Abstract
Objective
To investigate the association between multimorbidity – a construct comprised of several health domains (medical comorbidity, musculoskeletal, physical and social functional status, mental health, geriatric problems) – and overall self-rated health, an important chronic disease health outcome. We investigate whether medical comorbidity effects are mediated through other health domains and whether these domains have independent effects on self-rated health.
Study Design and Setting
Medicare recipients (n=958) completed a questionnaire 3 years post primary total hip replacement surgery. Self-reported sociodemographic characteristics, self-rated health, and health domain statuses were ascertained. Probit regressions and path analyses were used to evaluate the independent effects of the health domains on self-rated health, the inter-relationships between domains, and to quantify direct and mediated effects.
Results
All domains were independently associated with self-rated health. Medical comorbidity explained 11.7% of the variance in self-rated health and all other health domains explained 27.3%. The impact of medical comorbidity was largely direct (only 21.5% mediated through other domains). Medical comorbidity minimally explained the variance in other domain scores.
Conclusion
Self-rated health has multiple determinants. This finding suggests that an exclusive focus on any one domain in health research may limit researchers' ability to understand health outcomes for which self-rated health is predictive.
Keywords: burden of illness, comorbidity, self-rated health, health status, osteoarthritis, multimorbidity
INTRODUCTION
The literature has identified a number of health domains that influence both short- and long-term health outcomes. We will refer to multimorbidity as the co-occurrence of states or situations related to these health domains and refer to the collective impact of multimorbidity as the `aggregate health burden'. While work to date has focused predominantly on the domain of medical comorbidity (the co-occurrence of one or more diseases beyond an index disease [1]), other health domains, particularly physical and social functioning and mental health, have also been shown to have significant effects on outcomes [2–6]. In this study, we consider multimorbidity (medical comorbidity, musculoskeletal, general physical and social functioning, geriatric problems and mental health) and associated aggregate health burden and its association with self-rated health. Self-rated health has been shown to predict a range of outcomes, including morbidity [7–10], health care utilization [7;11;12], hospitalizations [7;11;13], and mortality [14–16], over varied time periods and after controlling for morbidity, health behaviours, and access to health services. And, importantly, assessing the inter-relationship between a number of health domains and their association with self-rated health permits a conceptual understanding of health from the patient's perspective.
The study is undertaken using a cohort of individuals who underwent a total hip replacement for osteoarthritis 3 years prior. Osteoarthritis is the most common joint disorder in the world, with significant impacts on functioning, disability and health care utilization [17–19]. It has also been reported that people with osteoarthritis experience concomitant medical conditions more often than age and sex matched peers in the general population [20–22], and that disability rises markedly with the number of coexistent medical conditions [23–25].
In this study, path analysis with probit regression is used to evaluate the inter-relationships between the health domains and to quantify the direct and mediated (indirect) effects of medical comorbidity on self-rated health considering these other relevant health domains.
METHODS
Study Sample
Analysis was based on a 3-year post-surgical survey of Medicare beneficiaries aged ≥65 years that underwent elective primary total hip replacement for osteoarthritis from July 1995 through June 1996. Recruitment details have been published [26].
Briefly, a 2-stage stratified random sample of 1,939 patients from 3 U.S. states (Colorado, Pennsylvania, and Ohio) was selected from a cohort of 7,092 who had primary total hip replacement. 32 died prior to contact and addresses were incorrect for 20. 519 never responded, 338 refused participation and 1,030 agreed to participate. Of these, 958 returned their questionnaire. Respondents were younger than non-respondents, and response rates were greater among white patients and those with higher incomes.
Study measures
Self-rated health
Patients were asked, “In general, how would you rate your health?” “Excellent; Very good; Good; Fair; or Poor.” Responses were scored 1 to 5.
Medical comorbidity count
Patients identified chronic diseases experienced in the last 10 years (stroke; cancer; heart attack; congestive heart failure; high blood pressure; diabetes; kidney disease; asthma, bronchitis, emphysema, or other lung disease; ulcer or stomach disease; anemia or other blood disease; rheumatoid arthritis). An unweighted summative index was calculated [27].
