Abstract
The spleen is one of the organs most frequently injured in blunt abdominal trauma. Computed tomography (CT) scanning can accurately detect splenic injury and is currently the imaging modality of choice in assessing clinically stable patients with blunt abdominal trauma. The CT features of spleen injury include lacerations, subcapsular or parenchymal haematomas, active haemorrhage, and vascular injuries. We present a pictorial review of the spectrum of CT findings for blunt splenic injuries. This article will be a useful reference for radiologists and surgeons as CT scan is widely used for the assessment of splenic injuries and contributes to the current trend towards nonsurgical management of this injury.
Keywords: abdomen, blunt injuries, computed tomography, medical imaging, spleen, trauma
Introduction
The spleen is one of the organs most frequently injured in blunt abdominal trauma, accounting for up to 49% of all visceral injuries (1,2). Physical examination and laboratory data are often nonspecific in the diagnosis of splenic injury (3). Contrast-enhanced computed tomography (CT) scanning is currently the diagnostic imaging tool of choice for the assessment of haemodynamically stable patients with spleen injury due to its speed, widespread availability, diagnostic accuracy, and relatively noninvasive nature (4). CT scanning can also provide an accurate appraisal of coexisting abdominal injuries, such as injuries to the retroperitoneum and the abdominal wall, and can exclude the presence of lesions requiring surgery, such as bowel or pancreatic injuries (5). The use of CT scanning has influenced the current trend in the management of spleen injuries towards nonsurgical managements (6,7). Even though the decision to use a surgical intervention is usually based on clinical criteria rather than on imaging findings, data from CT scans frequently increase the diagnostic confidence of surgeons and play an important role in decreasing the frequency of unnecessary exploratory laparotomy (7,8).
Over a 2-year period (2008–2009) in our hospital, there were 44 cases of spleen injury out of 151 cases for which an abdomen CT scan was performed for blunt abdominal trauma. All of these spleen injury cases were retrospectively reviewed. Of these 44 cases, 12 patients had Grade I injury, 9 patients had Grade II injury, 11 patients had Grade III injury, 4 patients had Grade IV injury, and 8 patients had Grade V injury. For all patients, the CT scans were performed using a 4-row multislice Somatom Siemens Volume Zoom CT scanner (Siemens Medical Systems, Erlangen, Germany) with a 10-mm slice width, 2.5-mm collimation, 0.75-s rotation time, 15-mm table feed, and 3-mm reconstruction interval. Pre- and post-contrast scans were routinely performed. Patients received 2 mL/kg of intravenous contrast medium (iohexol 300 mg I/mL). Oral contrast agents were not routinely given. The post-contrast scans were acquired during the portal venous phase, approximately 80 seconds after contrast injection. Multiplanar reconstruction (MPR) images in the sagittal and coronal planes were acquired when necessary. In this article, we present a spectrum of the CT findings for blunt splenic injuries. The spleen injury grading system was applied according to the classification system of the American Association for the Surgery of Trauma (AAST).
CT Features of Blunt Splenic Injury
The major CT features of blunt splenic injuries are lacerations, a non-perfused region, subcapsular and parenchymal haematomas, active haemorrhage, haemoperitoneum and vascular injury. Lacerations and intraparenchymal haematomas or contusions can be clearly observed using contrast-enhanced CT (Figures 1 and 2) (9). Subcapsular haematomas appear as an elliptic collection of low-attenuation blood between the spleen capsules and enhanced splenic parenchyma that causes the indentation or flattening of the underlying spleen margin. Free intraperitoneal blood in the perisplenic space does not cause this effect on the underlying spleen parenchyma (Figure 3) (4).
Figure 1:
Splenic laceration seen on contrast-enhanced computed tomography scan as linear irregular hypodense area (arrow). It was proven intraoperatively in this 15-year-old boy who was injured when his motorcycle skidded. He had an uneventful recovery after splenectomy.
Figure 2:
Parenchymal haematoma (arrow) seen on contrast-enhanced computed tomography scan as focal hypodense area within the enhanced splenic parenchyma with an intact capsule. This patient was injured in a motor vehicle collision and was managed conservatively.
