Abstract
Social characteristics (e.g. race, gender, age, education) are associated with health care disparities. We introduce social concordance, a composite measure of shared social characteristics between patients and physicians.
Objective
To determine whether social concordance predicts differences in medical visit communication and patients’ perceptions of care.
Methods
Regression analyses were used to determine the association of patient-provider social concordance with medical visit communication and patients’ perceptions of care using data from two observational studies involving 64 primary care physicians and 489 of their patients from the Baltimore, MD /Washington, DC/Northern Virginia area.
Results
Lower patient-physician social concordance was associated with less positive patient perceptions of care and lower positive patient affect. Patient-physician dyads with low vs. high social concordance reported lower ratings of global satisfaction with office visits (OR=0.64 vs. OR=1.37, p=0.036) and were less likely to recommend their physician to a friend (OR=0.61vs. OR=1.37, p=0.035). A graded-response was observed for social concordance with patient positive affect and patient perceptions of care.
Conclusion
Patient-physician concordance across multiple social characteristics may have cumulative effects on patient-physician communication and perceptions of care.
Practice Implications
Research should move beyond one-dimensional measures of patient-physician concordance to understand how multiple social characteristics influence health care quality.
Keywords: patient-provider communication, health care disparities, patient-provider concordance
1. Introduction
The notion that disparities in health and health care may result from a combination of relational factors within the patient-physician relationship and contextual and structural factors that result in status differentials for social groups within society based on race, gender, age, or other shared social or cultural characteristics is gaining support(1;2). Patient social characteristics such as race, gender, age, and education are associated with disparities in health care (3); are linked to treatment adherence (4), decision-making (5), and satisfaction (6–10); and are also associated with health outcomes(11–13). Research suggests physicians also bring expectations, biases, and values to medical visits (14;15). And, physicians’ own social characteristics influence the way they are perceived by patients (16–20).
Studies have found that physicians are more likely to view African-American patients as noncompliant or less intelligent than whites (14), and health care providers have more positive appraisals of patients who are better educated and employed (21). Our previous work demonstrated differences in the content and tone of medical visit communication for African-American versus white patients such that physicians are more verbally dominant with African Americans and have a less positive tone than with whites (22). Differences in patient-provider communication are also associated with patients’ social class (23) and gender (24), and with physician gender (25). Older patients also tend to have an expectation that the patient-physician relationship should be more dominated by physician expertise that do younger patients, which also has implications for medical visit communication (26).
Concordance is defined as the degree of patient and physician similarity or agreement across a given dimension. Sharing specific social characteristics (e.g. gender, race, socioeconomic status, education), expectations, beliefs, and perceptions impact health care quality (7–10;20;23;27;27;28;28–41). Current literature on patient-physician concordance studies most often involves analyses that examine one shared characteristic in isolation from others. Therefore, the need to understand the cumulative impact of patient-physician concordance on communication and healthcare quality persists. We establish a framework for a multidimensional measure of shared social characteristics, called social concordance.
Social concordance (SC) is related to the concepts of homophily and interpersonal perceptions(42;43), but it is a distinct construct. While homophily focuses on the probability of contact between people increasing with increasing similarity, SC is an evaluation of similarity with respect to social identity characteristics (e.g. race, gender, education, age) of participants in a specific interaction and does not evaluate the extent to which their social networks differ. While the concept of interpersonal perceptions applies directly to participants in a given interaction, it focuses on the extent to which participants (e.g. doctors and patients) share similar perceptions and values (43). That values and perceptions among members of the same social groups often correspond more closely than among members of different social groups is not insignificant (42), yet it does represent an important distinction between SC and interpersonal perceptions. We define SC in relation to status homophily because it is based on similarities with respect to status related identity characteristics (e.g. race, gender, age, education) versus an explicit set of shared values or beliefs (42;43). Our conceptualization of social concordance includes dimensions that are clearly visible (i.e. gender, ethnicity and age) and less immediately obvious identity characteristic (i.e. education). All of these relate to social status within interactions, which is what unifies them. As such, SC does not explicitly capture shared values, beliefs, or perceptions.
This study aims to determine whether SC is associated with differences in the quality of medical visit communication and patients’ perceptions of care. We hypothesized that lower patient-physician SC is associated with lower quality medical visit communication and less positive patient perceptions of care.
2. Methods
2.1 Study Design and Population
We used data from two brief cohort studies conducted from July 1998–June 1999 and January–November 2002. The details of data collection are summarized elsewhere (22;32). The protocols were reviewed and approved by the Johns Hopkins Medical Institutions Institutional Review Board and informed consent was obtained from all participants. Physicians were recruited from group practices and federally qualified health centers in the Baltimore/Washington, D.C./northern Virginia area. Both studies targeted practices with a high percentage of African-American physicians and patients.
Patients were eligible to participate if they were: 1) 18 years of age or older and 2) seeing their physician on the recruitment days. Only African-American and white patients were recruited for the 1998 study. Patients of all racial/ethnic backgrounds were eligible to participate in the 2002 study. Patients who appeared too acutely ill or cognitively impaired to complete study questionnaires and participate in the interview were not approached. Attempts were made to recruit patients who had previously seen the physician, but there was no pre-established length of relationship required for participation.
2.2 Data Collection
Informed consent was obtained from all participants. They were told the goal of the study was to learn about how doctors and patients communicate. Patients completed a 5-minute survey that included questions regarding their health status and social characteristics. Research assistants set up a tape recorder in the physician’s office, started the recording, and left the room. Physicians and patients were instructed that they could turn off the tape recorder or pause the recording at any time. Physicians also completed a background questionnaire and a post-visit questionnaire. The background questionnaire provided information about their social characteristics and medical credentials (e.g. time since completing training, exposure to communication skills training). The post-visit questionnaire asked physicians how well the physician felt he/she knew the patient seen during the preceding visit.