Musculoskeletal functional limitations
Patients reported whether their activities were limited by problems in 6 anatomic regions: hands, wrists, arms or shoulders; neck; back; hips; knees; ankles or feet [28]. Responses were summed, with scores ranging from 0–6.
Physical functioning
Concerning problems with work or daily activities as a result of physical health, patients were asked how much time “…have you accomplished less than you would like?” and “…were you limited in the kind of work or other activities you could do?”
Social functioning
Patients were asked how much time their physical health or emotional problems interfered with their social activities. For physical and social functioning, patients indicated: 4-All of the time; 3-Most of the time; 2-Some of the time; 1-A little of the time; or 0-None of the time. Responses were summed, and scores ranged from 0–8 and 0–4, respectively.
Mental health was assessed using the mental health inventory from the SF-36 Health Survey [29]. Scores ranged from 0–20. Scores for physical and social functioning and mental health were standardized to a 0–100 scale.
Geriatric problems [30] were recorded as memory problems or confusion; vision problems; hearing problems; falling down; difficulty controlling bowel or bladder; and poor balance. Positive responses were summed; scores ranged from 0–6.
For all measures, higher scores represented worse health/greater severity. The survey also elicited data on Age, Household Income (low (<$20,000); middle ($20,000–$50,000); high (>$50,000); missing (20.6% of sample)), Educational Attainment (<high school; high school; some college; 4-year college), and height and weight (from which body mass index (kg/m2) was calculated.
Analysis
Overall distributions were examined. Bivariate analyses examined health measure scores by self-rated health status.
Recognized as a proxy for an underlying continuous distribution, self-rated health was treated ordinaly and probit regression analyses employed. Analyses adjusted for age, sex, income, education, and body mass index. Initially, simple probit regressions evaluated the association between medical comorbidity count and self-rated health, followed by the addition of physical, social and musculoskeletal functional limitations, mental health and geriatric problems into the model.
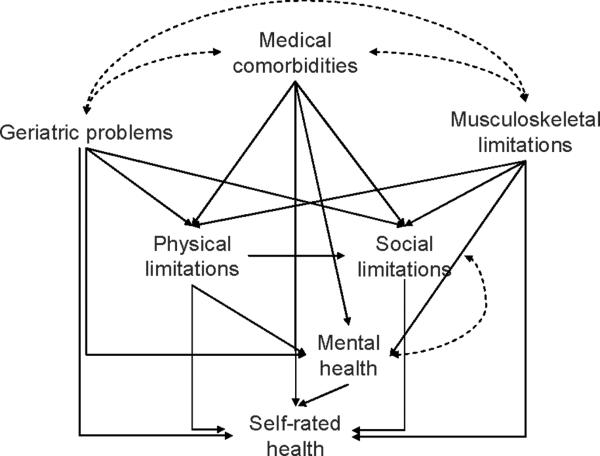
The hypothesis of a mediated effect of medical comorbidity on self-rated health through other health domains was assessed via path analysis (Figure 1). The directionality of effects was based on findings from the literature [2–6;31–34]. Where the literature suggested bi-directional effects, domains were specified to covary.
Figure 1.
Hypothesized path model (sociodemographic and body mass index effects not shown).
Different indices provide different information about model fit. Four indices were considered: weighted root mean square residual, root mean square error of approximation, comparative fit index, and Tucker-Lewis index. Good fit was supported by values ≤0.9, ≤0.05, ≥0.95 and ≥0.95, respectively [35;36], and small residual covariances. Analyses were carried out using Mplus 3.13.
Model coefficients represent z-score changes for unit changes in the independent variables. For interpretive ease, the change in probability of reporting fair/poor self-rated health over the range of values for each domain was calculated. While probabilities can be calculated for each domain for each level of self-rated health, fair/poor was chosen given that poorer self-rated health has been associated with poorer outcomes.
RESULTS
The sample demographic, body mass index and self-rated health distributions are summarized in Table 1. 68% reported ≥1 comorbid medical conditions, in addition to osteoarthritis (the index condition). 37.4% reported one other condition (other than osteoarthritis), while nearly 10% reported ≥3 other conditions. The poorest overall health domain scores were observed for physical function, followed by mental health, and social function (Table 2). On average, individuals reported 1.6 musculoskeletal regions that limited activities and 1 of 6 geriatric problems.