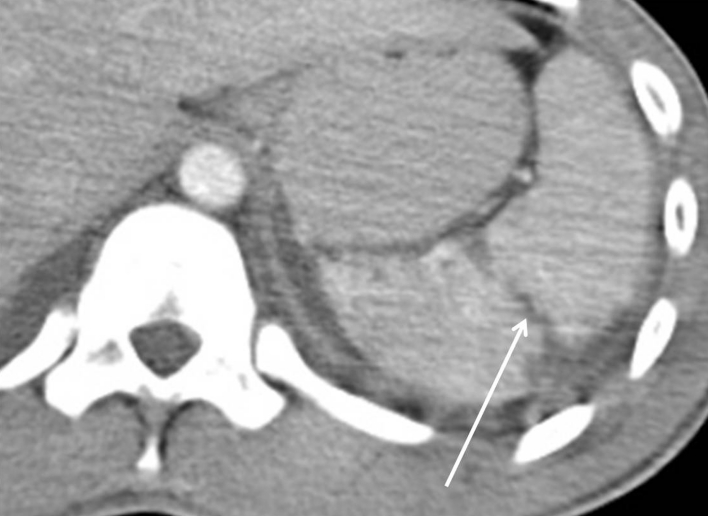
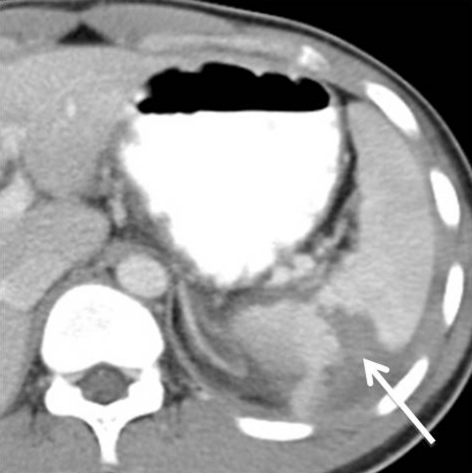
Figure 3a:
Subcapsular haematoma (arrow) seen as perisplenic collection that indents the underlying parenchyma.
Figure 3b:
Perisplenic blood collection (arrow) seen as collection surrounding the spleen with no mass effect to adjacent parenchyma.
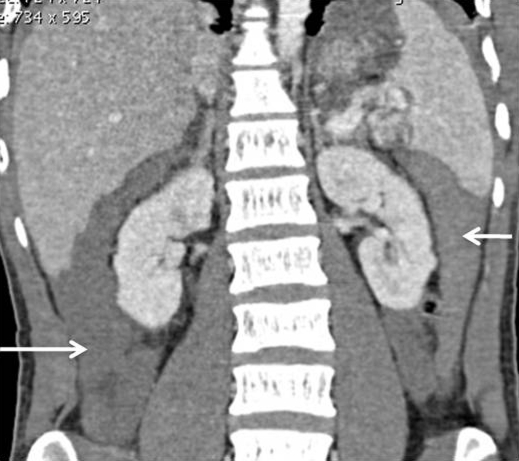
Haemoperitoneum can be accurately detected on a CT scan (10). When a patient is in the supine position, blood from the splenic injury passes via the phrenicocolic ligament to the left paracolic gutter and the pelvis. Blood can also pass into the right upper quadrant (Figure 4). Previously, the volume of haemoperitoneum has been considered to be a predictor of the need for surgery in patients with blunt splenic injury; however, recent reports have detailed the successful nonsurgical management of patients with a large amount of haemoperitoneum (11,12). Active haemorrhage appears as an area of high attenuation on a CT image with Hounsfield units value ranging 85–350 due to extravasated contrast material (Figure 5) (13). Contrast extravasation occurs in approximately 17.7% of patients with splenic injury and is a significant predictor of nonsurgical management failure (2).
Figure 4:
Haemoperitoneum from splenic injury in a 30-year-old man after being assaulted. Computed tomography scan showed massive haemoperitoneum (arrows) due to laceration at splenic hilum. This was confirmed intraoperatively with blood loss of 1L. There was no other intraabdominal injury.
Figure 5:
Active haemorrhage from splenic injury seen as contrast extravasation (arrow) in 18-year-old boy injured after motor vehicle accident. Blood loss of 2L was noted intraoperatively and splenectomy was done for this patient.