Audio taped medical visits were coded with the Roter Interaction Analysis System (RIAS), which provides a framework for understanding the dynamics of patient-physician communication medical visits and has well-established reliability and predictive validity (44;45). The RIAS captures four functions medical visits: data gathering, patient education and counseling, responding to patient emotions, and partnership building (44). Coders are asked to rate the global affect of the patient and the physician across several dimensions on a scale of 1–6 (1=low/none, 6=high). The two highly experienced coders (both white women) were unaware of study hypotheses. Overall reliability for RIAS coding of patient and physician talk were similar for the 1998 and 2002 studies (0.79–0.86 and 0.88–0.90 respectively)(22;32).
2.3 Measures
The independent variable in this study is social concordance (SC). SC is an additive composite score accounting for the degree of patient-physician concordance across four social characteristics: race, gender, age, and education. Study participants self-identified as: 1) white (not of Latino origin), 2) Black (not of Latino origin), 3) Hispanic or Latino, 4) Asian or Pacific Islander, and 5) American Indian or Alaskan Native. Physicians were also given the option to write-in their race in an “other” category. Patients (n=9) who identified as members of more than one racial/ethnic group or who identified their race as other than white or African-American (n=9) were excluded from analyses. Patient-physician dyads who reported membership in the same racial group were categorized as race concordant. Dyads were gender concordant when the patient and physician self-reported the same gender.
Patients in both cohorts and physicians in the 2002 cohort were asked their date-of-birth. Their age at the time of the medical visit was calculated using their reported birth date and the date of the audio taped medical visit. Age of physicians in the 1998 cohort was estimated since birthdates were not available. We used the mean age upon completing training from the 2002 cohort as the estimated age upon completing training for all physicians in the 1998–1999 cohort. Estimated physician age was equal to the estimated mean age upon completing training plus the subsequent number of years to the time of the study visit. The actual or estimated age of physicians was subtracted from the age of the patient at the time of the visit to obtain an absolute age difference (years) for each dyad. Dyads were categorized as age concordant when patient and physician ages were within 5 years of one another.
Each patient reported the total number of years of education he/she had completed on the background questionnaire. Patients who had completed 4 years or more of college were coded as having completed at least 4 years of post-high school education. Based on this coding system, all physicians would also have been coded as having completed at least 4 years of post-high school education. Any patient who reported completing at least 4 years of college was considered to be educationally concordant with his/her physician.
SC is a composite that attributes equal weight to all four social characteristics described above. For example, a race concordant, gender discordant, age discordant and educationally concordant dyad would receive the same overall score as a race discordant, gender concordant, age concordant, and educationally discordant dyad (SC score = 2). This approach generated SC scores ranging from 0 to 4. Because there were a small number (n=16) of completely concordant dyads, for analytic purposes, we collapsed the scale into three ordinal categories: high (reference group, score of 3 or more), medium (score =2), and low (score of 1 or less) SC.
Patient-physician communication and patients’ perceptions of care are the main outcomes. Patient-physician communication was assessed using measures derived from coding of audiotaped medical visit using the RIAS. Medical visit duration was based on the amount of time (in minutes) that transpired from the start of the medical visit until its conclusion. Physician verbal dominance and Physician patient-centeredness scores have been used in other manuscripts and are intended to reflect the overall patient-centered orientation of the visit (22;26;32;45;46). Positive affect scale scores were calculated separately for physicians and patients by summing coders' global ratings for each across several affective dimensions. Inter-item reliability (Cronbach’s α) for both scales was high (patient positive affect α=0.83; physician positive affect α=0.91) (22). A detailed description of the methods used to create these scores is described in an earlier publication (32).
Participatory Decision-Making (PDM Score)
Three items were used to evaluate patients’ perceptions of their physicians’ participatory decision-making style, each of which is rated on a five-point scale (from 0 to 4) and has been described in other publications by these authors (31;32). A higher PDM score means the visit was more participatory (31;47;48). Global Satisfaction – Patients were asked to report the degree to which they agreed (1=strongly disagree, to 5=strongly agree) with the statement: “Overall, I was satisfied with the visit”. Based on the distribution of responses, the global satisfaction score was dichotomized. Those patients reporting strong agreement were compared to all others. Recommendation of Physician to a Friend – Patients were asked whether they would recommend their physician to a friend or not. Responses were dichotomized such that patients reporting strong agreement that they would recommend their physician to a friend were compared to all others.
2.4 Statistical Analysis
Univariate linear regression analyses were performed relating all social characteristics and all concordance measures used to create the SC score with the outcomes of interest. Because age, race, gender, and education of both patients and physicians are used to calculate the SC score, we did not include these characteristics as individual-level covariates in our models. In all cases, inclusion of the individual-level covariates in addition to the composite SC score (i.e. including patient race, gender, age, or education and/or the physician equivalents) would be over-controlling the model and essentially controlling for these characteristics more than once, which would likely increase our likelihood of type 2 error and result in accepting the null hypothesis when it is actually false. We included only three covariates that we decided a priori may be important for patient-physician communication and patients’ ratings of care: 1) patient’s self-rated health status, 2) physician’s appraisals of how well they know a given patient, and 3) whether the dyad was from the 1998–1999 or the 2002 study sample.
We used the generalized estimating equation (GEE) method for correlated data (49) in all regression analyses in order to account for the inclusion of multiple patient visits with the same physician, which resulted in non-independence of physicians across multiple patient observations. An exchangeable correlation structure was assumed using robust estimation, which is likely to yield more accurate or valid coefficient estimates, even if the correlation structure is mis-specified (50). Because some physicians practiced at more than one site, analyses were not designed to account for intra-class correlation within sites.
3. Results
Data was collected for a total of 548 patients. All patients who did not report their race/ethnicity were excluded from analyses (n=9). Of the 539 patients who reported their race/ethnicity, those who reported membership in more than one racial/ethnic group (n=9) or who did not identify as either African American/black or white (n=9) were excluded from analyses in order to maximize the construct validity of the SC score. The final sample included 489 patients (255 African Americans and 234 whites) who saw one of 64 study physicians (35 whites, 19 African Americans, and 10 Asians). Sample characteristics are summarized in Tables 1–2.
