Abstract
Purpose
Several studies have reported that men with lower urinary tract symptoms (LUTS) are more likely to experience erectile dysfunction (ED). All but one of these studies was cross-sectional, limiting inferences about whether LUTS precipitate ED.
Materials and Methods
The association between LUTS and incident ED was examined prospectively in the Health Professionals Follow-up Study. LUTS were assessed biennially by the American Urological Association Symptom Index, which captures symptoms of frequency, urgency and force of urinary stream. Severe LUTS was defined as a symptom score of ≥ 20 points and no LUTS was defined as a score of ≤ 7 points, both among men not treated for LUTS. In 2000, the men were asked to rate their erectile function for several time periods. ED was defined as “poor” or “very poor” function or use of ED medications and no ED was defined as “very good” or “good” function and no use of ED medications. We estimated risk ratios using Poisson regression adjusting for age and other potentially confounding factors.
Results
We observed 3,953 incident ED cases among 17,086 men. Men with severe LUTS in 1994 or earlier had a statistically significant 40% higher risk of ED subsequently than men without LUTS. The risk of ED increased with increasing LUTS severity (p trend < 0.0001). The positive association between LUTS and ED was stronger among younger than older men (p interaction = 0.03).
Conclusions
This study provides evidence that men with LUTS are more likely to develop ED subsequently.
Keywords: erectile dysfunction, prostatic hyperplasia, urination disorders, prospective studies
INTRODUCTION
Lower urinary tract symptoms (LUTS), often secondary to benign prostatic hyperplasia (BPH), and erectile dysfunction (ED) are highly prevalent in older men. The prevalence of LUTS and ED in older men may be as high as 31% 2 and 52% 1, respectively. Both ED and LUTS are associated with decreased quality of life. 3,4
Many studies have found a positive association between LUTS and ED 2,5–16; all but one 16 were cross-sectional. Because the cross-sectional design cannot address the temporal relationship between LUTS and ED it remains unclear whether this association is causal. The one prospective study 16 supports a positive association between LUTS and incidence of ED, although the sample size was relatively small (n=1,683).
To further address whether LUTS is prospectively associated with incident ED, we conducted an investigation in the Health Professionals Follow-up Study (HPFS), a large study of US men.
METHODS
Study Population
The HPFS is a prospective cohort of 51,529 US male health professionals aged 40–75 years in 1986. Follow-up questionnaires are mailed every 2 years to update exposures and outcomes.
Men were excluded if they died before 2000 (13.7%), did not return the 2000 questionnaire on which ED was assessed (9.6%), or filled out only the short version, which did not ask about ED (9.2%). Men were excluded if they had cancer before 1986 (4.1%), had prostate, bladder, or testicular cancer before 2000 (4.5%), or responded in 2000 but did not provide ED information (4.5%).
Exposure Assessment (LUTS)
LUTS was assessed in 1992, 1994, and 1998. Surgery history, including transurethral resection of the prostate (TURP), was collected on all questionnaires. Use of medications to treat BPH was collected in 1998. Men were asked to indicate frequency (0,10, 25, 50, 75, or almost 100% of the time) of the following: 1) sensation of incomplete bladder emptying (incomplete emptying), 2) having to urinate again after less than 2 hours (frequency), 3) stopping and starting several times during urination (intermittency), 4) difficulty postponing urination (urgency), 5) weak urinary stream (weak stream), and 6) having to push or strain to begin urination (hesitancy). 17 Scores ranging from 0 to 5 were assigned, with a score of 0 corresponding to “0% of the time” and a score of 5 corresponding to “almost 100% of the time”. Men were also asked how many times they typically had to get up at night to urinate (0, 1, 2, 3, 4, 5, or 6 or more times) during the past month (nocturia). A score ranging from 0 to 5 was assigned with “5 times” or “6 or more times” corresponding to a score of 5. These scores were summed to create a score ranging from 0 to 35, which we categorized into 4 groups: no or low (0–7), low-moderate (8–14), high-moderate (15–19), and severe (20–35) symptoms.