CT-based Injury Grading System
Various CT-based grading systems have been developed for the assessment of splenic injury, with the goals of standardising reporting, planning appropriate management, and enabling comparisons between institutions and studies. However, none of the grading systems correlates well with the need for surgical intervention (7,11,14). Recently, a better correlation between a newly proposed CT grading system and surgical intervention was achieved if important CT findings such as active haemorrhage, pseudoaneurysm, arteriovenous fistula, and the severity of haemoperitoneum were included in the grading system (15). Radiologists should be familiar with CT-based grading systems to facilitate research and communications with the surgeons. The most widely used CT grading system for splenic injury in trauma patients is based on the AAST scale (Table 1) (16). The injuries covered in this study were categorised as Grade I (Figures 6 and 7), Grade II (Figures 8–10), Grade III (Figures 11–13), Grade IV (Figure 14), or Grade V (Figures 15 and 16).
Table 1:
Classification of splenic injuries as proposed by the American Association for the Surgery of Trauma (AAST), 1994 revision (16)
| Grade | Injury | Criteria |
|---|---|---|
| I | Haematoma | Subcapsular, <10% of surface area |
| Laceration | Capsular tear, <1-cm parenchymal depth | |
| II | Haematoma | Subcapsular, 10–50% of surface area Intraparenchymal, <5-cm diameter |
| Laceration | 1-cm to 3-cm parenchymal depth that does not involve a trabecular vessel | |
| III | Haematoma | Subcapsular, >50% of surface area or expanding Subcapsular or intraparenchymal, ruptured Intraparenchymal, ≥5-cm diameter or expanding |
| Laceration | >3-cm parenchymal depth or involving trabecular vessels | |
| IV | Laceration | Laceration involving segmental or hilar vessels producing major devascularization of >25% of the spleen |
| V | Laceration | Completely shattered spleen |
| Vascular | Hilar vascular injury that devascularizes the spleen |
Advance one grade for multiple injury (up to Grade III)
Figure 6:
Grade I spleen injury in a 17-year-old girl involved in motor vehicle accident. Coronal reformatted computed tomography showed a capsular tear less than 1 cm in the lower pole (arrow). She was managed conservatively with uneventful recovery. Note the minimal perisplenic collection.
Figure 7:
Grade I spleen injury in a 35-year-old male injured in an industrial accident. Axial contrast-enhanced computed tomography scan showed subcapsular hemorrhage (arrow) less than 10% of surface area. He was managed conservatively and recovered well.
Figure 8:
Grade II splenic injury in a 13-year-old boy injured after a fight. Computed tomography scan showed subcapsular haematoma involving 30%–40% of splenic surface area (arrow). He was managed conservatively with uneventful recovery.
Figure 10:
Grade II splenic injury in a 30-year-old man after being assaulted. Computed tomography scan showed a 2-cm laceration at the hilum (arrow) which was confirmed intraoperatively.
Figure 11:
Grade III splenic injury in a 15-year-old boy injured during football match. Axial contrast-enhanced computed tomography scan showed multiple lacerations and intraparenchymal haematoma (arrow). He was managed conservatively and recovered fully
Figure 13:
Grade III splenic injury in an 18-year-old boy, injured when his motorcycle hit a buffalo. Axial contrast-enhanced computed tomography scan showed a laceration at upper pole (arrow). Intraoperative findings confirmed a 6-cm laceration with haemoperitoneum of about 1L. Splenectomy was performed.
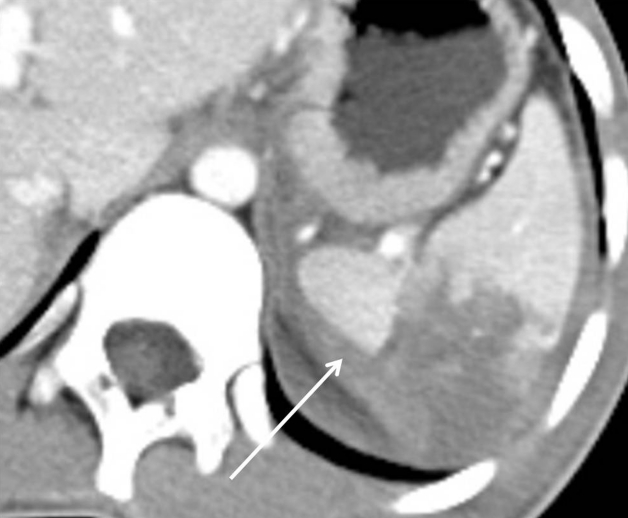
Figure 14:
Grade IV splenic injury in a 17-year-old boy injured in motor vehicle accident. Coronal reformatted computed tomography showed multiple lacerations causing major devascularisation of the spleen. Splenectomy was performed for this patient.