Table 1.
Sociodemographic, body mass index and self-rated health characteristics of total hip replacement study sample*
| Characteristic | Mean |
|---|---|
| Age, mean ± SD (range) years | 76.7 ± 5.6 (67.6–96.7) |
| Percentage | |
| Sex | |
| Female | 62.2 |
| Male | 37.8 |
| Household Income | |
| low | 36.0 |
| middle | 33.2 |
| high | 10.2 |
| missing | 20.6 |
| Education | |
| <high school | 19.8 |
| high school | 36.5 |
| some college | 23.3 |
| 4-yr college | 20.3 |
| Body Mass Index | |
| underweight(bmi<18.5) | 1.5 |
| normal (18.5≤bmi≤24.9) | 29.9 |
| overweight (25≤bmi≤29.9) | 42.5 |
| obese (bmi≥30) | 24.5 |
| Self-rated health | |
| Excellent | 9.0 |
| Very Good | 31.7 |
| Good | 39.6 |
| Fair | 16.8 |
| Poor | 3.9 |
N ranges from 924 to 958 for individual characteristic responses.
Table 2.
Mean health domain scores*, overall and by self-rated health status.
| Self-rated Health Status | linearity test | ||||||
|---|---|---|---|---|---|---|---|
| Health Domain (theoretical range) | Overall | Excellent | Very Good | Good | Fair | Poor | p-value |
| Medical comorbidity count** | 1.1 | 0.5 | 0.9 | 1.2 | 1.7 | 2.1 | <0.0001 |
| Musculoskeletal functional limitation† | 1.6 | 0.6 | 1.1 | 1.8 | 2.7 | 2.9 | <0.0001 |
| Physical functioning limitation‡ | 48.6 | 19.1 | 33.9 | 53.8 | 74.3 | 93.5 | <0.0001 |
| Social functioning limitation‡ | 16.6 | 2.5 | 7.8 | 15.7 | 37.3 | 57.3 | <0.0001 |
| Mental health inventory‡ | 20.3 | 11.2 | 15.0 | 20.4 | 31.3 | 51.7 | <0.0001 |
| Geriatric problems† | 1.0 | 0.6 | 0.7 | 0.9 | 1.7 | 1.9 | <0.0001 |
| N | 934 | 83 | 293 | 366 | 155 | 37 | |
higher scores indicate worse health/greater severity.
Theoretical range:
(0–11)
(0–6)
(0–100)
Reporting worse self-rated health was associated with worse domain scores (Table 2). From `excellent' to `poor' self-rated health, mean disease count increased from 0.5 to 2.1, and musculoskeletal limitations from 0.6 to 3. Equivalent estimates ranged from 19.1 to 93.5 for physical function, 2.5 to 57.3 for social function, and 11.2 to 51.7 for mental health.
Table 3 presents probit regression results. Sociodemographic characteristics and body mass index were considered in Model 1, followed by the addition of medical comorbidity count (Model 2), and other health domains (Model 3). The addition of medical comorbidity count increased the R2 for self-rated health by nearly 12 percentage points, from 8.7% to 20.4%. Comorbidity count was significantly associated with self-rated health; a higher count associated with worse self-rated health. The addition of musculoskeletal, physical and social functional status, mental health and geriatric problems increased R2 for self-rated health by a further 27.3 percentage points, to 48%. Each domain was significantly and independently associated with self-rated health, after adjustment for medical comorbidity count. Further, while comorbidity count remained a significant correlate, the magnitude of its coefficient attenuated by just over 20%, suggesting the likelihood of a partially mediated effect between medical comorbidity count and self-rated health through the other health domains.
Table 3.
