CASE PRESENTATION
A 58-year-old Hispanic man who has been dialysis dependent for 2 years because of diabetic nephropathy reports depressive symptoms during dialysis rounds. For the past 6 weeks, he has had reduced energy and difficulty sleeping and concentrating. He reports a loss of interest in his usual hobbies and family activities and notes an increasing sense of feeling worthless and guilty. He denies suicidal ideation. Medical history includes diabetic retinopathy and neuropathy, coronary artery disease treated with 4-vessel coronary artery bypass grafting 3 years ago, ischemic cardiomyopathy with an ejection fraction of 30%, and cerebrovascular disease. His wife recently has been given a diagnosis of breast cancer. His medications are aspirin, metoprolol, lisinopril, simvastatin, sevelamer, and epoetin alfa. His blood pressure is 130/75 mm Hg, pulse is 65 beats/min, and cardiac and pulmonary examination results are unremarkable. He is interviewed by the social worker in the dialysis unit, who diagnoses clinical depression by using standard Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) (DSM IV) criteria. The patient refuses to discuss his problems with the social worker and declines further psychiatric evaluation. His nephrologist discusses a trial of antidepressant medication, but the patient refuses to use additional medication. During the next month, the patient presents with greater interdialytic weight gains and begins to come late for dialysis sessions. He then presents to a dialysis session reporting dyspnea and orthopnea and is found to have a 10-kg weight gain. On physical examination, blood pressure is 196/96 mm Hg and he has increased jugular venous pressure and bibasilar crackles. He is admitted to the hospital with a diagnosis of congestive heart failure.
INDEX WORDS: Depression, chronic kidney disease, end-stage renal disease (ESRD), treatment
BACKGROUND
Depression is prevalent in patients with chronic kidney disease (CKD) and has been associated with increased morbidity and mortality. Whereas the point prevalence of depression is 2% to 4% in the general community and 5% to 10% in the primary care setting,1 20% to 30% of patients with CKD have clinical depression.2–4 This prevalence is even greater than that reported for patients with other chronic diseases, such as 14% for congestive heart failure5 and 16% for coronary artery disease after acute myocardial infarction.6 Several studies have established that depressive symptoms are associated with recurrent cardiac events in patients with coronary artery disease and new cardiac events in those with no known coronary artery disease.7–15 Depression is an independent risk factor for rehospitalization in patients with congestive heart failure and end-stage renal disease (ESRD)3,5,16–19 and death in patients with recent myocardial infarction, congestive heart failure, or ESRD.3,5,6,16,18–27 Patients with CKD and ESRD experience excessive rates of cardiovascular events and death.28,29 Importantly, in patients with CKD, as in the general population, depression also results in substantial decreases in quality of life, functional impairment, and sexual dysfunction.30–34 It therefore is important to better understand the problems and difficulties diagnosing and treating depression in patients with CKD and whether treatment of depression would improve medical outcomes and selected quality-of-life domains of patients with CKD.16,35 Despite the large randomized placebo-controlled Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) that showed a trend toward benefit of the serotonin-selective reuptake inhibitor (SSRI) sertraline on cardiovascular outcomes in patients with acute myocardial infarction or unstable angina,36 antidepressant medication treatment rates in patients with CKD are very low, in part because the efficacy and safety of antidepressant medications are not fully accepted by physicians caring for these patients.2,37–39 Nevertheless, small studies have explored the use of antidepressant medications, as well as such nonpharmacological treatment of depression as psychotherapy, exercise therapy, cognitive behavioral therapy, and modifications in the dialysis treatment regimen in patients with ESRD.40–44 It should be emphasized that treatment regimens for depression for patients need to be tailored to the individual patient, making it challenging to perform randomized treatment trials of depression in this complex patient population.
In this review, we emphasize the high prevalence of depression in patients with CKD, the association of depression with poor outcomes, and potential mechanisms for this association and review the data for pharmacological and nonpharmacological treatment of depression.
PREVALENCE OF DEPRESSION
Before discussing prevalence, a distinction must be made between depressive symptoms, assessed by using a score on a patient self-administered depression questionnaire, such as the Beck Depression Inventory (BDI), and a clinical diagnosis of major depressive disorder defined by using standard DSM-IV criteria. These criteria define a clinical syndrome lasting for at least 2 weeks, during which the patient experiences either depressed mood or anhedonia plus at least 5 of the 9 DSM-IV symptom domains (Box 1).2,45,46 Patients with CKD may report symptoms of decreased energy, poor appetite, and sleep disturbance on self-report depression questionnaires that may not be confirmed as an episode of a major depressive disorder by using a DSM-IV–based structured clinical interview.2,47 These increased somatic symptoms reported by a chronically ill patient therefore may be misdiagnosed as symptoms of a depressive disorder.48 Furthermore, use of different self-report questionnaires in various studies has likely contributed to the varying estimates (from 15% to 60%) of the prevalence of depression in patients with ESRD.2–4,17,20,30,37,47–51 The lack of consistency in these reports also could reflect different comorbid conditions, populations assessed at different times after the initiation of maintenance dialysis therapy, and different baseline characteristics of the sample population.2
Box 1. DSM-IV Criteria for Major Depressive Episode: Symptom Domains.