Outcome Assessment (ED)
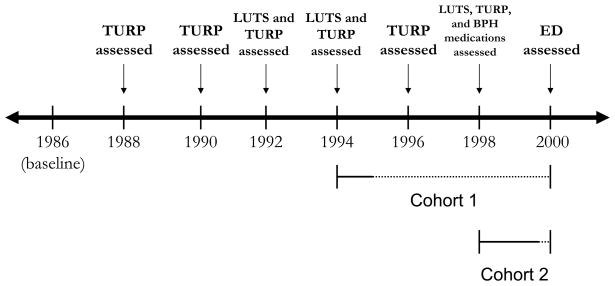
In 2000, men were asked, “Please rate your ability (without treatment) to have and maintain an erection good enough for intercourse for the following time periods: Before 1986, 1986–1989, 1990–1994, 1995 or later, in the last 3 months”. Men could rate their ability as “very good”, “good”, “fair”, “poor”, or “very poor”. Two cohorts were constructed: Cohort 1) Men with “very good” or “good” erectile function in every period prior to 1995, and Cohort 2) Men with “very good” or “good” erectile function in every period prior to the past three months (Figure 1). For the first cohort, incident ED was defined as “poor” or “very poor” erectile function in either “1995 or later” or “in the last 3 months” or treatment for ED “in the last 3 months” (irrespective of reported erectile function), and no ED was defined as “very good” or “good” erectile function and no treatment for ED “in the last 3 months”. For the second cohort, incident ED was defined as “poor” or “very poor” erectile function or treatment for ED (irrespective of erectile function) “in the last 3 months” and no ED was defined as “very good” or “good” erectile function and no treatment for ED “in the last 3 months”. To improve the specificity of the outcome definitions, men who reported “fair” function in “1995 or later” and “ in the last 3 months” (Cohort 1) or “in the last 3 months” (Cohort 2) were excluded from the analysis.
Figure 1.
Lower Urinary Tract Symptoms (LUTS) and Incident Erectile Dysfunction (ED) Assessment Timeline, Health Professionals Follow-up Study
..........Incident ED was assessed for this time interval.
__________Time after LUTS was assessed, but before incident ED was assessed.
Cohort 1: Analysis of incident ED in 1995 or later. Men reported on LUTS in 1992 and 1994 and TURP in 1994 or earlier. In 2000, men reported on ED for the time intervals “1995 or later” or “in the past 3 months”.
Cohort 2: Analysis of incident ED in 2000. Men who reported on LUTS in 1992, 1994, and 1998, TURP in 1998 and earlier, and use of medications to treat BPH in 1998. In 2000, men reported on ED for the time interval “in the past 3 months”.
Statistical Analysis
We estimated the risk ratio (RR) of ED and 95% confidence intervals (CI) using Poisson regression in SAS v 9.1 (SAS Institute, Cary, NC). Models included indicator variables for LUTS severity groups along with terms for TURP and BPH medications use. For cohort 1, LUTS severity was defined based on the 1992 and 1994 questionnaires and TURP was defined based on surgery in 1994 or earlier (Figure 1). For cohort 2, LUTS was defined based on the 1992, 1994, and 1998 questionnaires, medications to treat BPH was defined based on the 1998 questionnaire, and TURP was defined based on surgery in 1998 and earlier (Figure 1). Multivariable models were adjusted for: age, body mass index (BMI), lifetime cumulative cigarette smoking, physical activity, race, fruit and vegetable intake, alcohol intake, diabetes, hypertension, and cardiovascular disease. Trend tests were modeled using the median score for each symptom category. Sensitivity analyses were conducted restricting to healthy men (i.e., excluded 1,963 who ever had diabetes, cancer, myocardial infarction, stroke, coronary artery bypass, angioplasty, or angina). We conducted analyses stratified by age (<65, ≥ 65 years); statistical interaction was assessed using the likelihood ratio test.
RESULTS
In 1992 (the first time in which we assessed LUTS), men with higher AUA symptom scores were older. After age-standardization, men with higher scores were less physically active, were more likely to smoke, and were more likely to have diabetes, hypertension, and cardiovascular disease (Table 1). Similarly, men with ED that developed in 1995 or later were older, had higher BMI, were less physically active, and ate fewer fruits and vegetables than men without ED. Further, men with ED were more likely to smoke and have diabetes, hypertension, and cardiovascular disease.
Table 1.