Probit regressions*; outcome: self-rated health.
| Model 1 |
Model 2 |
Model 3 |
Path Model |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Direct Paths |
Indirect Paths |
|||||||||
| Estimate | p-value | Estimate | p-value | Estimate | p-value | Estimate | p-value | Estimate | p-value | |
| Female (ref: male) | 0.038 | 0.6334 | 0.031 | 0.7002 | −0.107 | 0.2522 | −0.077 | 0.2815 | 0.165 | 0.0000 |
| Age | 0.016 | 0.0112 | 0.016 | 0.0155 | −0.004 | 0.6341 | 0.000 | 0.9817 | 0.020 | 0.0000 |
| Income (ref: middle income) | ||||||||||
| low | 0.206 | 0.0296 | 0.193 | 0.0452 | 0.064 | 0.5592 | 0.105 | 0.2683 | 0.063 | 0.0127 |
| high | − 0.497 | 0.0001 | − 0.466 | 0.0003 | − 0.436 | 0.0016 | − 0.493 | 0.0001 | −0.052 | 0.1676 |
| missing | −0.006 | 0.9537 | 0.04 | 0.9681 | 0.009 | 0.9474 | −0.043 | 0.6936 | −0.006 | 0.8181 |
| Education (ref: 4-yr college) | ||||||||||
| <high school | 0.359 | 0.0045 | 0.356 | 0.0056 | 0.357 | 0.0135 | 0.325 | 0.0165 | ||
| high school | 0.171 | 0.1160 | 0.171 | 0.1192 | 0.135 | 0.2864 | 0.129 | 0.2670 | † | |
| some college | 0.138 | 0.2282 | 0.091 | 0.4325 | 0.059 | 0.6462 | 0.094 | 0.4395 | ||
| Body mass index | 0.011 | 0.0306 | 0.001 | 0.9219 | −0.008 | 0.3519 | −0.006 | 0.3976 | 0.025 | 0.000 |
| Comorbidity count | 0.388 | 0.0000 | 0.309 | 0.0000 | 0.234 | 0.0000 | 0.064 | 0.000 | ||
| Musculoskeletal functional limitations | 0.084 | 0.0057 | 0.065 | 0.0019 | 0.121 | 0.000 | ||||
| Physical function limitations | 0.011 | 0.0000 | 0.008 | 0.0000 | 0.002 | 0.000 | ||||
| Social function limitations | 0.006 | 0.0005 | 0.005 | 0.0006 | ‡ | |||||
| Mental health inventory | 0.013 | 0.0000 | 0.010 | 0.0000 | ||||||
| Geriatric problems | 0.136 | 0.0017 | 0.103 | 0.0006 | 0.076 | 0.000 | ||||
| Self-rated health R2 | 8.7% | 20.4% | 47.7% | 47.5% | ||||||
Estimates represent the impact of a unit change in the variable on the z-score for reporting worse self-rated health.
Adjusted for other model variables, education was not associated with any of the health domains and thus no indirect estimates are reported.
Indirect paths to SRH not specified.
Table 3 also presents results from the path analysis. The hypothesized model showed very good overall fit (weighted root mean square residual=0.541; root mean square error of approximation=0.001; comparative fit index=1.00; Tucker-Lewis index=1.01). Each health domain was significantly associated with self-rated health. The association between medical comorbidity count and self-rated health was significant both directly and mediated through the other health domains. As a proportion, 78.5% of the association was direct, while 21.5% was mediated through the other domains. Thus, the considered health domains accounted minimally for the relationship between medical comorbidity and self-rated health. Additionally, while comorbidity count exhibited statistically significant associations with the health domains (physical function: estimate=3.746, p=0.0004; social function: estimate=1.899, p=0.0128; mental health: estimate=1.715, p=0.0003) the R2 values for these domains ranged from 21% to 31% (with comorbidity count, sociodemographic characteristics and body mass index specified as predictors). Medical comorbidity count was only moderately, though significantly, correlated with geriatric problems (r=0.16, p<0.0001) and musculoskeletal limitations (r=0.20, p<0.0001).
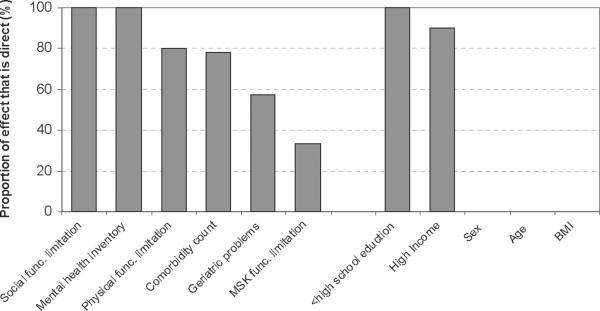
Figure 2 graphically depicts the proportion of the total effect of each health domain, demographic characteristic and body mass index on self-rated health which was direct.
