Clinical governance requires evidence based standards of clinical relevance to assess performance. The recommended interval between the decision to perform an “emergency” caesarean section and the procedure is 30 minutes1,2 but there is little objective evidence to support this recommendation. We conducted a prospective 12 month study in a large consultant obstetric teaching unit to examine whether the time between the decision to perform a caesarean section to actual delivery affects the success of the delivery.
Participants, methods, and results
Time intervals between a decision to deliver and actual delivery were collected prospectively for all caesarean sections from 1 January 1996 to 31 December 1996. Clinical staff were not aware of the audit since by April 1995 all staff had been required to record these times with the guidelines expecting all deliveries within 30 minutes. Caesarean sections were classified as emergency (decision made during labour because of evolving fetal distress, failing labour, or maternal reasons; 385 deliveries), crash (decision made if impending fetal death or serious maternal compromise anticipated—for example, cord prolapse, placental abruption, or uterine rupture; 24 deliveries), urgent (decision made during the 24 hours before delivery because of deteriorating fetal or maternal health before the onset of labour; 67 deliveries), pre-empted (decision made more than 24 hours before the onset of spontaneous labour or membrane rupture; 57 deliveries), or elective (decision made more than 24 hours before delivery; 368 deliveries).
Fetal distress was the primary clinical indication for intrapartum section if it was documented in the clinical records; if fetal distress was not documented, it was assumed to be absent. “Distress” during pregnancy was determined using various fetal diagnostic tests.
During the study period babies were delivered to 5846 mothers. Delivery was by caesarean section in 901 (15.4%) cases, with decision times available for 415 (77.8%) of the 533 non-elective deliveries and cord arterial pH values available for 490 (91.9%). Maternal age, parity, and gestation were similar for the 159 deliveries with fetal distress and the 374 deliveries without fetal distress.
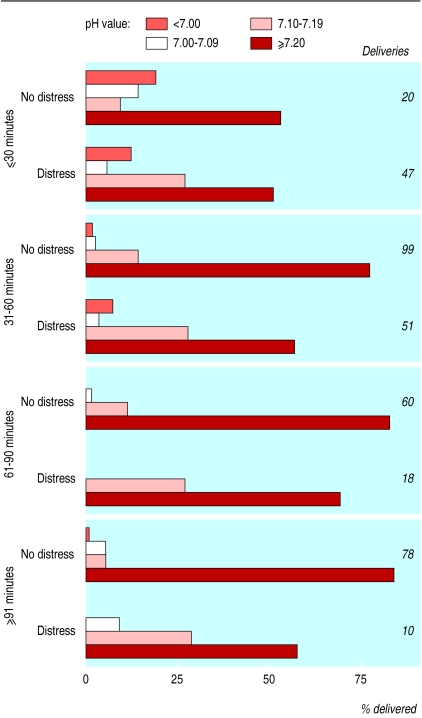
The figure shows the relation between the intervals from decision to delivery, with and without fetal distress, and the cord arterial pH values. The time interval with fetal distress (mean 42.9 (SD 24.1) min; median 35 min) was significantly shorter than without distress (71.1 (42.3) min; P<0.0001, Student's t test) and showed lower cord arterial pH values (7.20 (0.09) v 7.24 (0.09); P=0.0004). Overall, as time between decision and delivery lengthened, there was a trend towards less acidaemia. For all emergency caesarean sections there was a trend towards shorter time intervals for mothers in more advanced labour, but no trend in levels of acidaemia. General anaesthesia rather than regional anaesthesia resulted in shorter time intervals for fetal distress (22.6 (14.6) min v 50.0 (23.0) min; P<0.001). The time of day of delivery, the day of the week of delivery, and the seniority of the surgeon were not related to the time interval whether fetal distress was present or not.
Comment
In 1996, we succeeded in delivering fewer than 50% of the babies in 30 minutes despite a positive attempt to achieve this; our performance for delivery with fetal distress was similar to that reported from our unit for 1989 (median time 34 minutes).3 Possible explanations for this lack of improvement include fewer staff, increased caesarean section workload, increasing use of regional anaesthesia, and reduced experience of obstetric staff.
The trend of improved cord arterial pH values with more prolonged delivery times with and without fetal distress is important. It is hard to explain this trend, especially in the case of deliveries without fetal distress, although we found a similar trend with assisted vaginal vertex deliveries for fetal distress.4 The anxiety for the patient generated by the decision for caesarean section may provoke increased maternal catecholamine release that initially causes reduced perfusion of the placental bed and gas exchange, with temporary fetal acidosis. Cord pH values may not be a reliable assessment of fetal or neonatal wellbeing nor a good predictor of long term neurological outcome5 but we question the benefit and wisdom of aiming to achieve delivery in all cases within 30 minutes.
Figure.
Relation between cord arterial pH and decision to delivery interval for 126 caesarean sections performed because of fetal distress and 257 performed without fetal distress
Acknowledgments
We thank Mrs Maggie Jefferies and the maternity records coding staff who provided a crosscheck to confirm complete collection of data.
Editorial by James Papers p 1330
Footnotes
Funding: None declared.
Competing interests: None declared.
References
- 1.Hannah WJ, Baskett TJ, Chance GW, Hamilton EF, Huchcroft S, King JF, et al. Indications for cesarean section: final statement of the panel of the National Consensus Conference on Aspects of Cesarean Birth. Can Med Assoc J. 1986;134:1348–1352. [PMC free article] [PubMed] [Google Scholar]
- 2.Confidential Enquiry into Stillbirths and Deaths in Infancy. 7th Annual Report. London: Maternal & Child Health Research Consortium; 2000. pp. 41–52. [Google Scholar]
- 3.Dunphy BC, Robinson JN, Sheil OM, Nicholls JSD, Gillmer M. Caesarean section for fetal distress, the interval from decision to delivery, and the relative risk of poor neonatal condition. J Obstet Gynaecol. 1991;11:241–244. [Google Scholar]
- 4.Okunwobi-Smith Y, Cooke IE, MacKenzie IZ. Decision to delivery intervals for assisted vaginal vertex delivery. Br J Obstet Gynaecol. 2000;107:467–471. doi: 10.1111/j.1471-0528.2000.tb13263.x. [DOI] [PubMed] [Google Scholar]
- 5.Dennis J, Johnson A, Mutch L, Yudkin P, Johnson P. Acid-base status at birth and neurodevelopment outcome at four and one-half years. Am J Obstet Gynecol. 1989;161:213–220. doi: 10.1016/0002-9378(89)90269-x. [DOI] [PubMed] [Google Scholar]