Abstract
In a search for novel attenuated vaccine candidates for use against Yersinia pestis, the causative agent of plague, a signature-tagged mutagenesis strategy was used and optimized for a subcutaneously infected mouse model. A library of tagged mutants of the virulent Y. pestis Kimberley53 strain was generated. Screening of 300 mutants through two consecutive cycles resulted in selection of 16 mutant strains that were undetectable in spleens 48 h postinfection. Each of these mutants was evaluated in vivo by assays for competition against the wild-type strain and for virulence following inoculation of 100 CFU (equivalent to 100 50% lethal doses [LD50] of the wild type). A wide spectrum of attenuation was obtained, ranging from avirulent mutants exhibiting competition indices of 10−5 to 10−7 to virulent mutants exhibiting a delay in the mean time to death or mutants indistinguishable from the wild type in the two assays. Characterization of the phenotypes and genotypes of the selected mutants led to identification of virulence-associated genes coding for factors involved in global bacterial physiology (e.g., purH, purK, dnaE, and greA) or for hypothetical polypeptides, as well as for the virulence regulator gene lcrF. One of the avirulent mutant strains (LD50, >107 CFU) was found to be disrupted in the pcm locus, which is presumably involved in the bacterial response to environmental stress. This Kimberley53pcm mutant was superior to the EV76 live vaccine strain because it induced 10- to 100-fold-higher antibody titers to the protective V and F1 antigens and because it conferred efficacious protective immunity.
The three pathogenic Yersinia species, Yersinia pestis, Yersinia pseudotuberculosis, and Yersinia enterocolitica, are closely related but differ in the mode of infection. Both Y. enterocolitica and Y. pseudotuberculosis are fecal-oral pathogens that cause invasive gastrointestinal diseases. On the other hand, infection with Y. pestis, the causative agent of plague, which is transmitted either by an infected-flea bite or as an inhaled aerosol, culminates in a fatal disease. Most of the documented Y. pestis virulence factors are encoded by the 70-kb plasmid common to all three Yersinia pathogenic species (5, 12, 15, 16, 36). Only a few virulence factors that are unique to Y. pestis are known to reside on the strain-specific plasmids (pMT1 and pPCP1) (35). The pMT1 virulence plasmid (19, 26, 34) harbors, in addition to the sequences encoding the known virulence factors murine toxin and fraction 1 (F1) capsular antigen, sequences encoding several hypothetical proteins whose relevance to Y. pestis pathogenesis remains to be determined. Moreover, the recently completed genome sequences of two Y. pestis strains, CO92 and KIM (14, 34), revealed the dynamic nature of the genome, the presence of many pseudogenes, and the existence of genes encoding hypothetical proteins residing in several putative pathogenicity islands, whose effects on Y. pestis pathogenicity remain to be carefully studied (14, 34).
During the last decade, several methods have been developed for screening and identifying bacterial genes involved in conferring the ability to penetrate, colonize, and propagate in host tissues; these methods include in vivo expression technology (27), differential fluorescence induction (43), and signature-tagged mutagenesis (STM) (18). These strategies, particularly STM, led to identification of numerous attenuated mutants of both gram-negative and gram-positive pathogens, which resulted in characterization of potential bacterial virulence-associated genes (11, 29, 31, 40). Most of the genes identified were found to code for proteins involved in cell surface structure, transport, metabolism, transcription regulation, and stress response.
Use of STM recently led to identification of several virulence-associated genes of Y. enterocolitica and Y. pseudotuberculosis, most of which are involved in lipopolysaccharide (LPS) biosynthesis, type III secretion, and nutrient acquisition. Y. enterocolitica attenuated mutants were selected following intraperitoneal inoculation (13, 28), and attenuated Y. pseudotuberculosis strains were identified by using the orogastric or intravenous route of infection (20, 30).
The need for a new vaccine for pneumonic plague is evident given the limited efficacy of the current cellular vaccines, which consist of either the killed virulent 195/P or live EV76 strains (for a review see reference 42). While an efficient and safe live cellular vaccine has not been identified yet, there is an effort to develop alternative subunit vaccines based on various antigens, including F1 and V antigens (1, 17, 42).
Here we describe the use of STM for identification of novel Y. pestis vaccine candidate targets. Selection of attenuated mutants was performed by using an animal model in which mice were infected subcutaneously (s.c.) with the virulent Y. pestis Kimberley53 strain. Among the 300 tagged mutants screened, several highly attenuated strains were identified. One of these, the Kimberley53pcm mutant, may be a potential cellular vaccine candidate and may aid in identification of new protective antigen targets.
MATERIALS AND METHODS
Bacterial strains and growth conditions.
The virulent Y. pestis Kimberley53 strain was used to generate the mutant library for the STM screening. This strain was obtained by passage of the Kimberley strain (4) (originating from Instituto Oswaldo Cruz, Rio de Janeiro, Brazil) in mice (s.c. inoculation and harvesting from the spleen). The s.c. 50% lethal dose (LD50) of this strain in mice (OF1 or ICR outbred mice) is as low as 1 CFU (17; this study). The nonvirulent derivative Kimberley53pCD1−pPCP1− was used as a control representing an established attenuated strain. Y. pestis EV76 (Girard's strain [4]) was used for vaccination experiments. Inoculation of mice with the EV76 strain supplemented with FeSO4 restores the virulent phenotype (5).
Escherichia coli strains CC118λpir and S17-1λpir (18) (a gift from D. Holden, Royal Postgraduate Medical School, London, United Kingdom) were used for tagged-mutant library preparation.
Y. pestis strains were grown at 28°C either overnight in brain heart infusion (BHI) broth (Difco) or for 48 h on BHI agar plates. When Y. pestis bacteria were extracted from organs, the BIN rich selective agar medium (6) was used. Unless otherwise indicated, the antibiotics ampicillin and kanamycin (purchased from Sigma) were each added to the growth medium at a concentration of 100 μg/ml.
Generation of the transposon mutant library.
The tagged pUTmini-Tn5Km2 plasmid library was amplified in E. coli CC118λpir essentially by using the method described by Hensel et al. (18) and modified by Lestrate et al. (24). Plasmids carrying 20 different tags were selected to generate a Y. pestis mutant library consisting of 2,000 mutants. The 20 tags were selected based on their high efficiency for amplification and labeling and the absence of cross-hybridization (24). Each of the tagged plasmids was electroporated into E. coli S17-1λpir and independently transferred to Y. pestis strain Kimberley53 by conjugation. Briefly, donor and acceptor strains were grown on BHI agar for 24 h at 37°C (E. coli) or for 48 h at 28°C (Y. pestis). About 107 cells of the two strains, prewashed with phosphate-buffered saline (PBS), were mixed in 5 ml of 10 mM MgSO4 and filtered through 13-mm-diameter 0.2-μm-pore-size membranes. The filters were incubated on M9 agar (32) at 28°C for 4 h. Transconjugants were recovered in 5 ml of 0.8% NaCl, and 200-μl samples were spread onto BHI agar containing kanamycin (300 μg/ml) and irgasan (0.8 μg/ml; Ciba-Geigey) to select against the donor strain. The plates were incubated at 28°C for 48 h, and transconjugants were screened for sensitivity to ampicillin (indicating a legitimate transposition event). Ampicillin-resistant colonies, as well as poorly growing bacteria, were discarded. About 100 Aps Kmr Y. pestis transconjugants were obtained from each conjugation event. Mutants were assembled in 96-well microtiter dishes.
