Abstract
An enzyme immunoassay (EIA)—the commercially available Platelia Candida antigen test—developed for the diagnosis of systemic candidiasis is based on the detection of α-linked oligomannose residues (α-Man) released from Candida cells into the serum. This test has good specificity but has to be repeated frequently because of the rapid clearance of detectable mannanemia. We have developed a second EIA based on detection of beta-linked oligomannoses (β-Man), since β-Man are linked to different Candida molecules and interact differently with the host immune system and endogenous lectins and should therefore present different kinetics of serum clearance. In a guinea pig model of Candida albicans systemic infection, the relative amounts of detectable α- and β-Man differed considerably according to the virulence of the strain, the infecting dose, and the time after challenge that serum samples were drawn. Detection of α-Man was more sensitive per serum sample than that of β-Man, and the sensitivity for the combination reached 90%. The same tests were applied to 90 sera from 26 patients selected retrospectively for having been infected with the most-pathogenic Candida species: C. albicans (19), C. tropicalis (4), and C. glabrata (3). A total of 22 patients had positive antigenemia, 4 had α-mannanemia, 4 had β-mannanemia, and 14 showed the presence of both. For the patients showing the presence of both forms of mannanemia, the use of both tests enhanced the duration of the detection of mannanemia. Mannanemia was correlated with early clinical symptoms and isolation of Candida in culture, which occurred in 55% of the patients at an average of 4.7 days after the first positive mannanemia test result. A combination of the two tests had a cumulated specificity of 95%, and positive and negative predictive values were 79 and 97%, respectively. These findings provide evidence for different kinetics of β- and α-Man circulation during experimental and human candidiasis and suggest the joint detection of both types of epitopes as a rational approach contributing to increases in the sensitivity and earliness of diagnosis.
Systemic infections caused by Candida species are an increasing problem in clinical practice. Depending on the medical specialty, Candida species are the fourth or fifth most commonly recovered pathogens in blood cultures (27), with attributable mortality rates for candidemia of 40 to 60% (28, 41). The increasing incidence of systemic candidiasis and high mortality rates has been accompanied by escalating costs of prophylactic, preemptive, and empirical antifungal therapy (6, 7). These medical and economic problems are related to difficulties in establishing an early and specific diagnosis of infection (30, 31). The detection of several Candida-derived molecules in the serum samples of patients has been reported to be of diagnostic value. These molecules include metabolites (29, 43), proteins (25), nucleic acids (8, 22), and polysaccharides (either glucans or mannans) (25, 26, 33). Mannan is a large, complex, and highly immunogenic assembly of mannopyranose units linked through α-1,6, α-1,3, α-1,2, or β-1,2 bonds. It encompasses a large repertoire of antigenic oligomannose epitopes whose specificity is determined by the nature of the linkage between mannose residues and the length of the oligomannose chain (35). These epitopes are associated with a large variety of different yeast carrier molecules and may be species specific or shared by several species (3, 36-38). A clear-cut discrimination between α- and β-linked mannose residues is made by mammalian immune systems and endogenous lectins (11). The antibodies generated are highly specific for each category (15, 16, 24).
A large number of anti-mannan antibodies have been used for the development of antigen detection tests. For all of them, sensitivity is impaired by the rapid clearance by host catabolism of epitopes from the bloodstream (14, 21, 33). We have developed an enzyme immunoassay (EIA) for the detection of mannan and shown that its combination with detection of anti-mannan antibodies was useful for the early diagnosis of systemic candidiasis (32, 33, 44); these tests have been recently marketed as the Platelia Candida Ag and Platelia Candida Ab tests, respectively. The Platelia Candida Ag test detects an α-linked oligomannose residue (α-Man) epitope whose circulation was transient. As beta-linked oligomannose (β-Man) epitopes may be expressed on Candida molecules that differ from those expressing α-Man, it could be anticipated that these different families of epitopes and their respective carrier molecules have (i) different kinetics of release from cells of Candida spp. in tissues and (ii) different kinetics of catabolism by the host. The aim of this study was to examine whether the simultaneous detection of both α- and β-linked oligomannosaccharides could enhance the duration of detection of antigenemia. For this purpose, we used two monoclonal antibodies (MAbs) with different specificities. The first MAb, EB-CA1, recognizes α-1,2-linked oligomannose sequences with more than four residues (17, 19, 25) which are present in the acid-stable fraction of mannan as well as on a wide range of Candida albicans mannoproteins. They are also present in mannoproteins from C. glabrata and C. tropicalis and, at a lower level, from C. parapsilosis and C. krusei (19). This MAb was used in the commercial Pastorex Candida test and, more recently, in the Platelia test. MAb 5B2 reacts with β-1,2-linked oligomannosides which are present in both the acid-stable and acid-labile fractions of C. albicans mannan (18, 37). These epitopes are also present on mannoproteins of C. albicans, C. tropicalis, C. glabrata, and C. parapsilosis (2) and are highly expressed on the phospholipomannan, a glycolipid synthesized by C. albicans, C. dubliniensis, and C. tropicalis (18, 37).
Circulation of α- and/or β-1,2-linked oligomannosaccharides was first investigated in serum samples from guinea pigs experimentally infected with C. albicans. The diagnostic value of the EIA involving MAb 5B2 and MAb EB-CA1 (Platelia Candida Ag test) was then assessed retrospectively in 26 patients with systemic candidiasis caused by C. albicans, C. glabrata, and C. tropicalis, the most pathogenic species encountered in clinical practice.
This work was presented in part at the American Society for Microbiology Conference on Candida and Candidosis, 13 to 17 January 2001, Tampa, Florida.
MATERIALS AND METHODS
MAbs.