Figure 2.
Proportion of total effects (of health domains, sociodemographic characteristics and body mass index) on self-rated health that were direct; path analysis.
Over the range of their values, medical comorbidity count had the greatest impact on self-rated health, with the probability of reporting fair/poor self-rated health increasing by over 30 percentage points from the reporting of 0 to 6 medical conditions. Similar estimates for musculoskeletal limitations and geriatric problems were 14 points, near 11 for mental health, followed by physical and social functional limitations at 8 and 4 percentage points, respectively.
Only indirect effects of age, sex, and body mass index on self-rated health were found to be significant. For sex and body mass index, these were through physical and musculoskeletal limitations. Additionally for body mass index, comorbidity count was a significant mediating domain. Age was associated with self-rated health through geriatric problems. Increasing age, female sex, increasing body mass index and lower educational attainment were associated with worse self-rated health. Higher income was associated with better self-rated health.
DISCUSSION
Given the wide ranging impact of medical comorbidity and the increasing prevalence of coexistent medical conditions in the aging population, it is not surprising that comorbidity is quickly gaining traction in clinical and public health research. Comorbidity indices often rely on information available in medical records or administrative databases [37], however, and the effect is that these indices provide crude medical case-mix adjustment. This study's findings broaden our conceptual understanding of the burden of illness by identifying independent associations between several constituent health domains of multimorbidity and self-rated health.
Increasing medical comorbidity count was strongly associated with reporting worse self-rated health, consistent with a number of studies in the literature. Additionally, we report that the impact of medical comorbidity on self-rated health was by and large direct, with only 21.5% mediated through other health domains. And, all health domains were independently and significantly associated with a patient's view of their health. Often medical comorbidity is exclusively considered or adjusted for in analyses with the assumption that it is the singular upstream determinant of other health domains. However, medical comorbidity alone was not sufficient to fully account for an individual's overall health.
While medical comorbidity independently influenced the likelihood of reporting worse self-rated health more so than the other domains, musculoskeletal limitations, mental health and geriatric problems also had considerable effect. These findings support the adoption of practices or procedures which consider, review or assess a broad array of health domains to more wholly appraise a patient's or study participant's health.
Our findings are consistent with prior work which, though limited by the range of health domains simultaneously considered, showed independent domain effects, beyond medical comorbidity, for varied outcomes for which self-rated health is predictive. These include physical and cognitive health for mortality [7;38] and hospitalization [7], anxiety and depression for somatic symptom burden [2], and social support for life satisfaction and overall well-being [4;39]. An exclusive focus on any one domain, particularly medical comorbidity, in health research, therefore, is likely to limit the ability of researchers to predict outcomes or trajectories.
This study extends the work of Reichmann et al. [40] which, though comparatively limited in the breadth of domains considered, reported an independent effect of functional status on self-rated health, beyond disease count, among individuals with knee osteoarthritis. Our findings support earlier work in a similar clinical sample ranging in age from 18–88 years [41], though the emphasis was on latent health variables and not specific health domains as in the present study, and to an adolescent and adult general population-based study from the U.S. [42] and Canada [43].
Several studies have documented demographic correlates of self-rated health, including age, sex, and socioeconomic status [44–46]. Consistent with these reports, younger individuals reported better self-rated health, women worse self-rated health, and individuals of lower socioeconomic status poorer self-rated health. As these covariates are also associated with medical comorbidity, it was imperative to consider them in our effort to identify and tease apart individual health domain effects on self-rated health.
This study was carried out among a group of community-dwelling elderly individuals with osteoarthritis who underwent a total hip replacement 3 years prior. While total hip replacement has been well established as an effective intervention for osteoarthritis of the hip [47;48], it is important to bear in mind that improvements following surgery are predominantly localized to the index joint. Patients have threats to their health beyond osteoarthritis in the index joint, however. This is particularly important for patients with medical comorbidities. Therefore, the improved health status experienced by total hip replacement patients following surgery is perhaps best viewed as an interim episode against the backdrop of changes in health brought on by painful joints, osteoarthritis progression, and the onset and progression of other medical comorbidities.