Tag sequence amplification and hybridization.
Bacterial genomic DNA was extracted with a Wizard genomic kit (Promega). Tag amplification was performed as previously described (18), except that the first PCR products were purified by passage through Bio-Gel P30 columns (Bio-Rad) prior to labeling (24). PCR probe hybridizations were performed as described previously (18), except that aliquots of tagged plasmid DNA carrying the 20 selected tags were fixed onto membranes (plasmid DNA was isolated with a Qiagen plasmid purification kit).
Infection of mice.
Female OF1 outbred mice (5 to 6 weeks old; Charles River Laboratories, Saint Aubin les Elbeuf, France) were used for infection and were handled in accordance with the NIH Guide for the Care and Use of Laboratory Animals and the guidelines of the local commission for animal care. The optimal conditions for STM screening were determined as follows. Y. pestis cells were grown on BHI agar for 48 h at 28°C and were harvested in 2 ml of PBS. Groups of four to six mice were infected s.c. with different doses of bacteria (by using 0.1-ml portions of bacterial suspensions). Bacteria were quantified by serial dilution plating on BHI agar and on BIN selective agar medium (6). Following infection, the bacterial population from the spleen and the liver was monitored by counting CFU (whole organs were homogenized, and bacteria were recovered in PBS, serially diluted in PBS, and then plated on BHI agar). The presence of specific antibodies in the circulation was determined by an enzyme-linked immunosorbent assay (ELISA) (see below). The LD50 was calculated by the method described by Reed and Muench (39).
Screening of the Y. pestis tagged-mutant library was carried out by using pools of 20 differentially tagged mutants (input pools) and infecting six mice with each pool of mutants. Briefly, 20 tagged Y. pestis Kimberley53 mutants were propagated in a 96-well microtiter plate containing BHI broth supplemented with kanamycin (100 μg/ml). After incubation for 48 h at 28°C, the bacteria were diluted 1:40 into a fresh medium and incubated again at 28°C for 48 h, and then mutant cultures were pooled, washed with PBS, and resuspended in PBS to obtain a concentration of approximately 105 CFU/ml (input pool). Six mice were infected s.c. with 0.1 ml of each input pool suspension, and 48 h postinfection the spleens were recovered from three infected mice (the other three mice were monitored for disease development and death). The organs were pooled and homogenized, and the bacteria were extracted, serially diluted in PBS, and then plated onto BHI agar plates supplemented with kanamycin and on BIN agar medium. After incubation at 28°C for 48 h, at least 104 colonies were pooled for genomic DNA preparation.
Competition assays.
Wild-type Y. pestis Kimberley53 or tagged mutants of this strain were grown separately in BHI medium for 48 h. For in vitro competition assays, wild-type strain Kimberley53 and a relevant tagged, kanamycin-resistant mutant were mixed (input ratio, 1:1; total, 104 CFU). The mixed cultures were grown for 48 h, and then aliquots were plated on BHI agar, with and without kanamycin, to allow determination of the output ratio.
For in vivo competition assays, mixtures of the wild-type strain and mutants (input ratio, 1:1; total, 104 CFU) were used to infect mice s.c. (four mice in each assay). Forty-eight hours postinfection bacteria were harvested from spleens, and the output ratio of mutant to wild type was determined by plating preparations on BHI agar plates containing kanamycin and BHI agar plates. The competition index (CI) was defined as the ratio of the output mutant/wild type ratio to the input mutant/wild type ratio.
Colonization and persistence of Y. pestis strains in mouse organs.
The Kimberley53pcm, EV76, and Kimberley53 strains were grown on BHI agar for 48 h at 28°C and were harvested in 2 ml of PBS. Mice were s.c. infected with 106 CFU of each one of the strains. At various times postinfection, mice were sacrificed, and organs (spleens, livers, and lungs) were aseptically removed and homogenized in 2 ml of PBS. Bacteria were quantified by serial dilution plating on BHI agar and on BIN selective agar medium (6).
Immunization and challenge.
Groups of 20 mice were immunized once by s.c injection of a suspension of either the Kimberley53pcm or EV76 strain (0.1 ml). Control mice were given an equal volume of PBS. The presence of specific antibodies in the circulation was determined 46 days postinfection by ELISA (see below). Groups of 10 mice from each immunization group were challenged s.c. with different amounts of the Kimberley53 strain 50 days postimmunization. The survival of mice was monitored daily for 21 days.
Sequencing and identification of transposon insertion site.
A Wizard genomic DNA purification kit (Promega) was used for preparation of bacterial genomic DNA. The identity of the transposon insertion site was determined by the single-primer PCR method (21), with the following modifications. Prior to the first round of amplification, DNA was digested with NcoI, NheI, or SpeI (separately), and then the reaction mixtures were pooled and the DNA was ethanol precipitated. Following the first round of amplification (with the P6U or P7U primers), the PCR products were purified on Micro Bio-Spin P-30 chromatography columns (Bio-Rad), and DNA sequencing was carried out with an ABI PRISM 3100 genetic analyzer and the P6M or P7M primers (21). Usually, a few hundred nucleotides flanking both sides of the inserted kanamycin resistance gene were determined. The insertion mutagenesis position determined was verified by obtaining the expected PCR product by using primers derived from both sides of the inserted kanamycin resistance gene.
Bioinformatic analysis.
Sequence similarity searches were carried out by using Blast (splishpgp module of the SEALS package; National Center for Biotechnology Information [NCBI]) (46) against nonredundant (nr; against NCBI), completed, and unfinished microbial genomes, including Y. pestis (NCBI), Y. enterocolitica (Sanger), and ERGO (Integrated Genomics, Inc.) databases. Translation of the 20 Y. enterocolitica contigs (Sanger) and open reading frame (ORF) assignment were carried out by using the Wimklein module (SEALS package; NCBI) (46). Blast results were tabulated by using the BTAB program (NCBI) and were further parsed by in-house Perl scripts.
Antisera and serological tests.
Mouse anti-F1 and anti-V antigen immunoglobulin G (IgG) antibody titer determinations were performed by an ELISA. The capture ELISA for anti-F1 antigen antibodies titer determination was carried out as previously described (17) by using purified F1 antigen prepared as described by Baker et al. (3). To determine anti-V antigen IgG antibodies by ELISA, microtiter plates were coated with 500 ng of purified glutathione S-transferase-V-antigen fusion protein prepared as described by Leary et al. (23), and twofold dilutions of the mouse sera examined were added to wells and incubated for 1 h at 37°C. For both ELISAs, alkaline phosphatase-labeled rabbit anti-mouse IgG (1/2,000 dilution; Sigma) was used as the second layer. The titers were expressed as the reciprocals of the highest serum dilutions which displayed optical densities at 405 nm that were twofold higher than the values for the normal serum controls.