Depressed mood
Loss of interest or pleasure
Appetite disturbance
Sleep disturbance
Psychomotor agitation or retardation
Fatigue and tiredness
Worthlessness, feeling like a burden, or guilty
Difficulty concentrating
Recurring thoughts of death or suicide
Source: Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition).46
There is a large body of literature using self-administrated questionnaires, such as the BDI, as a screening tool for the identification of depressive symptoms in patients on maintenance dialysis therapy.2,20,30,35,37,47,51 For example, mean BDI scores in large cohorts of patients with ESRD have averaged about 12 in several studies. Even higher scores were noted in patients at the initiation of dialysis treatment.30,37 Other studies using different questionnaires, such as the Patient Health Questionnaire and the Center for Epidemiological Studies Depression Scale (CES-D), have emphasized the reporting of a large number of depressive symptoms by patients with CKD.4,38
However, few studies have used standard psychiatric criteria for diagnosing clinical depression in patients with CKD. Thus, 2 recent studies that used the health care provider–administered Structured Clinical Interview for Depression (SCID) as the DSM-IV–based standard for the diagnosis of a depressive disorder in cohorts of patients with ESRD deserve special mention.2,4 The SCID is a structured interview that has been validated against the DSM-IV for establishing a psychiatric diagnosis of depressive disorder.52,53 Hedayati et al2 included a cohort that was 85% African American, and Watnick et al4 included primarily white patients. The point prevalence of depressive disorder in patients with ESRD was 26% in both studies, with point prevalences of major depressive disorder of 17.3% and 19%, respectively. The remainder had dysthymia or minor depression based on the SCID.2,4
ASSOCIATION OF DEPRESSION WITH POOR OUTCOMES
Although numerous studies have investigated the association of depression with outcomes in patients with ESRD, interpretation of these studies has been complicated by the lack of standardized criteria for diagnosing depression.54 Documenting the association of depression with outcomes has been complicated further by the proximity of the depression measurement to the time of the outcome measure and persistence or change in depressive symptoms over time. Whereas a few studies involving small numbers of patients show no relationship between baseline depression scores and outcomes,20,55,56 the majority of studies underscore the significance of this relationship.17,20,21,32,57–64 The importance of examining the change in depressive symptom severity scores over time was emphasized in a prospective cohort study of 295 urban maintenance hemodialysis (HD) patients. Although baseline levels of depressive symptoms assessed by using the BDI were not a significant predictor of mortality, depressive symptoms analyzed with a time-varying analysis were significantly associated with mortality in multivariable analysis.20 Soucie and McClellan57 reported a greater rate of death within 90 days of dialysis therapy initiation for depressed versus nondepressed patients. In a study of peritoneal dialysis patients using a time-varying analysis, patients with BDI scores of 11 or higher had a 2-fold greater peritonitis rate than patients with lower BDI scores.64 In a multicenter study involving 9,382 HD patients from 12 countries using the CES-D questionnaire, elevated scores were associated with increased risks of mortality and hospitalization, and past physician diagnosis of depression ascertained from the medical chart was associated with mortality.38 In another population-based study of 1,588 men receiving maintenance HD in US Veterans Affairs facilities, after adjusting for age, race, and comorbid conditions, a diagnosis of depression (noted in the medical records) was significantly associated with increased cumulative hospital days (rate ratio for adjusted model, 1.31; 95% confidence interval [CI], 1.04 to 1.66) and increased number of hospitalizations (rate ratio for adjusted model, 1.30; 95% CI, 1.11 to 1.52).17 Analysis of the Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study showed that although baseline increased depressive symptoms were not associated with increased overall 2-year mortality, persistently greater levels of depressive symptoms over time were associated with increased risk of death and cardiovascular events.21
Perhaps the most compelling evidence for the independent association of depression with poor outcomes in patients with ESRD comes from a prospective observational study in which the diagnosis of depression was based on the DSM-IV–based SCID, administered blindly by a physician to 98 consecutively enrolled maintenance HD patients prospectively followed up for up to 1 year.16 Survival analysis was used to investigate the association between depression and time to the first event, which was defined as either death or hospitalization. The prevalence of depression diagnosed by using the SCID was 26.5%.16 Median time to first follow-up was 5.4 months. By first follow-up, 21 of 26 depressed patients and 31 of 72 nondepressed patients died or were hospitalized. In the unadjusted model, depression was associated with time to death or hospitalization with a hazard ratio of 2.11 (95% CI, 1.21 to 3.68).16
The association remained significant in multivariable models after adjusting for age, sex, race, time on dialysis therapy, and number of comorbid conditions (hazard ratio, 2.07; 95% CI, 1.10 to 3.90).16 To our knowledge, no published data exist to examine the association of depression with poor outcomes in outpatients with CKD before dialysis therapy initiation. One study of inpatients with CKD admitted with a diagnosis of congestive heart failure examined the relationships among severe CKD, corresponding to creatinine clearance less than 30 mL/min/72 kg; depression, diagnosed by using the National Institute of Mental Health Diagnostic Interview Schedule (DIS); and 12-month mortality.48,65 The point prevalence of major depressive disorder by using the DIS was 21.6% if severe CKD was present and 13.0% if absent.48 Both depression by means of the DIS and severe CKD were significant predictors of mortality at 12-month follow-up in adjusted models.48
RISK FACTORS ASSOCIATED WITH DEPRESSION
Younger age, white race, female sex, and longer duration of maintenance HD therapy were associated with a greater prevalence of physician-diagnosed depression in data from the Dialysis Outcomes and Practice Patterns Study (DOPPS).3 Across studies of depression in patients with ESRD, there appears to be a relationship between various comorbid conditions, such as diabetes mellitus, coronary heart disease, cerebrovascular disease, peripheral vascular disease, lung disease, and hypoalbuminemia,2,3,17,37 and depressive symptoms. This association between comorbidity and depressive symptoms is similar to that observed in the general medical population.66 Severity of predialysis CKD also has been associated with increased depressive symptoms.48 This correlation of increased comorbidity and disease severity with depression reported in patients with CKD and ESRD is important to keep in mind when evaluating outcome studies and depression.2,3,16,64 Not surprisingly, lower self-rated quality of life has been correlated with the presence of depressive symptoms.2,30–34,37,67
Depression also has been associated with problems with and disruptions of social interactions and relationships. These can result in an erosion of support provided by spouse and family, work, or community and religious organizations.68–72 Marital and family difficulties for patients with ESRD are well documented.70–72 Reasons for the disruption of social support networks for patients with ESRD and the isolation and withdrawal from social activities are complex and may be related in part to the patients’ various comorbidities, time required for the dialysis treatment itself, postdialysis fatigue, cognitive impairment, and so on.
