Abstract
Objective
To determine whether age at initiation of amblyopia treatment influences the response among children 3 to <13 years of age with unilateral amblyopia 20/40 to 20/400.
Methods
A meta-analysis of individual subject data from 4 recently completed randomized amblyopia treatment trials was performed to evaluate the relationship between age and improvement in logMAR amblyopic eye visual acuity. Analyses were adjusted for baseline amblyopic eye visual acuity, spherical equivalent refractive error in the amblyopic eye, type of amblyopia, prior amblyopia treatment, study treatment, and protocol. Age was categorized (3 to <5 years, 5 to <7 years, and 7 to <13 years) because there was a non-linear relationship between age and improvement in amblyopic eye acuity.
Results
Subjects 7 to <13 years were significantly less responsive to treatment compared with younger age groups (3 to <5 years, 5 to <7 years) for moderate and severe amblyopia (P<0.04 for all four comparisons). There was no difference in treatment response between subjects age 3 to <5 years and 5 to <7 years for moderate amblyopia (P=0.67), but there was a suggestion of greater responsiveness of 3- to <5-year olds compared with 5- to <7-year olds for severe amblyopia (P=0.09).
Conclusions
Amblyopia is more responsive to treatment among children younger than age 7 years. Although the average treatment response is smaller in 7- to <13-year olds, some individuals show a marked response to treatment.
Introduction
Evidence that amblyopia treatment is effective in some older children1, 2 raises the longstanding question of whether or not there is a relationship between age and magnitude of treatment response. We performed a meta-analysis of subject data from four completed randomized amblyopia treatment trials,2–5 with similar entry criteria and similar timing of masked outcome assessment. The meta-analysis addressed whether magnitude of treatment response is influenced by the child’s age, when treating with occlusion, atropine, or Bangerter filters.
Methods
Studies included for analysis
A meta-analysis was conducted by pooling data from 996 subjects aged 3 to <13 years, who participated in 4 randomized multicenter clinical trials of treatment2–5 for amblyopia caused by strabismus, anisometropia, or both, conducted by the Pediatric Eye Disease Investigator Group (PEDIG).6 The protocols were registered on www.clinicaltrials.gov as NCT00315198, NCT00315302, NCT00315328, NCT00525174 and were approved by the Institutional Review Boards covering the participating centers. The protocols were: 1. Patching 2 hours per day with near or distance activities in 3 to <7 year olds.3 2. Atropine with and without a plano lens in 3 to <7 year olds.4 3. Atropine vs. patching 2 hours per day in 7 to <13 years olds.2 4. Bangerter filter versus patching 2 hours per day in 3 to <10 year olds.5 The complete protocols are available on the PEDIG website (www.pedig.net) and summarized in Table 1.
Table 1.
Studies included in the Meta-analysis
| Protocol | Ref | N | Treatment Groups | Age (years) | Visual Acuity Testing Method | Amblyopia Severity At enrollment | Outcome Exam Time Point |
|---|---|---|---|---|---|---|---|
| 1 | 3 | 395 | 2 hr patching + Near activities 2 hr patching + Distance activities |
3 – <7 | ATS-HOTV© | 20/40 – 20/400 | 17 ± 1 week |
| 2 | 4 | 227 | Weekend Atropine Weekend Atropine + Plano Lens |
3 – <7 | ATS-HOTV© | 20/40 – 20/400 | 18 ± 1 week |
| 3 | 2 | 205 | 2 hr patching Weekend Atropine |
7 – <13 | E-ETDRS© | 20/40 – 20/400 | 17 ± 1 week |
| 4 | 5 | 169 | 2 hr patching Bangerter filter (full-time) |
3–<10 | ATS-HOTV© (age 3-<7y) E-ETDRS© (age 7-<10y) |
20/40 – 20/80 | 24 ± 2 weeks |
ATS-HOTV© - Amblyopia Treatment Study visual acuity test using single-surrounded H, O, T, and V optotypes
E-ETDRS© - electronic Early Treatment of Diabetic Retinopathy Study visual acuity test using single-surrounded optotypes
These trials were specifically chosen because all four protocols required stability of amblyopic eye visual acuity in spectacles prior to enrollment, defined as at least 4 weeks of stable visual acuity or 16 weeks of spectacle wear. Therefore, any improvement in visual acuity would be primarily due to the additional treatment prescribed (patching, atropine with or without a plano lens, or Bangerter filter), rather than from the spectacle correction. The four trials were not designed to determine the maximum treatment effect, and the primary outcome was assessed at 17 to 24 weeks following enrollment. Baseline characteristics of the cohort are summarized in Table 2 (online).