RESULTS AND DISCUSSION
Kinetics of subcutaneous infection in mice: determination of optimal conditions for screening the tagged-mutant library.
Critical considerations in applying the STM procedure include choosing the infection route and the bacterial dose used for inoculation (defining the input pool), as well as the time point and the target organ for harvesting bacteria during infection and mutant selection (defining the output pool). These parameters are expected to affect the spectrum of potentially attenuated mutants obtained. In addition, a requirement for meaningful screening is to use a large output pool (>104 CFU) to ensure representation of the maximal number of tags in a reproducible manner (18).
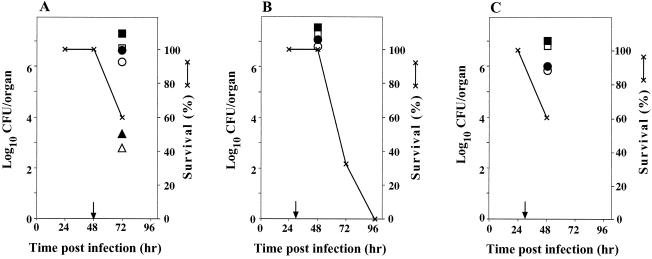
In previous reports the researchers noted the difficulty in establishing consistent measures for monitoring disease onset following s.c. infection of mice with Y. pestis (7, 45). This difficulty probably originates from the rapid dissemination of the pathogen in the host, which leads to death within a few days. In another laboratory, the researchers encountered similar difficulties in establishing a consistent infection model while trying to apply the STM strategy to Y. pestis (33). This emphasizes the need for meticulous monitoring of Y. pestis infection as a prerequisite for productive application of the STM strategy. In order to determine the narrow time window relevant to STM application (namely, after dissemination of the pathogen in the host and prior to death), mice were exposed s.c. to various doses of the virulent Y. pestis Kimberley53 strain. Representative results are shown in Fig. 1. Infected mice were sacrificed either at 48 h postinfection (for high infective doses) or at 72 h postinfection (for the low infective dose), and bacteria were extracted from spleens and livers, plated, and counted.
FIG. 1.
Accumulation of Y. pestis strain Kimberley53 in mice organs following s.c. infection. Groups of eight OF1 female mice were infected s.c. with three different doses of Y. pestis Kimberley53. At different times three mice were sacrificed, and bacteria were extracted from the spleen (solid symbols) and liver (open symbols) of each mouse for counting (by plating on BHI and BIN agar media). (A, B, and C) Survival and bacterial counts in organs following infection with 103, 104, and 105 CFU/mouse, respectively. The arrows indicate times when the first morbidity signs were observed.
Upon infection with 103 CFU/mouse, the first morbidity signs were detected after 48 h, and 40% mortality was observed 72 h postinfection (Fig. 1A). For mice sacrificed at this time there was great variability in the number of bacteria extracted from the liver or spleen (range, 102 to 106 CFU/organ), suggesting that these conditions are unsuitable for STM application. In contrast, upon infection of mice with a high dose of Y. pestis (105 CFU/mouse), the first morbidity signs appeared at about 30 h postinfection, and infection developed rapidly, resulting in high numbers of bacteria in target organs. However, about 40% of the mice were dead at 48 h postinfection (Fig. 1C). Thus, the time window for STM screening under these conditions is too short. More suitable conditions were identified by using an infection dose of 104 CFU/mouse, with which reproducible high counts of bacteria in target organs were achieved prior to death of the mice (Fig. 1B). Based on these observations, the optimal infection conditions chosen for the STM analysis were an infection dose of 104 CFU and sacrifice at 48 h postinfection for recovery of bacteria and the STM screening procedure. The spleen was chosen as the target organ due to the major role of the lymphatic system in Y. pestis spread in the host.
Screening of Y. pestis Kimberley53 tagged mutants by infection of mice and categorization of attenuated strains by their phenotypic properties.
A library of Y. pestis Kimberley53 tagged mutants was constructed (see Materials and Methods). As expected, all mutants tested were found to be Kmr Amps, verifying that there was correct transposition. The randomness of the transposon-mediated integration into the Y. pestis genome was verified by Southern hybridization by using the mini-Tn5Km2 kanamycin resistance gene as a probe; all 10 mutants tested had single insertions, and each insertion was in a different locus (data not shown).
Three hundred tagged mutants were grouped into several input pools, and each pool contained 20 mutant strains carrying different tags. The use of small pools was intended to increase the reproducibility of the infection system and to allow selection of a wide spectrum of attenuated mutants. For quality control purposes each input pool also included a severely attenuated Kimberley53 strain which did not harbor either pCD1 or the pPCP1 virulence plasmid. This mutant was consistently absent from spleens of infected mice under the screening conditions used.
Comparative tag hybridization analysis performed with output pools (collected from spleens of three infected mice) and input pools revealed several mutants which were either totally undetectable in the output pools (65 of 300 mutants) or displayed moderately diminished hybridization intensity (18 of 300 mutants). The 65 mutants that were totally undetectable in pooled spleens were subjected to a second cycle of selection, this time by infection of mice with input pools containing 10 mutants. Following the second cycle of selection, 16 mutants that exhibited pronounced and consistent attenuation (totally undetectable in spleens after two cycles of infection) were chosen for further analysis. This yield of apparently attenuated mutants (about 5%) is in the range of yields obtained during other previously reported STM screening procedures (29, 40).
None of the 16 mutants exhibited defective growth in rich medium in the presence of wild-type bacteria (1:1 ratio), and the in vitro CI values ranged from 0.9 to 1.6. Only one mutant (mutant 7) lost the low-calcium-response function, as observed by growth on Ca2+-deficient medium at 37°C, but this phenomenon could not be attributed to loss of the pCD1 virulence plasmid (data not shown). In agreement with this observation, we found that the insertion responsible for this mutation was located within the lcrF gene (see below).