Information about the MAbs is summarized in Table 1. MAb EB-CA1 is an immunoglobulin M (IgM) directed against α-linked pentaose (19) which was produced after injection of Lou/C rats with heat-killed C. albicans yeast cells (13). This MAb was kindly provided by Bio-Rad (Marnes la Coquette, France). MAb 5B2 is an IgM generated in our laboratory following a heterologous fusion between mouse myeloma cells and lymphocytes from a rat infected with C. albicans strain VW32 (18). This MAb reacts with C. albicans antigenic factors 5 and 6 (18).
TABLE 1.
Established characteristics of MAbsa
| MAb | Isotype (origin) | Immunogen | Recognized Candida molecules | Minimal epitope(s) | Recognized Candida species |
|---|---|---|---|---|---|
| 5B2 | Monoclonal IgM | C. albicans strain VW32 infection with live cells | Mannan, phospholipomannan, mannoproteins | β-1,2 Mannobiose (homopolymers and heteropolymers) | C. albicans (serotypes A and B) C. tropicalis, C. glabrata, C. guilliermondii, C. lusitaniae |
| EB-CA1 | Monoclonal IgM rat-mouse Lou/C | C. albicans formaldehyde-fixed yeast cells | Mannan, mannoproteins | Mannopentaose with α-1,2 mannotetraose sequence at the nonreducing end | C. albicans (serotypes A and B) C. glabrata, C. tropicalis, C. parapsilosis |
Experimental infection.
Two series of 12 male Pirbright guinea pigs (weighing approximately 500 g) were infected by intravenous inoculation with one of two strains of C. albicans serotype A, VW32 (1) or B2630 (23) (isolate held at the Janssen Research Foundation). For each strain, grading doses of 20,000, 30,000, and 40,000 CFU per gram of body weight were used according to a method described previously (12). Sera collected on days 1, 2, 3, and 7 and plasma collected on days 14, 21, and 28 were stored at −40°C.
Patients.
A total of 90 serum samples were selected retrospectively between January 1996 and December 1998 from 26 patients (9 females and 17 males; mean age, 56.6 years) with proven candidiasis due to C. albicans (19 patients), C. glabrata (4 patients), or C. tropicalis (3 patients). The average number of serum samples per patient was 3.46 ± 1.5 (Table 2). The following criteria were applied as retrospective selection rules: (i) fever nonresponsive to antibacterial therapy but responsive to antifungal therapy; (ii) positive culture for a Candida species from a normally sterile site (blood, bile, pericardial fluid, liver biopsy specimen, drain fluid, or wound); (iii) availability of serum samples within a range of 1 week before to 2 weeks after cultures tested positive; and (iv) analysis of the charts of patients with special attention to risk factors.
TABLE 2.
Underlying diseases and culture data for infected patients
| Patient | Sex | Age | Hospital ward | Underlying condition | Site of yeast isolation | Isolated species | No. of sera | Antifungal therapy |
|---|---|---|---|---|---|---|---|---|
| A1 | F | 42 | Surgery | Liver transplantation | Blood | C. albicans | 4 | FCZg |
| A2 | M | 68 | Gastroenterology | Pancreatic cancer | Blood | C. albicans | 4 | FCZ |
| A3 | M | 45 | ICU | Cardiopulmonary arrest | PLd (drain) | C. albicans | 3 | FCZ |
| A4 | M | 79 | ICU | Respiratory decompensation | Blood | C. glabrata | 3 | FCZ + AmBh |
| B1 | M | 66 | ICU | Respiratory decompensation | Blood | C. albicans | 5 | Nonei |
| B2 | M | 37 | Transplantation | Liver transplantation | BALe | C. albicans | 4 | FCZ |
| B3 | M | 46 | Hematology | MNHLa-ABMTb | Blood | C. tropicalis | 3 | AmB |
| B4 | M | 60 | Hematology | AMLc | Blood | C. tropicalis | 7 | AmB |
| C1 | F | 65 | ICU | Acute pulmonary edema | Blood | C. albicans | 2 | None |
| C2 | M | 64 | ICU | Acute pancreatitis | Blood | C. albicans | 4 | FCZ |
| C3 | F | 58 | ICU | MNHL | Blood | C. glabrata | 4 | FCZ + AmB |
| C4 | M | 75 | ICU | Febrile aplasia | BAL | C. tropicalis | 2 | AmB |
| D1 | M | 73 | ICU | Pneumopathy | PBBf | C. albicans | 1 | FCZ |
| D2 | M | 17 | ICU | AML-ABMT | Blood | C. albicans | 2 | FCZ + AmB |
| D3 | F | 62 | ICU | Bronchopneumonia | BAL | C. albicans | 4 | AmB |
| D4 | M | 31 | ICU | MNHL | Blood | C. albicans | 4 | FCZ |
| D5 | M | 76 | ICU | Bilateral pneumopathy | BAL | C. albicans | 3 | AmB |
| D6 | M | 47 | ICU | Cerebrovascular accident | BAL | C. albicans | 5 | FCZ |
| D7 | F | 70 | ICU | Hyperthermia | Blood | C. albicans | 5 | AmB |
| D8 | M | 71 | Surgery | Pancreatectomy | Blood | C. albicans | 1 | FCZ |
| D9 | F | 46 | Surgery | Acute pancreatitis | Blood | C. albicans | 2 | FCZ |
| D10 | F | 47 | Surgery | Appendicectomy | Blood | C. albicans | 2 | FCZ |
| D11 | M | 48 | Surgery | Ulcerative colitis | Blood | C. albicans | 4 | FCZ |
| D12 | M | 51 | Hematology | AML | Blood | C. albicans | 4 | FCZ |
| D13 | F | 64 | ICU | Acute respiratory distress | Blood | C. glabrata | 4 | FCZ + AmB |
| D14 | F | 65 | Surgery | Acute pancreatitis | Blood | C. tropicalis | 4 | FCZ |
MNHL, malignant non-Hodgkin's disease lymphoma.