Table 2.
Baseline characteristics of cohort
| PROCOTOL | OVERALL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||||||
| N | % | N | % | N | % | N | % | N | % | |
| AGE (Years) | ||||||||||
| <4 | 47 | 12% | 50 | 22% | 0 | 0 | 13 | 8% | 110 | 11% |
| 4–<5 | 89 | 23% | 65 | 29% | 0 | 0 | 31 | 18% | 185 | 19% |
| 5–<6 | 126 | 32% | 67 | 30% | 0 | 0 | 27 | 16% | 220 | 22% |
| 6–<7 | 133 | 34% | 45 | 20% | 0 | 0 | 38 | 22% | 216 | 22% |
| 7–<8 | 0 | 0 | 0 | 0 | 67 | 33% | 32 | 19% | 99 | 10% |
| 8–<10 | 0 | 0 | 0 | 0 | 86 | 42% | 28 | 17% | 114 | 11% |
| 10–<13 | 0 | 0 | 0 | 0 | 52 | 25% | 0 | 0 | 52 | 5% |
| Mean (SD) | 5.4 (1.0) | 5.0 (1.1) | 9.0 (1.6) | 6.3 (1.6) | 6.2 (2.0) | |||||
| GENDER | ||||||||||
| Female | 184 | 47% | 111 | 49% | 107 | 52% | 77 | 46% | 479 | 48% |
| RACE/ETHNICITY | ||||||||||
| White | 306 | 77% | 185 | 81% | 135 | 66% | 124 | 73% | 750 | 75% |
| Black/African American | 19 | 5% | 8 | 4% | 19 | 9% | 14 | 8% | 60 | 6% |
| Asian | 11 | 3% | 3 | 1% | 1 | <1% | 3 | 2% | 18 | 2% |
| Hispanic or Latino | 42 | 11% | 30 | 13% | 44 | 21% | 21 | 12% | 137 | 14% |
| More than one race | 5 | 1% | 0 | 0 | 3 | 1% | 5 | 3% | 13 | 1% |
| Unknown/not reported | 12 | 3% | 1 | <1% | 3 | 1% | 2 | 1% | 18 | 2% |
| PRIOR TREATMENT | ||||||||||
| No | 363 | 92% | 188 | 83% | 151 | 74% | 140 | 83% | 842 | 85% |
| AMBLYOPIA CAUSE | ||||||||||
| Strabismus | 112 | 28% | 91 | 40% | 58 | 28% | 44 | 26% | 305 | 31% |
| Anisometropia | 202 | 51% | 71 | 31% | 83 | 40% | 75 | 44% | 431 | 43% |
| Combined Mechanism | 81 | 21% | 65 | 29% | 64 | 31% | 50 | 30% | 260 | 26% |
| BASELINE AMBLYOPIC EYE VISUAL ACUITY | ||||||||||
| 20/40 | 65 | 16% | 28 | 12% | 33 | 16% | 41 | 24% | 167 | 17% |
| 20/50 | 79 | 20% | 40 | 18% | 55 | 27% | 37 | 22% | 211 | 21% |
| 20/63 | 85 | 22% | 55 | 24% | 44 | 21% | 54 | 32% | 238 | 24% |
| 20/80 | 44 | 11% | 28 | 12% | 23 | 11% | 37 | 22% | 132 | 13% |
| 20/100 | 43 | 11% | 21 | 9% | 17 | 8% | 0 | 0 | 81 | 8% |
| 20/125 | 30 | 8% | 18 | 8% | 10 | 5% | 0 | 0 | 58 | 6% |
| 20/160 | 23 | 6% | 9 | 4% | 9 | 4% | 0 | 0 | 41 | 4% |
| 20/200 | 10 | 3% | 8 | 4% | 6 | 3% | 0 | 0 | 24 | 2% |
| 20/250 | 7 | 2% | 4 | 2% | 6 | 3% | 0 | 0 | 17 | 2% |
| 20/320 | 7 | 2% | 8 | 4% | 1 | <1% | 0 | 0 | 16 | 2% |
| 20/400 | 2 | 1% | 8 | 4% | 1 | <1% | 0 | 0 | 11 | 1% |
| Mean (SD) logMAR | 0.57 (0.23) | 0.61 (0.26) | 0.54 (0.22) | 0.45 (0.11) | 0.55 (0.22) | |||||
| Snellen Equivalent | 20/80+2 | 20/80−1 | 20/63−2 | 20/50−2 | 20/63−2 | |||||
| AMBLYOPIC EYE SPHERICAL EQUIVALENT | ||||||||||
| <0 D | 23 | 6% | 0 | 0 | 4 | 2% | 9 | 5% | 36 | 4% |