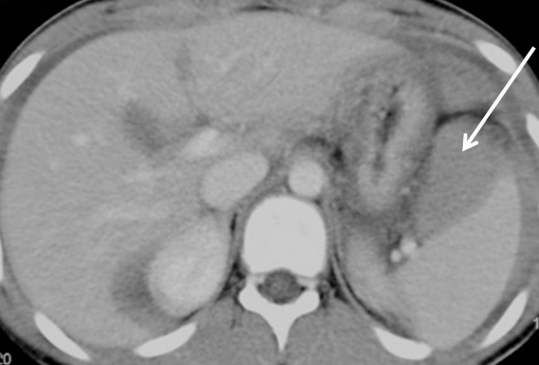
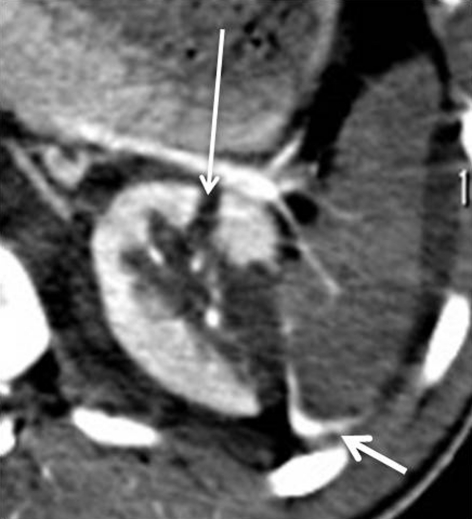
Figure 15:
Grade V splenic injury in an 18-year old man after his motorbike hit a lorry. Axial contrast-enhanced computed tomography scan showed shattered spleen with large-volume haemoperitoneum which was confirmed intraoperatively. Note the focal high attenuation (arrow) due to active hemorrhage. Splenectomy was done for this patient.
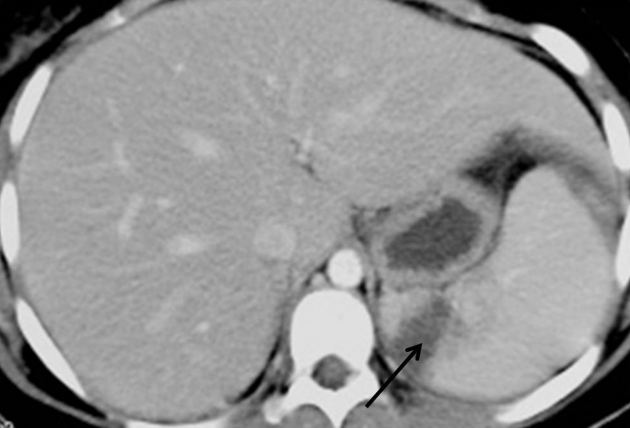
Figure 16:
Grade V splenic injury in a 17-year old boy involved in motor vehicle accident. Axial computed tomography showed non-perfusion of the spleen on this post contrast image. Perisplenic hyperdensity (short arrow) was due to contrast extravasation. He also had left renal injury (long arrow).
CT Features of Delayed Complications
There are few complications related to splenic injury. Delayed complications of splenic injury occur at least 48 hours after the initial injury and include pseudocysts, abscesses, pseudoaneurysms, and delayed rupture (17,18). Delayed splenic rupture has been reported to occur in approximately 5%–6% of nonsurgically managed adults. Post-traumatic pseudocysts were reported in 0.44% of splenic injury patients (18). Splenic abscess formation is a rare complication of blunt trauma (Figure 17). However, as the trend towards nonsurgical management continues, this rare complication may become more prevalent. Post-traumatic splenic artery pseudoaneurysm is also a rare complication that may develop after splenic injury of any grade.