POTENTIAL MECHANISMS FOR THE ASSOCIATION BETWEEN DEPRESSION AND OUTCOMES
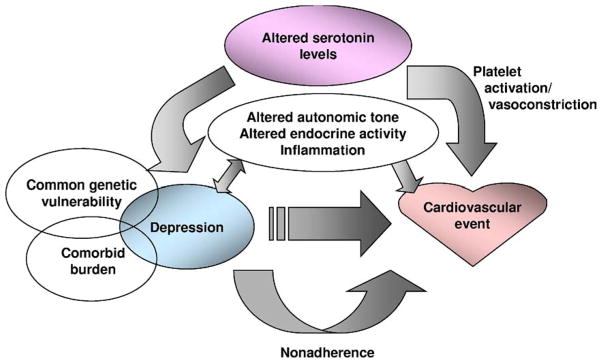
A key question is whether depression itself has a direct mechanistic role in the development of morbidity and mortality in patients with CKD or whether depressive symptoms are merely a surrogate marker for increased comorbidity and disease severity. Specific biological and behavioral factors have been proposed as potential mechanisms by which depression may lead to cardiac events (Fig 1).16,73–89 These factors include common genetic influences on depression and ischemic heart disease observed in twin studies,74,75 altered autonomic tone such as lower heart rate variability,76,77 enhanced hypothalamic-pituitary axis activity such as increased cortisol and norepinephrine excretion,78,79 and alterations in inflammation and immune status.47,80 Depressive symptoms also are associated with lower serum albumin levels.88 The relationship between depression and inflammation appears to be bidirectional.90 It now is well established that depression can result in upregulation of inflammatory mediators that can contribute to depressive symptoms.91 For example, 50% of patients who receive interferon alfa treatment, which can result in decreased brain concentration of serotonin and dopamine, develop clinical depression,92 and this depression can be ameliorated by paroxetine therapy.93 Treatment of cytokine activation associated with inflammatory conditions alone without antidepressants can result in amelioration of depressive symptoms. For example, in 618 patients with psoriatic arthritis treated with etanercept, there was marked improvement in depressive symptoms independent of improvement in associated skin or joint problems.94 Given the activated inflammatory state in many patients with CKD, the relationship between depression and inflammation deserves further exploration.
Figure 1.
Potential mechanisms by which depression may lead to cardiac events.
The relationship between the altered serotonin levels seen in depressed patients and increased platelet aggregation and vasoconstriction, which can lead to coronary events, deserves mention.81–84 There are reports to suggest that depression is associated with changes in platelet function, and SSRIs may have antiplatelet activities.82 Treatment of depressed patients after acute coronary syndrome with sertraline was associated with reductions in platelet activation and a trend toward improved cardiovascular outcomes in SADHART.36,82–84
Perhaps more compelling mechanisms in maintenance dialysis patients in particular are such behavioral factors as nonadherence, unhealthy lifestyle, poor nutrition, and lack of social support.62,85–89 The relationship between depressive symptoms and withdrawal from dialysis therapy noted in the DOPPS is particularly noteworthy.38 Depressive symptoms are associated with nonadherence to medical treatment in patients with ESRD, such as nonadherence to diet and interdialytic weight gain.62,95–99 There is an association between depressive symptoms and peritonitis rates in peritoneal dialysis patients.64 Decreased behavioral compliance is associated in turn with decreased survival.62 The strong correlation of depression with nonadherence suggests the importance of recognizing depression as a risk factor for poor outcomes in patients who may not be adhering to medical advice.100
DIAGNOSIS OF DEPRESSION IN PATIENTS WITH CKD AND ESRD
Although it has been established that such self-report measures of depression as the BDI cannot be used for the diagnosis of a depressive disorder in HD patients,2,4 these scales may serve as quick and easily administered screening tools to identify patients at high risk of depression.2 This becomes especially pertinent given the increasing demands on clinical nephrologists to diagnose and treat medical comorbidities.2 Based on the high prevalence of depression and its association with poor outcomes, we recommend that patients with ESRD be screened at the initiation of dialysis therapy, within 3 to 6 months after therapy initiation, and then yearly.2 Patients who have high scores on depression screening questionnaires should then undergo a structured clinical interview to confirm the presence of a major depressive disorder before treatment options are considered. A challenge for dialysis facilities is how to implement the screening program; can this be done with existing personnel within the facility (social workers, nursing staff, and nephrologists) or do outside consulting personnel need to be used? Some investigators have suggested that a depression screening program can be carried out with existing personnel in the dialysis unit.35
It also should be noted that a higher cutoff score on self-report screening tools should be used in patients with ESRD for a depression threshold, based on previous studies that validated such screening tools in ESRD samples2,4,51 (Table 1). For example, BDI cutoff scores of 14 and higher and 16 and higher were suggested as appropriate cutoff values using the SCID as the DSM-IV–based comparator2,4 and 15 or higher in another study using the DIS as the DSM-IV–based comparator51; these are higher than the cutoff score of 10 or higher validated in the general non-ESRD population.101 Similarly, the CES-D cutoff threshold score for depression of 18 or higher in data reported by Hedayati et al2 is higher than the cutoff score observed for the general population.
Table 1.
Depression Self-Administered Screening Scales Validated for Use in ESRD
| Depression Scale | Characteristics* | Non-ESRD† Cutoff Score | ESRD Cutoff Score |
|---|---|---|---|
| Beck Depression Inventory | 21 Items; score, 0–63 | ≥10 | ≥14–16 |
| Center for Epidemiologic Studies Depression Scale | 20 Items; score, 0–60 | ≥16 | ≥18 |
| Patient Health Questionnaire | 9 Items; score, 0–27 | ≥10 | ≥10 |
Abbreviation: ESRD, end-stage renal disease.
Higher scores represent higher degree of depressive symptoms.
Refers to cutoff scores validated in the general non-ESRD population.
Studies evaluating the use of such depression screening tools in predialysis patients with CKD are limited to a study in which Hedayati et al102 reported the best BDI cutoff score for depression in predialysis patients with stages 2 to 5 CKD to be ≥10, similar to the general population. A likely explanation for higher BDI cutoff scores validated in dialysis patients may be the greater frequency of somatic symptoms assessed by using this tool, such as sleep disturbance, poor appetite, and low energy level, which may not be manifest at earlier stages of predialysis CKD.2,39
PHARMACOLOGICAL TREATMENT OF DEPRESSION
Despite the high prevalence of depression and its association with poor outcomes, only a minority of patients with ESRD are given a diagnosis of and receive treatment for depression.2,37–39 When BDI scores of 15 or higher were used as a marker for depression in patients initiating HD therapy, only 16% were being treated with antidepressants.37 Using a DSM-IV–validated interview, less than half the depressed patients with ESRD were being treated with antidepressants2 and about half of those on drug treatment were receiving subtherapeutic doses.2 Undertreatment of depression and underdosing of antidepressant agents may be caused by nephrologists’ concerns about adverse effects of medications39 because little research has been performed regarding the safety of antidepressant medication use in patients with CKD. Unfortunately, such patients generally are excluded from antidepressant treatment trials because of concerns for safety.36,103
Generally, antidepressant medications are highly protein bound, hepatically metabolized, and not removed significantly by dialysis.104 Furthermore, the relative activity and mode of excretion of metabolites of these drugs in patients with kidney disease often are uncertain and may complicate the use of these drugs if adverse events occur. For example, the half-life of fluoxetine is 24 to 72 hours, and that of its active metabolite is even longer (7 to 9 days).104 Concerns about the safety of antidepressant medication use in patients with moderate to advanced CKD include increased risk of drug-drug interactions for monoamine oxidase inhibitors, tricyclics, and SSRIs104–106; anticholinergic effects and corrected QT interval prolongation for tricyclics104–106; accumulation of toxic metabolites with decreased renal clearance for nefazodone, venlafaxine, and bupropion105; and sexual dysfunction, central nervous system depression, and increased risk of bleeding for SSRIs, which becomes particularly problematic in patients with advanced CKD.39,107–110 SSRIs also have increased serotonergic activity in the gastrointestinal tract and may cause nausea.39,111,112 For these reasons, the safety and efficacy of antidepressant drug therapy in CKD populations have not been clearly established, and this presents a challenge for nephrologists. Table 2 lists commonly used antidepressant medications and potential problems for patients with ESRD.