| 0 to <+1.00D | 22 | 6% | 0 | 0 | 19 | 9% | 4 | 2% | 45 | 5% |
| +1.00 to <+2.00D | 29 | 7% | 7 | 3% | 18 | 9% | 9 | 5% | 63 | 6% |
| +2.00 to <+3.00D | 39 | 10% | 17 | 7% | 16 | 8% | 15 | 9% | 87 | 9% |
| +3.00 to <+4.00D | 43 | 11% | 34 | 15% | 37 | 18% | 20 | 12% | 134 | 13% |
| +4.00 to <+5.00D | 77 | 19% | 51 | 22% | 28 | 14% | 41 | 24% | 197 | 20% |
| +5.00 to <+6.00D | 75 | 19% | 54 | 24% | 41 | 20% | 29 | 17% | 199 | 20% |
| +6.00 to <+7.00D | 50 | 13% | 35 | 15% | 22 | 11% | 26 | 15% | 133 | 13% |
| ≥+7.00D | 37 | 9% | 29 | 13% | 20 | 10% | 16 | 9% | 102 | 10% |
| Mean (SD) | 4.03 (2.57) | 5.03 (1.67) | 4.06 (2.23) | 4.27 (2.36) | 4.31 (2.32) | |||||
| FELLOW EYE SPHERICAL EQUIVALENT | ||||||||||
| <0 D | 12 | 3% | 0 | 0 | 3 | 1% | 5 | 3% | 20 | 2% |
| 0 to <+1.00D | 98 | 25% | 0 | 0 | 65 | 32% | 32 | 19% | 195 | 20% |
| +1.00 to <+2.00D | 97 | 25% | 51 | 22% | 54 | 26% | 41 | 24% | 243 | 24% |
| +2.00 to <+3.00D | 49 | 12% | 42 | 19% | 20 | 10% | 24 | 14% | 135 | 14% |
| +3.00 to <+4.00D | 48 | 12% | 40 | 18% | 14 | 7% | 19 | 11% | 121 | 12% |
| +4.00 to <+5.00D | 42 | 11% | 41 | 18% | 23 | 11% | 20 | 12% | 126 | 13% |
| +5.00 to <+6.00D | 25 | 6% | 27 | 12% | 16 | 8% | 12 | 7% | 80 | 8% |
| +6.00 to <+7.00D | 12 | 3% | 17 | 7% | 4 | 2% | 10 | 6% | 43 | 4% |
| ≥+7.00D | 12 | 3% | 9 | 4% | 6 | 3% | 6 | 4% | 33 | 3% |
| Mean (SD) | 2.37 (2.05) | 3.60 (1.76) | 2.23 (2.07) | 2.64 (2.09) | 2.67 (2.06) | |||||
| TREATMENT | ||||||||||
| Atropine | 0 | 0 | 227 | 100% | 108 | 53% | 0 | 0 | 335 | 34% |
| Bangerter | 0 | 0 | 0 | 0 | 0 | 0 | 81 | 48% | 81 | 8% |
| Patching | 395 | 100% | 0 | 0 | 97 | 47% | 88 | 52% | 580 | 58% |
PEDIG Protocols included: 1. Patching 2 hours per day with near or distance activities in 3- to <7-year olds.3 2. Atropine with and without a plano lens in 3- to <7-year olds.4 3. Atropine versus patching 2 hours per day in 7- to <13-years olds.2 4. Bangerter filter versus patching 2 hours per day in 3- to <10-year olds.5
D = diopters
Measurement of visual acuity
Visual acuity at baseline was measured using either ATS HOTV©7 for subjects ages 3 to <7 years or Electronic Early Treatment Diabetic Retinopathy Study (E-ETDRS©)8 for subjects ages 7 to <13 years, each using the Electronic Visual Acuity tester.9 Baseline amblyopic eye acuities ranged from 20/40 to 20/400. Visual acuity at follow-up exams was measured using the same testing method performed at baseline, regardless of age at follow-up. All visual acuity measures were converted to logarithm of the minimum angle of resolution (logMAR) scores and change in amblyopic eye visual acuity from enrollment was computed in logMAR lines.
