Abstract
Necrotizing fasciitis of the head and neck is a rare, rapidly progressive infection involving the skin, subcutaneous tissue and fascia. We report three cases of necrotizing fasciitis that differ in their presentation and outcome. The first case involves a patient who presented with progressively enlarging anterior neck swelling that was later complicated by dehydration and reduced consciousness. The second case is a patient with neck swelling and ipsilateral otorrhea. The third case concerns a patient with a buccal ulcer complicated by ipsilateral facial swelling. All of them underwent a fasciotomy with wound debridement with the addition of a cortical mastoidectomy in the second case. Two of these patients recovered well. Unfortunately, the third case succumbed to death due to airway compromise and septicaemia. We advocate the importance of eradicating the source of infection followed by frequent, meticulous wound dressing and strict blood sugar control to obtain better outcomes in managing necrotizing fasciitis of the head and neck. However, involvement of the airway carries a grave prognosis despite aggressive treatment.
Keywords: mastoidectomy, necrotizing fasciitis, otitis media, medical sciences
Introduction
Necrotizing fasciitis is an uncommon, life-threatening, single or polymicrobial infection of the soft tissue characterized by widespread necrosis of the skin, subcutaneous fat and fascia. It typically spares the overlying skin and muscle until late in the disease. It has been recognized for centuries with various names, but the current name ‘necrotizing fasciitis’ was first used by Wilson in 1952 (1,2). Necrotizing fasciitis commonly affects the abdominal wall, perineum and extremities (2). This disease rarely involves the head and neck region; and if it occurs, it is usually due to the spread of infection from the teeth or pharynx (3). The incidence of necrotizing fasciitis is 0.40 cases per 100,000 people (4). Diabetes mellitus is known to be one of the comorbidities in the progression of the disease. Necrotizing fasciitis of the head and neck has a particularly high mortality rate due to the proximity of many vital anatomical structures. Known complications of cervical necrotizing fasciitis include airway compromise, arterial and venous occlusion and the extension of infection into the mediastinal and pleural spaces (5). Because of its high mortality rate, prompt and aggressive management with immediate surgical intervention is crucial. Management includes eradication of the source of infection, proper wound dressing, control of blood sugar, and broad spectrum antibiotic coverage. We report three cases of necrotizing fasciitis, which extensively involve the head and neck region with different sources of infection and outcomes.
Case Reports
Case 1
A 65-year-old female presented with a history of progressive neck swelling for one week and dysphagia for 3 days. She also developed recent dysphagia and vomiting. On examination, she was drowsy and dehydrated with poor oral hygiene and no evidence of respiratory compromise. There was necrotic skin on the anterior neck and cellulitis extending to the suprasternal notch. Her blood sugar was high with evidence of metabolic acidosis. She was resuscitated with intravenous fluids and an insulin infusion. Empirical broad spectrum antibiotics (amoxicillin clavulanate, cloxacillin and metronidazole) were started. Computerised tomography scan showed an extensive hypodense collection with air pockets in the left parapharyngeal space, displacing the midline structures. Wound debridement and drainage were performed after stabilizing her medical condition. A Klebsiella species was isolated from the wound. Post-operatively, the wound was cleaned twice daily with hydrogen peroxide and povidone. The wound granulated well after two weeks, and she was discharged home. Subsequently, the wound healed by secondary intention.
Case 2
A 70-year-old Chinese male with underlying diabetes mellitus and hypertension presented with painful progressive left neck swelling for two weeks. The swelling was associated with dysphagia, left otalgia, otorrhea and fever. Clinical examination revealed left neck swelling, extending from the mastoid region (Figure 1). Otoscopy showed features of acute otitis media. His high blood sugar was corrected with insulin infusion. Intravenous ceftriazone and metronidazole were also started. A high resolution computerised tomography scan revealed multiple air pockets within the parotid and submandibular spaces extending medially into the parapharyngeal space and inferiorly along the fascial planes of the posterior triangle. There was also the presence of fluid within the mastoid air cells suggestive of mastoiditis (Figure 2). Cortical mastoidectomy with myringotomy and grommet insertion, including fasciotomy and debridement of the neck, were performed the next day (Figure 3). Intraoperative findings revealed necrotic tissue from the mastoid tip to the supraclavicular region, and the mastoid air cells were filled with granulation tissue. There was no breach of the mastoid cortex. Post-operatively, wound debridement and dressing were performed three times daily with hydrogen peroxide and povidone. Enterobacter and Klebsiella species were isolated. The wound healed by secondary intention after 10 days.
Figure 1:
Necrotizing fasciitis involving the neck with post-auricular inflammation secondary to acute mastoiditis.