Table 2.
Common Antidepressant Medications and Potential Side Effects in Patients With ESRD
| Antidepressant Medication | Side Effects | Use in Patients With ESRD |
|---|---|---|
| Selective serotonin reuptake inhibitors (citalopram, fluoxetine, paroxetine, sertraline) | Sexual dysfunction, GI symptoms, CNS symptoms, risk of bleeding | Citalopram: use cautiously in severe renal impairment due to metabolites Fluoxetine: use with caution given long half-life Paroxetine: use lower doses Sertraline: no dose adjustment recommended |
| Serotonin-norepinephrine reuptake inhibitors (venlafaxine) | Accumulation of toxic metabolites, sexual dysfunction, hypertension | Reduce dose by 50% in mild to moderate renal impairment; use with caution |
| Serotonin modulators (nefazodone, trazodone) | Accumulation of toxic metabolites, liver failure (for nefazodone), CNS symptoms, hypotension and cardiac arrhythmias | Avoid use in patients with cardiac disease or hypotension |
| Noradrenergic and specific serotonergics (mirtazapine) | Sedation, weight gain | Give before sleep, reduce dose |
| Dopamine-norepinephrine reuptake inhibitors (bupropion) | Accumulation of toxic metabolites | Use with caution in renal impairment given metabolites |
| Tricyclics and tetracyclics (amitriptyline, desipramine, doxepin, nortriptyline) | CNS symptoms, anticholinergic effects, QTc prolongation, cardiac arrhythmia, orthostatic hypotension | Avoid if possible given cardiac side effects |
| Monamine oxidase inhibitors (phenelzine, selegiline, tranylcypromine) | Drug-drug interactions, enhanced sympathetic activity with ingestion of tyramine-containing foods | Avoid if possible given potential drug-drug interactions, significant side effects |
Note: Given the lack of large randomized well-controlled trials to test the safety of antidepressant medications in patients with ESRD, patients should be monitored closely for side effects, especially before dose escalation is considered.
Abbreviations: ESRD, end-stage renal disease; GI, gastrointestinal; CNS, central nervous system; QTc, corrected QT interval.
There are limited scientific data to clearly suggest that treatment of major depressive disorder is efficacious or that such treatment changes clinical outcomes in patients with CKD.2,47,113–118 Few studies have examined this issue, and they are fraught with limitations, including insufficient sample sizes,40,116–118 lack of placebo-control groups,33,40,115–117 and lack of DSM-IV–based gold-standard criteria for the establishment of a diagnosis of clinical depression.33,117,118 In 1 study, 14 HD patients with major depression were randomly assigned to fluoxetine or placebo.118 No patient discontinued medication. There was a statistically significant improvement in depression at 4, but not at 8, weeks.118 A nonrandomized observational study of antidepressant therapy in long-term peritoneal dialysis patients with a diagnosis of depression on the basis of a structured interview reported significant improvements in BDI scores with therapy (17.4 ± 6.6 at the start and 8.4 ± 3.0 at completion of treatment at 12 weeks).114,115 However, only half the patients with increased BDI scores agreed to be interviewed, and only half of those with a diagnosis of depression agreed to accept pharmacological treatment.114,115 Furthermore, only half of those started on medication successfully completed 12 weeks of treatment.114,115 Reasons for failure to complete a treatment course included the development of acute medical problems unrelated to the use of antidepressant medication, medication side effects, substance abuse, and the presence of concomitant DSM-IV Axis 2 disorders.114,115
NONPHARMACOLOGICAL TREATMENT OF DEPRESSION
Nonpharmacological treatments of depression in patients with ESRD have met with some success in small series (Box 2).40–44 These studies have examined the use of psychotherapy, exercise therapy, cognitive behavioral therapy, and other strategies that basically are not different from those used in the general population.
Box 2. Nonpharmacological Treatment of Depression.
Psychoeducation
Counseling, including cognitive behavioral therapy
Exercise programs
Modifications of the dialysis treatment regimen
Treating anxiety
Addressing difficulties in marital, family, and other supportive relationships, including caregiver burden
Exploring alternative therapies, such as sleep hygiene, meditation, muscle relaxation, and music
Cognitive behavioral therapy, a well-documented evidence-based therapy for depression, is based on the premise that “automatic thoughts” in response to strong negative feelings/emotions can result in distorted or emotional thinking and reasoning and, in turn, poor decisions and ineffective problem solving. However, logical thinking lowers the intensity of strong negative emotions and allows for more effective problem solving. In a recent randomized trial of cognitive behavioral therapy (published only in abstract form), 85 dialysis patients with interview-diagnosed clinical depression were randomly assigned to standard care versus cognitive behavioral therapy with a psychologist.119 Therapy considered the effects of kidney disease and its treatment on daily life, depressive symptoms, coping and cognitive remodeling techniques, relaxation activities, and so on. There was 80% adherence to the treatment regimen. After 3 months, there was a significant difference in BDI scores between the treatment and control groups (14.1 ± 8.7 versus 21.2 ± 9.1, respectively; P < 0.01).119
Exercise programs also may have a beneficial effect on depressive symptoms in patients with ESRD.120,121 In a recent study, 35 HD patients were randomly assigned to a 10-month intradialytic exercise training program.120 There was a 39% reduction in BDI scores in the exercise group after the 10-month study period.120
Considerable interest has been focused on the impact of alterations in the dialysis regimen on health-related quality-of-life assessments. Several studies have explored the impact of in-center nocturnal, home nocturnal, and short daily home or in-center HD on these measures. These studies often suggest improvements in selected health-related quality-of-life domains, including depression.122 For example, one 12-month nonrandomized study of 6-times-weekly in-center short HD was associated with a reduction in BDI scores from 15 to 8 (P < 0.01).123 In addition, an interim analysis of the Following Rehabilitation, Economics and Everyday-Dialysis Outcome Measurements (FREEDOM) study (published only in abstract form) indicated a significant reduction in BDI scores (from 12 to 7) in patients converted from conventional HD to 6-times-weekly short home HD.124 Results of the National Institutes of Health–sponsored randomized trial of more frequent HD (short daily and nocturnal) that is using BDI score as a secondary end point should help clarify the impact of these therapies on depressive symptoms.125 It should be emphasized that the impact of these newer therapies on BDI scores could indicate improvement in somatic symptoms and not affective symptoms. Future randomized trials investigating the effect of various interventions on depression in this chronically ill patient population should consider examining both the somatic and affective components of depressive symptoms.