Statistical Methods
A meta analysis of individual subject data was performed using a multivariate linear regression model10 evaluating the relationship between age group and improvement in amblyopic eye visual acuity (in logMAR lines of improvement), adjusting for factors which could be expected to influence outcome. Age was grouped into 3 categories (3 to <5 years, 5 to <7 years, and 7 to <13 years) because, in the initial analysis of these data, there was a non-linear relationship between age and improvement in amblyopic eye acuity. It was not possible to fit a random effects model11 for age due to the small number of protocols and partial overlap in age groups among the protocols; therefore, all factors, including age, were treated as fixed effects.
Covariate adjustments included the following: baseline amblyopic eye visual acuity, spherical equivalent refractive error in the amblyopic eye, prior amblyopia treatment (yes or no), type of amblyopia (anisometropic, strabismic, or combined anisometropic-strabismic), treatment (patching, atropine, Bangerter filter), and protocol. Two-way interaction terms of the adjustment covariates with age group were also tested, and terms meeting a statistical significance criterion of p<0.05 were retained in the model. Age group comparisons of adjusted mean acuity improvement according to amblyopia severity were performed using the Tukey-Kramer multiple comparisons test12 (2-sided alpha=0.05).
The final multivariate linear regression model derived from the pooled data was applied separately to each protocol to confirm that pooled data estimates were consistent with estimates from the individual protocols. Possible heterogeneity among protocols in adjusted mean visual acuity improvement was tested by adding to the final meta-analysis model the interactions with protocol for all model terms that included age.13 Linear contrasts were used to identify the protocols that differed when protocol interactions indicated significant heterogeneity. All analyses were performed using SAS Version 9.1 (SAS Institute, Cary, NC).
Results
Factors associated with visual acuity improvement
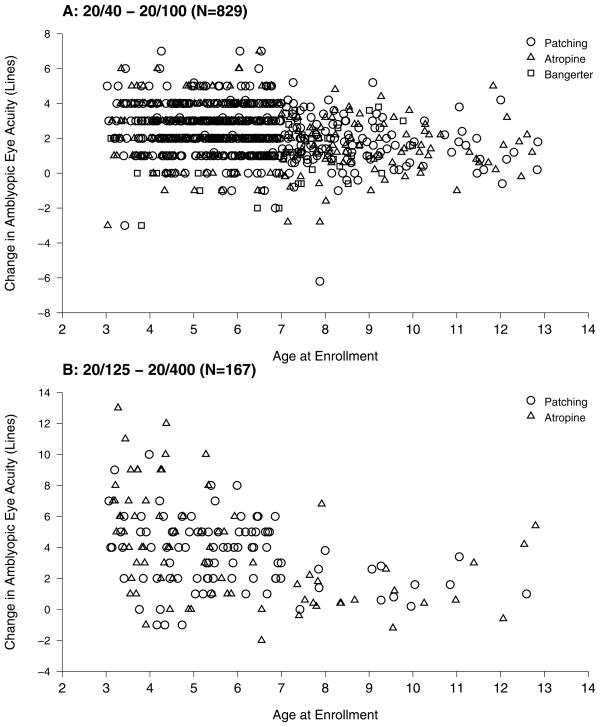
Based on scatter plots of visual acuity change versus age by amblyopia severity at enrollment (Figure 1A and 1B), there appeared to be a decrease in treatment response with increasing age that was most evident within those with more severe amblyopia. The difference, between severe and moderate amblyopia, in effect on treatment response, was confirmed by a highly significant interaction between age group and baseline amblyopic eye acuity (P<0.001) in the meta-analysis.
Figure 1.
Relationship between age and amblyopic eye visual acuity improvement by treatment type in subjects ages 3 to <13 years with moderate amblyopia (A) and severe amblyopia (B)
In addition to an overall effect of age, we found an association between greater improvement in amblyopic eye visual acuity and less hyperopic amblyopic eye spherical equivalent (P=0.002). There was a significant interaction between age group and prior amblyopia treatment (P=0.02), indicating less amblyopic eye acuity improvement with history of prior amblyopia treatment (1.83 lines) than without treatment (2.74 lines) in the 3 to <5 year age group (P=0.018). There was no association of amblyopic acuity improvement with amblyopia type (P=0.20), amblyopia study treatment (P=0.14), and protocol (P=0.28) (Table 3).
Table 3.