A limitation of our study is its cross-sectional nature. Analyses were limited to the diseases present at the time of the 3 year review and their impact on self-rated health and other domains are specific to this time. Accordingly, our discussion of trajectories is intended to convey theorized causal pathways and not longitudinal evolution. In addition, the moderately low response rate might have introduced selection bias, as responders may have been more health conscious and, more likely therefore, to report better self-rated health. Alternatively, non-respondents may have been in worse health.
While generalizability appears predominantly limited to elderly community-dwelling individuals having undergone primary total hip replacement for osteoarthritis, the relative consistency between our and previously cited works suggests the findings are not unique to this sample. The health domain questions utilized in this study elicited responses unattributed to osteoarthritis or the operated joint and the domains are reflective of general health states and (or) problems experienced by individuals with chronic conditions.
For the most part, comorbidity indices have relied on the use of a summative score. These have been operationalized as a simple count of diseases or a weighted index, with weights determined either by the association with a given outcome (predominantly mortality), and/or by severity rankings of diseases. In some cases the summary scores include severity rankings based on a specific health domain, predominantly physical impairment [49;50]. And, these weights often rely on specific information [37]. We assessed medical comorbidity in such a way that it was not linked to a specific outcome or domain and broadly applicable in that its scoring was not restricted to the availability of specific records or databases.
We believe a better and clearer characterization of the association between medical comorbidities and musculoskeletal limitations, mental health and geriatric problems and self-rated health facilitates a better evaluation of aggregate health burden for health research. Consequently, it also helps identify potential paths of greater or lesser impact to aid in developing more targeted and effective interventions for improving individuals' overall health. We identified a broad range of health domains, including and beyond medical comorbidity, which independently and aggregately impact a patient's overall health.
WHAT IS NEW?
Key Finding
In addition to medical comorbidity, other relevant domains of health (musculoskeletal functional status, general physical and social functional status, geriatric problems and mental health status), aggregately labelled multimorbidity, also contribute significantly and independently to perceptions of overall health.
What this adds to what is known
While medical comorbidity is associated with these health domains, its effects on overall health are for the most part direct, mediated only modestly through other health domains. These domains are not only inter-related, but display independent effects as well.
What is the implication, what should change now
Focussing exclusively on any one domain may limit the ability of researchers to understand health outcomes and trajectories. Investigators should consider multimorbidity and the role specific health domain plays in the achievement of good overall health.
ACKNOWLEDGEMENT
AV Perruccio was supported by a Canadian Institutes of Health Research Fellowship Award (SBM 90860) and the study supported by National Institutes of Health P60 AR 47782, K24 AR 057827, K24 AR 02123. There was no involvement by the funding agencies in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest/financial interests to disclose.
Reference List
- [1].Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chron Dis. 1970;23:455–468. doi: 10.1016/0021-9681(70)90054-8. [DOI] [PubMed] [Google Scholar]
- [2].Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29(2):147–155. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- [3].Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- [4].Bisconti TL, Bergeman CS. Perceived social control as a mediator of the relationships among social support, psychological well-being, and perceived health. Gerontologist. 1999;39(1):94–103. doi: 10.1093/geront/39.1.94. [DOI] [PubMed] [Google Scholar]