The relationship between depression and various inflammatory markers has been discussed. Given the activated inflammatory state in many patients with CKD, this relationship deserves further exploration. One is led to wonder whether treatment of depression can ameliorate the inflamed state or, conversely, lessening the inflammation can result in an improvement in depressive symptoms.
Given the magnitude of the problem of depression in patients with CKD, additional therapeutic approaches need to be examined. Interventions that address the problems with social interactions of patients need to be explored in terms of family and marital counseling and involvement of community and religious organizations.68–72 Support and education of caregivers and family members of patients may be helpful. The high incidence of anxiety in the ESRD population has been emphasized126; the well-documented relationship between anxiety and depression suggests that addressing anxiety may be another avenue of potential therapy.127 In addition, there are lessons to be learned from other less traditional approaches to treating depression in patients with other chronic illnesses. For example, a recent Cochrane analysis suggested that music therapy, which is generally accepted by depressed patients, can result in an improved mood.128 These findings were emphasized in a study involving 200 patients with a variety of chronic advanced illnesses who showed significant improvement in mood (P < 0.001) in response to music therapy.129
It should be emphasized that pharmacological and nonpharmacological treatment of depression can be used in combination. Combinations of medication and psychotherapy have been more efficacious than either treatment alone in patients with chronic major depressive disorders.130
CONCLUSION
Recent studies have focused attention on the high prevalence of depression in patients with CKD. It is important to understand the methods used to evaluate depression and the differences between the presence of depressive symptoms and clinical depression. The association of both depressive symptoms and clinical depression with a variety of outcomes is well documented. Several promising studies have explored pharmacological and nonpharmacological approaches to treat depressive symptoms in patients with CKD. It remains to be determined how these treatments will impact on morbidity and mortality, hospitalizations, costs, and health-related quality-of-life measures in these patients.
Acknowledgments
Support: Dr Hedayati’s research was supported by grants from the Veterans Integrated Systems Network 17 and the Veterans Affairs North Texas Health Care System Research Corp. Support also was provided by the University of Texas Southwestern Medical Center O’Brien Kidney Research Core Center (P30DK079328). Dr Finkelstein’s research was supported by grants from the Renal Research Institute.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Financial Disclosure: None.
References
- 1.Kessler RC, Berglund P, Demler O, et al. National Comorbidity Survey Replication. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication. JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Hedayati SS, Bosworth HB, Kuchibhatla M, Kimmel PL, Szczech LA. The predictive value of self-report scales compared with physician diagnosis of depression in hemodialysis patients. Kidney Int. 2006;69:1662–1668. doi: 10.1038/sj.ki.5000308. [DOI] [PubMed] [Google Scholar]
- 3.Lopes AA, Bragg J, Young E, et al. Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. 2002;62:199–207. doi: 10.1046/j.1523-1755.2002.00411.x. [DOI] [PubMed] [Google Scholar]
- 4.Watnick S, Wang PL, Demadura T, Ganzini L. Validation of 2 depression screening tools in dialysis patients. Am J Kidney Dis. 2005;46:919–924. doi: 10.1053/j.ajkd.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 6.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 7.Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 8.Wassertheil-Smoller S, Shumaker S, Ockene J, et al. Depression and cardiovascular sequelae in postmenopausal women. The Women’s Health Initiative (WHI) Arch Intern Med. 2004;164:289–298. doi: 10.1001/archinte.164.3.289. [DOI] [PubMed] [Google Scholar]
- 9.Bruce ML, Leaf PJ. Psychiatric disorders and 15-month mortality in a community sample of older adults. Am J Public Health. 1989;79:727–730. doi: 10.2105/ajph.79.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anda R, Williamson D, Jones D, et al. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of U.S. adults. Epidemiology. 1993;4:285–294. doi: 10.1097/00001648-199307000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Pratt LA, Ford DE, Crum RM, Armenian HK, Gallo JJ, Eaton WW. Depression, psychotropic medication, and risk of myocardial infarction. Prospective data from the Baltimore ECA follow-up. Circulation. 1996;94:3123–3129. doi: 10.1161/01.cir.94.12.3123. [DOI] [PubMed] [Google Scholar]
- 12.Ariyo AA, Haan M, Tangen CM, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Cardiovascular Health Study Collaborative Research Group. Circulation. 2000;102:1773–1779. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- 13.Applegate WB, Pressel S, Wittes J, et al. Impact of the treatment of isolated systolic hypertension on behavioral variables. Results from the Systolic Hypertension in the Elderly Program. Arch Intern Med. 1994;154:2154–2160. [PubMed] [Google Scholar]
- 14.Wassertheil-Smoller S, Applegate WB, Berge K, et al. Change in depression as a precursor of cardiovascular events. SHEP Cooperative Research Group (Systolic Hypertension in the Elderly) Arch Intern Med. 1996;156:553–561. [PubMed] [Google Scholar]
- 15.Penninx BW, Guralnik JM, Mendes de Leon CF, et al. Cardiovascular events and mortality in newly and chronically depressed persons 70 years of age. Am J Cardiol. 1998;81:988–994. doi: 10.1016/s0002-9149(98)00077-0. [DOI] [PubMed] [Google Scholar]