ABMT, allogeneic bone marrow transplantation.
AML, acute myelogenous leukemia.
PL, pleural liquid.
BAL, bronchoalveolar lavage fluid.
PBB, peribronchial biopsy.
FCZ, fluconazole. Patients received 400 mg per day as a loading dose and 200 mg per day as a maintenance dose.
AmB, amphotericin B. Depending on renal function, AmB was given at 0.5 to 1 mg/kg of body weight per day.
None, no therapy was administered.
In addition to fever, other clinical signs included endophthalmitis (patients B4 and D11) and cutaneous lesions (patients B4, D10, and D11). Curative antifungal management was instituted for all patients except for patients C1 and B1, who died the day after isolation of a Candida sp. from blood cultures. For all patients except D8, broad-spectrum antibiotics were first administered an average of 2 weeks before isolation of a Candida sp. In 23 patients, central venous catheters or peripheral venous access ports were in situ at the time of positive blood culture results. Neutropenia (<500 leukocytes/mm3) in seven patients (B3, B4, C4, D2, D4, and D12) and oral or intravenous immunosuppressive therapy (corticosteroids in 14 patients) were also documented. Five patients had diabetes mellitus.
Control sera.
Five groups of control sera were included in this study. Group 1 consisted of the serum samples of 15 patients at high risk for systemic candidosis who were hospitalized in intensive care units (ICU) or surgery or respiratory wards and for whom Candida colonization was documented at two or more body sites but who presented no evidence of Candida infection. Group 2 comprised the serum samples of 10 patients with deep fungal infection not caused by Candida (7 patients with invasive pulmonary aspergillosis and 3 patients with cryptococcal meningitis). Group 3 consisted of 10 sera from nine patients with high levels of Cytomegalovirus antigenemia. Group 4 consisted of sera drawn from 70 healthy blood donors. Sera from 14 patients with high levels of rheumatoid factor (known to generate interference with serological tests) were included as group 5.
Serological tests.
Detection of circulating α- and β-linked oligomannosides was performed.
Detection of α-1-2-linked oligomannosides.
The method employed was based on a commercially available Platelia Candida Ag test (Bio-Rad) (33). This one-step, sandwich, microplate EIA uses the MAb EB-CA1 (3.4 mg/ml) as a captor and detector antibody to allow the detection of mannan in serum samples. Each patient's serum sample (300 μl) was treated with 100 μl of dissociating solution, boiled for 3 min, and centrifuged for 10 min at 10,000 × g to release free antigens. Supernatant (50 μl) was added to EB-CA1-precoated microtiter plate wells with 50 μl of horseradish peroxidase (HRP)-conjugated MAb EB-CA1. After incubation for 90 min at 37°C, the plates were washed thoroughly and the reaction was detected by incubation with 200 μl of tetramethylbenzidine solution for 30 min according to the manufacturer's instructions. Each experiment included a calibration curve obtained with a pool of normal human sera spiked with different concentrations of mannan in the range of 0.1 to 2 ng/ml.
Detection of β-1-2-linked oligomannosides.
A similar method was developed for the detection of circulating β-1,2-linked oligomannosides. Polystyrene microtiter plates were coated with 100 μl of MAb 5B2 (1 μg/well). The subsequent steps were performed as described above except for the detection step, which was performed with HRP-conjugated MAb 5B2 for the homologous system (MAb 5B2 as captor and detector) or HRP-conjugated EB-CA1 for the heterologous system.
For MAb 5B2 conjugation, HRP (Boehringer) in HEPES buffer was activated by oxidation with sodium periodate (39). The activated peroxidase was then purified by column chromatography on PD10 Sephadex (Pharmacia Biotech, Uppsala, Sweden), diluted in phosphate-buffered saline, and subsequently incubated for 3 h with the MAb (enzyme/antibody ratio, 25/1 mol). The conjugated MAb 5B2 was dialyzed using phosphate-buffered saline and stored at 4°C in a solution of 0.01% sodium merthiolate. The optimal concentration of HRP-conjugated MAb 5B2 (determined in an EIA using a graded concentration of mannan) was 8 μg/ml.
RESULTS
Detection of α- and β-linked oligomannosides in sera from experimentally infected guinea pigs.
Figure 1 shows individual antigenemia values for each serum sample drawn from 24 guinea pigs intravenously injected with different doses of two C. albicans strains. Mortality was strain and inoculum dependent; at the end of the experiment (day 28), the overall mortality rates were 25% (three animals) and 58% (seven animals) for strains B2630 and VW32, respectively (Spearman correlation; P < 0.030). Both α- and β-oligomannoside epitopes could be detected in each of the infected animals. However, Figure 1 shows that among the 125 sera available, there was considerable variability in the quantity of antigen (0.1 to 9 ng/ml) detected for each epitope; the quantity depended on the strain, the challenge dose of C. albicans, and the day the sera were collected. For guinea pigs infected with strain B2630, 92% of sera presented results positive for α mannanemia and 78% presented results positive for β mannanemia. The values for both mannanemias were maximal during the first week after infection, became negative or weakly positive, and then increased again by day 28. For animals infected with strain VW32, only 56 sera were available due to mortality and disseminated intravascular coagulation. Variations in antigen levels were observed in successive serum samples drawn from the same animal. Although 82% of the serum samples were positive according to the results of at least one test, the sensitivity was 79 and 46% for α- and β-mannanemia. The amount of α-linked residues was higher than that of β-linked residues in 48% of the serum samples. For 6% of the serum samples, the quantity of β-linked residues was larger than that of α-linked residues.