Figure 17:
Splenic abscess as a complication of splenic injury in a 43-year-old man. He presented about 1 week after trivial trauma due to persistent abdominal pain. Computed tomography scan showed intraparenchymal haematoma with multiple air pockets within; this was confirmed intraoperatively.
Role of Follow-up CT in Splenic Injury
Follow-up imaging can provide valuable information about healing patterns (17,19). CT scanning demonstrates apparent complete healing of half of all splenic injuries after 6 weeks. Complete healing of all grades is observed 3 months after injury (20). However, this information has not been shown to significantly influence the management of the injury or affect patient outcome, and thus, follow-up CT scans are not currently recommended (18,21).
Conclusion
A shift towards nonsurgical management of blunt splenic injury in clinically stable trauma patients has been made possible by the widespread use of CT scanning as the initial imaging evaluation. CT scans accurately depict various patterns of splenic injuries and other associated surgically important findings. Knowledge of CT findings of spleen injury is important for both radiologists and surgeons for optimal patient care.
Figure 9:
Grade II splenic injury in a 14-year-old girl injured in motor vehicle accident. Computed tomography scan was done 2 days after the accident demonstrated intraparenchymal haematoma (arrow) less than 4 cm in diameter with no capsular tear. Surgery was performed in this case for continuous blood loss. There were lacerations of left broad ligament with bleeding from branches of left ovarian artery (images not shown). Splenic capsule was intact.
Figure 12:

Grade III spleen injury in a 32-year old man injured in motor vehicle accident. Axial contrast-enhanced computed tomography scan showed multiple intraparenchymal lacerations with subcapsular haematoma (arrow). Splenectomy was done with blood loss of 300 mL.
Acknowledgments
We would like to acknowledge all staff in the of Radiology, Surgery and Emergency Medicine Departments, Hospital Tengku Ampuan Afzan, and Kulliyyah of Medicine, International Islamic University Malaysia (IIUM), for their continuous effort and assistance in the care and treatment of the patients. The data obtained in this pictorial essay is part of a project funded by the IIUM Research Endowment Fund (Type A).
Footnotes
Authors’ Contributions
Conception and design, provision of patients, analysis and interpretation of data, final approval of the article: RH, AAA, ARMR, AS
Drafting of the article, collection and assembly of the data: RH
Critical revision of the article: RH, AAA
References
- 1.Kailidou E, Pikoulis E, Katsiva V, Karavokyros IG, Athanassopoulou A, Papakostantinou I, et al. Contrast-enhanced spiral CT evaluation of blunt abdominal trauma. JBR-BTR. 2005;88(2):61–65. [PubMed] [Google Scholar]
- 2.Yao DC, Jeffrey RB, Jr, Mirvis SE, Weekes A, Federle MP, Kim C, et al. Using contrast-enhanced helical CT to visualize arterial extravasation after blunt abdominal trauma: Incidence and organ distribution. AJR Am J Roentgenol. 2002;178(1):17–20. doi: 10.2214/ajr.178.1.1780017. [DOI] [PubMed] [Google Scholar]
- 3.Hoff WS, Holevar M, Nagy KK, Patterson L, Young JS, Arrillaga A, et al. Practice management guidelines for the evaluation of blunt abdominal trauma: The East practice management guidelines work group. J Trauma. 2002;53(3):602–615. doi: 10.1097/00005373-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 4.Becker CD, Mentha G, Terrier F. Blunt abdominal trauma in adults: Tole of CT in the diagnosis and management of visceral injuries. Part 1: Liver and spleen. Eur Radiol. 1998;8(4):553–562. doi: 10.1007/s003300050433. [DOI] [PubMed] [Google Scholar]