Age-Adjusted Baseline* Characteristics of Men by Lower Urinary Tract Symptom Severity (LUTS) or Surgery for BPH†, Health Professionals Follow-up Study
| AUA Symptom Index Score | |||||
|---|---|---|---|---|---|
| No to Low LUTS 0 – 7 N = 20,177 |
Low- Moderate LUTS 8 – 14 N = 4,244 |
High- Moderate LUTS 15 – 19 N = 913 |
Severe LUTS 20 – 35 N = 478 |
Surgery for BPH N = 1,070 |
|
| Age (years) | |||||
| mean | 56.1 | 60.3 | 62.1 | 62.0 | 65.8 |
|
| |||||
| Race (n,%) | |||||
| Southern European | 4,675 (22.9%) | 1,027 (25.1%) | 246 (27.4%) | 148 (33.1%) | 257 (29.1%) |
| Scandinavian | 2,202 (10.8 %) | 405 (9.7%) | 90 (9.9%) | 34 (7.2%) | 103 (10.1%) |
| Other Caucasian | 11,573 (57.7%) | 2,461 (57.2%) | 506 (54.3%) | 258 (52.8%) | 626 (53.5%) |
| African-American | 131 (0.7%) | 30 (0.6%) | 5 (0.6%) | 2 (0.2%) | 2 (0.2%) |
| Asian | 327 (1.6%) | 74 (1.8%) | 11 (1.5%) | 4 (0.8%) | 4 (0.4%) |
| Other/Missing | 1,269 (6.3%) | 247 (5.6%) | 55 (6.3%) | 32 (5.9%) | 78 (6.9%) |
|
| |||||
| BMI (kg/m2) | |||||
| mean | 25.5 | 25.6 | 25.8 | 25.7 | 25.5 |
|
| |||||
| Smoking (n,%) | |||||
| Never | 9,805 (47.8%) | 1,858 (45.5%) | 399 (45.3%) | 179 (41.1%) | 475 (48.8%) |
| Current | 1,379 (6.7%) | 236 (5.7%) | 38 (5.3%) | 23 (4.8%) | 47 (5.8%) |
| Former | 8.226 (41.7%) | 2,003 (45.4%) | 438 (45.2%) | 258 (50.4%) | 500 (41.1%) |
| Missing | 767 (3.8%) | 147 (3.4%) | 38 (4.2%) | 18 (3.6%) | 48 (4.3%) |
|
| |||||
| Physical Activity (MET-hrs/wk) | |||||
| Mean | 37.6 | 36.3 | 33.5 | 33.3 | 38.7 |
|
| |||||
| Fruits and Vegetables (servings/day) | |||||
| mean | 6.1 | 6.3 | 6.2 | 6.4 | 6.6 |
|
| |||||
| Alcohol Intake (g/day) (n,%) | |||||
| 0 | 4,667 (23.2%) | 1,033 (24.7%) | 214 (23.2%) | 119 (26.8%) | 310 (30.3%) |
| <5 | 5,282 (26.0%) | 1,167 (28.1%) | 264 (29.3%) | 136 (28.3%) | 285 (28.5%) |
| 5 – <15 | 5,476 (27.1%) | 1,070 (25.1%) | 224 (24.4%) | 116 (24.3%) | 291 (24.7%) |
| 15 – <30 | 2,565 (12.8%) | 534 (12.5%) | 106 (12.1%) | 61 (11.2%) | 92 (7.4%) |
| 30 – <50 | 1,587 (8.0%) | 318 (6.9%) | 68 (6.6%) | 26 (5.0%) | 70 (4.7%) |
| ≥ 50 | 445 (2.3%) | 92 (2.0%) | 29 (3.2%) | 16 (3.5%) | 7 (1.9%) |
| Missing | 155 (0.8%) | 30 (0.7%) | 8 (1.1%) | 4 (1.0%) | 15 (2.6%) |
|
| |||||
| Diabetes (n,%) | |||||
| Ever | 576 (3.1%) | 204 (4.2%) | 42 (4.1%) | 26 (4.7%) | 59 (3.3%) |
|
| |||||
| Hypertension (n,%) | |||||
| Ever | 4,871 (25.2%) | 1,303 (28.4%) | 310 (30.4%) | 157 (31.4%) | 399 (32.1%) |
|
| |||||
| Cardiovascular Disease (n,%) | |||||
| Ever | 1,608 (8.8%) | 536 (10.4%) | 145 (12.4%) | 81 (12.9%) | 197 (13.8%) |
LUTS were first assessed on the 1992 questionnaire. All characteristics are from the 1992 questionnaire, except: fruits and vegetables and alcohol are from the 1990 questionnaire; and diabetes, hypertension, and cardiovascular disease are cumulative and are derived from all questionnaires from 1992 to 2000.
