Abstract
Ketamine can be abused as a recreational drug, and there has been a recent surge in its usage. The effects of ketamine on the urinary system were unknown until the recent publication of a few case reports. Many doctors are still unaware of this new clinical entity, termed ketamine-associated ulcerative cystitis. We report a case that we encountered and discuss the diagnosis and disease management in addition to a review of the literature.
Keywords: cystitis, hydronephrosis, ketamine, medical sciences
Introduction
Ketamine, an anaesthetic drug, has been abused as a recreational drug since the 1980s. Lately, since 2007, there have been reports of urinary system complications arising from the chronic abuse of ketamine. This new clinical entity, termed ketamine-associated ulcerative cystitis, is characterised by symptoms of lower urinary tract irritation related to ketamine use among young people. It is relatively under-diagnosed because many medical professionals are still unaware of this disease. Here, we report a case of ketamine-associated ulcerative cystitis to highlight the diagnosis, pathology and management of this new clinical entity for clinicians who may increasingly encounter this disease in their practice.
Case report
A 21-year-old man presented with a nine-month history of frequent urination, nocturia and suprapubic pain. There was no history of dysuria or fever. Upon further questioning, he admitted that the onset of his symptoms was approximately concurrent with his beginning to use the recreational drug ketamine. He indicated that the drug was taken in white powder form, snorted about twice a week.
Urine analysis showed microscopic haematuria (10 red blood cells per high powered field). His serum urea level was 3.9 mmol/L, and his creatinine level was 79 μmol/L. The acid fast bacilli (AFB) stain for urine was negative. No Mycobacterium tuberculosis was isolated from the urine after 6 weeks of culture. Urine culture also did not grow any other organism.
Initial urinary system ultrasonography showed a small, shrunken right kidney with dilated pelvicalyceal system and distal ureter. This was accompanied by compensatory left kidney hypertrophy and moderate hydronephrosis. The bladder was small in capacity with irregular wall thickening, especially in the right lateral wall. Intravenous pyelography (IVP) showed left hydronephrosis and hydroureter with a non-excreting right kidney (Figure 1a). In the post-voiding pyelogram (Figure 1b), a right vesicoureteric reflux (VUR) and gross dilation of the right ureter was seen. The left collecting system is still visualised in the post-voiding pyelogram due to vesico-ureteric reflux.
Figure 1a:
Intravenous pyelogram showing moderate left hydronephrosis and hydroureter with a nonexcreting right kidney
Figure 1b:
Post-voiding pyelogram showing right vesico-ureteric reflux (VUR) with gross dilatation of right ureter
A diethylenetriamine pentaacetate (DTPA) scan showed that the right kidney was nonfunctioning with severe vesico-ureteric reflux; the left kidney had good function and was not obstructed. The normalised Gate’s glomerular filtration rate was 99 mL/min/1.73 m2. Although the right kidney was non-functioning, the left kidney was not obstructed despite the hydronephrosis, and the renal function was normal. Therefore, ureteric stenting was not performed.
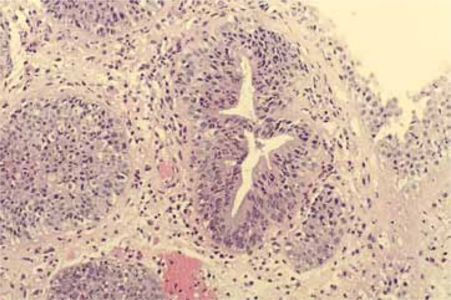
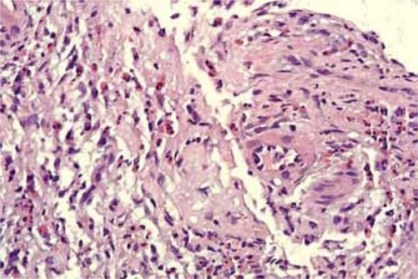
Cystoscopy showed inflamed bladder mucosa with superficial ulcers. Bladder biopsies (Figure 2) revealed urothelial epithelium with nodular proliferation in the lamina propria. The cells lining the cyst were characteristic of multilayered urothelial epithelium. Dense neutrophil infiltration was seen within the epithelium and lamina propria. Some of the fragments were composed of granulation tissue with eosinophil infiltration (Figure 3). No granuloma, dysplasia or malignancy was seen. On the whole, the biopsies showed changes consistent with severe cystitis with a proliferation of von Brunn’s nests.
