Abstract
Objective
Describe differences in smoking behaviors associated with occupation, workplace rules against smoking, and workplace smoking cessation programs.
Methods
We analyzed data from the Current Population Survey- Tobacco Use Supplement surveys from 1992 through 2007.
Results
After adjusting for demographic factors, blue-collar workers were at higher risk than white-collar workers for ever smoking, current smoking, and persistent smoking (current smoking among ever smokers). Construction workers were more likely to be current daily smokers than other blue-collar workers. Among ever smokers, current daily smoking was more common in the absence of both workplace rules against smoking and workplace smoking cessation programs.
Conclusions
Social or cultural effects related to occupation are important determinants of smoking. More aggressive promotion of smoking cessation programs and workplace rules prohibiting smoking could have a significant public health impact.
INTRODUCTION
Cigarette smoking is the leading cause of preventable morbidity and mortality in the United States. According to the 2008 National Health Interview Survey (NHIS), an estimated 20.6% of US adults are current smokers, a decrease from the 24.1% reported in 1998 but still above the target of <12% set in Healthy People 2010.1 The CDC estimates that between 2000 and 2004, smoking and exposure to second hand tobacco smoke in the United States resulted in 443,000 premature deaths, 5.1 million years potential life lost, and 96.8 billion dollars annually in productivity losses. These data indicate that the general population and the workforce of the United States continues to be adversely affected by smoking related illnesses.2
Over the past several decades, blue-collar workers have been identified as a high-risk group for smoking.3 Although overall smoking rates have declined in recent years, the disparity among occupational groups still exists.4 In the 2000 National Health Interview Survey (NHIS), blue-collar workers reported smoking rates more than twice those of white-collar workers.5 In addition, blue-collar workers smoke more heavily, initiate smoking at a younger age, and are less likely to quit compared to white-collar workers.4 Construction workers, a subset of blue-collar workers, have been identified as a particularly high-risk occupational group for smoking. In the NHIS survey period from 1997 – 2004, construction workers had the highest rate of current smoking, more than 1.5 times the rate reported in all workers (38.8% and 24.5%, respectively).6 This high rate of smoking affects a large subset of the population – more than 11 million people worked in construction industries in 2005.7
This study was designed to address several gaps in the existing literature. In addition to examining the differences in smoking behaviors between occupational groups, we analyzed the effects of two workplace policies aimed at reducing tobacco use: the presence of workplace smoking cessation programs and the presence of workplace rules limiting smoking. We also looked at changes over time in these policies and in several smoking behaviors by occupational group. While most previous studies have focused on current smoking as the main smoking outcome, we used additional measures to better describe occupational differences in tobacco use, including the initiation of smoking, continued smoking following initiation, intent to quit, and the number of cigarettes smoked per day. We adjusted differences between occupations on a variety of demographic factors known to affect smoking behavior.
To achieve these goals, we analyzed smoking and occupation data from a nationally representative survey, the Current Population Survey- Tobacco Use Supplement (CPS-TUS) from 2006–2007, as well as previous CPS-TUS surveys dating back to 1992. We used these data to examine the effect of occupation and workplace policies on smoking behaviors.
METHODS
Data Source and Inclusion Criteria
Data were obtained from Current Population Survey- Tobacco Use Supplements.8, 9 The Current Population Survey (CPS) is a national survey conducted by the Bureau of the Census for use by the Bureau of Labor that interviews 50,000 households monthly with the intent of describing the characteristics of the US labor force. While the CPS dates back 50 years, the Tobacco Use Supplement (CPS-TUS) was added in 1992 and has been administered approximately every 3 years since. The CPS-TUS is the only national survey that contains job classification, job-related tobacco policy, and smoking behavior variables. For current smoking prevalence rates, the 2006–2007 CPS-TUS was used, and for analyses of trends in smoking five time points were used: the 1993, 1996, 1999, 2001, and 2006–2007 CPS-TUS. We included adults age 18–64 who reported having been employed at any time in the last year. Those who worked in Armed Forces occupations and farm, fishing and forestry occupations were dropped from analyses due to small sample size. The final sample size was 106,604.
Definitions
Smoking Behaviors
Respondents were asked “Have you smoked at least 100 cigarettes in your entire life?”; “Do you now smoke cigarettes every day, some days, or not at all?”; and “Are you seriously considering quitting smoking within the next 6 months?” By survey design, “ever smoking” was defined as having smoked 100 cigarettes during the respondent’s lifetime. “Current daily smoking” referred to individuals who reported smoking every day. “Persistent smoking” was defined as current daily smoking among those who reported ever smoking. Since persistent smoking measures smoking only among those who started smoking, it is a more appropriate measure for assessing the success of smoking cessation efforts than current daily smoking, which is a function of smoking initiation as well as cessation.
Occupation
Occupational status was obtained from CPS-TUS and recoded to align with the US Standard Occupational Classification System.10 We classified occupations into “white-collar”, “blue-collar”, and “service workers” (see Appendix 1, http://links.lww.com/JOM/A74). Construction workers, which also include extraction workers, are those with occupations in SOC codes 6200 to 6940 and include occupations such as carpenters, sheet metal workers, brick masons, floor installers, highway maintenance workers, and earth drillers.
Statistical Analyses
We conducted univariate analyses to examine differences in the prevalence of smoking behaviors between different categories of occupations (white-collar, service, blue-collar, and construction). For each occupational group, we assessed the overall prevalence of ever smoking, current daily smoking, and persistent smoking. Intention to quit within six months and number of cigarettes per day were also examined in current smokers. Multivariate logistic regression analyses were performed for four primary outcomes: ever smoking, current daily smoking, persistent smoking, and intention to quit in six months among current smokers. Age, gender, race, education, income, geographic region, and occupational class (i.e. blue-collar, white-collar, service) were entered as predictors in all models. Age of onset of smoking was also included as a predictor for persistent smoking and intention to quit. Similar models were run to assess the effects of workplace rules limiting smoking and workplace smoking cessation programs as predictors of smoking behaviors. In a separate analysis, we compared the smoking behaviors listed above in construction workers versus all other blue-collar workers.