LUTS and surgery for BPH reported in 1994 or earlier
In the analysis of incident ED that developed in 1995 or later (Figure 1, cohort 1), we included 3,953 cases among 17,086 men who reported good or very good erectile function before 1995. Men with severe LUTS in 1994 or earlier had a statistically significant 40% higher risk of ED than men without LUTS (Table 2). Risk of ED increased with increasing LUTS severity (p trend < 0.0001). In the analysis of incident ED that developed in the last three months prior to the return of the 2000 questionnaire (Figure 1, cohort 2), we included 953 cases among 14,426 men. Men with severe LUTS in 1998 or earlier had a 59% higher risk of ED than men without LUTS (Table 2). Again, risk of incident ED increased with increasing LUTS severity (p trend = 0.0002). None of the covariates was an important confounder of the LUTS-ED association. When 0 LUTS was the reference instead of 0–7, the dose-response relation was steeper for both ED in 1995 or later (1–7: RR=1.47 95% CI 1.29–1.67, 8–14: RR=1.70 95% CI 1.48–1.96, 15–19: RR=1.95 95% CI 1.65–2.31, 20–35: RR= 2.00 95% CI 1.64–2.45; p trend<0.0001) and in the last three months (data not shown). The association was also increasing across quintiles of the score for ED in 1995 or later (Q2: RR=1.16 (95% CI 1.07–1.26) Q3: RR=1.40 (95% CI 1.28–1.53), Q4: RR=1.40 (95% CI 1.28–1.53), Q5: RR=1.51 (95% CI 1.39–1.64) p trend<0.0001) and in the last three months (data not shown). The association between LUTS and incident ED, both in 1995 or later and in the last three months, was similar in magnitude when the men were categorized by their most recent AUA score prior to ED assessment and when duration of BPH was used (data not shown).
Table 2.
Association of Lower Urinary Tract Symptoms with Erectile Dysfunction Health Professionals Follow-up Study
|
AUA Symptom Index Score§ |
Surgery for BPH | Medications for BPH | ||||
|---|---|---|---|---|---|---|
| No to Low LUTS 0 – 7 | Low-Moderate LUTS 8 – 14 | High-Moderate LUTS 15 – 19 | Severe LUTS 20 – 35 | |||
| Incident ED in 1995 or later† | ||||||
| #cases | 2,739 | 760 | 171 | 94 | 189 | - |
| RR (95%CI)* | 1.0 (ref) | 1.23 (1.15–1.31) | 1.37 (1.22–1.54) | 1.50 (1.28–1.75) | 1.16 (1.04–1.30) | - |
| RR (95%CI)** | 1.0 (ref) | 1.20 (1.12–1.27) | 1.37 (1.22–1.54) | 1.40 (1.20–1.64) | 1.17 (1.05–1.30) | - |
| p trend <0.0001 | ||||||
| Incident ED in the last three months‡ | ||||||
| # cases | 573 | 182 | 43 | 23 | 73 | 59 |
| RR (95%CI)* | 1.0 (ref) | 1.26 (1.08–1.47) | 1.52 (1.14–2.03) | 1.72 (1.17–2.54) | 1.44 (1.14–1.81) | 1.34 (1.05–1.72) |
| RR (95%CI)** | 1.0 (ref) | 1.23 (1.06–1.44) | 1.52 (1.14–2.03) | 1.59 (1.10–2.32) | 1.39 (1.11–1.75) | 1.25 (0.97–1.60) |
| p trend = 0.0002 | ||||||
Adjusting for age in years (continuous)
Adjusting for age in years (continuous), body mass index (BMI kg/m2, continuous), lifetime cumulative cigarette smoking (never, current <15 pack-years, current ≥ 15 pack-years, current unknown pack-years, former <5 pack-years, former 5–9 pack-years, former ≥ 10 pack-years, former unknown pack-years, missing smoking status), physical activity (none/missing, quartiles of MET-hrs/week), race (African-American, Asian, Southern European, Scandinavian, other Caucasian, other), fruit and vegetable intake (quintiles), alcohol intake (none, <5g/day, 5-<15 g/day, 15-<30 g/day, 30-<50 g/day, ≥ 50 g/day), diabetes (ever/never), hypertension (ever/never), and cardiovascular disease (ever/never)
LUTS or surgery for BPH reported in 1994 or earlier, and incident ED in 1995 or later (cohort 1)
LUTS or surgery for BPH, or medications for BPH reported in 1998 or earlier, and incident ED reported in the three months prior to the return of the 2000 questionnaire (cohort 2)
For the analysis of incident ED in 1995 or later, men categorized according to their maximum reported AUA Symptom Index score on 1992 or 1994 questionnaire. For the analysis of incident ED in the last three months, men categorized according to their maximum reported AUA Symptom Index score on 1992, 1994, or 1998 questionnaire.