Table 1.
Characteristics of Patients in Patient-Physician Dyads by Social Concordance Score
| Total | High Concordance (share 3 or more characteristics) |
Medium Concordance (share 2 characteristics) |
Low Concordance (share 1 or fewer characteristic) |
||
|---|---|---|---|---|---|
| (N=489)a | (n=74)a | (n=163)a | (n=252)a | p-value* | |
|
Time of Medical Visit and Questionnaire Completion | |||||
| Wave 1 (1998) | 221 (45.2) | 28 (37.8) | 101 (62.0) | 92 (36.5) | |
| Wave 2 (2002) | 268 (54.8) | 46 (62.2) | 62 (38.0) | 160 (63.5) | <0.001 |
|
Patient Demographics | |||||
| Mean Age (SD) | 49.8 (16.3) | 44.0 (13.8) | 48.4 (15.1) | 52.5 (17.2) | <0.001 |
| Gender (%) | |||||
| Male | 164 (33.5) | 29 (39.2) | 57 (35.0) | 78 (31.0) | |
| Female | 325 (66.5) | 45 (60.8) | 106 (65.0) | 174 (69.0) | 0.374 |
| Race (%) | |||||
| White | 234 (47.9) | 55 (74.3) | 75 (46.0) | 104 (41.3) | |
| African American | 255 (52.1) | 19 (25.7) | 88 (54.0) | 148 (58.7) | <0.001 |
| Mean (SD) Years of Education | 12.6 (2.7) | 15.7 (2.0) | 12.5 (2.5) | 11.8 (2.3) | <0.001 |
| Self-rated health status (%) | |||||
| Poor/Fair | 140 (28.8) | 4 (5.4) | 42 (25.8) | 94 (37.6) | |
| Good | 186 (38.2) | 23 (31.1) | 64 (39.2) | 99 (39.6) | |
| Very good/Excellent | 161 (33.0) | 47 (63.5) | 57 (35.0) | 57 (22.8) | <0.001 |
| How well patient is known by his/her physician (%)** | |||||
| Very well | 180 (42.4) | 25 (37.3) | 60 (46.5) | 95 (41.5) | |
| Somewhat | 160 (37.6) | 28 (41.8) | 48 (37.2) | 84 (36.7) | 0.619 |
| Not at all (new patient) | 85 (20.0) | 14 (20.9) | 21 (16.3) | 50 (21.8) | |
Differences across groups are analyzed using chi-square and analysis of variance for categorical and continuous variables respectively.
Sample sizes reflect total number of patient participants. Actual sample size is lower for certain characteristics due to item non-response.
This characteristic is derived from physician responses to a question about how well they know each patient of theirs who is included in this study.
Table 2.
Characteristics of Physicians in Patient-Physician Dyads by Social Concordance Score
| Total (N=489)a |
High Concordance (share 3 or more characteristics) (n=74)a |
Medium Concordance (share 2 characteristics) (n=163)a |
Low Concordance (share 1 or fewer characteristics) (n=252)a |
p- value* |
|
|---|---|---|---|---|---|
|
Demographics of Physicians Seen by Study Patients | |||||
| Gender of physician seen (%) | |||||
| Male | 255 (52.1) | 37 (50.0) | 71 (43.6) | 147 (58.3) | |
| Female | 234 (47.9) | 37 (50.0) | 92 (56.4) | 105 (41.7) | 0.012 |
| Race of physician seen (%) | |||||
| White | 274 (56.0) | 56 (75.7) | 78 (47.9) | 140 (55.6) | |
| African American | 139 (28.4) | 18 (24.3) | 70 (42.9) | 51 (20.2) | |
| Asian | 76 (15.6) | 0 | 15 (9.2) | 61 (24.2) | <0.001 |
| Has physician done communication skills training? | |||||
| Yes | 261 (53.4) | 41 (55.4) | 80 (49.1) | 140 (55.6) | |
| No | 228 (46.6) | 33 (44.6) | 83 (50.9) | 112 (44.4) | 0.404 |
| Mean Age (SD) | 42.6 (7.9) | 43.3 (8.3) | 43.0 (8.8) | 42.1 (7.0) | 0.333 |
| Mean (SD) years since MD completed training(%) | 10.1 (7.7) | 11.0 (7.8) | 10.4 (8.6) | 9.7 (7.0) | 0.359 |
Differences across groups are analyzed using chi-square and analysis of variance for categorical and continuous variables respectively.
Sample sizes reflect total number of patient participants. Actual sample size is lower for certain characteristics due to item non-response.
The mean age of patients overall was 49.8 years. Patients in mostly concordant dyads (high SC) were younger than those in somewhat concordant dyads (medium SC), who were younger than those in mostly discordant dyads (low SC). White patients were statistically significantly more likely (p<0.001) to be in high SC dyads (74.3% white v. 25.7% African American) versus medium (46% white v. 54% African American) or low SC dyads (41.3% white v. 58.7% African American).
The overall mean education level for patients was 12.6 years. Patients’ educational level decreases with decreasing SC such that patients in high SC dyads have the highest mean education level (15.7 years) and patients in medium and low SC dyads have statistically significantly lower (p<0.001) mean education levels (12.5 years and 11.8 years respectively). While only one third of patients in the sample reported their health as very good or excellent, statistically significantly (p<0.001) more patients in high SC dyads reported very good to excellent health (63.5%) versus medium (35%) or low (22.8%) SC dyads.