We also examined changes over time from 1992–2007 in the prevalence of ever smoking, current daily smoking, and persistent smoking in blue-collar, white-collar, service, and construction workers. Additionally, we assessed workplace smoking cessation programs and workplace rules limiting smoking among current daily smokers in the different occupational groups.
Analyses were conducted with SAS v9.2 and SUDAAN 10.0, using a Balanced Repeated Replications method to estimate variances and accommodate the complex sample design of the survey.11,12 All text and tables present weighted data. Associations between predictor variables and outcomes are reported as risk ratios rather than odds ratios, as the former are more easily interpreted as changes in average risk when outcomes are common.
RESULTS
The frequencies and distributions of the study population and various groupings of workers in the most recent CPS survey (2006–2007) are presented in Table 1. Data are based on 106,604 survey respondents who were 18–64 years old and had worked in the previous year. The workforce of the United States was 69% white, 54% male, 61% had at least some college education, and 50% had a combined household income over $50,000. Overall, 37% were ever smokers, 16% were current daily smokers, and 43% of ever smokers persisted as current daily smokers. Among current daily smokers 13% smoked more than 20 cigarettes per day, and 42% intended to quit in the next 6 months.
Table 1.
Sociodemographic and Smoking Characteristics of US Adults age 18–64: 2006–2007 Current Population Survey - Tobacco Use Supplement
| Sociodemographic / Smoking Characteristics | All Workers N=106,604 | White-Collar Workers N=67,565 | Service Workers N=16,576 | Blue-Collar Workers N=22,463 | Construction Workers+ N=6,418 |
|---|---|---|---|---|---|
| %, (95% CI) | %, (95% CI) | %, (95% CI) | %, (95% CI) | %, (95% CI) | |
| Age, years | |||||
| 18–24 | 14.0 (13.9–14.2) | 11.1 (10.9–11.4) | 23.7 (22.9–24.5) | 15.0 (14.4–15.6) | 17.7 (16.3–18.8) |
| 25–34 | 22.7 (22.6–22.9) | 22.7 (22.4–23.0) | 22.7 (22.0–23.3) | 22.8 (22.2–23.5) | 28.1 (26.6–29.1) |
| 35–44 | 25.0 (24.9–25.1) | 25.2 (24.9–25.5) | 22.6 (21.9–23.3) | 26.0 (25.4–26.6) | 25.0 (24.0–26.2) |
| 45–54 | 24.5 (24.4–24.7) | 25.7 (25.4–26.0) | 19.8 (19.2–20.5) | 24.6 (24.0–25.2) | 21.0 (20.0–22.5) |
| 55–64 | 13.7 (13.6–13.9) | 15.2 (15.0–15.5) | 11.2 (10.7–11.7) | 11.5 (11.0–11.9) | 8.2 (7.5–9.0) |
|
| |||||
| Gender (Male) | 53.6 (53.4–53.8) | 44.6 (44.2–45.0) | 42.4 (41.5–43.2) | 85.3 (84.9–85.8) | 97.0 (96.6–97.4) |
|
| |||||
| Race | |||||
| White | 68.6 (68.5–68.8) | 73.9 (73.6–74.3) | 57.2 (56.2–58.3) | 62.5 (61.8–63.3) | 61.1 (59.9–62.9) |
| Black | 11.2 (11.0–11.3) | 9.8 (9.5–10.0) | 16.7 (15.9–17.4) | 11.0 (10.5–11.5) | 5.4 (4.7–6.2) |
| American Indian/Alaskan | 0.5 (0.4–0.5) | 0.4 (0.3–0.4) | 0.6 (0.5–0.8) | 0.5 (0.4–0.6) | 0.6 (0.4–0.9) |
| Native | |||||
| Asian | 4.6 (4.5–4.7) | 5.6 (5.4. 5.8) | 3.8 (3.5–4.2) | 2.4 (2.1–2.6) | 0.8 (0.6–1.2) |
| Hawaiian/Pacific Islander | 0.2 (0.2–0.3) | 0.2 (0.2–0.3) | 0.3 (0.2–0.4) | 0.2 (0.2–0.3) | 0.3 (0.1–0.4) |
| Hispanic | 13.8 (13.7–13.9) | 9.0 (8.7–9.3) | 20.2 (19.3–21.0) | 22.2 (21.5–22.9) | 30.6 (28.7–31.8) |
| Multiracial | 1.2 (1.1–1.2) | 1.2 (1.1–1.3) | 1.2 (1.1–1.3) | 1.2 (1.0–1.3) | 1.2 (1.1–1.2) |
|
| |||||
| Educational Level | |||||
| < 4 years HS | 9.8 (9.5–10.1) | 3.4 (3.2–3.6) | 18.6 (17.7–19.4) | 20.8 (20.0–21.6) | 27.8 (26.2–28.9) |
| HS Diploma | 28.3 (27.9–28.7) | 19.6 (19.1–20.0) | 37.3 (36.4–38.2) | 45.5 (44.6–46.4) | 43.3 (41.8–44.7) |
| Some College | 20.0 (19.7–20.3) | 19.6 (19.2–20.0) | 23.5 (22.6–24.4) | 18.6 (17.9–19.2) | 16.1 (15.2–17.4) |
| College Degree | 41.2 (39.9–41.5) | 57.5 (57.0–58.0) | 20.6 (19.8–21.4) | 15.2 (14.6–15.8) | 12.7 (11.9–13.9) |
|
| |||||
| Household Income | |||||
| <$10,000 | 3.8 (3.6–4.0) | 2.4 (2.3–2.6) | 8.4 (7.8–9.0) | 4.2 (3.8–4.5) | 4.5 (3.8–5.4) |
| $10,000–29,999 | 16.3 (15.9–16.6) | 10.9 (10.5–11.2) | 28.0 (27.2–28.7) | 22.5 (21.7–23.3) | 24.8 (23.3–26.3) |
| $30,000–49,999 | 19.5 (19.1–19.8) | 16.9 (16.6–17.2) | 21.8 (21.0–22.5) | 24.7 (24.0–25.5) | 24.5 (23.0–25.9) |
| $50,000–74,999 | 20.0 (19.5–20.3) | 20.8 (20.4–21.3) | 15.5 (15.0–16.1) | 20.6 (20.0–21.3) | 19.0 (17.7–20.2) |
| >$75,000 | 30.1 (29.6–30.6) | 39.0 (38.4–39.5) | 15.1 (14.4–15.8) | 17.1 (16.4–17.9) | 16.1 (15.0–17.2) |
| Unknown | 10.4 (10.1–10.8) | 10.6 (10.2–11.5) | 11.2 (10.5–12.0) | 10.9 (10.2–11.5) | 11.1 (10.0–12.2) |
|
| |||||