No differences in risk of ED were observed for obstructive (incomplete emptying, hesitancy, weak stream, and intermittency) versus irritative (frequency, urgency, and nocturia) symptoms (data not shown). Men who had undergone TURP or took medications to treat BPH had a higher risk of ED compared with men with no or low LUTS (Table 2). The association between LUTS and ED was stronger in younger than older men (Table 3).
Table 3.
Association of Lower Urinary Tract Symptoms Severity with Erectile Dysfunction by Age, Health Professionals Follow-up Study
| Age <65 | Age >65 | |||||
|---|---|---|---|---|---|---|
| # Cases | RR (95%CI)* | RR (95%CI)** | # Cases | RR (95%CI)* | RR (95%CI)** | |
| Incident ED 1995 or later† | ||||||
| AUA Symptom Score§ | ||||||
| No to Low LUTS: 0–7 | 1,145 | 1.0 (ref) | 1.0 (ref) | 1,594 | 1.0 (ref) | 1.0 (ref) |
| Low-Moderate LUTS: 8–14 | 187 | 1.31 (1.14–1.50) | 1.28 (1.11–1.46) | 573 | 1.19 (1.11–1.27) | 1.16 (1.08–1.24) |
| High-Moderate LUTS: 15–19 | 50 | 1.85 (1.46–2.34) | 1.75 (1.39–2.22) | 121 | 1.22 (1.07–1.39) | 1.24 (1.09–1.42) |
| Severe LUTS: 20–35 | 31 | 2.39 (1.80–3.18) | 2.25 (1.68–3.00) | 63 | 1.25 (1.05–1.49) | 1.18 (0.99–1.41) |
| p trend | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 | ||
| Surgery for BPH | 17 | 1.30 (0.85–1.99) | 1.33 (0.87–2.05) | 172 | 1.13 (1.01–1.27) | 1.13 (1.01–1.26) |
| p for interaction = 0.03 | ||||||
|
| ||||||
| Incident ED in the last three months‡ | ||||||
| AUA Symptom Score§ | ||||||
| No to Low LUTS: 0–7 | 262 | 1.0 (ref) | 1.0 (ref) | 311 | 1.0 (ref) | 1.0 (ref) |
| Low-Moderate LUTS: 8–14 | 49 | 1.08 (0.80–1.46) | 1.07 (0.79–1.44) | 133 | 1.33 (1.11–1.60) | 1.31 (1.09–1.57) |
| High-Moderate LUTS: 15–19 | 18 | 2.12 (1.34–3.35) | 2.07 (1.31–3.28) | 25 | 1.26 (0.88–1.81) | 1.27 (0.89–1.83) |
| Severe LUTS: 20–35 | 8 | 2.22 (1.14–4.36) | 2.24 (1.13–4.41) | 15 | 1.53 (0.96–2.44) | 1.37 (0.89–2.13) |
| p trend | 0.004 | 0.004 | 0.0002 | 0.0006 | ||
| Surgery for BPH | 15 | 2.33 (1.42–3.83) | 2.22 (1.37–3.59) | 58 | 1.30 (1.01–1.67) | 1.25 (0.98–1.61) |
| Medications for BPH | 13 | 1.35 (0.78–2.34) | 1.22 (0.71–2.10) | 46 | 1.32 (1.00–1.75) | 1.24 (0.94–1.65) |
| p for interaction = 0.19 | ||||||
Adjusting for age in years (continuous)
Adjusting for age in years (continuous), body mass index (BMI kg/m2, continuous), lifetime cumulative cigarette smoking (never, current <15 pack-years, current ≥ 15 pack-years, current unknown pack-years, former <5 pack-years, former 5–9 pack-years, former ≥ 10 pack-years, former unknown pack-years, missing smoking status), physical activity (none/missing, quartiles of MET-hrs/week), race (African-American, Asian, Southern European, Scandinavian, other Caucasian, other), fruit and vegetable intake (quintiles), alcohol intake (none, <5g/day, 5-<15 g/day, 15-<30 g/day, 30-<50 g/day, ≥ 50 g/day), diabetes (ever/never), hypertension (ever/never), and cardiovascular disease (ever/never)
LUTS or surgery for BPH reported in 1994 or earlier, and incident ED newly reported 1995 or later (cohort 1)
LUTS or surgery for BPH, or medications for BPH reported in 1998 or earlier, and incident ED in the three months prior to the return of the 2000 questionnaire (cohort 2)
For the analysis of incident ED in 1995 or later, men categorized according to their maximum reported AUA Symptom Index score on 1992 or 1994 questionnaire. For the analysis of incident ED in the last three months, men categorized according to their maximum reported AUA Symptom Index score on 1992, 1994, or 1998 questionnaire.