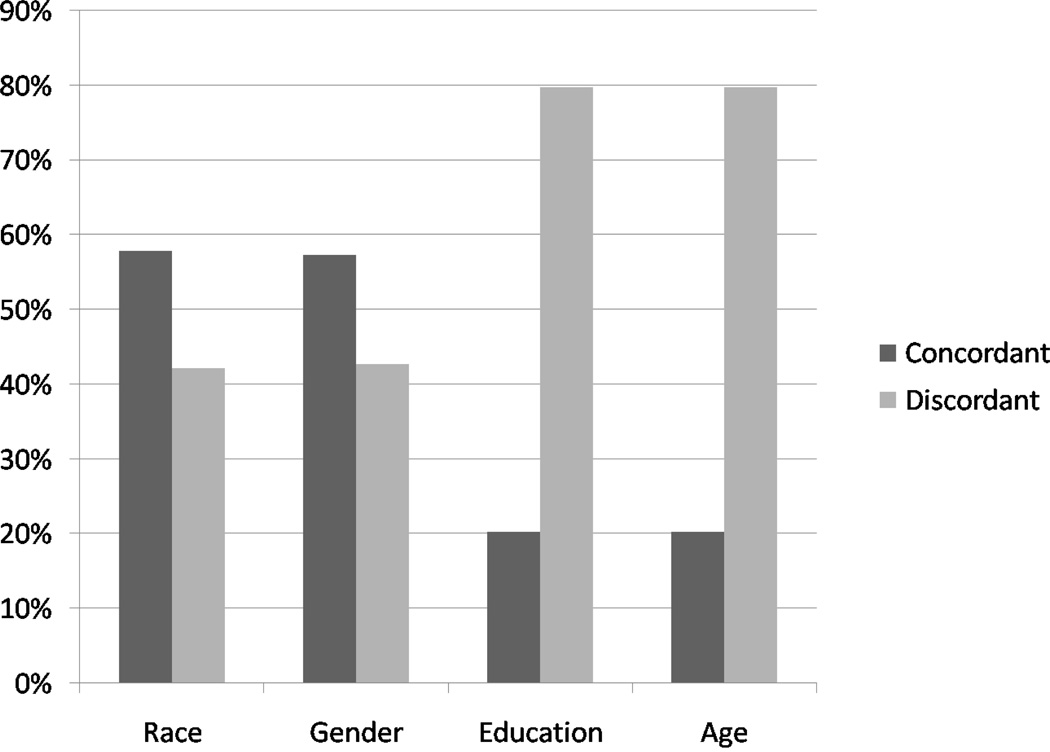
Table 2 summarizes the characteristics of physicians in high, medium, and low SC dyads. All Asian physicians were from the 2002 study and were part of medium or low SC dyads (n=15 and n=61, respectively). Statistically significantly (p<0.001) more high SC dyads (76%) involved white physicians versus medium and low SC (47.9% and 55.6% respectively). Figure 1 summarizes the proportion of concordant versus discordant dyads for each of the 4 social characteristics included in the SC score. Table 3 examines the patterns of concordance across high, medium, and low SC dyads. Of interest, nearly 99% of the dyads with high SC were race concordant whereas only 55% of high SC dyads were age concordant.
Figure 1.
Proportion of Concordant vs. Discordant Patient-Physician Dyads with Respect to Each Social Characteristic Included in the Social Concordance Score
Table 3.
Characteristics of Patient-Physician Dyads by Social Concordance Score
| High Concordance (share 3 or 4 characteristics) (N=74) |
Medium Concordance (share 2 characteristics) (N=163) |
Low Concordance (share 1 or fewer characteristic) (n=252)a |
p-value | |
|---|---|---|---|---|
| Physician-patient race concordance (%) | ||||
| Concordant | 73 (98.7) | 132 (81.0) | 78 (31.0) | |
| Discordant | 1 (1.3) | 31 (19.0) | 174 (69.0) | <0.001 |
| Physician-patient gender concordance (%) | ||||
| Concordant | 64 (86.5) | 127 (77.9) | 89 (35.3) | |
| Discordant | 10 (13.5) | 36 (22.1) | 163 (64.7) | <0.001 |
| Physician-patient education concordance | ||||
| Concordant (patient with 4+ yrs of college) | 60 (81.1) | 27 (16.6) | 12 (4.8) | |
| Discordant (patient with <4 yrs of college) | 14 (18.9) | 136 (83.4) | 240 (95.2) | <0.001 |
| Physician-patient age concordance | ||||
| Concordant (+/−5yrs difference in ages) | 41 (55.4) | 40 (24.5) | 18 (7.1) | |
| Discordant (>5 yrs difference in ages) | 33 (44.6) | 123 (75.5) | 234 (92.9) | <0.001 |
Differences across patient-physician groups are analyzed using chi-square and analysis of variance for categorical and continuous variables respectively.
Sample sizes here reflect the total number of patient participants. Actual sample size is lower for certain characteristics due to item non-response
Decreasing patient-physician SC was statistically significantly associated with decreasing patient positive affect for both medium and low SC dyads as compared to high SC dyads in multivariate analyses (Table 4). Furthermore, there appeared to be a graded-response relation between social concordance and positive affect (p for trend=0.017).
Table 4.