Amblyopic eye visual acuity improvement according to age group and other covariates
| Variable | Observed (Unadjusted) Means | Adjusted Means | |||
|---|---|---|---|---|---|
| N | Mean ± SE | 95% CI | Adjusted Mean* ± SE | 95% CI | |
| Age Group and Amblyopic Eye Visual Acuity | Lines of Visual Acuity Improvement | ||||
| Moderate Amblyopia | |||||
| 3 to <5 yrs | 222 | 2.61 ± 0.10 | (2.41, 2.81) | 2.29 ± 0.15 | (2.00, 2.57) |
| 5 to <7 yrs | 375 | 2.50 ± 0.08 | (2.34, 2.65) | 2.41 ± 0.12 | (2.17, 2.65) |
| 7 to <13 yrs | 232 | 1.62 ± 0.10 | (1.43, 1.80) | 1.65a ± 0.17 | (1.31, 1.99) |
| Severe Amblyopia | |||||
| 3 to <5 yrs | 73 | 4.70 ± 0.37 | (3.95, 5.44) | 4.16 ± 0.21 | (3.75, 4.58) |
| 5 to <7 yrs | 61 | 3.72 ± 0.28 | (3.15, 4.29) | 3.60 ± 0.22 | (3.17, 4.02) |
| 7 to <13 yrs | 33 | 1.59 ± 0.30 | (0.98, 2.21) | 1.99a ± 0.30 | (1.41, 2.57) |
|
| |||||
| Amblyopia Cause | Lines of Visual Acuity Improvement | ||||
| Strabismus | 305 | 2.69 ± 0.10 | (2.48, 2.89) | 2.43 ± 0.11 | (2.22, 2.65) |
| Anisometropia | 431 | 2.43 ± 0.09 | (2.26, 2.60) | 2.30 ± 0.10 | (2.11, 2.49) |
| Combined Mechanism | 260 | 2.48 ± 0.14 | (2.21, 2.75) | 2.18 ± 0.12 | (1.95, 2.41) |
| Randomized Treatment | |||||
| Atropine | 335 | 2.61 ± 0.13 | (2.36, 2.86) | 2.28 ± 0.15 | (1.99, 2.57) |
| Bangerter | 81 | 1.89 ± 0.18 | (1.53, 2.25) | 2.13 ± 0.22 | (1.70, 2.56) |
| Patching | 580 | 2.56 ± 0.07 | (2.42, 2.70) | 2.50 ± 0.11 | (2.29, 2.71) |
| Amblyopic Eye Spherical Equivalent | 996 | −0.02 ± 0.03 | (−0.07, 0.03) | −0.07† ± 0.02 | (−0.11, −0.02) |
| Age Group and Prior Amblyopia Treatment | |||||
| No Prior Treatment | |||||
| 3 to <5 yrs | 270 | 3.18 ± 0.14 | (2.91, 3.44) | 2.74 ± 0.14 | (2.47, 3.00) |
| 5 to <7 yrs | 381 | 2.63 ± 0.09 | (2.46, 2.80) | 2.55 ± 0.13 | (2.30, 2.80) |
| 7 to <13 yrs | 191 | 1.56 ± 0.11 | (1.33, 1.78) | 1.68a ± 0.19 | (1.31, 2.05) |
| Prior Amblyopia Treatment | |||||
| 3 to <5 yrs | 25 | 2.56± 0.49 | (1.54, 3.58) | 1.83 ± 0.38 | (1.08, 2.58) |
| 5 to <7 yrs | 55 | 2.95 ± 0.21 | (2.52, 3.37) | 2.92a ± 0.25 | (2.43, 3.41) |
| 7 to <13 yrs | 74 | 1.76 ± 0.15 | (1.45, 2.07) | 1.87 ± 0.23 | (1.42, 2.32) |
Adjusted means with superscripts are statistically different from those without whereas means that share the superscript letter are not statistically different, based on the Tukey-Kramer multiple comparisons test12 with an overall significance level of p<0.05.
Adjusted for: amblyopia cause, amblyopic eye spherical equivalent, treatment group, the 2-way interactions between age group with baseline amblyopic eye acuity and with prior treatment (plus nested terms), and protocol.
Every additional 4.00 diopter increase in amblyopic eye spherical equivalent of hyperopia corresponds to approximately a 0.3 line less improvement in amblyopic eye visual acuity
CI = confidence interval
Effect of age by amblyopia severity
Adjusting for covariates in the regression model, subjects 7 to <13 years old were significantly less responsive to treatment compared with younger subjects (3 to <5 years and 5 to <7 years) for both moderate amblyopia (P<0.04 for all comparisons) and severe amblyopia (P<0.001 for all comparisons) (Table 3). Treatment response did not differ statistically among subjects age <7 years old (3 to <5 years versus 5 to <7 years) for moderate amblyopia (P=0.67) or severe amblyopia (P=0.09), although the data suggested a steeper decline in response with age among subjects with severe amblyopia (Table 3).