Table 1 shows the in vivo phenotypic characteristics of the 16 attenuated mutants. Based on their infectivity in mice as monitored by s.c. administration of 100 CFU (equivalent to 100 LD50 of the wild type) and on their ability to compete with the wild type (in in vivo competition assays), the mutants were placed into four groups: (i) nonlethal mutants (mutants 1, 7, and 9), which exhibited very low in vivo CI (10−5 to 10−7), consistent with their severe attenuation (group A); (ii) mutants that exhibited a significant delay in the mean time to death (more than 5 days) (mutants 2 and 8) (group B); (iii) mutants which were indistinguishable from the wild-type strain in terms of inducing mouse mortality but exhibited significantly low CI (CI, <0.3) (mutants 10, 11, 12, 14, and 15) (group C); and (iv) mutants that were indistinguishable from the wild-type strain in terms of causing mice mortality and exhibited CI which were not significantly low (CI, >0.3) (mutants 3, 4, 5, 6, 13, and 16) (group D). It should be noted that mutants in group D, which had relatively high in vivo CI values, were consistently undetectable in the spleens of mice when they were administered as part of an input pool comprising at least 10 differently tagged mutants. This phenomenon reflected the effect of input pool size on the spectrum of attenuated mutants identified by STM. Further analysis and appropriate criteria are needed for better characterization of these presumably slightly attenuated mutants. Notably, about 60% of the 16 selected mutants were found to display significantly low in vivo CI values. This percentage is comparable to data obtained in another STM study in which two cycles of mutant screening were used (13).
TABLE 1.
Phenotypic characterization of 16 selected Y. pestis Kimberley53 attenuated mutants
| Group | Mutant | Survivala | In vivo CIb | Interrupted sequence
|
Annotation or protein | |
|---|---|---|---|---|---|---|
| CO92 | KIM | |||||
| A | 1 | 3/3 | <10−7 | YPO3728 | y0502 | PurH |
| 7 | 3/3 | <10−7 | YPCD1.49 | Y0032 | LcrF | |
| 9 | 3/3 | 3 × 10−5 | YPO3357 | y0832 | Pcm | |
| B | 2 | 0/3 (8) | 0.002 | YPO3077 | y1102 | PurK |
| 8 | 0/3 (6) | 0.08 | YPO3505 | y0679 | GreA | |
| C | 10 | 0/3 (5) | 0.035 | YPMT1.89 | Y1106 | DnaE |
| 12 | 0/3 (4) | 0.054 | YPO2027 | y2285 | Sulfate transporter | |
| 11 | 0/3 (3) | 0.057 | YPO0458-9 | y3719-20 | Intergenic | |
| 14 | 0/3 (4) | 0.15 | YPO3045-6 | y1436-7 | Intergenic | |
| 15 | 0/3 (4) | 0.26 | YPO1179 | y3010 | Conserved hypothetical | |
| D | 5 | 0/3 (5) | 0.52 | YPO3973 | y3857 | Metalloprotease |
| 16 | 0/3 (4) | 0.56 | YPO1994 | y2316 | Hypothetical | |
| 6 | 0/3 (5) | 0.78 | YPO2793 | y1136 | Putative membrane | |
| 13 | 0/3 (4) | 1.07 | YPO2947 | y1537 | Conserved hypothetical | |
| 3 | 0/3 (5) | 1.54 | YPO2471 | y1718 | Putative exported | |
| 4 | 0/3 (5) | 1.87 | YPO1003-4 | y3395-6 | Intergenic | |
OF1 mice were injected s.c. with 100 CFU of each mutant, and survival was monitored for 21 days. The values are the number of mice that survived/number of mice tested. The values in parentheses are the mean time to death (in days). The mean time to death for mice injected with 100 CFU of the Kimberley53 wild-type strain was 4 days.
Mice were infected with a 1:1 mixture of the mutant and the wild type (total, 104 CFU). In vivo CIs were determined based on counts of bacteria extracted from spleens at 48 h postinfection.
The profile of the Y. pestis virulence-associated genes identified in this study was found to differ from that previously reported in STM studies of the other two Yersinia species. Most prominent is the absence of genes involved in LPS biosynthesis, which constituted 15 to 30% of the attenuated Y. pseudotuberculosis and Y. enterocolitica strains, as identified by STM (13, 20, 30). This may have been due to the fact that genes involved in O-antigen biosynthesis are inactivated in Y. pestis (35, 38, 41) and/or to the minor role of LPS in the pathogenicity of Y. pestis. Moreover, this finding may have resulted from the unique route of infection used in this study or the limited representation of the library used for screening.
It should be noted that most of the genes inactivated in the selected attenuated mutants, particularly pcm (mutant 9), greA (mutant 8), and the gene coding for a putative metalloprotease (mutant 5), are implicated here for the first time to be associated with Y. pestis virulence.
Genetic analysis of selected attenuated Kimberley53 mutants.
All 16 insertional mutants were sequenced on both sides of the kanamycin resistance gene insertion (a few hundred nucleotides in each direction). DNA sequences were then analyzed by standard bioinformatic procedures and compared to the complete genomes of both Y. pestis CO92 and KIM, as well as to other bacterial genomes. Three mutants, which were not lethal when 100 CFU was used to inoculate mice, were identified as carrying inactivated purH (mutant 1), lcrF (mutant 7), and pcm (mutant 9) loci. PurH is involved in synthesis of purines (49), a biosynthetic pathway already found to be required for pathogenesis of Y. pestis, as well as other microorganisms (9). This phenomenon reflects the auxotrophy of the pathogens for purines when they infect the host (9). STM analysis of Vibrio cholerae mutants also led to selection of the same pur gene as a virulence-associated gene (10). lcrF codes for a transcriptional activator of the Yop regulon, which is a well-established virulence factor in Yersinia (12). Mutation in virF (an lcrF orthologue) has been shown previously by STM to lead to attenuation in Y. enterocolitica (13).
Disruption of the pcm gene locus generated a highly attenuated strain, indicating that the corresponding gene product, protein-l-isoaspartate O-methyl transferase, may have a major contribution to Y. pestis pathogenesis. The pcm gene is part of a chromosomal set of genes involved in the bacterial response to stress conditions; these genes include surE, pcm, nlpD, and rpoS (22) (ERGO database; Integrated Genomics, Inc.). In E. coli, the pcm gene was shown to be responsible for host survival under stress conditions like stationary-phase growth, heat shock, and osmotic stress (25, 44). Directed mutagenesis of the pcm gene in Y. pestis is under way to validate the specific effect of the gene product on Y. pestis virulence. Use of STM in mice infected intraperitoneally by Y. enterocolitica has shown that disruption of the nlpD gene, located downstream of pcm, has only a subtle effect on Y. enterocolitica virulence (13).
In the second group (which caused a significant delay in the mean time to death of mice infected s.c. with 100 CFU), mutations in the purK (mutant 2) and greA (mutant 8) genes were identified. purK is part of the genetic system responsible for the biochemical pathway of purine synthesis (49), and mutagenesis of this gene in other pathogens has been found to lead to attenuation as well (10). The greA gene codes for a transcription elongation factor and was found to suppress transcriptional arrest of RNA polymerase in E. coli (8). To the best of our knowledge, no previous evidence has associated this gene with bacterial pathogenicity.
