: performance of CT without oral contrast material. Radiology. 2004;233:689–694. doi: 10.1148/radiol.2333031972. [DOI] [PubMed] [Google Scholar]
- 38.Daly KP, Ho CP, Perrson DL, Gay SB. Traumatic retroperitoneal injuries: review of multidetector CT findings. RadioGraphics. 2008;28:1571–1580. doi: 10.1148/rg.286075141. [DOI] [PubMed] [Google Scholar]
- 39.Sivit CJ, Taylor GA, Eichelberger MR. Chest injury in children with blunt abdominal trauma: evaluation with CT. Radiology. 1989;171:815–818. doi: 10.1148/radiology.171.3.2717758. [DOI] [PubMed] [Google Scholar]