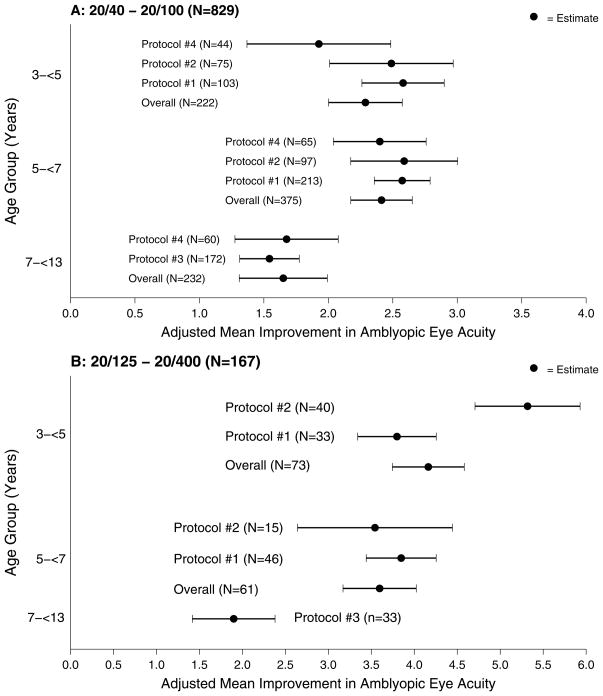
Consistency between protocols
There was some heterogeneity among protocols in adjusted mean visual acuity improvement, but only for the 3 to <5 age group within the severe baseline amblyopia strata (P=0.002). Specifically, there was a significantly greater response to treatment with atropine (protocol #2)4 compared with patching (protocol #1) for subjects age 3 to <5 years with severe amblyopia at baseline3 (Figure 2A and 2B). Otherwise, the overall adjusted mean visual acuity improvement for each age group in the meta-analysis was consistent with the individual estimates from each protocol.
Figure 2.
Forest plots of adjusted mean amblyopic acuity improvement within age group in subjects with moderate amblyopia (A) and severe amblyopia (B). The dots indicate the adjusted mean for each age group for each protocol and the horizontal lines indicate the 95% CI for each mean.
Discussion
In a meta-analysis of outcome data from four randomized clinical trials mean visual acuity improved with amblyopia therapy throughout the age range of 3 to <13 years. Subjects ages 7 to <13 years had less improvement than subjects ages 3 to <7 years for both moderate and severe amblyopia. Although treatment response was not statistically different across the 3 to <7-year old range for both moderate and severe amblyopia, there was a suggestion of a steeper decline in response with age for subjects with severe amblyopia at baseline.
Earlier PEDIG studies did not require stability of visual acuity prior to starting patching or atropine, but we had reached similar conclusions regarding the effect of age on treatment response. For example, among children 3 to <7 years old, we found no evidence of reduced response in older children compared with younger children when treating with patching14 or atropine15 for moderate amblyopia. In contrast, for severe amblyopia we previously found the youngest children (3 to <5 years old) were somewhat more responsive to either 6 hours/day patching or full-time patching than older children (5 to <7 years of age).16 Retrospective studies by Fulton and Mayer17 and Flynn et al.18 have also reported reduced response to amblyopia treatment in older children, but these studies were limited by lack of a standardized outcome assessment. Conversely, other authors have reported significant improvement in amblyopic eye visual acuity in children older than 7 years.19, 20
There are at least two possible reasons for reduced response to amblyopia treatment in older children. It is widely believed that there is declining plasticity of the central nervous system as children age, although recent data on the treatment of amblyopia1 suggest the plasticity of the nervous system remains throughout adolescence. Secondly, there may be poorer compliance when treating older children. Such compliance issues could be studied by using occlusion dose monitors,21–23 but these devices are not currently commercially available and were not used in our studies.
Despite the reduced treatment response in older subjects aged 7 to <13 years compared with younger subjects, there was still an improvement of mean visual acuity with treatment and some individuals responded dramatically. This difference in individual response also was found in the PEDIG study of treatment of teenagers;1 some had a dramatic response to 2 to 6 hours/day of prescribed patching, whereas others had little or no response. Stewart et al.24 used occlusion dose monitors in somewhat younger children (mean age 5.6 years +/− 1.5 years), and they observed a wide range of visual acuity improvement to a given dose of patching. The disparity of visual acuity response among teenagers in an earlier PEDIG study1 may have been due to variable compliance, but the issue of compliance cannot be resolved because actual wearing time was not measured. Nevertheless, it seems reasonable to offer treatment to even older teenagers (for example, through age 17 years), since we are currently unable to predict which patients will or will not respond.