| Geographic Region | |||||
| Northeast | 18.5 (18.4–18.7) | 19.6 (19.2–20.0) | 18.4 (17.7–19.0) | 15.9 (15.3–16.6) | 15.7 (14.4–16.5) |
| Midwest | 22.9 (22.7–23.1) | 22.7 (22.3–23.1) | 21.9 (21.1–22.7) | 24.1 (23.4–24.7) | 18.5 (17.4–19.7) |
| South | 35.6 (35.4–35.9) | 34.3 (33.8–34.8) | 36.1 (25.1–37.0) | 38.8 (37.9–39.7) | 40.9 (29.3–42.8) |
| West | 23.0 (22.8–23.2) | 23.5 (23.1–23.9) | 23.7 (22.8–24.6) | 21.2 (20.4–21.8) | 25.0 (23.5–26.5) |
|
| |||||
| Ever Smoking | 37.0 (36.6–37.4) | 33.3 (32.8–33.7) | 37.6 (36.7–38.5) | 46.4 (45.4–47.3) | 48.4 (46.8–50.0) |
|
| |||||
| Current Daily Smoking | 15.8 (15.5–16.1) | 11.7 (11.4–12.0) | 19.7 (18.8–20.5) | 24.0 (23.2–24.8) | 25.6 (24.5–27.1) |
|
| |||||
| Persistent Smoking* | 42.7 (42.1–43.3) | 35.2 (34.4–35.9) | 52.2 (50.5–53.1) | 51.8 (50.4–53.1) | 53.3 (51.1–55.5) |
|
| |||||
| Cigarettes per day among Current Daily Smokers** | |||||
| <11 | 36.6 (35.8–37.5) | 41.4 (40.2–42.6) | 41.6 (39.5–43.6) | 27.6 (26.0–29.2) | 23.5 (20.7–26.4) |
| 11 to 20 | 50.2 (49.4–51.0) | 49.5 (48.3–50.6) | 47.1 (45.1–49.0) | 52.9 (51.2–54.6) | 57.3 (54.2–60.3) |
| 21 to 29 | 7.8 (7.3–8.3) | 6.0 (5.5–6.5) | 7.1 (5.9–8.3) | 10.6 (9.6–11.5) | 10.0 (8.0–11.9) |
| >30 | 5.4 (5.0–5.8) | 3.1 (2.6–3.6) | 4.3 (3.4–5.2) | 8.9 (8.0–9.8) | 9.3 (7.5–11.0) |
|
| |||||
| Intend to quit in next 6 months among Current Daily Smokers** | 41.9 (40.9–42.9) | 46.0 (43.3–46.3) | 41.7 (38.7–43.7) | 38.6 (36.7–40.4) | 37.6 (34.8–40.5) |
|
| |||||
| Presence of Worplace Smoking Cessation Program** | 19.6 (19.2–20.0) | 23.0 (22.5–23.4) | 13.1 (12.3–13.9) | 14.7 (14.1–15.3) | 7.5 (6.4–8.7) |
|
| |||||
| Presence of Workplace Rules Limiting Smoking** | 88.9 (88.6–89.2) | 90.7 (90.4–91.0) | 86.4 (85.4–87.3) | 83.2 (82.1–84.2) | 67.8 (64.3–71.4) |
All Workers (n=41,591); White-Collar Workers (n=23,790); Service Workers (n=6775); Blue-Collar Workers (n=11,025); Construction/Extraction Workers (n=3274)
All Workers (n=17,109); White-Collar Workers (n=8072); Service Workers (n=3481); Blue-Collar Workers (n=5556); Construction/Extraction Workers (n=1681)
Construction Workers are a subset of Blue-Collar Workers
Differences across occupational groups
Compared to white-collar workers, blue-collar workers were more likely to be male (85% vs., 45%), less likely to have a college degree (15% vs. 58%), and less likely to earn above $50,000 annually (38% vs. 60%). A higher proportion of blue-collar workers had initiated smoking (46% vs. 33% reported ever smoking), and of those who had ever been smokers, a higher proportion continued smoking as current daily smokers (52% vs. 35%). This higher prevalence of initiation, coupled with a higher rate of persistent smoking, resulted in a higher rate of current daily smokers in blue-collar workers compared to white-collar (39% versus 12%). Among current daily smokers, 20% of blue-collar workers vs. 9% of white-collar workers smoked more than 20 cigarettes per day. Thus, blue-collar workers were more likely to start smoking, more likely to keep smoking, and more likely to smoke more heavily. Among blue-collar workers, 39% of current daily smokers intended to quit in the next 6 months, compared to 46% of white-collar current daily smokers.
Service workers were mostly female (58%), and the lowest paid of the three groups (69% earned less than $50,000 annually). Current smoking (20%) was intermediate between that of blue- and white-collar workers. Interestingly, while initiation of smoking was similar to that of white-collar workers (38% of service workers were ever smokers), persistence of smoking was similar to that of blue-collar workers (52% of ever smokers were current daily smokers).
Effects of Occupational Group after Adjustment for Individual Factors
Table 2 shows the results of multivariate logistics models for each of our four primary outcomes: ever smoking, current daily smoking, persistent smoking, and intent to quit in the next 6 months among current smokers. Being older, white, male, less educated, and poorer were associated with being an ever smoker. Blue-collar and service workers were more likely than white-collar workers to be ever smokers, even after adjustment for all available demographic factors. Being younger, white, male, less educated, and poorer were associated with being a current daily smoker. Blue-collar and service workers were more likely than white-collar workers to be current daily smokers after controlling for these other risk factors.
Table 2.