Relationship of Patient-Physician Dyad Social Concordance Score to Medical Visit Communication
| Total Sample | High Concordance (share 3 or more social characteristics)€ |
Medium Concordance (share 2 social characteristics)€ |
Low Concordance (share 1 or fewer social characteristics)€ |
||
|---|---|---|---|---|---|
| (N=453) | (n=48) a | (n=154)a | (n=184)a | ||
| Mean (95% CI) | Mean (95% CI) | p- value* |
Mean (95% CI) | p- value** |
|
| Duration of Visit (minutes) | |||||
| Univariate Model | 15.95 (13.29–18.62) | 15.83 (14.40–17.27) | 0.935 | 16.27 (14.72–17.82) | 0.827 |
| Multivariate Model*** | 16.92 (13.97–19.87) | 16.10 (14.45–17.76) | 0.610 | 15.72 (13.97–17.47) | 0.473 |
| Speech Speed‡ | |||||
| Univariate Model | 24.07 (21.97–26.17) | 25.22 (23.78–26.66) | 0.328 | 24.86 (23.74–25.98) | 0.459 |
| Multivariate Model*** | 24.56 (22.26–26.85) | 25.31 (23.85–26.78) | 0.578 | 24.93 (23.65–26.21) | 0.762 |
| Physician Verbal Dominance†† | |||||
| Univariate Model | 1.43 (1.30–1.56) | 1.55 (1.43–1.68) | 0.135 | 1.54 (1.43–1.64) | 0.160 |
| Multivariate Model*** | 1.44 (1.31–1.58) | 1.60 (1.45–1.75) | 0.100 | 1.58 (1.48–1.69) | 0.077 |
| Physician Patient-Centeredness¥ | |||||
| Univariate Model | 1.29 (1.00–1.59) | 1.29 (1.03–1.54) | 0.984 | 1.25 (1.09–1.42) | 0.829 |
| Multivariate Model*** | 1.39 (1.04–1.74) | 1.32 (1.02–1.63) | 0.745 | 1.15 (1.03–1.26) | 0.180 |
| Patient Positive Affect | |||||
| Univariate Model | 17.61 (170.05–18.17) | 17.10 (16.62–17.59) | 0.097 | 17.06 (16.71–17.44) | 0.085 |
| Multivariate Model***† | 18.03 (17.47–18.59) | 17.16 (16.63–17.69) | 0.010 | 17.02 (16.63–17.42) | 0.003 |
| Physician Positive Affect | |||||
| Univariate Model | 0.52 (0.20–0.84) | 0.64 (0.09–1.20) | 0.568 | 0.65 (0.37–0.93) | 0.369 |
| Multivariate Model*** | 0.54 (0.13–0.96) | 0.64 (0.01–1.27) | 0.672 | 0.64 (0.41–0.87) | 0.633 |
The social characteristics are: race, gender, age, and years of education. Dyads share a given characteristic when they concordant as defined in Table 3.
The sample size reflects the number of observations included in most univariate analyses (within 1%). Multivariate analyses include 14–15% fewer cases due to item non-response.
P-value from GEE for medium concordance vs. high concordance dyads (reference group).
P-value from GEE low concordance vs. high concordance dyads (reference group).
Multivariate Model covariates: individual patient self-rated health status, 1998 vs. 2002 cohort, physician appraisal of how well he/she knows patient.
Speech speed = (all patient talk + all physician talk) / visit duration (in minutes).
Verbal Dominance score = total physician talk / total patient talk.
Patient-Centered Interviewing score =all psychosocial and socioemotional talk / all biomedical talk
p for trend <0.05
As displayed in Table 5, social concordance was associated with several measures of patient perception of care. The odds of patients strongly agreeing that they were completely satisfied with their care was statistically significantly lower for patients in low versus high SC dyads in univariate and multivariate analyses (OR=0.64 95% CI 0.39–0.89, p=0.036 for multivariate analysis). In addition, there appeared to be a graded-response relation between SC and odds of satisfaction with care (p for trend= 0.011and 0.016 for univariate and multivariate models respectively). Patients in low versus high SC dyads were less likely to strongly agree that they would recommend their physician to a friend (OR=0.55, 95% CI 0.26–0.84 in unadjusted analyses p=0.051). This relationship was statistically significant in the adjusted model (OR=0.61, 95%CI 0.26–0.95, p=0.035). As with global satisfaction, there were no statistically significant differences in the odds of recommending one’s physician to a friend among patients in medium versus high SC dyads, but as above, there was a statistically significant trend indicating the presence of a likely graded-response relation between SC and odds of recommending one’s physician to a friend (p for trend=0.035 and 0.027 univariate and multivariate models respectively).
Table 5.
Relationship of Overall Patient-Physician Social Concordance Score to Patient Perceptions of Care
| Total Sample | High Concordance (share 3 or more social characteristics) |
Medium Concordance (share 2 social characteristics) |
Low Concordance (share 1 or fewer social characteristics) |
||
|---|---|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | p- value* |
Mean (95% CI) | p- value** |
|
| (N=486) | |||||
| Participatory Decision-Making Score₣ | |||||
| Univariate Model | 80.40 (76.06–84.75) | 81.08 (77.88–84.28) | 0.804 | 78.62 (75.63–81.62) | 0.516 |
| Multivariate Model*** | 79.62 (75.14–84.10) | 81.49 (78.22–84.76) | 0.529 | 77.96 (74.52–81.40) | 0.569 |
| OR (95% CI) | OR (95% CI) |
p- value* |
OR (95% CI) |
p- value** |
|
| Global Satisfaction Rating (1=strongly agree, 0=agree/neutral/disagree) π | |||||
| Univariate Model† | 1.21 (0.64–1.79) | 0.76 (0.40–1.13) | 0.174 | 0.53 (0.27–0.80) | 0.023 |
| Multivariate Model***† | 1.37 (0.72–2.02) | 0.80 (0.40–1.20) | 0.126 | 0.64 (0.39–0.89) | 0.036 |
| Recommendation of Physician to a Friend (1=strongly agree, 0=agree/neutral/disagree)¶ | |||||
| Univariate Model† | 1.09 (0.60–1.58) | 0.81 (0.42–1.20) | 0.344 | 0.55 (0.26–0.84) | 0.051 |
| Multivariate Model***† | 1.37 (0.76–1.98) | 0.97 (0.52–1.42) | 0.268 | 0.61 (0.26–0.95) | 0.035 |
The social characteristics are: race, gender, age, and years of education. Dyads share a given characteristic when they are concordant as defined in Table 3.
The sample size reflects the number of observations included in most univariate analyses (within 1%), with the exception of participatory decision-making score (n=425). Multivariate analyses include 12–13.5% fewer cases than univariate analyses due to item non-response.
P-value from GEE for medium concordance vs. high concordance dyads (reference group).
P-value from GEE low concordance vs. high concordance dyads (reference group).
Multivariate Model covariates: individual patient self-rated health status, 1998 vs. 2002 cohort, physician appraisal of how well he/she knows patient.
Participatory Decision-Making Score uses patient ratings of physicians' likelihood of giving them choice, control, and responsibility in decision-making (0–100 point scale).
Global satisfaction reflects patient responses to: “Overall, I was satisfied with this visit.” (5-point Likert scale). The item was dichotomized: 1=strongly agree, 0=less than strongly agree.