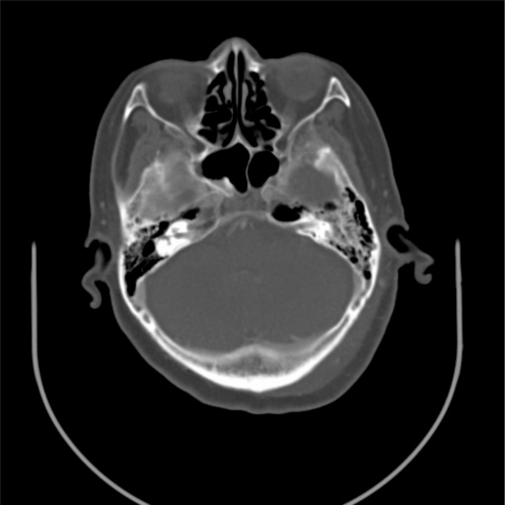
Figure 2:
Computerised tomography scan of the temporal bone showing a soft tissue density within the left mastoid air cells suggestive of mastoiditis.
Figure 3:
Cortical mastoidectomy performed concomitantly with fasciotomy.
Case 3
A 70-year-old Chinese female presented with a three-day history of painful left facial and neck swelling associated with odynophagia. She had a recent hospital admission for uncontrolled diabetes mellitus. Examination revealed a dehydrated patient with an inflamed left hemifacial region extending to the submandibular region and crossing the midline. She also had trismus. Intraoral examination revealed a left buccal ulcer and dental carries affecting the left lower canine and premolars. Ultrasonography of the neck showed an ill-defined hypoechoic collection with air pockets located at the left submandibular and submental regions. She was started on intravenous amoxicillin clavulanate and metronidazole. Wound debridement and fasciotomy were performed the following day. Extensive necrotic tissue extending to the zygoma, posterior triangle and clavicle was encountered. Swab culture and sensitivity isolated Klebsiella and Candida species. Post-operatively, she was haemodynamically unstable with signs of septicaemic shock and was ventilated in the Intensive Care Unit. Despite aggressive wound debridement and dressing, the infection progressed to involve the larynx and mediastinum. Subsequently, she developed septicaemic multi-organ dysfunction. Family members were consulted regarding her poor prognosis, and they requested to bring her home. She then expired at home a few days later.
Discussion
Necrotizing fasciitis of the head and neck region is uncommon (2–3,6). In a large series of 128 cases of necrotizing fasciitis, only five of them involved the head and neck region (1). The severity of necrotizing fasciitis depends on the aetiology, anatomical site, depth of tissue involvement, bacteriology and general condition of the patient. Low immunity plays an important role in determining the initiation, progression and outcome of the disease. Diabetes mellitus is the most common comorbidity in this life-threatening disease. In our series, all patients were elderly and had a history of diabetes mellitus. Another study reported that 58.6% of 75 cases had underlying diabetes mellitus (1). Other risk factors include adrenal insufficiency, liver cirrhosis, cancer, drug abuse, peripheral vascular disease, chronic renal failure, chronic hepatitis and alcoholism (1).
All our patients presented with painful swelling of the head and neck region. Hsiao et al. reported that the most common symptoms were swelling and pain, which occurred in 71.1% and 54.7% of cases, respectively (1). Dysphagia and odynophagia are also common symptoms (6).
The most frequent source of infection for necrotizing fasciitis involving the head and neck region are the teeth or pharynx. Periapical infection of the second or third molar is the usual culprit for cervicofacial infection. This is because the roots of these molars extend below the insertion of the mylohyoid muscle, which is connected to the submandibular space (7). Other sources include the ear, lymph node, cutaneous infection or extension of infection from adjacent structures.
Once the infection has involved the soft tissues, the spread of the disease subsequently follows the fascial planes. The greatest clinical importance of the cervical fascia is that it divides the neck into potential spaces and involves a number of adjoining areas. Although this infection primarily involves the superficial space, other fascial spaces may be involved depending on the stage of the disease and the portal of entry. The parapharyngeal space communicates with all the major fascial spaces. Thus, it may be involved with infection via direct spread from another space or vice versa. Any delay in the treatment of necrotizing fasciitis of the parapharyngeal spaces will expedite the spread of infection to dangerous spaces and subsequently to the mediastinum inferiorly, causing potentially lethal mediastinitis.
In this series, we postulate that the source of infection for the first and third cases were of dental or oropharynx origin. In the first case, the infection involved the superficial fascial plane and spread into the parapharyngeal space. In the third case, we postulate that the source of infection was the left buccal ulcer and dental carries. Submandibular space infections spread readily beneath the anterior belly of the digastric muscles to involve the adjacent spaces, such as the sublingual, lateral pharyngeal or retropharyngeal space. An infection involving the lateral pharyngeal space may extend into the mediastinum along the carotid sheath or through the risky space. This observation emphasizes the clinical importance of the aggressive nature of the infection in necrotizing fasciitis if it is not treated early.
On the other hand, Chua et al. reported the only other case in the literature of cervical necrotizing fasciitis secondary to a mastoid infection (8). However, in our second case, there was no evidence of a subperiosteal abscess unlike in Chua et al. Therefore, we postulate that necrotizing fasciitis in the neck may be secondary to postauricular lymphadenitis.