Multiple Logistic Regressions Comparing Smoking Behaviors as Outcomes Between Different Occupational Groupings*
| Characteristic | Ever Smoking N= 106,604 | Current Daily Smoking N=106,604 | Persistent Smoking | Intention to Quit N=17,109 | ||
|---|---|---|---|---|---|---|
| Model 1 N=41,591 | Model 2 N=24,439 | Model 3 N=29,420 | ||||
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Age, years | ||||||
| 18–24 | 0.53 (0.51–0.56) | 1.02 (0.94–1.10) | 1.77 (1.66–1.89) | 1.76 (1.64–1.89) | 1.67 (1.56–1.79) | 1.06 (0.97–1.16) |
| 25–34 | 0.75 (0.72–0.77) | 1.35 (1.26–1.44) | 1.68 (1.60–1.78) | 1.68 (1.57–1.80) | 1.60 (1.51–1.69) | 1.09 (1.00–1.20) |
| 35–44 | 0.74 (0.71–0.76) | 1.33 (1.25–1.42) | 1.68 (1.59–1.78) | 1.70 (1.60–1.82) | 1.62 (1.53–1.73) | 1.12 (1.04–1.20) |
| 45–54 | 0.89 (0.86–0.91) | 1.39 (1.30–1.50) | 1.49 (1.40–1.58) | 1.50 (1.41–1.60) | 1.46 (1.37–1.56) | 1.04 (0.96–1.12) |
| 55–64 | 1 | 1 | 1 | 1 | 1 | 1 |
|
| ||||||
| Gender (Female) | 0.85 (0.83–0.86) | 0.91 (0.88–0.95) | 1.06 (1.03–1.09) | 1.07 (1.03–1.12) | 1.08 (1.04–1.12) | 1.02 (0.97–1.07) |
|
| ||||||
| Race | ||||||
| White | 1 | 1 | 1 | 1 | 1 | 1 |
| Black | 0.55 (0.53–0.57) | 0.47 (0.44–0.51) | 0.91 (0.86–0.97) | 0.90 (0.83–0.98) | 0.92 (0.86–0.99) | 1.20 (1.11–1.30) |
| Am. Ind/Alaskan Native | 1.06 (0.92–1.21) | 1.02 (0.82–1.27) | 0.99 (0.85–1.15) | 1.04 (0.86–1.25) | 1.05 (0.90–1.23) | 0.91 (0.69–1.20) |
| Asian | 0.54 (0.50–0.58) | 0.51 (0.44–0.58) | 1.04 (0.94–1.16) | 1.02 (0.89–1.17) | 1.04 (0.92–1.17) | 0.76 (0.62–0.93) |
| Hawaiian/Pacific Islander | 0.80 (0.64–0.99) | 0.97 (0.65–1.44) | 1.21 (0.95–1.55) | 1.17 (0.81–1.69) | 1.15 (0.87–1.51) | 1.24 (0.81–1.91) |
| Hispanic | 0.46 (0.44–0.48) | 0.25 (0.22–0.28) | 0.58 (0.53–0.63) | 0.63 (0.56–0.70) | 0.58 (0.53–0.64) | 0.99 (0.90–1.09) |
| Multiracial | 1.11 (1.02–1.19) | 1.26 (1.09–1.45) | 1.13 (1.03–1.24) | 1.12 (0.97–1.29) | 1.11 (0.99–1.24) | 1.15 (1.00–1.32) |
|
| ||||||
| Educational Level | ||||||
| < 4 yrs HS | 1.62 (1.56–1.68) | 3.12 (2.92–3.33) | 1.78 (1.70–1.86) | 1.84 (1.72–1.98) | 1.70 (1.62–1.78) | 0.81 (0.73–0.89) |
| Graduated HS | 1.52 (1.48–1.67) | 2.52 (2.38–2.66) | 1.61 (1.55–1.67) | 1.64 (1.57–1.71) | 1.53 (1.47–1.59) | 0.88 (0.83–0.93) |
| Some College | 1.40 (1.36–1.44) | 1.91 (1.81–2.01) | 1.36 (1.30–1.42) | 1.41 (1.34–1.48) | 1.35 (1.29–1.41) | 0.99 (0.93–1.06) |
| College Degree | 1 | 1 | 1 | 1 | 1 | 1 |
|
| ||||||
| Income | ||||||
| < $10,000 | 1.45 (1.38–1.53) | 2.46 (2.22–2.72) | 1.64 (1.51–1.77) | 1.69 (1.53–1.88) | 1.61 (1.46–1.77) | 0.85 (0.75–0.98) |
| $10,000–29,999 | 1.36 (1.32–1.40) | 2.14 (2.00–2.29) | 1.52 (1.45–1.60) | 1.58 (1.49–1.68) | 1.46 (1.38–1.54) | 0.90 (0.84–0.96) |
| $30,000–49,999 | 1.27 (1.24–1.31) | 1.82 (1.71–1.94) | 1.39 (1.32–1.47) | 1.45 (1.36–1.54) | 1.37 (1.29–1.44) | 0.94 (0.87–1.01) |
| $50,000–74,999 | 1.15 (1.12–1.18) | 1.41 (1.31–1.51) | 1.21 (1.14–1.28) | 1.24 (1.16–1.33) | 1.20 (1.13–1.27) | 1.02 (0.95–1.10) |
| Unknown | 0.94 (0.91–0.98) | 1.34 (1.24–1.46) | 1.36 (1.27–1.45) | 1.37 (1.27–1.48) | 1.30 (1.21–1.40) | 0.77 (0.68–0.86) |
| >$75,000 | 1 | 1 | 1 | 1 | 1 | 1 |
|
| ||||||
| Geographic Region | ||||||
| Northeast | 1.00 (0.97–1.04) | 0.92 (0.87–0.98) | 0.93 (0.89–0.97) | 0.91 (0.85–0.96) | 0.91 (0.86–0.96) | 1.07 (0.99–1.15) |
| South | 0.95 (0.92–0.98) | 0.98 (0.94–1.03) | 1.04 (1.00–1.07) | 1.03 (0.98–1.08) | 1.02 (0.98–1.07) | 0.89 (0.83–0.95) |
| West | 0.92 (0.89–0.95) | 0.79 (0.74–0.83) | 0.87 (0.83–0.91) | 0.87 (0.82–0.92) | 0.88 (0.84–0.92) | 1.00 (0.93–1.07) |
| Midwest | 1 | 1 | 1 | 1 | 1 | 1 |
|
| ||||||
| Age Started Smoking | ||||||
| <15 | --- | --- | 1 | 1 | 1 | 1 |
| 15–16 | --- | --- | 0.95 (0.90–0.99) | 0.96 (0.90–1.02) | 0.96 (0.91–1.01) | 0.99 (0.92–1.07) |
| 17–18 | --- | --- | 0.89 (0.85–0.93) | 0.89 (0.84–0.93) | 0.89 (0.85–0.94) | 1.06 (0.98–1.14) |
| >19 | --- | --- | 0.94 (0.90–0.99) | 0.95 (0.89–1.01) | 0.95 (0.90–1.00) | 1.19 (1.12–1.27) |
|
| ||||||
| Occupation Class 1 | ||||||
| Service | 1.07 (1.04–1.10) | 1.25 (1.18–1.32) | 1.15 (1.10–1.20) | 1.18 (1.12–1.24) | 1.18 (1.12–1.24) | 0.99(0.92–1.06) |