FIG. 1.
Kinetics of circulating α- and β-linked mannoglycoconjugates as detected by MAb EB-CA1 (Platelia Ag) or MAb 5B2 (EIA 5B2) (boxes with or without • symbols, respectively) in sequentially drawn serum samples from guinea pigs experimentally infected by two strains of C. albicans. For each test, the levels of α- and β-mannanemia were graded from minimal (mannanemia levels of <0.1 ng/ml [white boxes]) to peak (mannanemia levels of ≥1 ng/ml [black boxes]) on the basis of the detected mannan concentrations; intermediate values are represented by light-grey box shading (mannanemia levels between ≤0.1 ng/ml and <0.5 ng/ml) or dark-grey box shading (mannanemia levels between ≤0.5 ng/ml and <1 ng/ml). nd, tests not done; †, deceased animals.
Detection of Candida-derived oligomannosides in control and patients' sera.
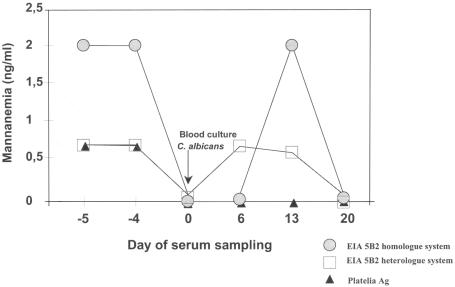
The results for mannanemia detection tests are shown in Table 3. Patients were classified into four groups which correlated with their serologic patterns. In the first group (patients A1 to A4; n = 4 [15.3%]), no antigenemia was detectable at any time despite the availability of several sera from each patient. In the second group (patients B1 to B4; n = 4 [15.3%]), β-mannanemia results were negative throughout but a significant α-mannanemia result was detected. In the third group (patients C1 to C4; n = 4 [15.3%]), β-mannanemia was detected in at least one sample but without evidence of α-mannanemia. For 54% of the patients (group D), both antigenemia detection test results were positive for a given patient (although usually not in the same serum sample). A representative example of the differences observed in the time course of α- and β-mannanemia detection in such patients is shown in Fig. 2. For this patient (D7) (Table 2 and Table 3), Platelia Ag test (α mannanemia) and β-mannanemia test results were positive 5 days before the positive-testing blood culture was drawn (and 7 days before C. albicans grew in culture). α-Mannanemia results then became consistently negative, whereas a peak of β-mannanemia, which was coherent with the persistence of an infectious syndrome, was observed 2 weeks after the sample giving a positive blood culture result was drawn.
TABLE 3.
Results of antigen and antibody testing in patients with candidiasis
| Patient | Result of:
|
|||||
|---|---|---|---|---|---|---|
| Platelia Candida Ag test (ng/ml)
|
EIA β-Man 5B2/5B2 captor-detector test (ng/ml)
|
EIA β-Man EB-CA1/5B2 captor-detector test (ng/ml)
|
||||
| Peak | Mean | Peak | Mean | Peak | Mean | |
| A1 | 0 | 0 | 0.4 | 0.1 | 0 | 0 |
| A2 | 0 | 0 | 0 | 0 | 0 | 0 |
| A3 | 0 | 0 | 0 | 0 | 0.4 | 0.2 |
| A4 | 0 | 0 | 0.4 | 0.1 | 0.4 | 0.1 |
| B1 | 0.6 | 0.2 | 0 | 0 | 0 | 0 |
| B2 | 0.5 | 0.2 | 0 | 0 | 0 | 0 |
| B3 | 0.6 | 0.2 | 0.4 | 0.1 | 0 | 0 |
| B4 | 2 | 0.6 | 0.4 | 0.1 | 0.4 | 0.05 |
| C1 | 0 | 0 | 2 | 1.5 | 0.7 | 0.4 |
| C2 | 0 | 0 | 2 | 0.5 | 2 | 0.6 |
| C3 | 0 | 0 | 0.7 | 0.2 | 0 | 0.2 |
| C4 | 0.4 | 0.2 | 0.5 | 0.3 | 0.6 | 0.3 |
| D1 | 2 | 2 | 2 | 2 | 2 | 2 |
| D2 | 1.2 | 1.1 | 0.8 | 0.7 | 0.5 | 0.5 |
| D3 | 0.8 | 0.2 | 1.1 | 0.5 | 1.1 | 0.3 |
| D4 | 0.7 | 0.5 | 2 | 0.5 | 0 | 0 |
| D5 | 2 | 1.3 | 2 | 1.3 | 2 | 1.2 |
| D6 | 0.7 | 0.5 | 1.6 | 0.7 | 1.2 | 0.7 |
| D7 | 0.7 | 0.3 | 2 | 1.2 | 0.6 | 0.2 |
| D8 | 2 | 2 | 2 | 2 | 2 | 2 |
| D9 | 2 | 1 | 1.2 | 0.6 | 2 | 1 |
| D10 | 1.5 | 0.8 | 1 | 0.7 | 0.6 | 0.5 |
| D11 | 1 | 0.25 | 1 | 0.25 | 1 | 0.25 |
| D12 | 2 | 1 | 0.4 | 0.1 | 1 | 0.4 |
| D13 | 0.6 | 0.2 | 0.5 | 0.1 | 0 | 0 |
| D14 | 2 | 0.6 | 2 | 0.7 | 2 | 0.6 |
FIG. 2.