- 16.Hedayati SS, Bosworth H, Briley L, et al. Death or hospitalization of patients on chronic hemodialysis is associated with a physician-based diagnosis of depression. Kidney Int. 2008;74:930–936. doi: 10.1038/ki.2008.311. [DOI] [PubMed] [Google Scholar]
- 17.Hedayati SS, Grambow SC, Szczech LA, Stechuchak KM, Allen AS, Bosworth HB. Physician-diagnosed depression as a correlate of hospitalizations in patients receiving long-term hemodialysis. Am J Kidney Dis. 2005;46:642–649. doi: 10.1053/j.ajkd.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Jiang W, Kuchibhatla M, Cuffe MS, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110:3452–3456. doi: 10.1161/01.CIR.0000148138.25157.F9. [DOI] [PubMed] [Google Scholar]
- 19.Krumholz HM, Butler J, Miller J. Prognostic importance of emotional support for elderly patients hospitalized with heart failure. Circulation. 1998;97:958–964. doi: 10.1161/01.cir.97.10.958. [DOI] [PubMed] [Google Scholar]
- 20.Kimmel PL, Peterson RA, Weihs KL, et al. Multiple measurements of depression predict mortality in a longitudinal study of chronic hemodialysis outpatients. Kidney Int. 2000;57:2093–2098. doi: 10.1046/j.1523-1755.2000.00059.x. [DOI] [PubMed] [Google Scholar]
- 21.Boulware LE, Liu Y, Fink NE, et al. Temporal relation among depression symptoms, cardiovascular disease events, and mortality in end-stage renal disease: Contribution of reverse causality. Clin J Am Soc Nephrol. 2006;1:496–504. doi: 10.2215/CJN.00030505. [DOI] [PubMed] [Google Scholar]
- 22.Ziegelstein RC. Depression in patients recovering from a myocardial infarction. JAMA. 2001;286:1621–1627. doi: 10.1001/jama.286.13.1621. [DOI] [PubMed] [Google Scholar]
- 23.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 24.Bush DE, Ziegelstein RC, Tayback M, et al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol. 2001;88:337–341. doi: 10.1016/s0002-9149(01)01675-7. [DOI] [PubMed] [Google Scholar]
- 25.Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation. 2002;105:1049–1053. doi: 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]
- 26.Frasure-Smith N, Lesperance F, Gravel G, et al. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000;101:1919–1924. doi: 10.1161/01.cir.101.16.1919. [DOI] [PubMed] [Google Scholar]
- 27.Carinci F, Nicolucci A, Ciampi A, et al. Role of interactions between psychological and clinical factors in determining 6-month mortality among patients with acute myocardial infarction. Application of recursive partitioning techniques to the GISSI-2 database. Gruppo Italiano per lo Studio della Sopravvivenza nell’ Infarto Miocardico. Eur Heart J. 1997;18:835–845. doi: 10.1093/oxfordjournals.eurheartj.a015349. [DOI] [PubMed] [Google Scholar]
- 28.McMurray JJ, Velazquez EJ, Solomon SD, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]
- 29.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 30.Walters BA, Hays RD, Spritzer KL, et al. Health-related quality of life, depressive symptoms, anemia, and malnutrition at hemodialysis initiation. Am J Kidney Dis. 2002;40:1185–1194. doi: 10.1053/ajkd.2002.36879. [DOI] [PubMed] [Google Scholar]
- 31.Dogan E, Erkoc R, Eryonucu B, et al. Relation between depression, some laboratory parameters, and quality of life in hemodialysis patients. Ren Fail. 2005;27:695–699. doi: 10.1080/08860220500242728. [DOI] [PubMed] [Google Scholar]
- 32.Drayer RA, Piraino B, Reynolds CF, III, et al. Characteristics of depression in hemodialysis patients: Symptoms, quality of life and mortality risk. Gen Hosp Psychiatry. 2006;28:306–312. doi: 10.1016/j.genhosppsych.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 33.Turk S, Atalay H, Altintepe L, et al. Treatment with antidepressive drugs improved quality of life in chronic hemodialysis patients. Clin Nephrol. 2006;65:113–118. doi: 10.5414/cnp65113. [DOI] [PubMed] [Google Scholar]
- 34.Peng YS, Chiang CK, Hung KY, et al. The association of higher depressive symptoms and sexual dysfunction in male haemodialysis patients. Nephrol Dial Transplant. 2007;22:857–861. doi: 10.1093/ndt/gfl666. [DOI] [PubMed] [Google Scholar]
- 35.Finkelstein FO, Wuerth D, Troidle LK, Finkelstein SH. Depression and end-stage renal disease: A therapeutic challenge. Kidney Int. 2008;74:843–845. doi: 10.1038/ki.2008.222. [DOI] [PubMed] [Google Scholar]
- 36.Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 37.Watnick S, Kirwin P, Mahnensmith R, Concato J. The prevalence and treatment of depression among patients starting dialysis. Am J Kidney Dis. 2003;41:105–110. doi: 10.1053/ajkd.2003.50029. [DOI] [PubMed] [Google Scholar]
- 38.Lopes AA, Albert JM, Young EW, et al. Screening for depression in hemodialysis patients: Associations with diagnosis, treatment, and outcomes in the DOPPS. Kidney Int. 2004;66:2047–2053. doi: 10.1111/j.1523-1755.2004.00977.x. [DOI] [PubMed] [Google Scholar]
- 39.Cohen SD, Norris L, Acquaviva K, et al. Screening, diagnosis, and treatment of depression in patients with end-stage renal disease. Clin J Am Soc Nephrol. 2007;2:1332–1342. doi: 10.2215/CJN.03951106. [DOI] [PubMed] [Google Scholar]
- 40.Koo JR, Yoon JY, Joo MH, et al. Treatment of depression and effect of antidepression treatment on nutritional status in chronic hemodialysis patients. Am J Med Sci. 2005;329:1–5. doi: 10.1097/00000441-200501000-00001. [DOI] [PubMed] [Google Scholar]
- 41.Friend R, Singletary Y, Mendell NR, Nurse H. Group participation and survival among patients with end-stage renal disease. Am J Public Health. 1986;76:670–672. doi: 10.2105/ajph.76.6.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kouidi E, Iacovides A, Iordanidis P, et al. Exercise renal rehabilitation program: Psychosocial effects. Nephron. 1997;77:152–158. doi: 10.1159/000190266. [DOI] [PubMed] [Google Scholar]