| Blue-Collar | 1.18 (1.15–1.22) | 1.41 (1.34–1.49) | 1.19 (1.14–1.24) | 1.17 (1.10–1.24) | 1.21 (1.15–1.27) | 0.94 (0.88–1.01) |
| White-Collar | 1 | 1 | 1 | 1 | 1 | 1 |
|
| ||||||
| Lack of Workplace Rules | --- | --- | --- | 1.09 (1.03–1.17) | --- | --- |
|
| ||||||
| Lack of Cessation Program | --- | --- | --- | --- | 1.14 (1.10–1.19) | --- |
Each model includes all predictor variables listed in the table with the following exceptions: Age Started Smoking was not entered as a predictor for Ever Smoking and Current Daily Smoking; Workplace Rules was only entered as a predictor for Persistent Smoking Model 2; Cessation Program was only entered as a predictor for Persistent Smoking Model 3.
Persistence of smoking (current daily smoking among ever smokers) was predicted by being younger, white, female, less educated, poorer, and having started smoking at an earlier age. Again, blue-collar workers and service workers were more likely than white-collar workers to be current daily smokers (see Persistent Smoking, Model 1).
Intention to quit smoking in the next six months was associated with being more educated and having a higher income. Occupational group had no effect on intention to quit after adjustment for demographic factors.
Construction Workers
Among survey respondents, 6418 (6%) were construction workers (See Table 1). Construction workers were predominantly male (97%), and more likely to be Hispanic (30% compared to 13% for all other occupations). The prevalence of all smoking behaviors (i.e. ever smoking, current daily smoking, and persistent smoking) was higher in construction workers compared to workers in all other blue-collar occupational groups (Table 3). When compared to all other occupational groups, construction workers ranked highest in ever smoking (48% compared to 39% for all other occupations combined p<0.0001), and current daily smoking (25.8% compared to 15.1% for all other occupations combined p<0.0001). Construction workers had the third highest rate of persistent smoking behind Food Preparation and Serving occupations (59%) and Healthcare Support occupations (54%), (Table 3) with significantly higher rates of persistent smoking compared to all other occupations combined (53.3% vs. 41.7%, p<0.0001)
Table 3.
Smoking rates for major occupational groups
| CPS Occupation Description* | N | % Ever Smoker (95% CI) | % Current Daily Smoker (95% CI) | % Persistent Smoker(95% CI) | |
|---|---|---|---|---|---|
| White-collar | Management Occupations | 11812 | 36.9 (36.0–37.9) | 11.7 (10.9–12.4) | 31.6 (29.7–33.5) |
| Business and financial operations occupations | 4895 | 32.0 (30.6–33.4) | 9.8 (8.9–10.7) | 30.7 (28.4–33.0) | |
| Computer and mathematical science occupations | 2584 | 30.6 (28.7–32.6) | 7.8 (6.7–8.9) | 25.4 (22.1–28.7) | |
| Architecture and engineering occupations | 2135 | 29.0 (26.5–31.4) | 7.2 (6.0–8.5) | 24.9 (21.1–28.8) | |
| Life, physical, and social science occupations | 1273 | 27.3 (24.1–30.4) | 6.8 (5.0–8.6) | 25.0 (19.5–30.5) | |
| Community and social service occupations | 1893 | 29.0 (26.3–31.7) | 9.3 (7.6–11.0) | 31.1 (27.3–36.9) | |
| Legal occupations | 1321 | 31.6 (28.8–34.3) | 7.2 (5.5–8.9) | 22.8 (17.6–28.1) | |
| Eductation, training, and library occupations | 7143 | 23.5 (22.4–24.5) | 5.2 (4.6–5.8) | 22.1 (19.7–24.5) | |
| Arts, design, entertainment, sports, and media occupations | 2168 | 33.8 (31.1–36.5) | 9.4 (7.4–10.8) | 27.6 (24.0–31.3) | |
| Healthcare practitioner and technical occupations | 5769 | 26.4 (25.1–27.7) | 8.1 (7.3–8.9) | 30.6 (27.9–33.2) | |
| Sales and related occupations | 11161 | 37.0 (36.0–38.0) | 16.0 (15.2–16.9) | 43.3 (41.6–45.0) | |
| Office and administrative support occupations | 15411 | 36.9 (36.0–37.8) | 15.9 (15.1–16.6) | 43.0 (41.6–44.5) | |
|
| |||||
| Service | Healthcare support occupations | 2526 | 36.8 (34.5–39.0) | 19.9 (18.1–21.6) | 54.0 (50.6–57.3) |
| Protective service | 2084 | 33.5 (31.3–35.7) | 13.3 (11.5–15.1) | 39.6 (35.2–44.0) | |
| Food preparation and serving related occupations | 4701 | 40.9 (39.2–42.5) | 24.3 (22.6–25.9) | 59.5 (56.8–62.1) | |