Mutants belonging to the third group (indistinguishable from the wild type in terms of the kinetics of mice mortality but exhibiting significantly low in vivo CI) were found to carry insertion mutations in ORFs coding for the DNA polymerase III α subunit (mutant 10), a sulfate transporter (mutant 12), a hypothetical protein (mutant 15), and an insertion in an intergenic sequence (mutants 11 and 14). The inactivated dnaE gene (in mutant 10), coding for the DNA polymerase III α subunit, is located on the pMT1 plasmid, in a region that was found to be identical to the pHCM2 plasmid of Salmonella enterica serovar Typhi (37). This gene and the ORF coding for a sulfate transporter (mutant 12) were described as pseudogenes in the CO92 strain (but not in the KIM strain) due to the presence of an insertion (IS) element in the C-terminal region (34), which created new premature stop codons close to the C terminus. Unlike these IS elements, the insertions of the kanamycin resistance gene in both tagged mutants reported here were found to be located in the N-terminal part of the protein. The fact that the two mutants had significantly low in vivo CI may therefore suggest that the IS element-containing genes are not completely nonfunctional with respect to Y. pestis pathogenesis (note that the Kimberley53 strain, like CO92, also has an IS element at the C terminus of each of these ORFs [data not shown]). The ORF inactivated in mutant 15 is a conserved hypothetical protein which exhibits high sequence similarity to hypothetical proteins of several enteric pathogens, including Y. pseudotuberculosis and Y. enterocolitica. The mutations of mutants 11 and 14 are located in intergenic regions of the Y. pestis CO92 and KIM chromosomes according to the ORF assignment published by Parkhill et al. (34) and Deng. et al. (14), respectively. Mutant 11 carries the insertional mutation within an intergenic sequence located 750 bp upstream of an aspartokinase gene (thrA). Mutant 14 carries the insertion 560 bp downstream of a putative sulfatase modifier gene.
Within the fourth group of mutants we identified a mutational insertion in an ORF coding for a metalloprotease (mutant 5) and another mutation in an intergenic sequence (mutant 4) 500 bp upstream of a putative autotransporter gene (yapH). However, the majority of the mutants in this group carry insertional mutations in ORFs coding for hypothetical proteins (mutants 3, 6, 13, and 16). The ORF disrupted in mutant 13 is located within a potential pathogenicity island (34). Interestingly, the ORF interrupted in mutant 16 was suggested to be involved in Y. pseudotuberculosis YPIII virulence based on an STM study in which a model of intravenously infected mice was used (20). Moreover, this ORF exhibited high sequence similarity (97%) to its orthologue in Y. pestis (20).
Bioinformatic analysis indicated that the ORFs disrupted in mutants 3 and 16 have orthologues only in the closely related organism Y. pseudotuberculosis (on the basis of Blast analysis of the nr databank and other bacterial draft genome sequences [ERGO] available at the time of the present study). Mutants 6 and 13 carry mutations in ORFs having sequence homologues in other enteric pathogens. Mutant 6 carries a mutation in a gene coding for an Hcp-like protein found in Pseudomonas aeruginosa and V. cholerae (47); orthologues were also identified in both Y. pseudotuberculosis and Y. enterocolitica. The function of these genes in the Y. pestis life cycle and pathogenesis warrants a thorough analysis. It should be noted again that all the hypothetical proteins described above are present in both Y. pestis CO92 and KIM.
Evaluation of Y. pestis pcm mutant as a potential vaccine target.
The most severely attenuated mutants carrying inactivated lcrF, purH, or pcm genes may be considered potential targets for vaccine development, yet lcrF and purH appear to be less attractive candidates. Inactivation of lcrF is known to lead to dysfunction of the type III secretion system which is crucial for survival of the pathogen in the host, as well as for expression of the protective V antigen. Y. pestis pur phenotypic mutants were previously found to exhibit various levels of attenuation, correlated with the metabolic position of the mutated gene relative to the generation of IMP (9). Accordingly, the purH mutant was found to be partially attenuated compared to a wild-type Y. pestis strain (s.c. LD50, 4 × 105 CFU). This level of attenuation renders the purH mutant unsuitable for further evaluation as a potential vaccine strain. The pcm mutant, on the other hand, appears to be highly attenuated when it is administered s.c., with LD50s of >107 CFU (the survival ratios were 17/20 and 7/7 for inoculation doses of 107 and 6 × 107 CFU, respectively). Colonization and persistence of the pcm mutant in the spleen and liver were substantially reduced compared to the colonization and persistence of the wild type (Table 2), corroborating the low in vivo CI (Table 1). Upon inoculation of 106 CFU/mouse, the bacteria colonized the spleen and liver at low rates and with low numbers and were cleared within approximately 1 week (Table 2). A total of 18 mice were sacrificed at various times (up to 29 days), and colonization of the spleen was observed only in 2 animals, while colonization of the liver was evident in 5 animals; no spread to the lungs was detected. Essentially, the persistence of the Kimberley53pcm mutant is not very different from that of the EV76 vaccine strain (Table 2).
TABLE 2.
Colonization and persistence of Y. pestis strains in mice organs
| Day postinoculation | Mouse | CFU/organa
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Kimberley53pcm
|
EV76
|
Kimberley53
|
|||||||
| Spleen | Liver | Lungs | Spleen | Liver | Lungs | Spleen | Liver | ||
| 2 | 1 | 2 × 103 | 1 × 103 | <2 | 3 × 103 | 6 × 103 | <2 | 1 × 107 | 1 × 107 |
| 2 | <2 | <2 | <2 | 1 × 102 | 2 × 102 | <2 | 5 × 106 | 1 × 107 | |
| 3 | <2 | <2 | <2 | <2 | <2 | <2 | 6 × 106 | 5 × 106 | |
| 3 | 1 | 5 × 105 | 3 × 104 | <2 | <2 | <2 | <2 | —b | — |
| 2 | <2 | 2 × 103 | <2 | <2 | <2 | <2 | — | — | |
| 3 | <2 | <2 | <2 | <2 | <2 | <2 | — | — | |
| 7 | 1 | <2 | 5 × 105 | <2 | <2 | <2 | <2 | ||
| 2 | <2 | <2 | <2 | <2 | <2 | <2 | |||
| 3 | <2 | <2 | <2 | <2 | <2 | <2 | |||
| 10 | 1 | <2 | <2 | <2 | 1 × 103 | <2 | <2 | ||
| 2 | <2 | <2 | <2 | <2 | <2 | <2 | |||
| 3 | <2 | <2 | <2 | <2 | <2 | <2 | |||
OF1 mice were s.c. inoculated with 106 CFU of either Kimberley53pcm, EV76, or Kimberley53. Animals were sacrificed on days 2, 3, 7, 10, 17, and 29 postinoculation. On days 17 and 29 postinoculation the organs of most sacrificed animals did not contain bacterial counts; the only exception was one animal inoculated with the Kimberley53pcm strain, which on day 17 had a low bacterial count in the liver (300 CFU). The limit of detection was 2 CFU/organ.
—, the mouse was dead on day 3.