Example of kinetic evolution of mannanemia as detected by different tests. Patient D6 had systemic candidiasis; the date of mycological isolation of C. albicans from blood culture is indicated by the arrow.
Figure 2 also illustrates how the use of heterologous detection systems gave insights into the complex nature of circulating Candida antigens. Although sera drawn on both day 6 and day 13 gave negative results with MAb EB-CA1 in the homologous system (Platelia Ag) for detection of α-Man (when the same MAb was used as a captor and MAb 5B2 [anti-β-Man] was used as a detector), antigenemia was detected. Similar results were obtained with sera from patients C1 and C4. This means that in antigens released from C. albicans, both α- and β-Man epitopes were associated. These antigens were detectable in host serum, although the level of α-Man repetitive epitopes alone was not high enough to allow their detection. Interestingly, mannanemia could be detected before culture positivity. α-Mannanemia was detected in 62% of patients at an average of 5.6 days before cultures gave positive results, and β-mannanemia was detected in 48% patients at an average of 3.9 days before cultures gave positive results.
Controls consisted of a panel of representative hospitalized patients, including (i) patients at high risk for systemic candidosis who were hospitalized in clinical wards and for whom Candida colonization was documented but who presented no evidence of Candida infection, (ii) patients with deep fungal infection not caused by Candida spp. (including patients with invasive pulmonary aspergillosis, cryptococcal meningitis, and cytomegalovirus infection), (iii) patients with high levels of rheumatoid factor (known to generate interference with serological tests), and (iv) healthy blood donors. The results obtained with these control sera are summarized in Table 4. Depending on the tests, positive antigenemia (at low levels) results were observed for 2.5 to 5.6% of control sera. Most of the patients with low-level results had several colonized body sites, a context that cannot exclude the presence of a subclinical Candida infection. This choice of control population probably accounts for the relatively low cumulative predictive positive value of the tests (79%) (Table 5).
TABLE 4.
Results of antibody and antigen testing on sera from control populations
| Category | No. of patients | No. of sera | No. of sera that tested positivea
|
||
|---|---|---|---|---|---|
| Platelia Candida Ag test | EIA 5B2 homologous system | EIA 5B2 heterologous system | |||
| Intensive care patients without invasive candidiasis | 15 | 44 | 1 | 5 | 1 |
| Aspergillosis | 7 | 7 | 0 | 0 | 0 |
| Cryptococcosis | 3 | 3 | 0 | 0 | 0 |
| Cytomegalovirus infection | 9 | 10 | 2 | 2 | 2 |
| Healthy blood donors | 70 | 70 | 0 | 0 | 0 |
| Patients with rheumatoid factor activity | 14 | 14 | 0 | 0 | 0 |
| Total | 118 | 148 | 3 (2) | 7 (4.7) | 3 (2) |
Values in parentheses are percentages.
TABLE 5.
Sensitivity, specificity and predictive values for the detection of α- and β-mannanemia detection testsa
| Parameter | Value (%) for test
|
||
|---|---|---|---|
| Platelia Candida Ag | EIA 5B2 homologous system | Combination of both tests | |
| Sensitivity | 69 | 69 | 85 |
| Specificity | 98 | 95 | 95 |
| Positive predictive value | 86 | 75 | 79 |
| Negative predictive value | 94 | 94 | 97 |
Results (per patient) were calculated following an analysis of 90 serum samples from 26 patients with systemic candidiasis and 148 sera from 118 controls.
Altogether, the results obtained showed that the combination of the Platelia Ag test and 5B2 EIA increased the sensitivity of mannan detection from 69 to 85%; their negative predictive value was 95%.
DISCUSSION
In this report we demonstrate that α- and β-oligomannosides synthesized by Candida species have different kinetics of circulation during experimental and human candidosis. This was evidenced by the use of sensitive immunoassays involving MAbs, each previously characterized for its specificity for an epitope type (18, 19) and for the nature of the structural Candida molecules carrying the respective epitopes (1, 37). Both epitopes were distributed over a large variety of molecules expressed by the major pathogenic Candida species (13, 19). Such a high level of expression is a necessary condition for sensitive detection.
Since the initial observation by Weiner and Coasts-Stephen (40), a large number of studies have been designed to examine detection of mannan in serum for diagnostic purposes (9, 24, 42). However, with few exceptions, the nature of the epitope detected in these studies was unknown. Thanks to progress made in epitope determination, it can be now concluded retrospectively that both α- and β-mannosaccharides released by Candida spp. can be detected (14, 19, 35, 37). Whatever the specificity of the antibody used, a rapid clearance of detectable antigen impaired the sensitivity of the tests (5, 21). Considering that the α- and β-Man epitopes detected here may be expressed on the same carrier molecule but also on different molecules, we hypothesized that their release in the infected host, their uptake by host endogenous lectins and antibodies, and their catabolism occur at different rates. This was observed in both experimentally infected animals but also in sera from patients infected by Candida species. Use of a combined system for detection of multiple epitope types thus led to increasing antigen detection sensitivity that compensated for the transitory nature of individual residues in circulation.
No conclusion can yet be drawn concerning the pathophysiological significance of each type of mannoside residue in circulation. In animals there was an obvious dose dependence relationship between fungal load and antigenemia for the less pathogenic strain. In individual animals the kinetics were similar: high antigenemia levels following intravenous injection and bloodstream dissemination, a relative decrease observed when fungal growth begin to develop in tissues, and—for animals that survived further—another late peak of antigenemia seen at the stage at which their organs were deeply invaded and their condition deteriorated. Interestingly, infection with the more virulent C. albicans strain (which was presumably eliminated in lower quantities by host defenses) led to lower levels of antigenemia. This conclusion is not definitive, since rapid death and disseminated intravascular coagulation in this group of animals limited the availability of sera from later stages of infection. High variability of results between animals infected by the same strain at the same dose probably reflects individual susceptibility differences to C. albicans challenge.
