Dear Editor
Spontaneous intracranial hypotension (SIH) is an uncommon condition characterized by the depletion of cerebrospinal fluid (CSF) volume [3]. Enlargement of the pituitary gland may occur in SIH due to compensatory engorgement of the epidural venous plexus, which is a potential diagnostic pitfall [2]. We report a 46-year-old woman who presented with a 2-week history of headache and a partial right abducens nerve palsy. Her pituitary hormonal profiles were normal except for raised serum alpha-subunit, follicle stimulating hormone and luteinizing hormone levels, compatible with her previous oophorectomy.
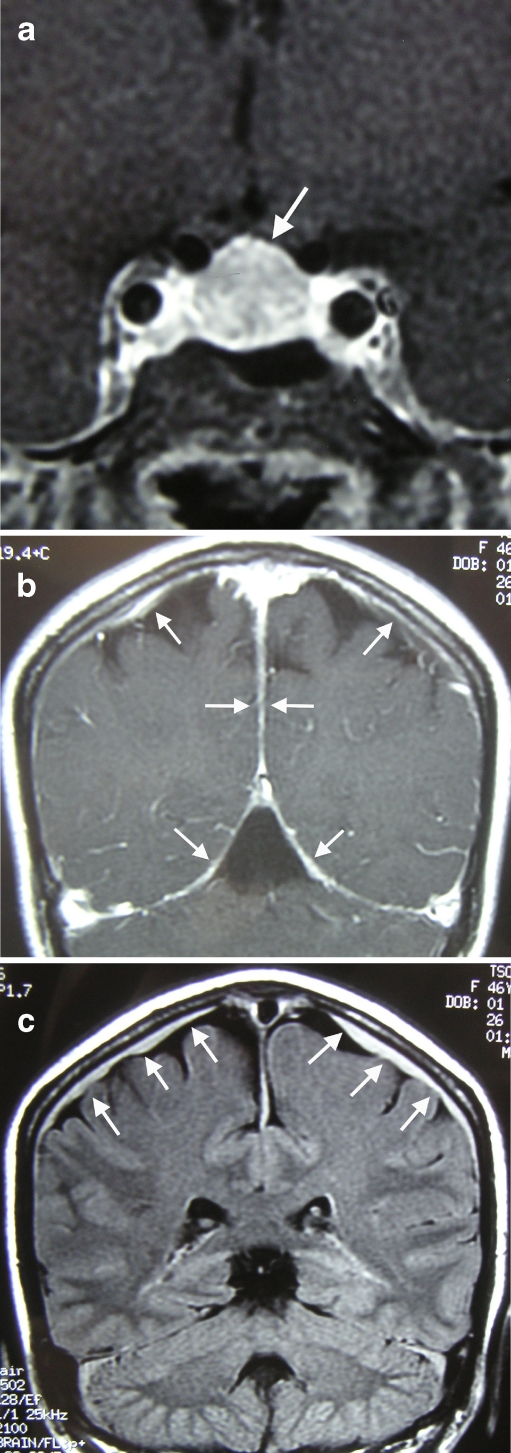
Magnetic resonance (MR) studies showed an enlarged pituitary gland, which was then diagnosed as a non-functioning pituitary macroadenoma. Less emphasis was placed on other MR findings including bilateral subdural effusion, pachymeningeal enhancement, and sagging of the midbrain, which were suggestive of SIH (Fig. 1). Endoscopic transsphenoidal surgery was performed, which revealed a diffusely enlarged pituitary gland. Biopsy showed no inflammatory or neoplastic changes. Her headache and diplopia resolved 2 weeks later. A follow-up MR study showed complete resolution of the pachymeningeal enhancement, bilateral subdural effusion, and pituitary enlargement. The overall picture was that of SIH that had resolved spontaneously.
Fig. 1.
a, b Post-contrast T1-weighted coronal images showing an enlarged and homogeneously enhancing pituitary gland, and diffuse pachymeningeal enhancement (arrows); c coronal FLAIR image showing the bilateral subdural effusion (arrows)
SIH is most commonly due to spontaneous CSF leakage at the lower cervical and upper thoracic spine. Mechanical stress, meningeal diverticula, and connective tissue disorders have been identified as potential risk factors. The estimated incidence is around 5 per 100,000 per year, with a female predominance and a peak incidence around the 4th decade [8]. Patients may present with orthostatic headache, nausea, vomiting, neck rigidity, and cranial nerve palsies [4]. The characteristic MR findings include pachymeningeal thickening and enhancement, tonsillar descent into the foramen magnum, and subdural effusion [8]. As the craniospinal axis attempts to maintain volume homeostasis in the face of continuous CSF loss, dural hyperemia and associated enlargement of the pituitary gland may occur in up to two-thirds of the cases [6].