The results were unchanged after restricting to healthy men (data not shown). After further restricting to men without hypertension the results were unchanged. When we restricted the analysis to healthy men who were normal weight (BMI <25), active (≥17.5 MET-hr/wk), ate the recommended 5 servings of fruits and vegetables daily, and never smoked, the results were similar (data not shown).
DISCUSSION
Results from this prospective study provide support for a positive association between LUTS and incident ED. The increasing risk of ED with increasing AUA symptom score was observed with both standard categories and quintiles of the score. The positive association was stronger when men without any of the six symptoms were the referent. We also found that the association between LUTS and ED may be stronger in younger men.
Because most studies to date have been cross-sectional, we also performed a cross-sectional analysis (versus 0–7, 8–14: RR=1.28, 15–19: RR=1.36, 20–35: RR=1.44) and these findings were comparable to our prospective results. The inferences from our cross-sectional results and those previously published are the same. Cross-sectional studies have reported ORs for the LUTS-ED association ranging from 1.39 to 9.9. 2,5,8,9,12,13,15 Only one study 18 reported no association between LUTS and ED, but it had methodologic limitations.
Our results are similar to those from the one published prospective study (comparing LUTS ≥12 to 0 OR=3.1, 95%CI 1.5–6.4). 16 However, our substantially larger study allowed us to categorize LUTS into finer categories and conduct stratified analyses, as well as multiple sensitivity analyses.
Although our results are consistent with the existing literature, it is difficult to compare the magnitude of our results with those from previous studies. First, LUTS was not consistently categorized among studies. In the other prospective study, men with a score ≥ 12 were compared with men with a score of 0 16; other studies selected different cutpoints. Second, the previous studies reported odds ratios as estimates of the risk ratio, whereas we report risk ratios. Because LUTS and ED are common among older men, for positive associations, the odds ratio will overestimate the risk ratio. Therefore, our directly calculated risk ratios are somewhat smaller than previous estimates for this association.
Several possible noncausal and causal explanations for the apparent association between LUTS and ED exist.
ED and LUTS are both strongly positively associated with age, which could lead to their spurious association if age is not fully taken into account 19; most of the prior studies took into account age to some extent,2,6–9,11–14,16 although one did not. 10
LUTS and ED share many similar risk factors, which could cause an apparent statistical association even if a biological association does not exist. Although some of the prior studies conducted multivariable adjustment 2,5,6,9,13,16, many did not. 7,8,10–12,14,15
Treatment for LUTS may influence ED. 19 5α-Reductase inhibitors have been shown to decrease sexual function, whereas some evidence suggests that α1-adrenergic receptor blockers may improve sexual function. 19 In the past, transurethral resection of the prostate (TURP) was a common surgical treatment for LUTS and studies have reported differing information as to how surgery influences sexual function. 19
Several pathophysiologic pathways may underlie both conditions. Increased α1-adrenergic activity and changes in α1-adrenergic receptor subtypes expressed increase smooth muscle tone; these changes may be common causes of both LUTS and ED. 19 Decreases in nitric oxide bioavailability in older men may cause endothelial dysfunction, which may lead to both LUTS and ED. 19
BPH nodules, which may compress the urethra and produce LUTS, may be an independent risk factor for ED. This hypothesis is supported by studies suggesting that removal of BPH nodules during TURP improves erectile function. 20
Decreased quality of life associated with LUTS may have a negative psychological influence that may manifest as decreased sexual function. 19
Our results suggest that the association between LUTS and ED is not due to residual confounding by age or solely the effect of treatment: we controlled for age as a continuous variable and created separate categories of exposure for men who had received treatment for LUTS and still observed in untreated men an association between LUTS and ED. We observed an increased risk of ED among men who had undergone surgery or were taking medication for BPH compared with men with no or low LUTS, although their ED risk was lower than for men with severe LUTS. It is not clear whether this finding is due to BPH treatment or reflects that men who received treatment had worse LUTS. Alternatively, these findings may suggest that treatment for severe LUTS moderates ED risk in men with severe LUTS.