Regarding treatment of amblyopia with optical correction alone,25 we do not know whether the response is age-dependent, because the study protocols included in the present meta-analysis required wearing of optical correction for at least 16 weeks or until stable visual acuity was demonstrated prior to randomization. Nevertheless, it is noteworthy that a previous study of teenagers1 have shown improvement in amblyopic visual acuity from optical correction alone.
The strength of the present study is the application of meta-analysis to four randomized trials of individual subject data with similar entry criteria, the length of follow-up, and the use of a masked and standardized outcome assessment. There are several limitations of our analysis. Our ability to separate protocol effects from age effects is dependent on a single protocol (#4) which was the only protocol that had overlap in age with all other protocols (Table 1). Also, protocol #4 did not include any subjects with severe amblyopia. Thus, separating an age effect from a protocol effect in severe amblyopia relied on assuming the same protocol effects that were seen in moderate amblyopia (Figure 2A and 2B) i.e. assuming the lesser improvement seen in the 7- to <13-year age group was due to age and not to protocol.
Additional limitations include using arbitrary age categories to model age effects and using different visual acuity testing methods in those <7 years7 and those age 7 and older.8 We used age categories to model age effects because there was evidence that the age effect was nonlinear; but, it is likely that this effect follows a non-linear continuum that we were unable to identify due to lack of sufficient overlap in ages included in each protocol, and coarser granularity of change measurements in younger children tested with ATS HOTV© compared with older children tested with E-ETDRS© (Figure 1). ATS HOTV© testing leads to slightly higher visual acuity scores than E-ETDRS© testing, particularly in amblyopic eyes,26, 27 (an average of 0.08 logMAR and 0.07 logMAR respectively) but we do not believe that this influenced our primary finding of less responsiveness in older children because visual acuity was measured using the same method at enrollment and outcome, so the potential bias between methods is minimized when looking at change. It is also possible that if there was a learning or maturation effect, such an effect might be greater in younger children. Nevertheless, improvement in the sound eye visual acuity was similar in younger and older children treated with patching in our studies. For example, sound eye visual acuity improvement was 1.5 letters (0.3 logMAR lines) in children 7 to <13 years old,2 and 0.3 logMAR lines in children 3 to <7 years old.3 None of the protocols collected visual acuity data beyond the 17- to 24-week study outcome exam, and we have no data on duration of amblyopia prior to treatment. Finally, these data can only be generalized to children with amblyopia caused by strabismus, anisometropia, or both combined.
In conclusion, while there is improvement of visual acuity across all age range of 3 to <13 years, subjects ages 7 to <13 years are least responsive to amblyopia treatment. Although treatment response is not statistically different across the 3 to <7 year old range for both moderate and severe amblyopia, there is a suggestion of a steeper decline in response with age for subjects with severe amblyopia at baseline. Despite reduced average treatment response in 7-to <13-year olds, some 7- to <13 year olds show marked improvement with treatment.
Acknowledgments
Supported by Grants from the National Institutes of Health (EY011751 and EY018810) and Research to Prevent Blindness, New York, New York (JMH as Olga Keith Weiss Scholar and an Unrestricted Grant to Mayo Clinic Department of Ophthalmology). The funding organizations had no role in the design of the studies. The NIH provided external oversight through an independent data and safety monitoring committee.