The initial MR findings should have raised the suspicion of SIH in our patient. On retrospective enquiry, her headache was indeed postural in nature. We performed surgery with a view to improve her abducens nerve palsy. The latter was a recognized feature of SIH, accounting for up to 80% of reported ocular manifestations of this syndrome [10]. The optic, oculomotor, trochlear, and trigeminal nerves may also be affected [1]. Other unusual pituitary manifestations of SIH include hemorrhage [9] and partial insufficiency [7]. Interestingly, an unusual case of SIH associated with a pituitary macroadenoma and subdural hemorrhage has also been described [5].
The majority of patients with SIH improve on conservative management, and almost all cases with pituitary enlargement have normalization of gland size on follow-up MR [2]. For refractory cases, myelography is the study of choice to identify the site of spinal CSF leakage, followed by definitive treatments such as epidural blood patching, percutaneous placement of fibrin sealant, and open surgical repair.
In summary, SIH should be considered in patients who present with postural headache and the characteristic MR findings. Initial conservative management should be adopted, which is effective in the majority of cases. The present case illustrates the importance of careful history taking and clinical examination as well as an awareness of this diagnostic pitfall.
Acknowledgments
Conflicts of interest
None
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Albayram S, Asik M, Hasiloglu ZI, Dikici AS, Erdemli HE, Altintas A. Pathological contrast enhancement of the oculomotor and trigeminal nerves caused by intracranial hypotension syndrome. Headache. 2011;51:804–808. doi: 10.1111/j.1526-4610.2010.01825.x. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez-Linera J, Escribano J, Benito-Leon J, Porta-Etessam J, Rovira A. Pituitary enlargement in patients with intracranial hypotension syndrome. Neurology. 2000;55:1895–1897. doi: 10.1212/wnl.55.12.1895. [DOI] [PubMed] [Google Scholar]
- 3.Couch JR. Spontaneous intracranial hypotension: the syndrome and its complications. Curr Treat Options Neurol. 2008;10:3–11. doi: 10.1007/s11940-008-0001-5. [DOI] [PubMed] [Google Scholar]
- 4.Ferrante E, Savino A, Sances G, Nappi G. Spontaneous intracranial hypotension syndrome: report of twelve cases. Headache. 2004;44:615–622. doi: 10.1111/j.1526-4610.2004.446012.x. [DOI] [PubMed] [Google Scholar]
- 5.Firat AK, Karakas HM, Firat Y, Kahraman B, Erdem G. Spontaneous intracranial hypotension with pituitary adenoma. J Headache Pain. 2006;7:47–50. doi: 10.1007/s10194-006-0269-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forghani R, Farb RI. Diagnosis and temporal evolution of signs of intracranial hypotension on MRI of the brain. Neuroradiology. 2008;50:1025–1034. doi: 10.1007/s00234-008-0445-z. [DOI] [PubMed] [Google Scholar]
- 7.Platz J, Glucker T, Gratzl O, Woydt M. Spontaneous intracranial hypotension: case report with subdural hematomas, steroid dependency and clinical improvement after myelography. Zentralbl Neurochir. 2007;68:87–90. doi: 10.1055/s-2007-977738. [DOI] [PubMed] [Google Scholar]
- 8.Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286–2296. doi: 10.1001/jama.295.19.2286. [DOI] [PubMed] [Google Scholar]
- 9.Spero M, Lazibat I, Stojic M, Vavro H (2011) Normal pressure form of the spontaneous intracranial hypotension: a case report with pituitary enlargement and asymptomatic pituitary haemorrhage. Neurol Sci PMID 21484357 [DOI] [PubMed]
- 10.Zada G, Solomon TC, Giannotta SL. A review of ocular manifestations in intracranial hypotension. Neurosurg Focus. 2007;23:E8. doi: 10.3171/FOC-07/11/E8. [DOI] [PubMed] [Google Scholar]