Figure 2:
Bladder mucosa biopsy showing tissue lined by urothelial epithelium with nodular proliferation in the lamina propria. Dense neutrophil infiltration also seen. (H&E stain, 100x)
Figure 3:
Biopsy of ulcerated bladder mucosa showing eosinophil infiltration. (H&E stain 200x)
After cessation of ketamine and a course of antibiotic for a week, the patient noted that his haematuria and lower urinary tract symptoms had resolved. At three months of follow up, he was asymptomatic, and his renal profile remained normal. He declined further imaging of his urinary system.
Discussion
Ketamine is a derivative of phencyclidine and has been used to induce and maintain general anaesthesia for more than 30 years. Unfortunately, since the 1980s, this drug has been abused as a recreational drug in nightclubs. Its popularity has increased tremendously because it has been erroneously believed to be safer than other recreational drugs. It is available in white powder, tablet or capsule form. When inhaled through the nostril, its effects appear after about ten minutes. When taken orally, its effects appear after about 20 minutes. The psychedelic experience (‘trip’) includes the sensation of light throughout the body, the sensation of being weightless and floating or hovering, colourful visions and out-of body experiences. The bulk of the ‘trip’ lasts about an hour and the effects diminish gradually over another hour (1). This is the experience that addicts crave. However, many recreational users are unaware of the detrimental effects of ketamine on the central nervous system, respiratory and cardiovascular systems.
Recently, there have been reports of unwanted effects of ketamine on the genitourinary system. This new clinical entity has been termed ketamine-associated ulcerative cystitis (2). It is characterised by lower urinary tract symptoms related to ketamine use among young adults. It was first identified in 2007; because then, case reports and series have been published from Canada, Belgium, Hong Kong and Taiwan (2–5).
Currently, little is known about this disease entity. The common presentations of lower urinary tract symptoms include dysuria, frequency, urgency, urge incontinence and painful haematuria. Cystoscopic findings include inflammatory changes, neovascularisation, ulceration and small, contracted bladder. Complications include renal impairment with raised serum urea and creatinine levels. Radiological investigations may show unilateral or bilateral hydronephrosis and hydroureter.
The pathophysiology involved in the damage inflicted by ketamine on the urinary system is not well understood, but several possible mechanisms of injury have been proposed. One is the direct toxic effect of ketamine and its metabolites on the interstitial cells of the bladder. Ketamine may also have direct toxic effects on papillary medullary interstitial cells, causing papillary necrosis with interstitial fibrosis and structural damage that will result in renal impairment. The second proposed mechanism involves microvascular changes in the bladder and kidney causing endothelial cell injury of microvessels. This may lead to either compromised intrinsic microcirculation or decreased microvascular density in the subendothelium. The cystoscopic findings of neovascularisation support this hypothesis. Furthermore, the observed suprapubic pain could be attributed to bladder ischemia during bladder filling. The third hypothesis involves an autoimmune reaction of the bladder urothelium and submucosa triggered by urinary ketamine or ketamine metabolites. This reaction could result in autoimmune-mediated vascular congestion, submucosal oedema and scarring, leading to diminished bladder capacity and poor compliance (6).