| Building and grounds cleaning and maintenance occupations | 3727 | 38.9 (37.0–40.8) | 20.2 (18.7–21.6) | 51.9 (49.1–54.7) | |
| Personal care and service occupations | 3538 | 34.6 (32.7–36.5) | 16.2 (14.7–17.6) | 46.8 (43.3–50.2) | |
|
| |||||
| Blue-collar | Construction and extraction occupations | 6418 | 48.4 (46.8–50.0) | 25.6 (24.5–27.1) | 53.3 (51.1–55.5) |
| Installation, maintenance, and repair occupations | 3652 | 47.9 (46.0–49.7) | 24.6 (22.8–26.4) | 51.4 (48.6–54.2) | |
| Production occupations | 6755 | 44.3 (42.9–45.7) | 22.7 (21.4–24.0) | 51.2 (49.0–54.2) | |
| Transportation and material moving occupations | 5638 | 45.4 (43.9–47.0) | 23.1 (21.8–24.3) | 50.8 (48.5–53.0) | |
|
| |||||
| TOTAL -all occupations combined | 106,604 | 37.0 (36.6–37.4) | 15.8 (15.5–16.1) | 42.7 (42.1–43.3) | |
Standard Occupational Classification System
Compared to other occupations, construction workers began smoking at an earlier age (78% by age 18 vs. 71%), smoked more (18% smoke 20 or more cigarettes per day vs. 16%), had fewer quit attempts in their lifetime (62% vs. 66%), had fewer quit attempts in last 12 months (34% vs. 36%), and fewer intended to quit in the next 6 months (40% vs. 45%). As shown in Table 1, these higher rates of current daily smoking and higher maintenance of smoking among construction workers were accompanied by markedly lower rates of availability of workplace smoking cessation programs and less frequent rules against workplace smoking. Due to the survey design, the question on rules against workplace smoking was only asked for those who reported working primarily indoors (17.7% of construction workers worked indoors vs. 71.3% of other workers). After adjustment for all other factors, construction workers were more likely to be current daily smokers than other blue-collar workers (RR=1.14, 1.07 – 1.21).
Effects of Workplace Smoking Cessation Programs and Workplace Rules Limiting Smoking
The effects of workplace smoking policies on persistent smoking are presented in Table 2. Persistent smoking model 2 includes all demographic factors as predictors plus lack of workplace smoking rules as an additional predictor. The absence of a workplace rules limiting smoking was associated with being a current daily smoker (RR=1.09, 1.03 – 1.17). Similarly, model 3 includes demographic factors plus the lack of workplace cessation program, which was also associated with persistent smoking (RR=1.14, 1.10 – 1.19).
We also assessed the effects of workplace policies on current daily smoking and intention to quit. Across the working population as a whole, the absence of workplace rules limiting smoking was strongly associated with being a current daily smoker (RR=1.32, 1.22 – 1.42) after adjustment for all other factors. Additionally, the absence of a workplace smoking cessation program was associated with a lower probability of intention to quit in the next six months (RR=0.85, 0.80 – 0.90) after adjustment for all other factors. The full results of these models are not presented in the table; however, the addition of these predictors did not significantly change the risk ratios of the other factors in the model.
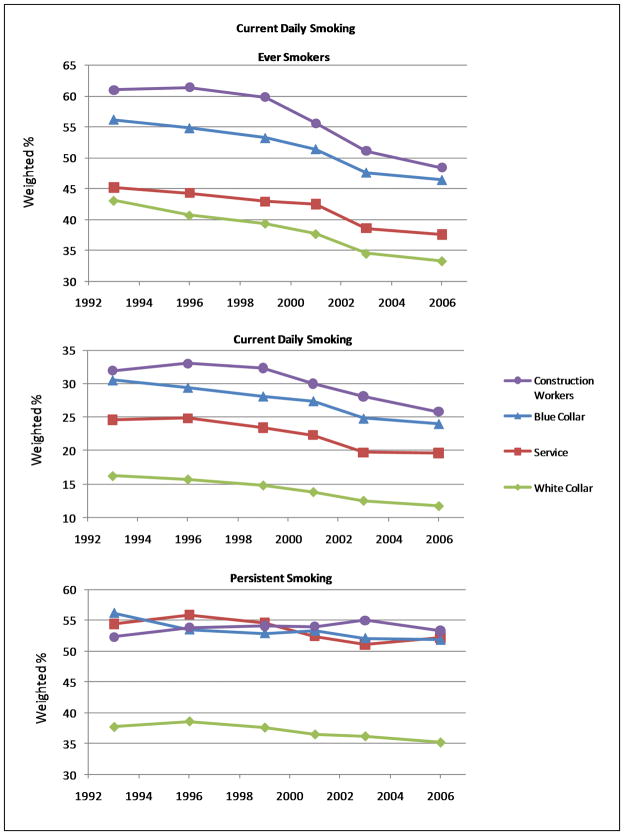
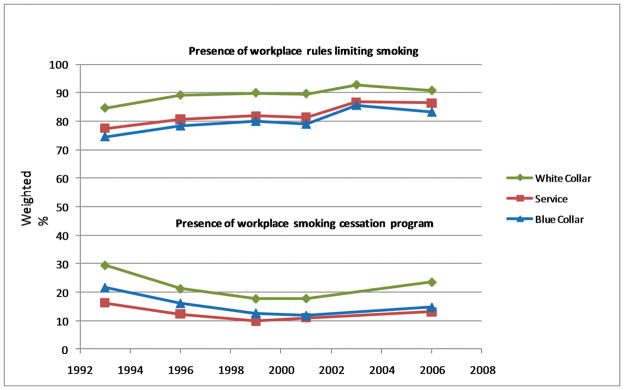
Time Trends
Figure 1 shows the pattern of decline of smoking initiation (i.e. ever smoking), current daily smoking, and current daily smoking among ever smokers across all occupational groups. Construction and blue-collar workers reported the highest rates of ever smoking and current daily smoking at all time points and white-collar workers reported the lowest rates. Service workers were more similar to white-collar workers in smoking initiation, but closer to blue-collar workers in current daily smoking. Among ever smokers, the prevalence of current daily smoking was substantially lower among white-collar workers, indicating greater success in smoking cessation among white-collar workers. Figure 2 shows that more white-collar workers had rules limiting smoking at work, and were offered workplace cessation programs more often than service and blue-collar workers.