Recommendation of physician to a friend reflects patient responses to: “I would recommend this physician to a friend.” (5-point Likert scale). The item was dichotomized: 1=strongly agree, 0=less than strongly agree
p for trend <0.05
4. Discussion and Conclusion
Social identity often evokes images of status, power and privilege. In this regard, lower levels of social concordance in the doctor and patient relationship almost always reflects higher levels of patient vulnerability. But the construct of social concordance also embodies areas of commonality, and in this regard it provides a wider window into the nature of social relationships that develop between doctors and patients during medical visits. In fact, to the extent that shared social characteristics between patients and doctors create a space for common understanding or shared context that serves as the backdrop for improving communication, our exploration of social concordance is a way of understanding the complex web of social characteristics that influence medical visit communication and patients’ perceptions of care.
4.1 Discussion
The results of this study suggest that SC is positively associated with patient satisfaction with care and may affect the communication and affective tone of medical visits. While one could view such research as supporting matching patients with providers who share particular social characteristics, we argue that this is not the principal implication of our findings. Rather, when taking into account the differences that exist in the demographic composition of the physician workforce and the U.S. population, it is clear that understanding the potential cumulative effects of social status differences in patient-physician dyads is critical to improving the quality of care for patients who are less likely to share social characteristics with their physicians. This could be accomplished through many mechanisms but will likely require concerted efforts on the part of physicians to bridge the divide with patients whose social status differs significantly on multiple dimensions from their physicians. Furthermore, we think it important to emphasize that while SC is associated with patient positive affect and patient perceptions of care (global satisfaction and recommendation of physician to a friend), it is worth noting that explicit communication elements of the medical dialogue do not seem to vary with SC. We think it is reasonable to suggest that the primary response to social concordance is in the affective and non-verbal realm, rather than the more cognitive and verbally explicit domains of communication (51).
Many outcomes associated with SC were also associated with race concordance (32). Given the high correspondence between SC and race concordance, our result might not be unexpected. However, in light of the statistically significant graded-response trends observed, it would be inappropriate to wholly attribute our findings to race concordance alone. The nature of social relationships that develop between patients and their doctors is more complex and rich than is represented by a single marker, even one as culturally meaningful for American society as race and ethnicity. In exploratory analyses (data not presented), we found that each concordance measure was independently associated with several outcomes, however, the pattern of relationships observed for the 4-measure social concordance composite is unique and is not entirely duplicated by race, gender, education or age concordance as an independent covariate. That being said, it is possible that there is a threshold at which concordance with respect to social characteristics can be most strongly associated with medical visit communication. Because the SC scale we employed in this analysis does not differentially weight one social characteristic versus another, it is possible that the specific influence or dominance of a social characteristic such as race is underappreciated. In fact, identifying the threshold at which concordance on one versus another social characteristic matters more would be a logical next step in further characterizing the extent to which shared social characteristics have cumulative versus threshold effects on interpersonal interactions in the patient-provider relationship.
Furthermore, our conceptualization of SC is based on only four social identity characteristics. It should be considered a first attempt at characterizing the cumulative shared social identities that affect patient-physician relationships. There may be other markers to consider for instance, when patients do not speak the same primary language as their physician, or when the patient uses another mode of communication such as American Sign Language, or when patients' limited literacy restricts their ability to understand and be understood by their physician (52). In a similar vein, our measure does not account for values, beliefs, and ideologies that may represent additional sources of SC; nor does it address perceived similarity. Work by Street et al (41) suggests, however, that perceived similarity is highly correlated with race concordance.
That being said, it is quite possible that other characteristics matter more to some patients than any of the social status characteristics included in the SC score. Understanding more about how a wide array of shared characteristics exerts cumulative effects on patient-provider communication is an area ripe for further research. Furthermore, understanding how attitudes and implicit stereotypes affect patient-provider interactions is critical to improving our understanding of the potential mechanisms by which social status characteristics affect patient-provider interactions.
Additional limitations of this study include non-random sampling of physicians and patients, and inclusion of a limited range of racial/ethnic groups. In particular, we were unable to assess within group heterogeneity for any of the ethnic groups included in this study. While this issue is most often raised as a methodological concern for Hispanic and Asian research participants, we recognize that African-Americans represent a broad array of cultural groups as do whites. The precision associated with individual concordance measures may differ across social characteristics and patient and physician self-reports of their own race/ethnicity may not always reflect how they are perceived by one another. We did not collect information on post-college-graduate education for patients, which might have diminished the precision of the educational concordance measure and our narrow criteria (within 5 years) for age concordance may have over-specified perceived age concordance.
While some may argue that attempts should have been made to control for race and gender of dyad participants or conduct stratified analyses to evaluate whether SC has the same associations with medical visit communication and patients’ perceptions of care across different racial/ethnic groups, we hold that given the limited sample size, controlling for patient race in our multivariate model would have resulted in over-controlling the model. Similarly, our sample size did not provide adequate statistical power to examine how race, age, education, and gender might each act to modify the effect of the other, on outcomes.
4.2 Conclusion
Despite these limitations, we believe that our findings suggest that consideration of simultaneously held multiple identity characteristics can foster a more transparent and nuanced approach to understanding the varied pathways by which therapeutic relationships are shaped and how they contribute to health care quality.
4.3 Practice Implications
This research is a first step in better understanding the implications of cumulative patient-physician social concordance for medical visit communication and patients’ perceptions of care. It suggests the need to improve our understanding of how patients and physicians process information about differences and similarities and how this influences the quality of patient-provider interactions. A more complete understanding is required in order to develop interventions aimed at physician training as well as patient education and activation training to improve interpersonal interactions. Additional work in this area will likely elucidate structural interventions, such as enhancing diversity among medical students that may be important to address the extent to which patient-physician social discordance systematically affects certain racial/ethnic groups disproportionately.