In patients, our results also showed that the circulation characteristics of α-Man and β-Man epitopes were different for sera drawn successively from the same patient. Sera from four patients (C1 to C4) displayed only β-Man antigenemia, whereas only α-Man antigenemia could be detected in sera from patients B1 to B4 (Table 3). The Platelia Candida Ag assay was positive for 18 (69%) of the 26 patients with systemic candidiasis. The two versions of the test involving MAb 5B2 (homologous and heterologous systems) had sensitivity levels of 69 and 58%, respectively. In several cases, patients displayed positive results with only one test. The association of all three tests would have allowed a diagnosis of candidiasis in 85% of the patients. The results obtained by the heterologous system (MAb EB-CA1 as captor and MAb 5B2 as detector) revealed circulating macromolecules which expressed both α- and β-Man epitopes, although the level of α-Man repetitive epitopes alone was not high enough to allow their detection. The reciprocal heterologous test was also tried (MAb 5B2 as captor and MAb EB-CA1 as detector), and no significant difference in sensitivity was observed.
All antigen detection tests displayed good specificity, even though specificity was well challenged by a control population chosen to include many individuals likely to induce false-positive reactions. This population consisted of patients suffering from other deep-seated mycoses (invasive aspergillosis, cryptococcosis) or afebrile hospitalized patients known to be colonized with Candida species but showing no mycological evidence of Candida infection. The best performance of the tests was their negative predictive value (97%), which is of interest to those in clinical practice facing situations in which the majority of patients present multiple risk factors for developing a Candida infection. As stated recently in a review by Stevens (34), serological tests of high negative predictive value could be of help to identify those who do not require prescription of antifungals.
An alternative strategy for diagnosis of systemic candidiasis is PCR, which has recently been found to give promising results. This method is based on the amplification of more or less specific portions of DNA sequences from Candida species whose presence in blood or serum was shown to be specific for infection (4, 8, 22, 29). In a preliminary study, Sendid et al. showed that serology and PCR contribute equally to the diagnosis of Candida infections proved by autopsy (E. Norberg, L. Klingspor, B. Sendid, L. Dumortier, N. Francois, J. Tollemar, and D. Poulain, Abstr. 6th Trends Invasive Fungal Infect., Prague, abstr. P36, 18-20 October, 2001). In the same way as for antigens, the physiology and kinetics of the release and degradation of nucleic acids from infecting fungi are still unknown. Although diagnostic sequences may encode essential yeast genes and can be easily amplified, these molecules are pathophysiologically inert. Antigens, by contrast, can (by definition) induce an antibody response, and a clear-cut balance between high anti-mannan antibody levels and mannanemia in sera from patients with systemic candidiasis led us to propose a strategy based on a joint detection of both antigen and anti-mannan antibodies. Through the same logic as that developed here for antigen detection, however, it is now well established that anti-mannan antibodies are directed against a mixture of epitopes including α- and β-Man homopolymers or heteropolymers. Moreover, it has been experimentally shown that anti-β-Man antibodies were protective whereas anti-α-Man antibodies were not (15, 16, 24). Interestingly, Joualt et al. have shown that in patients with Candida infection, but not in patients colonized with a Candida sp., there was a down regulation of anti-β-Man “protective” antibodies which was not observed for the “nonprotective” anti-α-Man antibodies (20). At the moment, the Platelia Ab test detects antibodies against the whole mannan oligomannose repertoire containing both epitope types (33). Studies are in progress for developing multiparametric tests involving Candida oligomannose synthetic analogues to detect separately antibodies specific for different types of residues (10). Together with joint detection of the same residues, this would provide a coherent model with the goal of gaining a better understanding of the pathophysiology of this disease together with a higher sensitivity level for the diagnostic or even prognostic significance of the tests.
Acknowledgments
We thank Laurence Richard, Nadine François, and Frans Van Gerven for their expert technical assistance.
This work was supported by a grant from the Programme Hospitalier de Recherche Clinique du Ministère des Affaires Sociales, de la Santé et de la Ville, No. 1918.