The hydronephrosis and hydroureter seen in radiological images could be the result of a longterm decrease in bladder compliance and vesicoureteric reflux. Moreover, papillary necrosis and the resultant migration of the sloughed papilla into the ureters can cause complete ureteric obstruction. Another proposed mechanism for ureteric obstruction is the immunological mediated fibrosis and stricture of the ureters, which may lead to obstructive uropathy (6). Biopsies are non-specific, showing features of chronic cystitis. Histology reveals infiltrations of granulocytes (mostly eosinophils) and mast cells within the bladder tissue (6).
In our patient, the non-obstructive left hydronephrosis and hydroureter is most likely due to vesico-ureteric reflux as a result of decreased bladder compliance. Severe vesicoureteric reflux on the right could have damaged the right kidney, causing it to be non-functional. The left collecting system was non-obstructed despite hydronephrosis and hydroureter and was able to compensate for the non-functioning right kidney. Therefore, serum urea and creatinine levels remained normal.
The treatment of ketamine-associated ulcerative cystitis depends on the severity of the disease. In mild cases, cessation of ketamine use is sufficient for the return of normal bladder activity. In patients with obstructive hydronephrosis, early stenting or nephrostomy would be able to preserve renal function before irreversible damage occurs. In patients with markedly diminished bladder capacity due to bladder fibrosis and contracture, an augmentation or substitution cystoplasty may be indicated. Pentosan polysulphate (2) and intravesical instillation of hyaluronan solution (7) has also been shown to significantly reduce irritative voiding symptoms.
In conclusion, ketamine induced ulcerative cystitis is an emerging disease that is threatening to become a major burden on our healthcare system due to the increasing abuse of ketamine as a recreational drug and its therapeutic use in hospice care to palliate complex pain, in addition to its current usage as an anaesthetic drug. Healthcare workers should be alert to this possible diagnosis when seeing young patients with lower urinary tract symptoms in the absence of a urinary tract infection. A thorough history of ketamine use should be obtained. The mainstay of treatment involves cessation of ketamine usage.
Footnotes
Authors’ contributions
Conception and design: CCKH
Drafting the article: CCKH, HP
Critical revision of the article, final approval of the article: SP, EHG, BCL, MZZ
Provision of study materials or patients: CCKH, HP
References
- 1.Hansen G, Jenson SB, Chandresh L. The Psychotropic Effect of Ketamine. J Psychoact Drugs. 1988;20:419–425. doi: 10.1080/02791072.1988.10472511. [DOI] [PubMed] [Google Scholar]
- 2.Shahani R, Streutker C, Dickson B, Stewart RJ. Ketamine Associated Ulcerative Cystitis: A New Clinical Entity. Urology. 2007;69:810–812. doi: 10.1016/j.urology.2007.01.038. [DOI] [PubMed] [Google Scholar]
- 3.Colebunders B, Van Erps P. Cystitis due to the Use of Ketamine as a Recreational Drug Report. J Med Case Reports. 2008;2:219. doi: 10.1186/1752-1947-2-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chu PS, Kwok SC, Lam KM. ‘Street ketamine’—Associated Bladder Dysfunction: A Report of 10 Cases. Hong Kong Med J. 2007;13:311–313. [PubMed] [Google Scholar]
- 5.Huang YC, Jeng CM, Cheng TC. Ketamine-Associated Ulcerative Cystitis. Tzu Chi Med J. 2008;20(2):144–146. [Google Scholar]
- 6.Chu PSW, Ma WK, Wong SCW, Chu RWH, Cheng CH, Wong S, et al. The Destruction of the Lower Urinary Tract by Ketamine Abuse: A New Syndrome? BJU Int. 2008;102:1612–1622. doi: 10.1111/j.1464-410X.2008.07920.x. [DOI] [PubMed] [Google Scholar]
- 7.Tsai TH, Cha TL, Lin CM, Tsao CW, Tang SH, Chuang FP, et al. Ketamine-Associated Bladder Dysfunction. Int J Urol. 2009;16(10):826–829. doi: 10.1111/j.1442-2042.2009.02361.x. Epub 2009 Jul 29. [DOI] [PubMed] [Google Scholar]