We suggest that our conceptualization of SC might also contribute to the discourse surrounding cultural health capital (CHC). As articulated by Shim, CHC is “a repertoire of skills, verbal and nonverbal competencies, and interactional styles that can influence health care interactions” (p.2) (2); we contend that SC implicitly recognizes that shared characteristics have the potential to create opportunities for cultural understanding. It also implies that lacking these shared characteristics may have negative health implications that are inequitably distributed among population certain sub-groups. social concordance captures interpersonal and structural aspects of CHC and could be used to operationalize CHC and identify ways to build CHC among subpopulations currently experiencing systematic disadvantage, less positive interpersonal relationships, and disparities in health and health care.
Acknowledgements
This work was supported by research grants from the Commonwealth Fund and the Bayer Institute for Health Care Communication. In addition, the corresponding author, Dr. Johnson Thornton was supported in part by a National Research Service Award from the Agency for Healthcare Research and Quality (1 F31 HS 013265 0) in 2002–2003. Dr. Cooper is supported by a grant from the National Heart, Lung, and Blood Institute (K24HL083113).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimer: The views presented here are those of the authors and not necessarily those of the Commonwealth Fund, its directors, officers, or staff.
Prior Presentations: An earlier version of this work was presented at the European Association for Communication in Health Care (EACH) International Conference on Communication in Health Care, September 16, 2004, Brugges, Belgium.
Contributor Information
Rachel L. Johnson Thornton, Johns Hopkins School of Medicine, Division of General Pediatrics and Adolescent Medicine, 200 N. Wolfe Street, 2nd floor, Baltimore, MD 21287.
Neil R. Powe, University of California San Francisco, San Francisco General Hospital.
Debra Roter, Johns Hopkins Bloomberg School of Public Health, Department of Health, Behavior, and Society and Johns Hopkins School of Medicine, Division of General Internal Medicine.
Lisa A. Cooper, Johns Hopkins School of Medicine, Division of General Internal Medicine & Johns Hopkins Bloomberg School of Public Health, Departments of Epidemiology, Health Policy & Management, & Health, Behavior, and Society.
Reference List
- 1.Ackerson LK, Viswanath K. The social context of interpersonal communication and health. J Health Commun. 2009;14 Suppl 1:5–17. doi: 10.1080/10810730902806836. 5-17. [DOI] [PubMed] [Google Scholar]
- 2.Shim JK. Cultural health capital: A theoretical approach to understanding health care interactions and the dynamics of unequal treatment. J Health Soc Behav. 2010;51(1):1–15. doi: 10.1177/0022146509361185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 4.Kalichman SC, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14(5):267–273. doi: 10.1046/j.1525-1497.1999.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor-patient communication about drugs: the evidence for shared decision making. Soc Sci Med. 2000;50(6):829–840. doi: 10.1016/s0277-9536(99)00376-7. [DOI] [PubMed] [Google Scholar]
- 6.Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med. 1997;45(12):1829–1843. doi: 10.1016/s0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- 7.Hall JA, Horgan TG, Stein TS, Roter DL. Liking in the physician--patient relationship. Patient Educ Couns. 2002;48(1):69–77. doi: 10.1016/s0738-3991(02)00071-x. [DOI] [PubMed] [Google Scholar]
- 8.Bell RA, Kravitz RL, Thom D, Krupat E, Azari R. Unmet expectations for care and the patient-physician relationship. J Gen Intern Med. 2002;17(11):817–824. doi: 10.1046/j.1525-1497.2002.10319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Derose KP, Hays RD, McCaffrey DF, Baker DW. Does physician gender affect satisfaction of men and women visiting the emergency department? J Gen Intern Med. 2001;16(4):218–226. doi: 10.1046/j.1525-1497.2001.016004218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makoul G. Perpetuating passivity: reliance and reciprocal determinism in physician-patient interaction. J Health Commun. 1998;3(3):233–259. doi: 10.1080/108107398127355. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Rathore SS, Radford MJ, Wang Y, Krumholz HM. Racial differences in the use of cardiac catheterization after acute myocardial infarction. N Engl J Med. 2001;344(19):1443–1449. doi: 10.1056/NEJM200105103441906. [DOI] [PubMed] [Google Scholar]
- 12.Todd KH, Deaton C, D'Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35(1):11–16. doi: 10.1016/s0196-0644(00)70099-0. [DOI] [PubMed] [Google Scholar]
- 13.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 14.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med. 2000;50(6):813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 15.van Wieringen JC, Harmsen JA, Bruijnzeels MA. Intercultural communication in general practice. Eur J Public Health. 2002;12(1):63–68. doi: 10.1093/eurpub/12.1.63. [DOI] [PubMed] [Google Scholar]
- 16.Sinclair L, Kunda Z. Reactions to a black professional: motivated inhibition and activation of conflicting stereotypes. J Pers Soc Psychol. 1999;77(5):885–904. doi: 10.1037//0022-3514.77.5.885. [DOI] [PubMed] [Google Scholar]
- 17.Gerbert B, Berg-Smith S, Mancuso M, Caspers N, Danley D, Herzig K, et al. Video study of physician selection: preferences in the face of diversity. J Fam Pract. 2003;52(7):552–559. [PubMed] [Google Scholar]
- 18.Cooper LA, Powe NR. Disparities in Patient Experiences, Health Care Processes, and Outcomes: The Role of Patient-Provider Racial, Ethnic, and Language Concordance. 753. 7-1-2004. Commonwealth Fund.