REFERENCES
- 1.Cailliez, J. C., and D. Poulain. 1988. Cytologic analysis of the expression of an epitope carried by glycoproteins excreted by Candida albicans. Ann. Inst. Pasteur Microbiol. 139:171-188. [DOI] [PubMed] [Google Scholar]
- 2.Cantelli, C., P. A. Trinel, A. Bernigaud, T. Jouault, L. Polonelli, and D. Poulain. 1995. Mapping of beta-1,2-linked oligomannosidic epitopes among glycoconjugates of Candida species. Microbiology 141:2693-2697. [DOI] [PubMed] [Google Scholar]
- 3.Cassone, A., A. Torosantucci, M. Boccanera, G. Pellegrini, C. Palma, and F. Malavasi. 1988. Production and characterisation of a monoclonal antibody to a cell-surface, glucomannoprotein constituent of Candida albicans and other pathogenic Candida species. J. Med. Microbiol. 27:233-238. [DOI] [PubMed] [Google Scholar]
- 4.Chryssanthou, E., L. Klingspor, J. Tollemar, B. Petrini, L. Larsson, B. Christensson, and O. Ringden. 1999. PCR and other non-culture methods for diagnosis of invasive Candida infections in allogeneic bone marrow and solid organ transplant recipients. Mycoses 42:239-247. [DOI] [PubMed] [Google Scholar]
- 5.Day, J. F., R. W. Thornburg, S. R. Thorpe, and J. W. Baynes. 1980. Carbohydrate-mediated clearance of antibody antigen complexes from the circulation. The role of high mannose oligosaccharides in the hepatic uptake of IgM antigen complexes. J. Biol. Chem. 255:2360-2365. [PubMed] [Google Scholar]
- 6.Debra, A. G., J. S. Sondra, and J. F. Robert. 1996. Cost analysis of Candida infection among surgical intensive care unit patients. Clin. Drug Investig. 12:176-180. [Google Scholar]
- 7.De Pauw, B. E., and J. F. Meis. 1998. Progress in fighting systemic fungal infections in haematological neoplasia. Support Care Cancer 6:31-38. [DOI] [PubMed] [Google Scholar]
- 8.Einsele, H., H. Hebart, G. Roller, J. Loffler, I. Rothenhofer, C. A. Muller, R. A. Bowden, J. van Burik, D. Engelhard, L. Kanz, and U. Schumacher. 1997. Detection and identification of fungal pathogens in blood by using molecular probes. J. Clin. Microbiol. 35:1353-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erjavec, Z., and P. E. Verweij. 2002. Recent progress in the diagnosis of fungal infections in the immunocompromised host. Drug Resist. Updates 5:3-10. [DOI] [PubMed] [Google Scholar]
- 10.Esnault, J., P. Sinay, R. Chevalier, J. F. Colombel, J. M. Mallet, B. Sendid, T. Jouault, D. Poulain, and P. A. Trinel. 23November1999. Oligomannosides de synthèse, leur préparation et leurs utilisations. European patent 99/14747.
- 11.Fradin, C., D. Poulain, and T. Jouault. 2000. β-1,2-linked oligomannosides from Candida albicans bind to a 32-kilodalton macrophage membrane protein homologous to the mammalian lectin galectin-3. Infect. Immun. 68:4391-4398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fransen, J., J. Van Cutsem, R. Vandesteene, and P. A. Janssen. 1984. Histopathology of experimental systemic candidosis in guinea-pigs. Sabouraudia 22:455-469. [DOI] [PubMed] [Google Scholar]
- 13.Georges, E., M. L. Garrigues, D. Stynen, and J. L. Poirot. 1991. Spécificité in vitro d'un anticorps monoclanal (Acm) anti-mannane et du latex sensibilisé par cet anticorps au cours de la candidose disséminée expérimentale. J. Mycol. Med. 1:21-24. [Google Scholar]
- 14.Girmenia, C., P. Martino, F. De Bernardis, and A. Cassone. 1997. Assessment of detection of Candida mannoproteinemia as a method to differentiate central venous catheter-related candidemia from invasive disease. J. Clin. Microbiol. 35:903-906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han, Y., T. Kanbe, R. Cherniak, and J. E. Cutler. 1997. Biochemical characterization of Candida albicans epitopes that can elicit protective and nonprotective antibodies. Infect. Immun. 65:4100-4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han, Y., M. H. Riesselman, and J. E. Cutler. 2000. Protection against candidiasis by an immunoglobulin G3 (IgG3) monoclonal antibody specific for the same mannotriose as an IgM protective antibody. Infect. Immun. 68:1649-1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herent, P., D. Stynen, F. Hernando, J. Fruit, and D. Poulain. 1992. Retrospective evaluation of two latex agglutination tests for detection of circulating antigens during invasive candidosis. J. Clin. Microbiol. 30:2158-2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hopwood, V., D. Poulain, B. Fortier, G. Evans, and A. Vernes. 1986. A monoclonal antibody to a cell wall component of Candida albicans. Infect. Immun. 54:222-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacquinot, P. M., Y. Plancke, B. Sendid, G. Strecker, and D. Poulain. 1998. Nature of Candida albicans-derived carbohydrate antigen recognized by a monoclonal antibody in patient sera and distribution over Candida species. FEMS Microbiol. Lett. 169:131-138. [DOI] [PubMed] [Google Scholar]
- 20.Jouault, T., C. Delaunoy, B. Sendid, F. Ajana, and D. Poulain. 1997. Differential humoral response against alpha- and beta-linked mannose residues associated with tissue invasion by Candida albicans. Clin. Diagn. Lab. Immunol. 4:328-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kappe, R., and J. Muller. 1991. Rapid clearance of Candida albicans mannan antigens by liver and spleen in contrast to prolonged circulation of Cryptococcus neoformans antigens. J. Clin. Microbiol. 29:1665-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loeffler, J., N. Henke, H. Hebart, D. Schmidt, L. Hagmeyer, U. Schumacher, and H. Einsele. 2000. Quantification of fungal DNA by using fluorescence resonance energy transfer and the light cycler system. J. Clin. Microbiol. 38:586-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maesaki, S., P. Marichal, H. Vanden Bossche, D. Sanglard, and S. Kohno. 1999. Rhodamine 6G efflux for the detection of CDR1-overexpressing azole-resistant Candida albicans strains. J. Antimicrob. Chemother. 44:27-31. [DOI] [PubMed] [Google Scholar]
- 24.Martinez, J. P., M. L. Gil, J. L. Lopez-Ribot, and W. L. Chaffin. 1998. Serologic response to cell wall mannoproteins and proteins of Candida albicans. Clin. Microbiol. Rev. 11:121-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mitsutake, K., T. Miyazaki, T. Tashiro, Y. Yamamoto, H. Kakeya, T. Otsubo, S. Kawamura, M. A. Hossain, T. Noda, Y. Hirakata, and S. Kohno. 1996. Enolase antigen, mannan antigen, Cand-Tec antigen, and β-glucan in patients with candidemia. J. Clin. Microbiol. 34:1918-1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Obayashi, T., M. Yoshida, T. Mori, H. Goto, A. Yasuoka, H. Iwasaki, H. Teshima, S. Kohno, A. Horiuchi, A. Ito, et al. 1995. Plasma (1→3)-beta-d-glucan measurement in diagnosis of invasive deep mycosis and fungal febrile episodes. Lancet 345:17-20. [DOI] [PubMed] [Google Scholar]
- 27.Pfaller, M. A., R. N. Jones, S. A. Messer, M. B. Edmond, R. P. Wenzel, and SCOPE Participant Group. 1998. National surveillance of nosocomial blood stream infection due to species of Candida other than Candida albicans: frequency of occurrence and antifungal susceptibility in the SCOPE Program. Surveillance and Control of Pathogens of Epidemiologic. Diagn. Microbiol. Infect. Dis. 30:121-129. [DOI] [PubMed] [Google Scholar]
- 28.Pittet, D. 1993. Nosocomial bloodstream infections, p. 512-555. In R. P. Wenzel (ed.), Prevention and control of nosocomial infections, 2nd ed. Williams and Wilkins, Baltimore, Md.