References
- 1.Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123(4):437–47. doi: 10.1001/archopht.123.4.437. [DOI] [PubMed] [Google Scholar]
- 2.Pediatric Eye Disease Investigator Group. Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Arch Ophthalmol. 2008;126(12):1634–42. doi: 10.1001/archophthalmol.2008.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pediatric Eye Disease Investigator Group. A randomized trial of near versus distance activities while patching for amblyopia in children aged 3 to less than 7 years. Ophthalmology. 2008;115(11):2071–8. doi: 10.1016/j.ophtha.2008.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pediatric Eye Disease Investigator Group. Pharmacological plus optical penalization treatment for amblyopia: results of a randomized trial. Arch Ophthalmol. 2009;127(1):22–30. doi: 10.1001/archophthalmol.2008.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pediatric Eye Disease Investigator Group. A randomized trial comparing Bangerter Filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010;117(5):998–1004. doi: 10.1016/j.ophtha.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beck RW. The Pediatric Eye Disease Investigator Group. J AAPOS. 1998;2(5):255–6. doi: 10.1016/s1091-8531(98)90079-9. [DOI] [PubMed] [Google Scholar]
- 7.Holmes JM, Beck RW, Repka MX, et al. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119(9):1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 8.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135(2):194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 9.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132(6):903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 10.Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer-Verlag; 2000. Estimation of the Marginal Model; pp. 41–54. [Google Scholar]
- 11.Higgins JP, Whitehead A, Turner RM, Omar RZ, Thompson SG. Meta-analysis of continuous outcome data from individual patients. Statist Med. 2001;20(15):2219–41. doi: 10.1002/sim.918. [DOI] [PubMed] [Google Scholar]
- 12.Kramer CY. Extension of multiple range tests to group means with unequal numbers of replications. Biometrics. 1956;12(3):307–10. [Google Scholar]
- 13.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to Meta-Analysis. West Sussex, United Kingdom: John Wiley & Sons, Ltd; 2009. Indentifying and quantifying heterogeneity; pp. 107–25. [Google Scholar]
- 14.Pediatric Eye Disease Investigator Group. The course of moderate amblyopia treated with patching in children: experience of the Amblyopia Treatment Study. Am J Ophthalmol. 2003;136(4):620–9. doi: 10.1016/s0002-9394(03)00392-1. [DOI] [PubMed] [Google Scholar]
- 15.Pediatric Eye Disease Investigator Group. The course of moderate amblyopia treated with atropine in children: experience of the Amblyopia Treatment Study. Am J Ophthalmol. 2003;136(4):630–9. doi: 10.1016/s0002-9394(03)00458-6. [DOI] [PubMed] [Google Scholar]
- 16.Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075–87. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Fulton AB, Mayer DL. Esotropic children with amblyopia: effects of patching on acuity. Graefes Arch Clin Exp Ophthalmol. 1988;226(4):309–12. doi: 10.1007/BF02172956. [DOI] [PubMed] [Google Scholar]
- 18.Flynn JT, Woodruff G, Thompson JR, et al. The therapy of amblyopia: an analysis comparing the results of amblyopia therapy utilizing two pooled data sets. Trans Am Ophthalmol Soc. 1999;97:373–95. [PMC free article] [PubMed] [Google Scholar]
- 19.Kracht J, Bachert I, Diehl CM, et al. Electronically recorded occlusion treatment in amblyopes older than 7 years: acuity gain after more than 4 months of treatment? Klin Monbl Augenheilkd. 2010;227(10):774–81. doi: 10.1055/s-0029-1245752. [DOI] [PubMed] [Google Scholar]
- 20.Mintz-Hittner HA, Fernandez KM. Successful amblyopia therapy initiated after age 7 years: compliance cures. Arch Ophthalmol. 2000;118(11):1535–41. doi: 10.1001/archopht.118.11.1535. [DOI] [PubMed] [Google Scholar]
- 21.Fielder AR, Irwin M, Auld R, Cocker KD, Jones HS, Moseley MJ. Compliance in amblyopia therapy: objective monitoring of occlusion. Br J Ophthalmol. 1995;79(6):585–9. doi: 10.1136/bjo.79.6.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simonsz HJ, Polling JR, Voorn R, et al. Electronic monitoring of treatment compliance in patching for amblyopia. Strabismus. 1999;7(2):113–23. doi: 10.1076/stra.7.2.113.645. [DOI] [PubMed] [Google Scholar]
- 23.Loudon SE, Polling JR, Simonsz HJ. Electronically measured compliance with occlusion therapy for amblyopia is related to visual acuity increase. Graefes Arch Clin Exp Ophthalmol. 2003;241(3):176–80. doi: 10.1007/s00417-002-0570-z. [DOI] [PubMed] [Google Scholar]
- 24.Stewart CE, Stephens DA, Fielder AR, Moseley MJ for the ROTAS Cooperative. Objectively monitored patching regimens for treatment of amblyopia: randomised trial. BMJ. 2007;335(7622):707–13. doi: 10.1136/bmj.39301.460150.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pediatric Eye Disease Investigator Group. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006;113(6):895–903. doi: 10.1016/j.ophtha.2006.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rice ML, Leske DA, Holmes JM. Comparison of the Amblyopia Treatment Study HOTV and Electronic-Early Treatment of Diabetic Retinopathy Study visual acuity protocols in children aged 5 to 12 years. Am J Ophthalmol. 2004;137(2):278–82. doi: 10.1016/j.ajo.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 27.Birch EE, Strauber SF, Beck RW, Holmes JM Pediatric Eye Disease Investigator Group. Comparison of the amblyopia treatment study HOTV and the electronic-early treatment of diabetic retinopathy study visual acuity protocols in amblyopic children aged 5 to 11 years. J AAPOS. 2009;13(1):75–8. doi: 10.1016/j.jaapos.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]