- [5].Glass TA, De Leon CF, Bassuk SS, Berkman LF. Social engagement and depressive symptoms in late life: longitudinal findings. J Aging Health. 2006;18(4):604–628. doi: 10.1177/0898264306291017. [DOI] [PubMed] [Google Scholar]
- [6].Seeman TE. Health promoting effects of friends and family on health outcomes in older adults. Am J Health Promot. 2000;14(6):362–370. doi: 10.4278/0890-1171-14.6.362. [DOI] [PubMed] [Google Scholar]
- [7].Dominick KL, Ahern FM, Gold CH, Heller DA. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clin Exp Res. 2002;14(6):499–508. doi: 10.1007/BF03327351. [DOI] [PubMed] [Google Scholar]
- [8].Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152(9):874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- [9].Rosso AL, Gallagher RM, Luborsky M, Mossey JM. Depression and self-rated health are proximal predictors of episodes of sustained change in pain in independently living, community dwelling elders. Pain Med. 2008;9(8):1035–1049. doi: 10.1111/j.1526-4637.2008.00533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Wilcox VL, Kasl SV, Idler EL. Self-rated health and physical disability in elderly survivors of a major medical event. J Gerontol B Psychol Sci Soc Sci. 1996;51(2):S96–104. doi: 10.1093/geronb/51b.2.s96. [DOI] [PubMed] [Google Scholar]
- [11].Kennedy BS, Kasl SV, Vaccarino V. Repeated hospitalizations and self-rated health among the elderly: a multivariate failure time analysis. Am J Epidemiol. 2001;153(3):232–241. doi: 10.1093/aje/153.3.232. [DOI] [PubMed] [Google Scholar]
- [12].Menec VH, Chipperfield JG. A prospective analysis of the relation between self-rated health and health care use among elderly Canadians. Canadian Journal on Aging. 2001;20:293–306. [Google Scholar]
- [13].Weinberger M, Darnell JC, Tierney WM, Martz BL, Hiner SL, Barker J, et al. Self-rated health as a predictor of hospital admission and nursing home placement in elderly public housing tenants. Am J Public Health. 1986;76(4):457–459. doi: 10.2105/ajph.76.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Benyamini Y, Idler EL. Community Studies Reporting Association Between Self-Rated Health and Mortality: Additional Studies, 1995 to 1998. Research on Aging. 1999;21:392–401. [Google Scholar]
- [15].Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- [16].Kawada T. Self-rated health and life prognosis. Arch Med Res. 2003;34(4):343–347. doi: 10.1016/S0188-4409(03)00052-3. [DOI] [PubMed] [Google Scholar]
- [17].Prevalence of disabilities and associated health conditions among adults--United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50(7):120–125. [PubMed] [Google Scholar]
- [18].Power JD, Perruccio AV, Desmeules M, Lagace C, Badley EM. Ambulatory physician care for musculoskeletal disorders in Canada. J Rheumatol. 2006;33(1):133–139. [PubMed] [Google Scholar]
- [19].Verbrugge LM, Patrick DL. Seven chronic conditions: their impact on US adults' activity levels and use of medical services. Am J Public Health. 1995;85(2):173–182. doi: 10.2105/ajph.85.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Gabriel SE, Crowson CS, O'Fallon WM. Comorbidity in arthritis. J Rheumatol. 1999;26(11):2475–2479. [PubMed] [Google Scholar]
- [21].Kadam UT, Jordan K, Croft PR. Clinical comorbidity in patients with osteoarthritis: a case-control study of general practice consulters in England and Wales. Ann Rheum Dis. 2004;63(4):408–414. doi: 10.1136/ard.2003.007526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Schellevis FG, van d V, van de LE, van Eijk JT, van Weel C. Comorbidity of chronic diseases in general practice. J Clin Epidemiol. 1993;46(5):469–473. doi: 10.1016/0895-4356(93)90024-u. [DOI] [PubMed] [Google Scholar]
- [23].Kadam UT, Croft PR. Clinical comorbidity in osteoarthritis: associations with physical function in older patients in family practice. J Rheumatol. 2007;34(9):1899–1904. [PubMed] [Google Scholar]
- [24].Rupp I, Boshuizen HC, Roorda LD, Dinant HJ, Jacobi CE, van den BG. Poor and good health outcomes in rheumatoid arthritis: the role of comorbidity. J Rheumatol. 2006;33(8):1488–1495. [PubMed] [Google Scholar]
- [25].Verbrugge LM, Gates DM, Ike RW. Risk factors for disability among U.S. adults with arthritis. J Clin Epidemiol. 1991;44(2):167–182. doi: 10.1016/0895-4356(91)90264-a. [DOI] [PubMed] [Google Scholar]
- [26].Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2001;83-A(11):1622–1629. doi: 10.2106/00004623-200111000-00002. [DOI] [PubMed] [Google Scholar]