Residual confounding by risk factors for LUTS and ED, particularly co-morbidities, is unlikely because the associations were unchanged when restricted analyses were conducted. Nevertheless, it is possible that our results could be partly explained by confounding by unrecognized, shared risk factors for LUTS and ED. Our results cannot distinguish among the other proposed explanations for the association between LUTS and ED.
The association between LUTS and ED was more pronounced among younger than older men, although the absolute increase in risk was comparable (~15% increase comparing severe to no/low symptoms). In younger men, a greater proportion of ED may be caused by the same pathophysiologic mechanisms that cause LUTS in older men, but in older men a greater proportion of ED may be caused by other factors, such as co-morbidities. Alternatively, the difference by age may reflect a difference in the accuracy of reporting ED by age because of differential expectations by age about the quality of erectile function.
The prospective design and large sample size are strengths of our study. We assessed both LUTS and ED by mailed questionnaires, which may have minimized embarrassment and increased the accuracy of report. Further, because LUTS status was collected prior to occurrence and assessment of ED, the extent of any inaccuracy in the report of LUTS is unlikely to be different by ED status, and any such bias would tend to attenuate the association. We asked the men in 2000 when in the past they first experienced ED, and thus, there is the potential for inaccurate recollection of ED. However, the association between LUTS and incident ED was comparable for both remotely recollected ED (back to 1995) and for very recently recollected ED (in the past 3 months), suggesting that inaccurate remote recall is not greatly influencing the observed association.
CONCLUSIONS
This study provides evidence that men who have LUTS are more likely to develop ED subsequently. Work is needed to determine whether targeting the pathologies underlying LUTS through dietary and lifestyle modifications or therapies would prevent ED.
Acknowledgments
Grant Support:
The National Institutes of Health provided funding for HPFS general follow-up (grants # CA55075, HL35464). Pfizer, Inc., provided funding for the examination of causes of sexual dysfunction. Ms. Mondul was supported by the National Institutes of Health National Research Service Award T32 CA009314. The sponsor, Pfizer Inc, represented by Dr. Glasser, was involved in the review of the manuscript. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Abbreviations Key
- LUTS
lower urinary tract symptoms
- BPH
benign prostatic hyperplasia
- ED
erectile dysfunction
- HPFS
Health Professionals Follow-up Study
- TURP
transurethral resection of the prostate RR, relative risk
- CI
confidence interval
- BMI
body mass index
- AUA
American Urological Association
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bacon CG, Mittleman MA, Kawachi I, Giovannucci E, Glasser DB, Rimm EB. Sexual function in men older than 50 years of age: results from the health professionals follow-up study. Ann Intern Med. 2003;139:161. doi: 10.7326/0003-4819-139-3-200308050-00005. [DOI] [PubMed] [Google Scholar]
- 2.Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) Eur Urol. 2003;44:637. doi: 10.1016/j.eururo.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Roberts RO, Jacobsen SJ, Rhodes T, Girman CJ, Guess HA, Lieber MM. Natural history of prostatism: impaired health states in men with lower urinary tract symptoms. J Urol. 1997;157:1711. doi: 10.1016/s0022-5347(01)64842-0. [DOI] [PubMed] [Google Scholar]