- 5.Fang JF, Wong YC, Lin BC, Hsu YP, Chen MF. Usefulness of multidetector computed tomography for the initial assessment of blunt abdominal trauma patients. World J Surg. 2006;30(2):176–182. doi: 10.1007/s00268-005-0194-7. [DOI] [PubMed] [Google Scholar]
- 6.Taviloglu K, Yanar H. Current trends in the management of blunt solid organ injuries. Eur J Trauma Emerg Surg. 2009;35(2):90–94. doi: 10.1007/s00068-009-9051-y. [DOI] [PubMed] [Google Scholar]
- 7.Schwab CW. Selection of nonoperative management candidates. World J Surg. 2001;25(11):1389–1392. doi: 10.1007/s00268-001-0137-x. [DOI] [PubMed] [Google Scholar]
- 8.Neish AS, Taylor GA, Lund DP, Atkinson CC. Effect of CT information on the diagnosis and management of acute abdominal injury in children. Radiology. 1998;206(2):327–331. doi: 10.1148/radiology.206.2.9457182. [DOI] [PubMed] [Google Scholar]
- 9.Urban BA, Fishman EK. Helical CT of the spleen. AJR Am J Roentgenol. 1998;170(4):997–1003. doi: 10.2214/ajr.170.4.9530050. [DOI] [PubMed] [Google Scholar]
- 10.Federle MP, Jeffrey RB., Jr Hemoperitoneum studied by computed tomography. Radiology. 1983;148(1):187–192. doi: 10.1148/radiology.148.1.6856833. [DOI] [PubMed] [Google Scholar]
- 11.Becker CD, Spring P, Glättli A, Schweizer W. Blunt splenic trauma in adults: can CT findings be used to determine the need for surgery? AJR Am J Roentgenol. 1994;162(2):343–347. doi: 10.2214/ajr.162.2.8310923. [DOI] [PubMed] [Google Scholar]
- 12.Shuman WP. CT of blunt abdominal trauma in adults. Radiology. 1997;205(2):297–306. doi: 10.1148/radiology.205.2.9356606. [DOI] [PubMed] [Google Scholar]
- 13.Lubner M, Menias C, Rucker C, Bhalla S, Peterson Cm, Wang L, et al. Blood in the belly: CT findings of hemoperitoneum. Radiographics. 2007;27(1):109–125. doi: 10.1148/rg.271065042. [DOI] [PubMed] [Google Scholar]
- 14.Umlas SL, Cronan JJ. Splenic trauma: Can CT grading systems enable prediction of successful nonsurgical treatment? Radiology. 1991;178(2):481–487. doi: 10.1148/radiology.178.2.1987612. [DOI] [PubMed] [Google Scholar]
- 15.Marmery H, Shanmuganathan K, Alexander MT, Mirvis SE. Optimization of selection for nonoperative management of blunt splenic injury: Comparison of MDCT grading systems. AJR Am J Roentgenol. 2007;189(6):1421–1427. doi: 10.2214/AJR.07.2152. [DOI] [PubMed] [Google Scholar]
- 16.Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: Spleen and liver (1994 revision) J Trauma. 1995;38(3):323–324. doi: 10.1097/00005373-199503000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Emery KH, Babcock DS, Borgman AS, Garcia VF. Splenic injury diagnosed with CT: US follow-up and healing rate in children and adolescents. Radiology. 1999;212(2):515–518. doi: 10.1148/radiology.212.2.r99au25515. [DOI] [PubMed] [Google Scholar]
- 18.Kristoffersen KW, Mooney DP. Long-term outcome of nonoperative pediatric splenic injury management. J Pediatr Surg. 2007;42(6):1038–1041. doi: 10.1016/j.jpedsurg.2007.01.039. discussion 1041–1032. [DOI] [PubMed] [Google Scholar]
- 19.Uranüs S, Pfeifer J. Nonoperative treatment of blunt splenic injury. World J Surg. 2001;25(11):1405–1407. doi: 10.1007/s00268-001-0141-1. [DOI] [PubMed] [Google Scholar]
- 20.Do HM, Cronan JJ. CT appearance of splenic injuries managed nonoperatively. AJR Am J Roentgenol. 1991;157(4):757–760. doi: 10.2214/ajr.157.4.1892031. [DOI] [PubMed] [Google Scholar]
- 21.Stylianos S. Evidence-based guidelines for resource utilization in children with isolated spleen or liver injury. The APSA Trauma Committee. J Pediatr Surg. 2000;35(2):164–167. doi: 10.1016/s0022-3468(00)90003-4. discussion 167–169. [DOI] [PubMed] [Google Scholar]