- [27].Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49(2):156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- [28].Katz JN, Wright EA, Baron JA, Losina E. Development and validation of an index of musculoskeletal functional limitations. BMC Musculoskelet Disord. 2009;10:62. doi: 10.1186/1471-2474-10-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr., Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- [30].Bischoff-Ferrari HA, Lingard EA, Losina E, Baron JA, Roos EM, Phillips CB, et al. Psychosocial and geriatric correlates of functional status after total hip replacement. Arthritis Rheum. 2004;51(5):829–835. doi: 10.1002/art.20691. [DOI] [PubMed] [Google Scholar]
- [31].Finch JF, Graziano WG. Predicting depression from temperament, personality, and patterns of social relations. J Pers. 2001;69(1):27–55. doi: 10.1111/1467-6494.00135. [DOI] [PubMed] [Google Scholar]
- [32].Gil KM, Keefe FJ, Crisson JE, Van Dalfsen PJ. Social support and pain behavior. Pain. 1987;29(2):209–217. doi: 10.1016/0304-3959(87)91037-2. [DOI] [PubMed] [Google Scholar]
- [33].Russell DW, Cutrona CE. Social support, stress, and depressive symptoms among the elderly: test of a process model. Psychol Aging. 1991;6(2):190–201. doi: 10.1037//0882-7974.6.2.190. [DOI] [PubMed] [Google Scholar]
- [34].Sherman AM. Social relations and depressive symptoms in older adults with knee osteoarthritis. Soc Sci Med. 2003;56(2):247–257. doi: 10.1016/s0277-9536(02)00023-0. [DOI] [PubMed] [Google Scholar]
- [35].Hu L, Bentler PM. Fit indices in covariance strucuture modeling: Sensitivity to underparameterized model misspecification. Psychol Methods. 1998;3:424–453. [Google Scholar]
- [36].Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- [37].Bayliss EA, Edwards AE, Steiner JF, Main DS. Processes of care desired by elderly patients with multimorbidities. Fam Pract. 2008;25(4):287–293. doi: 10.1093/fampra/cmn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279(15):1187–1193. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- [39].Ferreira VM, Sherman AM. The relationship of optimism, pain and social support to well-being in older adults with osteoarthritis. Aging Ment Health. 2007;11(1):89–98. doi: 10.1080/13607860600736166. [DOI] [PubMed] [Google Scholar]
- [40].Reichmann WM, Katz JN, Kessler CL, Jordan JM, Losina E. Determinants of self-reported health status in a population-based sample of persons with radiographic knee osteoarthritis. Arthritis Rheum. 2009;61(8):1046–1053. doi: 10.1002/art.24839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Perruccio AV, Badley EM, Hogg-Johnson S, Davis AM. Characterizing self-rated health during a period of changing health status. Soc Sci Med. 2010;71(9):1636–1643. doi: 10.1016/j.socscimed.2010.07.042. [DOI] [PubMed] [Google Scholar]
- [42].Boardman JD. Self-rated health among U.S. adolescents. J Adolesc Health. 2006;38(4):401–408. doi: 10.1016/j.jadohealth.2005.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Bailis DS, Segall A, Chipperfield JG. Two views of self-rated general health status. Soc Sci Med. 2003;56(2):203–217. doi: 10.1016/s0277-9536(02)00020-5. [DOI] [PubMed] [Google Scholar]
- [44].Mantyselka PT, Turunen JH, Ahonen RS, Kumpusalo EA. Chronic pain and poor self-rated health. JAMA. 2003;290(18):2435–2442. doi: 10.1001/jama.290.18.2435. [DOI] [PubMed] [Google Scholar]
- [45].Perruccio AV, Power JD, Badley EM. Arthritis onset and worsening self-rated health: a longitudinal evaluation of the role of pain and activity limitations. Arthritis Rheum. 2005;53(4):571–577. doi: 10.1002/art.21317. [DOI] [PubMed] [Google Scholar]
- [46].Dominick KL, Ahern FM, Gold CH, Heller DA. Health-related quality of life among older adults with arthritis. Health Qual Life Outcomes. 2004;2(1):5. doi: 10.1186/1477-7525-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- [48].Harris WH, Sledge CB. Total hip and total knee replacement (2) N Engl J Med. 1990;323(12):801–807. doi: 10.1056/NEJM199009203231206. [DOI] [PubMed] [Google Scholar]
- [49].de G V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003;56(3):221–229. doi: 10.1016/s0895-4356(02)00585-1. [DOI] [PubMed] [Google Scholar]
- [50].Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54(7):661–674. doi: 10.1016/s0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]