Computed tomography is useful in the diagnosis of necrotizing fasciitis. It can detect air pockets, which are difficult to see on plain radiographs, and determine the extent of the infection prior to surgery (7). Although beta haemolytic Streptococcus is the most common causative organism, polymicrobial (mixed aerobic and anaerobic) infections also play an important role in spreading the disease (9). The pathogenesis of the aggressive disease is believed to be due to necrosis and separation of the dermal collagen by mucopeptides, which are present in the bacterial cell wall. There is a synergistic effect between the aerobes and anaerobes in the spread of infection. The aerobes provide a favourable environment for anaerobes through oxygen removal (7). On the other hand, the metabolic substance produced by anaerobes is able to enhance the virulence of the aerobes. However, a single pathogen infection by Klebsiella has also been reported (10). Empirical broad spectrum antibiotics should be started without delay while awaiting surgery. This is because most patients require further stabilization before debridement under general anaesthesia.
Early aggressive surgical intervention with eradication of the source of infection is important to achieve good prognosis as demonstrated in our first and second cases. In addition, we also advocate regular and frequent debridement with appropriate wound dressing for better outcomes. Povidone appears to have broad spectrum activity against bacteria and is a common ingredient in topical disinfectants. Hydrogen peroxide is a weak acid with strong oxidizing properties, which can also be used as a disinfectant. We found that this dressing combination allowed adequate wound desloughing in the ward. However, in the third case, this method was unsuccessful because the infection continued to spread to the larynx, leading to mediastinitis, and the patient succumbed to death. Involvement of the larynx and mediastinum carries a higher mortality rate. Those who survive experience prolonged wound healing (6). Death is most often secondary to sepsis, multi-organ failure or respiratory failure (3,6,7).
Hsiao et al. reported five factors that contribute to high mortality, including Aeromonas infection, Vibrio infection, cancer, hypotension and a white blood count greater than 10% (1). In our case series, we postulate that airway involvement is another predictor of mortality.
Conclusion
Early diagnosis with aggressive surgical intervention, eradication of the source of infection, control of blood sugar, broad spectrum antibiotic coverage and appropriate wound dressing are crucial in achieving a favourable outcome for this fatal disease. Mastoidectomy must be performed concomitantly with fasciotomy if there is evidence of mastoiditis either clinically or radiologically. Involvement of the airway may be associated with poor prognosis.
Footnotes
Authors’ contributions
Conception and design: PPSHA
Data collection and assembly: SMM
Drafting the article: SMM, MMB Administrative, technical and/or logistic support: MRMY
Critical revision of the article: MA
References
- 1.Hsiao CT, Weng HH, Yuan YD, Chen CT, Chen IC. Predictors of mortality in patients with necrotizing fasciitis. Am J Emerg Med. 2008;26:170–175. doi: 10.1016/j.ajem.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 2.Bono G, Argo A, Zerbo S, Triolo V, Procaccianti P. Cervical necrotizing fasciitis and descending necrotizing mediastinitis in a patient affected by neglected peritonsillar abscess: a case of medical negligence. J Forensic Leg Med. 2008;15:391–394. doi: 10.1016/j.jflm.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Shindo ML, Nalbone VP, Dougherty WR. Necrotizing fasciitis of the face. Laryngoscope. 1997;107:1071–1079. doi: 10.1097/00005537-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Trent JT, Kirsner RS. Diagnosing necrotizing fasciitis. Adv Skin Wound Care. 2002;15:135–138. doi: 10.1097/00129334-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee AR, Murty GE, Moir AA. Cervical necrotizing fasciitis: a distinct clinicopathological entity? J Laryngol Otol. 1996;110:81–86. doi: 10.1017/s0022215100132797. [DOI] [PubMed] [Google Scholar]
- 6.Lin C, Yeh FL, Lin JT, Ma H, Hwang CH, Shen BH, et al. Necrotizing fasciitis of the head and neck: An analysis of 47 cases. Plast Reconstr Surg. 2001;107:1684–93. doi: 10.1097/00006534-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 7.De Backer T, Bossuyt M, Schoenaers J. Management of necrotizing fasciitis in the neck. J Craniomaxillofac Surg. 1996;24:366–371. doi: 10.1016/s1010-5182(96)80038-2. [DOI] [PubMed] [Google Scholar]
- 8.Chua HK, Chandra Segar CB, Krishnan R, Ho CK. Cervical Necrotizing Fasciitis Consequent to Mastoid infection. Med Malaysia J. 2002;57:104–107. [PubMed] [Google Scholar]
- 9.Bilbault P, Castelain V, Schenck-Dhif M, Schneider F, Charpiot A Life-threatening cervical necrotizing fasciitis after a common dental extraction. Am J Emerg Med. 2008;26:971.e5–7. doi: 10.1016/j.ajem.2008.01.053. [DOI] [PubMed] [Google Scholar]
- 10.Mazita A, Abdullah A, Primuharsa Putra SHA. Cervical Necrotizing Fasciitis due to Klebsiella. Med Malaysia J. 2006;60:657–659. [PubMed] [Google Scholar]