To evaluate its potential as a live vaccine, the Kimberley53pcm mutant was compared to the EV76 vaccine by using the mouse model system. The antibody response directed against both F1 capsular antigen and the protective V antigen was monitored in individual animals, and the protective efficacy against challenges with 103 and 105 LD50s of the virulent strain was determined 2 months following inoculation (Table 3). In general, the antibody response to the F1 antigen was greater than that to the V antigen in vaccine strains, which is consistent with a previous report on EV76 vaccination (48). Nevertheless, the results indicate that the antibody response to the F1 and V antigens in mice vaccinated with the Kimberley53pcm mutant is clearly greater than that observed following vaccination with the EV76 strain. Notably, the antibody titer induced by the Kimberley53pcm mutant after low-dose vaccination (105 CFU) was even greater than the titer obtained after administration of a 100-fold-higher vaccination dose of EV76 (Table 4). Furthermore, in a preliminary experiment, in which mice were immunized with high doses (6 × 106 CFU) of the Kimberley53pcm mutant, geometric mean antibody titers as high as 38,000 and 6,300 were achieved for the anti-F1 and anti-V antigens, respectively.
TABLE 3.
Comparison of antibody titers elicited in individual mice vaccinated with either Y. pestis Kimberley53pcm or EV76 strain and survival after lethal challengea
| Kimberley53 challenge dose | Antibody titers and survival after vaccination with:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kimberley53pcm vaccine
|
EV76 vaccine
|
|||||||||||
| 105 CFU
|
106 CFU
|
105 CFU
|
106 CFU
|
|||||||||
| Anti-V antigen | Anti-F1 antigen | Survivalb | Anti-V antigen | Anti-F1 antigen | Survival | Anti-V antigen | Anti-F1 antigen | Survival | Anti-V antigen | Anti-F1 antigen | Survival | |
| 103 LD50 | 100 | 25,000 | + | 6,400 | 100,000 | + | 10 | 320 | − | 320 | 640 | + |
| 200 | 25,000 | + | 2,500 | 50,000 | + | <10 | 160 | + | 40 | 160 | + | |
| 800 | 12,500 | + | 10 | 50,000 | + | <10 | 80 | − | <10 | 160 | + | |
| 100 | 12,500 | + | 20 | 25,000 | + | 10 | 40 | − | 20 | 80 | + | |
| 20 | 12,500 | + | 10 | 25,000 | + | <10 | 20 | − | <10 | 20 | − | |
| 1,600 | 6,400 | + | 6,400 | 12,500 | + | <10 | 10 | − | <10 | 10 | − | |
| 10 | 6,400 | + | 1,600 | 12,500 | + | <10 | 10 | − | 20 | <10 | − | |
| 100 | 3,200 | − | 40 | 12,500 | + | 10 | <10 | − | 20 | <10 | − | |
| 80 | 3,200 | + | 10 | 3,200 | + | <10 | <10 | − | <10 | <10 | − | |
| 20 | 3,200 | + | <10 | <10 | − | <10 | ||||||
| 105 LD50 | 800 | 25,000 | + | 40 | 50,000 | + | <10 | 640 | − | <10 | 320 | + |
| 10 | 25,000 | + | 20 | 50,000 | + | <10 | 320 | + | 10 | 80 | − | |
| 12,500 | 25,000 | + | 800 | 25,000 | + | <10 | 160 | − | 20 | 40 | − | |
| 20 | 12,500 | + | 800 | 12,500 | + | <10 | 20 | − | <10 | 40 | + | |
| 10 | 12,500 | + | 6,400 | 6,400 | + | <10 | 10 | − | 20 | 10 | + | |
| 10 | 12,500 | + | 400 | 6,400 | + | <10 | <10 | − | 10 | 10 | − | |
| 400 | 6,400 | + | 40 | 6,400 | + | <10 | <10 | − | 20 | <10 | − | |
| 400 | 6,400 | + | 1,600 | 3,200 | + | <10 | <10 | − | 10 | <10 | − | |
| 100 | 3,200 | + | 100 | 3,200 | + | <10 | <10 | − | <10 | <10 | − | |
| 10 | 3,200 | + | NDc | ND | + | <10 | <10 | − | <10 | <10 | − | |
Four groups of animals (20 mice each) were vaccinated once s.c. with a dose of 105 or 106 CFU of strain Kimberley 53pcm or EV76. Anti-F1 and anti-V ELISA titers for each animal were determined 46 days following vaccination (titers of <10 were observed in the control group). Animals were challenged, 50 days postvaccination, with the virulent Kimberley 53 strain, and survival of mice was monitored for 21 days. None of the mice in the control group survived (data not shown).
+, survived; −, did not survive.
ND, not done.
TABLE 4.
Vaccine potential of the Y. pestis Kimberley53pcm mutant straina
| Vaccination
|
Antibody responseb
|
Survival after challenge withc:
|
|||
|---|---|---|---|---|---|
| Strain | Dose (CFU) | Anti-F1 antigen | Anti-V antigen | 103 LD50s | 105 LD50s |
| Kimberley53pcm | 105 | 9,248 (2.0) | 93 (7.7) | 10/10 | 9/10 |
| 106 | 15,274 (2.8) | 216 (10.7) | 9/9 | 10/10 | |
| EV76 | 105 | 29 (4.2) | <10 (1) | 1/10 | 1/10 |
| 106 | 28 (3.8) | 15 (2.2) | 4/10 | 3/10 | |
| 107 | 799 (5.9) | 27 (2.7) | 9/10 | 8/10 | |
| Control | <10 | <10 | 0/10 | 0/10 | |
For experimental details see Table 3, footnote a.
The values are geometric mean titers (GeoStDv).
The values are number of mice that survived/number of mice tested.
The protection conferred by the two vaccines correlates well with the serological data, and the Kimberley53pcm mutant appears to be a more efficacious vaccine than EV76. At a vaccination dose as low as 105 CFU, the Kimberley53pcm mutant conferred almost full protection against challenge with a large amount (105 CFU) of a virulent strain, whereas the EV76 strain failed to elicit significant protective immunity at this dose. The EV76 vaccine strain appears to be effective only when a high vaccination dose is used (107 CFU) (Table 4). This difference in the efficacies of the two attenuated strains may be related, at least in part, to the somewhat extended persistence of the Kimberley53pcm mutant in the vaccinated animals (Table 2) or to differences in the mode of the host-bacterium interaction. Table 3 shows that some mice vaccinated with either strain exhibiting low levels of anti-V and anti-F1 antibodies were still protected against a high-level challenge. Equivalent levels of antibodies that are induced by subunit F1 and V vaccines do not protect against a high challenge dose (1). These results may be due to better presentation of the antigens by the live vaccines and/or to involvement of other antigens in the protection process. Further studies, such as serological proteomic analysis in which antisera from animals inoculated with the Kimberley53pcm mutant are used, may allow determination and verification of the existence of such protective antigens, as demonstrated recently for Bacillus anthracis (2).
In conclusion, the results reported here indicate that mutants with mutations in the pcm locus can serve as a platform for generation of a novel live vaccine with more promise for inducing efficacious protective immunity to virulent Y. pestis strains than previously suggested mutants (42).