- 43.van Vilsteren MC, Greef MH, Huisman RM. The effects of a low-to-moderate intensity pre-conditioning exercise programme linked with exercise counseling for sedentary hemodialysis patients in The Netherlands: Results of a randomized clinical trial. Nephrol Dial Transplant. 2004;20:141–146. doi: 10.1093/ndt/gfh560. [DOI] [PubMed] [Google Scholar]
- 44.Cukor D. Use of cognitive behavioral therapy to treat depression among patients on hemodialysis. Psychiatr Serv. 2007;58:711–712. doi: 10.1176/ps.2007.58.5.711. [DOI] [PubMed] [Google Scholar]
- 45.Snow V, Lascher S, Mottur-Pilson C. Pharmacologic treatment of acute major depression and dysthymia. Ann Intern Med. 2000;132:738–742. doi: 10.7326/0003-4819-132-9-200005020-00010. [DOI] [PubMed] [Google Scholar]
- 46.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 47.Kimmel PL, Weihs K, Peterson RA. Survival in hemodialysis patients: The role of depression. J Am Soc Nephrol. 1993;4:12–27. doi: 10.1681/ASN.V4112. [DOI] [PubMed] [Google Scholar]
- 48.Hedayati SS, Jiang W, O’Connor CM, et al. The association between depression and chronic kidney disease and mortality among patients hospitalized with congestive heart failure. Am J Kidney Dis. 2004;44:207–215. doi: 10.1053/j.ajkd.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 49.Kimmel PL. Depression in patients with chronic renal disease: What we know and what we need to know. J Psychosom Res. 2002;53:951–956. doi: 10.1016/s0022-3999(02)00310-0. [DOI] [PubMed] [Google Scholar]
- 50.Parkenson GR, Gutman RA. Predictors of functional health status of end-stage renal disease patients. Health Care Financing Rev. 1997;18:37–49. [PMC free article] [PubMed] [Google Scholar]
- 51.Craven JL, Rodin GM, Littlefield C. The BDI as a screening device for major depression in renal dialysis patients. Int J Psychiatry Med. 1998;18:365–374. doi: 10.2190/m1tx-v1ej-e43l-rklf. [DOI] [PubMed] [Google Scholar]
- 52.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IVAxis I Disorders—Non-patient Edition (SCID-I/NP, Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 53.Skre I, Onstad S, Torgensen S, Kringlen E. High interrater reliability for the Structured Clinical Interview for DSM-III-R axis I (SCID I) Acta Psychiatr Scand. 1991;84:167–173. doi: 10.1111/j.1600-0447.1991.tb03123.x. [DOI] [PubMed] [Google Scholar]
- 54.Cukor D, Peterson RA, Cohen SD, Kimmel PL. Depression in end-stage renal disease hemodialysis patients. Nat Clin Pract Nephrol. 2006;2:678–687. doi: 10.1038/ncpneph0359. [DOI] [PubMed] [Google Scholar]
- 55.Devins GM, Mann J, Mandin H. Psychosocial predictors of survival in end-stage renal disease. J Nerv Ment Dis. 1990;178:127–133. doi: 10.1097/00005053-199002000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Christensen AJ, Wiebe JS, Smith TW, Turner CW. Predictors of survival among hemodialysis patients: Effects of perceived family support. Health Psychol. 1994;13:521–525. doi: 10.1037//0278-6133.13.6.521. [DOI] [PubMed] [Google Scholar]
- 57.Soucie JM, McClellan WM. Early death in dialysis patients: Risk factors and impact on incidence and mortality rates. J Am Soc Nephrol. 1996;10:2169–2175. doi: 10.1681/ASN.V7102169. [DOI] [PubMed] [Google Scholar]
- 58.Shulman R, Price JDE, Spinelli J. Biopsychosocial aspects of long-term survival on end-stage renal failure therapy. Psychol Med. 1989;19:945–954. doi: 10.1017/s0033291700005663. [DOI] [PubMed] [Google Scholar]
- 59.Wai L, Burton H, Richmond J, Lindsay RM. Influence of psychosocial factors on survival of home dialysis patients. Lancet. 1981;2:1155–1156. doi: 10.1016/s0140-6736(81)90599-7. [DOI] [PubMed] [Google Scholar]
- 60.Burton HJ, Kline SA, Lindsay RM, Heidenheim AP. The relationship of depression to survival in chronic renal failure. Psychosom Med. 1986;48:261–269. doi: 10.1097/00006842-198603000-00011. [DOI] [PubMed] [Google Scholar]
- 61.Ziarnik JP, Freeman CW, Sherrard DJ, Calsyn DA. Psychological correlates of survival on renal dialysis. J Nerv Ment Dis. 1977;164:210–213. doi: 10.1097/00005053-197703000-00007. [DOI] [PubMed] [Google Scholar]
- 62.Kimmel PL, Peterson RA, Weihs KL, et al. Psychosocial factors, behavioral compliance and survival in urban hemodialysis patients. Kidney Int. 1998;54:245–254. doi: 10.1046/j.1523-1755.1998.00989.x. [DOI] [PubMed] [Google Scholar]
- 63.Peterson RA, Kimmel PL, Sacks CR, Mesquita ML, Simmens SJ, Reiss D. Depression, perception of illness and mortality in patients with end-stage renal disease. Int J Psychiatry Med. 1991;21:343–354. doi: 10.2190/D7VA-FWEU-JN5Y-TD3E. [DOI] [PubMed] [Google Scholar]
- 64.Troidle L, Watnick S, Wuerth DB, Gorban-Brennan N, Kliger AS, Finkelstein FO. Depression and its association with peritonitis in long-term peritoneal dialysis patients. Am J Kidney Dis. 2003;42:350–354. doi: 10.1016/s0272-6386(03)00661-9. [DOI] [PubMed] [Google Scholar]
- 65.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule, its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 66.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 67.Kimmel PL. Psychosocial factors in adult end-stage renal disease patients treated with hemodialysis: Correlates and outcomes. Am J Kidney Dis. 2000;35(suppl 1):S132–S140. doi: 10.1016/s0272-6386(00)70240-x. [DOI] [PubMed] [Google Scholar]
- 68.Cohen SD, Sharma T, Acuaviva K, Peterson RA, Patel SS, Kimmel PL. Social support and chronic kidney disease: An update. Adv Chronic Kidney Dis. 2007;14:335–344. doi: 10.1053/j.ackd.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 69.Patel SS, Peterson RA, Kimmel PL. The impact of social support on end-stage renal disease. Semin Dial. 2005;18:98–102. doi: 10.1111/j.1525-139X.2005.18203.x. [DOI] [PubMed] [Google Scholar]
- 70.Daneker B, Kimmel PL, Ranich T, Petersom RA. Depression and marital dissatisfaction with end-stage renal disease and their spouses. Am J Kidney Dis. 2001;38:839–846. doi: 10.1053/ajkd.2001.27704. [DOI] [PubMed] [Google Scholar]