- 29.Reiss, E., T. Obayashi, K. Orle, M. Yoshida, and R. M. Zancope-Oliveira. 2000. Non-culture based diagnostic tests for mycotic infections. Med. Mycol. 38(Suppl. 1):147-159. [PubMed] [Google Scholar]
- 30.Richardson, M. D., and M. H. Kokki. 1998. Diagnosis and prevention of fungal infection in the immunocompromised patient. Blood Rev. 12:241-254. [DOI] [PubMed] [Google Scholar]
- 31.Richardson, M. D., and M. H. Kokki. 1999. New perspectives in the diagnosis of systemic fungal infections. Ann. Med. 31:327-335. [DOI] [PubMed] [Google Scholar]
- 32.Sendid, B., J. L. Poirot, M. Tabouret, D. Caillot, A. Bonnin, D. Camus, and D. Poulain. 2002. Combined detection of mannanemia and anti-mannan antibodies for the diagnosis of systemic infection determined by the most pathogenic Candida species. J. Med. Microbiol. 51:1-10. [DOI] [PubMed] [Google Scholar]
- 33.Sendid, B., M. Tabouret, J. L. Poirot, D. Mathieu, J. Fruit, and D. Poulain. 1999. New enzyme immunoassays for sensitive detection of circulating Candida albicans mannan and antimannan antibodies: useful combined test for diagnosis of systemic candidiasis. J. Clin. Microbiol. 37:1510-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stevens, D. A. 2002. Diagnosis of fungal infections: current status. J. Antimicrob. Chemother. 49(Suppl. A):11-19. [DOI] [PubMed] [Google Scholar]
- 35.Suzuki, S. 1997. Immunochemical study on mannans of genus Candida. I. Structural investigation of antigenic factors 1, 4, 5, 6, 8, 9, 11, 13, 13b and 34. Curr. Top. Med. Mycol. 8:57-70. [PubMed] [Google Scholar]
- 36.Trinel, P. A., C. Cantelli, A. Bernigaud, T. Jouault, and D. Poulain. 1996. Evidence for different mannosylation processes involved in the association of beta-1,2-linked oligomannosidic epitopes in Candida albicans mannan and phospholipomannan. Microbiology 142:2263-2270. [DOI] [PubMed] [Google Scholar]
- 37.Trinel, P. A., C. Faille, P. M. Jacquinot, J. C. Cailliez, and D. Poulain. 1992. Mapping of Candida albicans oligomannosidic epitopes by using monoclonal antibodies. Infect. Immun. 60:3845-3851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trinel, P. A., Y. Plancke, P. Gerold, T. Jouault, F. Delplace, R. T. Schwarz, G. Strecker, and D. Poulain. 1999. The Candida albicans phospholipomannan is a family of glycolipids presenting phosphoinositolmannosides with long linear chains of beta-1,2-linked mannose residues. J. Biol. Chem. 274:30520-30526. [DOI] [PubMed] [Google Scholar]
- 39.Tsang, V. C., R. M. Greene, and J. B. Pilcher. 1995. Optimization of the covalent conjugating procedure (NaIO4) of horseradish peroxidase to antibodies for use in enzyme-linked immunosorbent assay. J. Immunoass. 16:395-418. [DOI] [PubMed] [Google Scholar]
- 40.Weiner, M. H., and M. Coats-Stephen. 1979. Immunodiagnosis of systemic candidiasis: mannan antigenemia detected by radioimmunoassay in experimental and human infections. J. Infect. Dis. 140:989-993. [DOI] [PubMed] [Google Scholar]
- 41.Wenzel, R. P. 1995. Nosocomial candidemia: risk factors and attributable mortality. Clin. Infect. Dis. 20:1531-1534. [DOI] [PubMed] [Google Scholar]
- 42.Yeo, S. F., and B. Wong. 2002. Current status of nonculture methods for diagnosis of invasive fungal infections. Clin. Microbiol. Rev. 15:465-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yeo, S. F., Y. Zhang, D. Schafer, S. Campbell, and B. Wong. 2000. A rapid, automated enzymatic fluorometric assay for determination of d-arabinitol in serum. J. Clin. Microbiol. 38:1439-1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yera, H., B. Sendid, N. François, D. H. Camus, and D. Poulain. 2001. Contribution of serology and blood culture to the early diagnosis of systemic candidiasis. Eur. J. Clin. Microbiol. Infect. Dis. 20:864-870. [DOI] [PubMed] [Google Scholar]