Acknowledgments
We thank D. Holden and J. J. Letesson for the gift of tagged pUTminiTn5Km2 plasmids. We also thank I. Inbar, G. Friedman, and D. Stein for excellent technical assistance.
Editor: D. L. Burns
REFERENCES
- 1.Anderson G. W., Jr., D. G. Heath, C. R. Bolt, S. L. Welkos, and A. M. Friedlander. 1998. Short- and long-term efficacy of single-dose subunit vaccines against Yersinia pestis in mice. Am. J. Trop. Med. Hyg. 58:793-799. [DOI] [PubMed] [Google Scholar]
- 2.Ariel, N., A. Zvi, K. S. Makarova, T. Chitlaru, E. Elhanany, B. Velan, S. Cohen, A. M. Fridlander, and A. Shafferman. 2003. Genome-based bioinformatic selection of chromosomal Bacillus anthracis putative vaccine candidates coupled with proteomic identification of surface-associated antigens. Infect. Immun. 71:4563-4579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker, E. E., H. Sommer, L. E. Foster, and K. F. Meyer. 1952. Studies on immunization against plague. I. Isolation and characterization of the soluble antigen of Pasteurella pestis. J. Immunol. 68:131-145. [PubMed] [Google Scholar]
- 4.Ben-Gurion, R., and I. Hertman. 1958. Bacteriocin-like material produced by Pasteurella pestis. J. Gen. Microbiol. 19:289-297. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Gurion, R., and A. Shafferman. 1981. Essential virulence determinants of different Yersinia species are carried on a common plasmid. Plasmid 5:183-187. [DOI] [PubMed] [Google Scholar]
- 6.Ber, R., E. Mamroud, M. Aftalion, D. Gur, A. Tidhar, Y. Flashner, and S. Cohen. 2003. Development of an improved selective agar medium for isolation of Yersinia pestis. Appl. Environ. Microbiol. 69:5787-5792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonacorsi, S. P., M. R. Scavizzi, A. Guiyoule, J. H. Amouroux, and E. Carniel. 1994. Assessment of a fluoroquinolone, three β-lactams, two aminoglycosides, and a cycline in treatment of murine Yersinia pestis infection. Antimicrob. Agents Chemother. 38:481-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borukhov, S., A. Polyakov, V. Nikiforov, and A. Goldfarb. 1992. GreA protein: a transcription elongation factor from E. coli. Proc. Natl. Acad. Sci. 89:8899-8902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brubaker, R. R. 1970. Interconversion of purine mononucleotides in Pasteurella pestis. Infect. Immun. 1:446-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiang, S. L., and J. J. Mekalanos. 1998. Use of signature-tagged transposon mutagenesis to identify Vibrio cholerae genes critical for colonization. Mol. Microbiol. 27:797-805. [DOI] [PubMed] [Google Scholar]
- 11.Chiang, S. L., J. J. Mekalanos, and D. W. Holden. 1999. In vivo genetic analysis of bacterial virulence. Annu. Rev. Microbiol. 53:129-154. [DOI] [PubMed] [Google Scholar]
- 12.Cornelis, G. R., A. Boland, A. P. Boyd, C. Geuijen, M. Iriarte, C. Neyt, M. P. Sory, and I. Stainier. 1998. The virulence plasmid of Yersinia, an antihost genome. Microbiol. Mol. Biol. Rev. 62:1315-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Darwin, A. J., and V. L. Miller. 1999. Identification of Yersinia enterocolitica genes affecting survival in an animal host using signature-tagged transposon mutagenesis. Mol. Microbiol. 32:51-62. [DOI] [PubMed] [Google Scholar]
- 14.Deng, W., V. Burland, G. Plunkett III, A. Boutin, G. F. Mayhew, P. Liss, N. T. Perna, D. J. Rose, B. Mau, S. Zhou, D. C. Schwartz, J. D. Fetherston, L. E. Lindler, R. R. Brubaker, G. V. Plano, S. C. Straley, K. A. McDonough, M. L. Nilles, J. S. Matson, F. R. Blattner, and R. D. Perry. 2002. Genome sequence of Yersinia pestis KIM. J. Bacteriol. 184:4601-4611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferber, D. M., and R. R. Brubaker. 1981. Plasmids in Yersinia pestis. Infect. Immun. 31:839-841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gemski, P., J. R. Lazere, and T. Casey. 1980. Plasmids associated with pathogenicity and calcium dependency of Yersinia enterocolitica. Infect. Immun. 27:682-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grosfeld, H., S. Cohen., T. Bino., Y. Flashner., R. Ber, E. Mamroud, C. Kronman, A. Shafferman, and B. Velan. 2003. Effective immunity to Yersinia pestis infection conferred by DNA vaccine coding for derivatives of the F1 capsular antigen. Infect. Immun. 71:374-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hensel, M., J. E. Shea, C. Gleeson, M. D. Jones, E. Dalton, and D. W. Holden. 1995. Simultaneous identification of bacterial virulence genes by negative selection. Science 269:400-403. [DOI] [PubMed] [Google Scholar]
- 19.Hu, P., J. Elliot, P. McCready, E. Skowronski, J. Garnes, A. Kobayashi, R. R. Brubaker, and E. Garcia. 1998. Structural organization of virulence-associated plasmids of Yersinia pestis. J. Bacteriol. 180:5192-5202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karlyshev, A. V., P. C. Oyston, K. Williams, G. C. Clark, R. W. Titball, E. A. Winzeler, and B. W. Wren. 2001. Application of high-density array-based signature-tagged mutagenesis to discover novel Yersinia virulence-associated genes. Infect. Immun. 69:7810-7819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karlyshev, A. V., M. J. Pallen, and B. W. Wren. 2000. Single-primer PCR procedure for rapid identification of transposon insertion sites. BioTechniques 28:1078-1082. [DOI] [PubMed] [Google Scholar]
- 22.Lange, R., and R. Hengge-Aronis. 1994. The nlpD gene is located in an operon with rpoS on the Escherichia coli chromosome and encodes a novel lipoprotein with a potential function in cell wall formation. Mol. Microbiol. 13:733-743. [DOI] [PubMed] [Google Scholar]
- 23.Leary, S. E., D. Williamson, K. F. Griffin, P. Russell, S. M. Eley, and R. W. Titball. 1995. Active immunization with recombinant V antigen from Yersinia pestis protects mice against plague. Infect. Immun. 63:2854-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lestrate, P., R. M. Delrue, I. Danese, C. Didembourg, B. Taminiau, P. Mertens, X. de Bolle, A. Tibor, C. M. Tang, and J. J. Letesson. 2000. Identification and characterization of in vivo attenuated mutants of Brucella melitensis. Mol. Microbiol. 38:543-551. [DOI] [PubMed] [Google Scholar]
- 25.Li, C., and S. Clarke. 1992. A protein methyltransferase specific for altered aspartyl residues is important in Escherichia coli stationary-phase survival and heat-shock resistance. Proc. Natl. Acad. Sci. 89:9885-9889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lindler, L. E., G. V. Plano, V. Burland, G. F. Mayhew, and F. R. Blattner. 1998. Complete DNA sequence and detailed analysis of the Yersinia pestis KIM5 plasmid encoding murine toxin and capsular antigen. Infect. Immun. 66:5731-5742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahan, M. J., J. M. Slauch, and J. J. Mekalanos. 1993. Selection of bacterial virulence genes that are specifically induced in host tissues. Science 259:686-688. [DOI] [PubMed] [Google Scholar]
- 28.Mamroud, E., Y. Flashner, A. Tidhar, R. Ber, D. Gur, M. Aftalion, S. Lazar, B. Velan, A. Shafferman, and S. Cohen. 2003. Evaluation of protective immunity induced by Yersinia enterocolitica type-III secretion system mutants. Adv. Exp. Med. Biol. 529:425-430. [DOI] [PubMed] [Google Scholar]
- 29.Mecsas, J. 2002. Use of signature-tagged mutagenesis in pathogenesis studies. Curr. Opin. Microbiol. 5:33-37. [DOI] [PubMed] [Google Scholar]
- 30.Mecsas, J., I. Bilis, and S. Falkow. 2001. Identification of attenuated Yersinia pseudotuberculosis strains and characterization of an orogastric infection in BALB/c mice on day 5 postinfection by signature-tagged mutagenesis. Infect. Immun. 69:2779-2787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Merrell, D. S., and A. Camilli. 2000. Detection and analysis of gene expression during infection by in vivo expression technology. Philos. Trans. R. Soc. London B Biol. Sci. 355:587-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller, J. H. 1972. Experiments in molecular genetics. Cold Spring Harbor Laboratory, Cold Spring Harbor, N.Y.