- 19.Cooper LA, Roter DL. Patient-Provider Communication: The Effect of Race and Ethnicity on Process and Outcomes of Healthcare. In: Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: The National Academies Press; 2002. pp. 552–593. [Google Scholar]
- 20.Roter DL, Hall JA. Doctors talking with patient / patients talking with doctors: improving communication in medical visits. 2nd ed. Westport, CT: Praeger; 2006. [Google Scholar]
- 21.Ratanawongsa N, Haywood C, Jr, Bediako SM, Lattimer L, Lanzkron S, Hill PM, et al. Health care provider attitudes toward patients with acute vaso-occlusive crisis due to sickle cell disease: development of a scale. Patient Educ Couns. 2009;76(2):272–278. doi: 10.1016/j.pec.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wiggers JH, Sanson-Fisher R. Duration of general practice consultations: association with patient occupational and educational status. Soc Sci Med. 1997;44(7):925–934. doi: 10.1016/s0277-9536(96)00175-x. [DOI] [PubMed] [Google Scholar]
- 24.Roter D, Lipkin M, Jr, Korsgaard A. Sex differences in patients' and physicians' communication during primary care medical visits. Med Care. 1991;29(11):1083–1093. doi: 10.1097/00005650-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Hall JA, Irish JT, Roter DL, Ehrlich CM, Miller LH. Gender in medical encounters: an analysis of physician and patient communication in a primary care setting. Health Psychol. 1994;13(5):384–392. doi: 10.1037//0278-6133.13.5.384. [DOI] [PubMed] [Google Scholar]
- 26.Roter DL, Stewart M, Putnam SM, Lipkin M, Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA. 1997;277(4):350–356. [PubMed] [Google Scholar]
- 27.Malat J. Social distance and patients' rating of healthcare providers. J Health Soc Behav. 2001;42(4):360–372. [PubMed] [Google Scholar]
- 28.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 29.Kuder JM, Vilmain JA, Demlo LK. Exploring physician responses to patients' extramedical characteristics. The decision to hospitalize. Med Care. 1987;25(9):882–893. [PubMed] [Google Scholar]
- 30.Aruguete MS, Roberts CA. Participants' ratings of male physicians who vary in race and communication style. Psychol Rep. 2002;91(3 Pt 1):793–806. doi: 10.2466/pr0.2002.91.3.793. [DOI] [PubMed] [Google Scholar]
- 31.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 32.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 33.LaVeist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43(3):296–306. [PubMed] [Google Scholar]
- 34.Ferguson WJ, Candib LM. Culture, language, and the doctor-patient relationship. Fam Med. 2002;34(5):353–361. [PubMed] [Google Scholar]
- 35.Rohrbaugh M, Rogers JC. What did the doctor do? When physicians and patients disagree. Arch Fam Med. 1994;3(2):125–128. doi: 10.1001/archfami.3.2.125. [DOI] [PubMed] [Google Scholar]
- 36.Krupat E, Bell RA, Kravitz RL, Thom D, Azari R. When physicians and patients think alike: patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001;50(12):1057–1062. [PubMed] [Google Scholar]
- 37.Street RL, Jr, Krupat E, Bell RA, Kravitz RL, Haidet P. Beliefs about control in the physician-patient relationship: effect on communication in medical encounters. J Gen Intern Med. 2003;18(8):609–616. doi: 10.1046/j.1525-1497.2003.20749.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haidet P, O'Malley K, Aniol J, Gladney A, Sarf B, Street R, et al. A tool to measure patients' and physicians' explanatory models of illness. J.Gen.Intern.Med. 2002;17(196) Suppl 1 [Google Scholar]
- 39.Lukoschek P, Fazzari M, Marantz P. Patient and physician factors predict patients' comprehension of health information. Patient Educ Couns. 2003;50(2):201–210. doi: 10.1016/s0738-3991(02)00128-3. [DOI] [PubMed] [Google Scholar]
- 40.Barry CA, Stevenson FA, Britten N, Barber N, Bradley CP. Giving voice to the lifeworld. More humane, more effective medical care? A qualitative study of doctor-patient communication in general practice. Soc Sci Med. 2001;53(4):487–505. doi: 10.1016/s0277-9536(00)00351-8. [DOI] [PubMed] [Google Scholar]
- 41.Street RL, Jr, O'Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6(3):198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McPherson M, Smith-Lovin L, Cook JM. Birds of a Feather: Homophily in Social Networks. Annu Rev Sociol. 2001;27:415–444. [Google Scholar]
- 43.Kenny DA, Veldhuijzen W, van der Weijden T, LeBlanc A, Lockyer J, Legare F, et al. Interpresonal perception in the context of doctor-patient relationships: A dyadic analysis of doctor-patient communication. Soc Sci Med. 2009;70:763–768. doi: 10.1016/j.socscimed.2009.10.065. [DOI] [PubMed] [Google Scholar]
- 44.Roter DL, Larson S. The relationship between residents' and attending physicians' communication during primary care visits: an illustrative use of the Roter Interaction Analysis System. Health Commun. 2001;13(1):33–48. doi: 10.1207/S15327027HC1301_04. [DOI] [PubMed] [Google Scholar]
- 45.Mead N, Bower P. Measuring patient-centredness: a comparison of three observation-based instruments. Patient Educ Couns. 2000;39(1):71–80. doi: 10.1016/s0738-3991(99)00092-0. [DOI] [PubMed] [Google Scholar]
- 46.Wissow LS, Roter D, Bauman LJ, Crain E, Kercsmar C, Weiss K, et al. Med Care. 10. Vol. 36. Bethesda, MD: The National Cooperative Inner-City Asthma Study, National Institute of Allergy and Infectious Diseases, NIH; 1998. Patient-provider communication during the emergency department care of children with asthma; pp. 1439–1450. [DOI] [PubMed] [Google Scholar]
- 47.Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323(7318):908–911. doi: 10.1136/bmj.323.7318.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 49.Liang KY, Zeger SL. Regression analysis for correlated data. Annu Rev Public Health. 1993;14:43–68. doi: 10.1146/annurev.pu.14.050193.000355. [DOI] [PubMed] [Google Scholar]
- 50.Diggle PJ, Heagerty P, Liang K, Zeger SL. Analysis of Longitudinal Data. 2nd ed. Oxford: Oxford University Press; 2002. [Google Scholar]
- 51.Epstein S. Integration of the cognitive and psychodynamic unconscious. American Psychologist. 1994;49:709–724. doi: 10.1037//0003-066x.49.8.709. [DOI] [PubMed] [Google Scholar]
- 52.Roter D. Three blind men and an elephant: reflections on meeting the challenges of patient diversity in primary care practice. Fam Med. 2002;34(5):390–393. [PubMed] [Google Scholar]