Figure 1.
Smoking behaviors by occupational group 1993 – 2006
Figure 2.
Workplace smoking policies by occupational group 1993 – 2006
DISCUSSION
Our results highlight several important trends. Consistent with other studies, demographic factors including age, race, gender, educational level, and income influenced the prevalence of being a current smoker. Additionally, we show that these same factors are associated with being an ever smoker and with persistence of smoking among ever smokers. Thus, the prevalence of current daily smoking is a function of factors that influence both initiation of smoking (ever smokers) and the persistence of smoking (current daily smokers among ever smokers).
Importantly, our analyses showed that workplace rules limiting smoking and workplace smoking cessation programs were strong predictors of smoking among workers. Across all occupational groups, the absence of workplace rules limiting smoking was associated with higher rates of current daily smoking and with the persistence of smoking. Though smokers may self-select to workplaces that allow smoking, it is also likely that such rules discourage smoking among those who would otherwise smoke, due to the inconvenience or stigma created by the rules. The absence of a workplace smoking cessation program was associated with a higher probability of persistent smoking and with a lower likelihood of an intent to quit, suggesting that workplace smoking cessation programs are useful in helping smokers to quit. Our findings are consistent with previous studies which found that people who worked in places with smoke-free policies were 1.9 – 2.3 times more likely to quit smoking than those whose worksites permitted smoking.13, 14 The last study to examine this issue in a nationally representative sample used the 1992 – 93 CPS-TUS data and found that smoke-free worksites were effective in reducing smoking in nearly all industries.15 More than a decade later, our study found that workplace rules against smoking and workplace smoking cessation programs continue to be a major determinant of persistent smoking; the lower availability of such worksite measures for blue-collar and service workers may in part explain health disparities in smoking.
When comparing the three broad occupation categories of blue-collar, white-collar, and service workers, several themes emerged. Consistent with other studies, blue-collar workers tended to smoke the most with service workers second. This holds true for ever smoking, current daily smoking, and persistent smoking. Even after controlling for demographic risk factors, white-collar workers were less likely to initiate smoking (lower prevalence of ever smokers), and were more likely to quit smoking (lower prevalence of persistent smoking). However, intent to quit was similar among the 3 groups of workers. While current smokers across all occupations intend to quit, white-collar workers are likely to have better resources and support, or greater cultural stigmatization of smoking, leading white-collar workers to more success in quitting than blue-collar and service workers. These data indicate that there are important differences between occupational groups that cannot be explained by the sociodemographic factors available for this study.
The role of cultural norms in different occupational groups has been little studied, and may represent a persistent health disparity that drives smoking behaviors. The high prevalence of smoking seen in construction workers can be partly contributed to the workplace culture of the construction industry. Smoking is generally tolerated on construction worksites - data from the 1992 – 93 CPS-TUS showed that among all occupations studied, construction trade workers had one of the lowest rates of smoke-free policies at work and one of the highest rates of smoking.16 Furthermore, most contractors are small, worksites are scattered, and workers frequently change employers, making traditional employer-based smoking cessation programs infeasible. Individual or social culture may also vary by occupational group and be tied to smoking behaviors. Smoking initiation usually occurs before people enter the workforce, yet there are large occupational discrepancies in the prevalence of ever smokers. Sorenson et al. proposes using a social-contextual model that incorporates individual, interpersonal, organizational (i.e. workplace), community, and societal factors in designing effective interventions.17 Examples of organizational factors that may influence smoking are job stress, hazardous working conditions, pace of work, and the meaning of smoking among workers. Smoking cessation efforts in construction workers and other high risk occupational groups may be more effective if they take into account the worksite culture and the social context of the individual workers.18
Our data suggest that occupational disparities in smoking behaviors are in some cases widening. Although the prevalence of ever smokers has declined steadily across all groups since 1992 (Figure 1), prevalence of current daily smoking has declined more quickly among white-collar workers than among service- and blue-collar workers. The prevalence of current smokers among ever smokers (Figure 1) is significantly higher and trending down less among blue-collar and service workers than in white-collar workers, indicating more persistence among the blue-collar and service groups. The greater success of white-collar workers in quitting smoking is particularly striking when compared with the trends shown in Figure 2: white-collar workers have greater access to workplace smoking cessation programs and more frequently have workplace rules limiting smoking.
The occupational disparities in smoking behaviors observed in our study and others19 point toward opportunities to target specific populations with high smoking prevalence through worksite tobacco control programs. By providing the opportunity to target high-risk populations, worksite tobacco control programs may be more effective than community-based efforts, constituting an important link between occupational health and public health by facilitating strategies “to reach hitherto untouched groups of smokers.”20. In addition to the public health benefits of smoking cessation, several studies report that employer provision of workplace smoking cessation benefits results in substantial health and economic gains to the employer, with economic savings exceeding the cost of the benefit within a relatively short period.21–22 While many employers have initiated smoking cessation benefits, such benefits are not distributed equally across all occupational categories – as noted above, our study shows that smoking cessation benefits are least available to worker groups with the highest rates of smoking.
There are several limitations of our study. The CPS-TUS is based on self report, and it is possible that there is differential reporting by occupational group. Due to the skip patterns in the survey, only the 17.7% of construction workers who worked indoors were asked about workplace rules limiting smoking; these data probably overestimate the prevalence of workplace smoking rules in construction workers, as those working outdoors are even less likely to have restrictions. The classification of occupations to occupational groupings can be arbitrary; we used a standard occupational schema based on a national coding system that has been used in other smoking studies. This study examined differences in smoking between very broad occupational categories, and it is likely that more detailed examination of occupational groups will yield even more differences than observed here. Within each of the broad occupational groups described in our study, there are distinct subgroups with higher and lower smoking rates; we have highlighted one group with particularly heavy smoking, construction workers.