- 33.Oyston, P. C., A. V. Karlyshev, B. W. Wren, and R. W. Titball. 2003. Signature-tagged mutagenesis of Yersinia pestis. Adv. Exp. Med. Biol. 529:39-41. [DOI] [PubMed] [Google Scholar]
- 34.Parkhill, J., B. W. Wren, N. R. Thomson, R. W. Titball, M. T. Holden, M. B. Prentice, M. Sebaihia, K. D. James, C. Churcher, K. L. Mungall, S. Baker, D. Basham, S. D. Bentley, K. Brooks, A. M. Cerdeno-Tarraga, T. Chillingworth, A. Cronin, R. M. Davies, P. Davis, G. Dougan, T. Feltwell, N. Hamlin, S. Holroyd, K. Jagels, A. V. Karlyshev, G. Leather, S. Moule, P. C. Oyston, M. Quail, K. Rutherford, M. Simmonds, J. Skelton, K. Stevens, S. Whitehead, and B. G. Barrell. 2001. Genome sequence of Yersinia pestis, the causative agent of plague. Nature 413:523-527. [DOI] [PubMed] [Google Scholar]
- 35.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perry, R. D., S. C. Straley, J. D. Fetherston, D. J. Rose, J. Gregor, and F. R. Blattner. 1998. DNA sequencing and analysis of the low-Ca2+-response plasmid pCD1 of Yersinia pestis KIM5. Infect. Immun. 66:4611-4623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prentice, M. B., K. D. James, J. Parkhill, S. G. Baker, K. Stevens, M. N. Simmonds, K. L. Mungall, C. Churcher, P. C. Oyston, R. W. Titball, B. W. Wren, J. Wain, D. Pickard, T. T. Hien, J. J. Farrar, and G. Dougan. 2001. Yersinia pestis pFra shows biovar-specific differences and recent common ancestry with Salmonella enterica serovar Typhi plasmid. J. Bacteriol. 183:2586-2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prior, J., P. G. Hitchin, E. D. Williamson, A. J. Reason, H. R. Morris, A. Dell, and B. W. Wren. 2001. Characterization of the lipopolysaccharide of Yersinia pestis. Microb. Pathog. 30:49-57. [DOI] [PubMed] [Google Scholar]
- 39.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 40.Shea, J. E., J. D. Santangelo, and R. G. Feldman. 2000. Signature-tagged mutagenesis in the identification of virulence genes in pathogens. Curr. Opin. Microbiol. 3:451-458. [DOI] [PubMed] [Google Scholar]
- 41.Skurnik, M., A. Peippo, and E. Ervela. 2000. Characterization of the O-antigen gene clusters of Yersinia pseudotuberculosis and the cryptic O-antigen gene cluster of Yersinia pestis shows that the plague bacillus is most closely related to and evolved from Y. pseudotuberculosis serotype 0:1b. Mol. Microbiol. 37:316-330. [DOI] [PubMed] [Google Scholar]
- 42.Titball, R. W., and E. D. Williamson. 2001. Vaccination against bubonic and pneumonic plague. Vaccine 19:4175-4184. [DOI] [PubMed] [Google Scholar]
- 43.Valdivia, R. H., and S. Falkow. 1997. Fluorescence-based isolation of bacterial genes expressed within host cells. Science 277:2007-2011. [DOI] [PubMed] [Google Scholar]
- 44.Visick, J. E., H. Cai, and S. Clarke. 1998. The l-isoaspartyl protein repair methyltransferase enhances survival of aging Escherichia coli subjected to secondary environmental stresses. J. Bacteriol. 180:2623-2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walker, D. L., L. E. Foster, T. H. Chen, A. Larson, and K. F. Meyer. 1953. Studies on immunization against plague. V. Multiplication and persistence of virulent and avirulent Pasteurella pestis in mice and guinea pigs. J. Immunol. 70:245-252. [PubMed] [Google Scholar]
- 46.Walker, D. R., and E. V. Koonin. 1997. SEALS: a system for easy analysis of lots of sequences. Proc. Int. Conf. Intell. Syst. Mol. Biol. 5:333-339. [PubMed] [Google Scholar]
- 47.Williams, S. G., L. T. Varcoe, S. R. Attridge, and P. A. Manning. 1996. Vibrio cholerae Hcp, a secreted protein coregulated with HlyA. Infect. Immun. 64:283-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williamson, E. D., S. M. Eley, K. F. Griffin, M. Green, P. Russell, S. E. Leary, P. C. F. Oyston, T. Easterbrook, K. M. Reddin, A. Robinson, and R. W. Titball. 1995. A new improved sub-unit vaccine for plague: the basis of protection. FEMS Immunol. Med. Microbiol. 12:223-230. [DOI] [PubMed] [Google Scholar]
- 49.Zalkin, H., and P. Nygaard. 1996. Biosynthesis of purine nucleotides, p. 561-579. In F. C. Neidhardt, R. Curtiss III, J. L. Ingraham, E. C. C. Lin, K. B. Low, B. Magasanik, W. S. Reznikoff, M. Riley, M. Schaechter, and H. E. Umbarger (ed.), Escherichia coli and Salmonella: cellular and molecular biology, 2nd ed. American Society for Microbiology, Washington, D.C.