- 4.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 5.Ponholzer A, Temml C, Obermayr R, Madersbacher S. Association between lower urinary tract symptoms and erectile dysfunction. Urology. 2004;64:772. doi: 10.1016/j.urology.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Elliott SP, Gulati M, Pasta DJ, Spitalny GM, Kane CJ, Yee R, et al. Obstructive lower urinary tract symptoms correlate with erectile dysfunction. Urology. 2004;63:1148. doi: 10.1016/j.urology.2004.01.039. [DOI] [PubMed] [Google Scholar]
- 7.Hoesl CE, Woll EM, Burkart M, Altwein JE. Erectile dysfunction (ED) is prevalent, bothersome and underdiagnosed in patients consulting urologists for benign prostatic syndrome (BPS) Eur Urol. 2005;47:511. doi: 10.1016/j.eururo.2004.10.029. [DOI] [PubMed] [Google Scholar]
- 8.Terai A, Ichioka K, Matsui Y, Yoshimura K. Association of lower urinary tract symptoms with erectile dysfunction in Japanese men. Urology. 2004;64:132. doi: 10.1016/j.urology.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 9.Braun MH, Sommer F, Haupt G, Mathers MJ, Reifenrath B, Engelmann UH. Lower urinary tract symptoms and erectile dysfunction: co-morbidity or typical “Aging Male” symptoms? Results of the “Cologne Male Survey”. Eur Urol. 2003;44:588. doi: 10.1016/s0302-2838(03)00358-0. [DOI] [PubMed] [Google Scholar]
- 10.el-Sakka AI. Lower urinary tract symptoms in patients with erectile dysfunction: analysis of risk factors. J Sex Med. 2006;3:144. doi: 10.1111/j.1743-6109.2005.00132.x. [DOI] [PubMed] [Google Scholar]
- 11.Chung WS, Nehra A, Jacobson DJ, Roberts RO, Rhodes T, Girman CJ, et al. Lower urinary tract symptoms and sexual dysfunction in community-dwelling men. Mayo Clin Proc. 2004;79:745. doi: 10.4065/79.6.745. [DOI] [PubMed] [Google Scholar]
- 12.Braun M, Wassmer G, Klotz T, Reifenrath B, Mathers M, Engelmann U. Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’. Int J Impot Res. 2000;12:305. doi: 10.1038/sj.ijir.3900622. [DOI] [PubMed] [Google Scholar]
- 13.Blanker MH, Bohnen AM, Groeneveld FP, Bernsen RM, Prins A, Thomas S, et al. Correlates for erectile and ejaculatory dysfunction in older Dutch men: a community-based study. J Am Geriatr Soc. 2001;49:436. doi: 10.1046/j.1532-5415.2001.49088.x. [DOI] [PubMed] [Google Scholar]
- 14.Frankel SJ, Donovan JL, Peters TI, Abrams P, Dabhoiwala NF, Osawa D, et al. Sexual dysfunction in men with lower urinary tract symptoms. J Clin Epidemiol. 1998;51:677. doi: 10.1016/s0895-4356(98)00044-4. [DOI] [PubMed] [Google Scholar]
- 15.Boyle P, Robertson C, Mazzetta C, Keech M, Hobbs R, Fourcade R, et al. The association between lower urinary tract symptoms and erectile dysfunction in four centres: the UrEpik study. BJU Int. 2003;92:719. doi: 10.1046/j.1464-410x.2003.04459.x. [DOI] [PubMed] [Google Scholar]
- 16.Shiri R, Hakkinen JT, Hakama M, Huhtala H, Auvinen A, Tammela TL, et al. Effect of lower urinary tract symptoms on the incidence of erectile dysfunction. J Urol. 2005;174:205. doi: 10.1097/01.ju.0000162042.90554.64. [DOI] [PubMed] [Google Scholar]
- 17.Barry MJ, Fowler FJ, Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 18.Leungwattanakij S, Roongreungsilp U, Lertsithichai P, Ratana-Olarn K. The association between erectile function and severity of lower urinary tract symptoms. J Med Assoc Thai. 2005;88:91. [PubMed] [Google Scholar]
- 19.Schiff JD, Mulhall JP. The link between LUTS and ED: clinical and basic science evidence. J Androl. 2004;25:470. doi: 10.1002/j.1939-4640.2004.tb02818.x. [DOI] [PubMed] [Google Scholar]
- 20.Brookes ST, Donovan JL, Peters TJ, Abrams P, Neal DE. Sexual dysfunction in men after treatment for lower urinary tract symptoms: evidence from randomised controlled trial. BMJ. 2002;324:1059. doi: 10.1136/bmj.324.7345.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]