The strengths of our study included a large sample size, analysis of multiple outcomes including initiation of smoking, intent to quit, current daily smoking in the entire population, current daily smoking among ever smokers, and number of cigarettes per day. We also used multiple predictors of smoking behaviors, including the presence of a smoking cessation program at work and the presence of workplace rules limiting smoking. We analyzed smoking trends over multiple time points including the most recent CPS-TUS, and provided data on one particularly high risk group of workers, those in construction and extraction industries.
After controlling for known risk factors for smoking, including age, race, gender, income, education, and geographic region, we found that the presence of smoking cessation programs at work and the presence of workplace rules limiting smoking reduced smoking behaviors. We also found differences in smoking behaviors between different occupational groups that were not accounted for by other risk factors. These occupational differences may be related to the culture within different occupational groups and should be taken into account when considering efforts to decrease smoking initiation and increase smoking cessation. Disparities in health and health behaviors are usually couched in terms of race, gender, income, or education. Our study suggests that cultural factors within occupational groups are also important determinants of health disparities. Workplace health initiatives will not be maximally effective unless they target the groups at highest risk and take into account cultural differences between worker groups.
Acknowledgments
This work was supported by grants from the National Cancer Institute P50CA095815 (PI - Kreuter), and P01 CA89392 (PI - Bierut); from the National Institute on Drug Abuse K02 DA21237 (PI -Bierut); and from the National Center for Research Resources UL1 RR024992 (PI – Evanoff).
Footnotes
Financial Disclosures: Dr. LJ Bierut, is listed as an inventor on a patent (US 20070258898) covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction. Dr. Bierut has acted as a consultant for Pfizer, Inc. in 2008.
References
- 1.Cigarette smoking among adults - United States, 2004. MMWR. 2005;54(44):1121–1142. [PubMed] [Google Scholar]
- 2.Smoking-attributable mortality, years of potential life lost, and productivity loses - United States, 2000–2004. MMWR. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- 3.Smith D. Tobacco smoking by occupation in Australia and the United States: a review of national surveys conducted between 1970 and 2005. Ind Health. 2008;46(1):77–89. doi: 10.2486/indhealth.46.77. [DOI] [PubMed] [Google Scholar]
- 4.Giovino GA, Pederson LL, Trosclair A. The prevalence of selected cigarette smoking behaviors by occupational class in the United States. Work, Smoking, and Health: A National Institute of Occupational Safety and Health (NIOSH) Scientific Workshop; Washington DC: NIOSH; 2000. [Google Scholar]
- 5.Barbeau E, Krieger N, Soobader M. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health. 2004;94(2):269–278. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee D, Fleming L, Arheart K, et al. Smoking rate trends in U.S. occupational groups: the 1987 to 2004 National Health Interview Survey. J Occup Environ Med. 2007;49(1):75–81. doi: 10.1097/JOM.0b013e31802ec68c. [DOI] [PubMed] [Google Scholar]
- 7.Construction Chart Book. CPWR – The Center for Construction Research and Training. (4) 2008 Available at: http://www.cpwr.com/rp-chartbook.html.
- 8.Current Population Survey. 1992–2007 Technical Documentation. 2007 Retrieved July 15, 2009 from www.census.gov/aspd/techdoc/cps/cps-main.html.
- 9.U.S. Census Bureau and Bureau of Labor Statistics. Design Methodology: Current Population Survey. Technical Paper. :66. Retrieved July 15, 2009 from www.census.gov/prod/2006pubs/tp-66.pdf.
- 10.United States Department of Labor. Standard Occupational Classification System. Available at: http://www/bls.gov/SOC/
- 11.SAS Institute. SAS, v9.2. Cary, NC: SAS Institute; 2009. [Google Scholar]
- 12.Research Triangle Institute. SUDAAN Language Manual, Release 10.0. Research Triangle Park, NC: Research Triangle Institute; 2008. [Google Scholar]
- 13.Bauer J, Hyland A, Li Q, Steger C, Cummings M. A longitudinal assessment of the impact of smoke-free worksite policies on tobacco use. Am J Public Health. 2005;95(6):1024–1029. doi: 10.2105/AJPH.2004.048678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shields M. Smoking bans: influence on smoking prevalence. Health Reports (Statistics Canada, Catalogue 82–003) 2007;18(3):9–24. [PubMed] [Google Scholar]
- 15.Farrelly M, Evans W, Sfekas A. The impact of workplace smoking bans: results from a national survey. Tob Control. 1999;8:272–277. doi: 10.1136/tc.8.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gerlach K, Shopland D, Hartman A, Gibson JT, Pechacek TF. Workplace smoking policies in the United States: results from a national survey of more than 100 000 workers. Tob Control. 1997;6:199–206. doi: 10.1136/tc.6.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorensen G, Barbeau E, Hunt M, Emmons K. Reducing social disparities in tobacco use: a social-contextual model for reducing tobacco use among blue-collar workers. Am J Public Health. 2004 Feb;94(2):230–239. doi: 10.2105/ajph.94.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barbeau E, Li Y, Calderon P, et al. Results of a union-based smoking cessation intervention for apprentice iron workers (United States) Cancer Cause Control. 2006 Feb;17(1):53–61. doi: 10.1007/s10552-005-0271-0. [DOI] [PubMed] [Google Scholar]
- 19.Smith DR, Leggat PA. Tobacco smoking by occupation in Australia: results from the 2004 to 2005 National Health Survey. J Occup Environ Med. 2007;49:437–45. doi: 10.1097/JOM.0b013e3180430134. [DOI] [PubMed] [Google Scholar]
- 20.Smith DR. Workplace tobacco control: the nexus of public and occupational health. Public Health. 2009;123:817–9. doi: 10.1016/j.puhe.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 21.Halpern MT, Dirani R, Schmier JK. Impacts of a smoking cessation benefit among employed populations. J Occup Environ Med. 2007;49:11–21. doi: 10.1097/JOM.0b013e31802db579. [DOI] [PubMed] [Google Scholar]
- 22.Ryan PJ, Forster NJ, Holder D. Evaluation of a worksite smoking-cessation program. J Occup Environ Med. 2002;44:703–4. doi: 10.1097/00043764-200208000-00001. [DOI] [PubMed] [Google Scholar]