- 71.Steele TE, Finkelstein SH, Finkelstein FO. Hemodialysis patients and spouses: Marital discord, sexual problems, and depression. J Nerv Ment Dis. 1976;162:225–237. [PubMed] [Google Scholar]
- 72.Steidl JH, Finkelstein FO, Wexler JP, et al. Medical condition, adherence to treatment regimens and family functioning. Arch Gen Psychiatry. 1980;37:1025–1027. doi: 10.1001/archpsyc.1980.01780220063006. [DOI] [PubMed] [Google Scholar]
- 73.Whooley MA. Depression and cardiovascular disease: Healing the broken-hearted. JAMA. 2006;295:2874–2881. doi: 10.1001/jama.295.24.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McCaffery JM, Frasure-Smith N, Dube MP. Common genetic vulnerability to depressive symptoms and coronary artery disease: A review and development of candidate genes related to inflammation and serotonin. Psychosom Med. 2006;68:187–200. doi: 10.1097/01.psy.0000208630.79271.a0. [DOI] [PubMed] [Google Scholar]
- 75.Scherrer JF, Hong X, Bucholz KK, et al. A twin study of depression symptoms, hypertension, and heart disease in middle-aged men. Psychosom Med. 2003;65:548–557. doi: 10.1097/01.psy.0000077507.29863.cb. [DOI] [PubMed] [Google Scholar]
- 76.Carney RM, Blumenthal JA, Stein PK. Depression, heart rate variability, and acute myocardial infarction. Circulation. 2001;104:2024–2028. doi: 10.1161/hc4201.097834. [DOI] [PubMed] [Google Scholar]
- 77.Krittayaphong R, Cascio WE, Light KC. Heart rate variability in patients with coronary artery disease: Differences in patients with higher and lower depression scores. Psychosom Med. 1997;59:231–235. doi: 10.1097/00006842-199705000-00004. [DOI] [PubMed] [Google Scholar]
- 78.Otte C, Marmar CR, Pipkin SS, et al. Depression and 24-hour urinary cortisol in medical outpatients with coronary heart disease: The Heart and Soul Study. Biol Psychiatry. 2004;56:241–247. doi: 10.1016/j.biopsych.2004.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Otte C, Neylan TC, Pipkin S, et al. Depressive symptoms and 24-hour urinary norepinephrine excretion levels in patients with coronary disease: Findings from the Heart and Soul Study. Am J Psychiatry. 2005;162:2139–2145. doi: 10.1176/appi.ajp.162.11.2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Empana JP, Sykes DH, Luc G. Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men: The Prospective Epidemiological Study of Myocardial Infarction (PRIME) Circulation. 2005;111:2299–2305. doi: 10.1161/01.CIR.0000164203.54111.AE. [DOI] [PubMed] [Google Scholar]
- 81.Butler J, Leonard BE. The platelet serotonergic system in depression and following sertraline treatment. Int Clin Psychopharmacol. 1988;3:343–347. doi: 10.1097/00004850-198810000-00005. [DOI] [PubMed] [Google Scholar]
- 82.Serebruany VL, Glassman AH, Malinin AI, et al. SADHART Study Group: Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin re-uptake inhibitor sertraline after acute coronary events. Circulation. 2003;108:939–944. doi: 10.1161/01.CIR.0000085163.21752.0A. [DOI] [PubMed] [Google Scholar]
- 83.Serebruany VL, Glassman AH, Malinin AI, et al. Enhanced platelet/endothelial activation in depressed patients with acute coronary syndromes: Evidence from recent clinical trials. Blood Coagul Fibrinol. 2003;14:563–567. doi: 10.1097/00001721-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 84.Serebruany VL, Suckow RF, Cooper TB, et al. Sertraline Antidepressant Heart Attack Randomized Trial. Relationship between release of platelet/endothelial biomarkers and plasma levels of sertraline and N-desmethylsertraline in acute coronary syndrome patients receiving SSRI treatment for depression. Am J Psychiatry. 2005;162:1165–1170. doi: 10.1176/appi.ajp.162.6.1165. [DOI] [PubMed] [Google Scholar]
- 85.Ziegelstein RC, Fauerbach JA, Stevens SS, et al. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med. 2000;160:1818–1823. doi: 10.1001/archinte.160.12.1818. [DOI] [PubMed] [Google Scholar]
- 86.Barefoot JC, Burg MM, Carney RM. Aspects of social support associated with depression at hospitalization and follow-up assessment among cardiac patients. J Cardio-pulm Rehabil. 2003;23:404–412. doi: 10.1097/00008483-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 87.Bonnet F, Irving K, Terra JL, et al. Anxiety and depression are associated with unhealthy lifestyle in patients at risk of cardiovascular disease. Atherosclerosis. 2005;178:339–344. doi: 10.1016/j.atherosclerosis.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 88.Friend R, Hatchett L, Wadhwa NK, Suh H. Serum albumin and depression in end-stage renal disease. Adv Perit Dial. 1997;13:155–157. [PubMed] [Google Scholar]
- 89.Koo JR, Yoon JW, Kim SG, et al. Association of depression with malnutrition in chronic hemodialysis patients. Am J Kidney Dis. 2003;41:1037–1042. doi: 10.1016/s0272-6386(03)00201-4. [DOI] [PubMed] [Google Scholar]
- 90.Raison CL, Capuron L, Miller AH. Cytokines sing the blues: Inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Miller AH, Maletic V, Raison CL. Inflammation and its discontents: The role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–741. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Capuron L, Miller AH. Cytokines and psychopathology: Lessons from interferon-alpha. Biol Psychiatry. 2004;56:819–824. doi: 10.1016/j.biopsych.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 93.Musselman DL, Lawson DH, Gumnick JF, et al. Paroxetine for the prevention of depression induced by high-dose interferon alfa. N Engl J Med. 2001;344:961–966. doi: 10.1056/NEJM200103293441303. [DOI] [PubMed] [Google Scholar]
- 94.Tyring S, Gottlieb A, Papp K, et al. Etarnecept and clinical outcomes, fatigue, and depression in psoriasis: Double-blind placebo-controlled randomised phase III trial. Lancet. 2006;367:29–35. doi: 10.1016/S0140-6736(05)67763-X. [DOI] [PubMed] [Google Scholar]
- 95.Kimmel PL, Peterson RA, Weihs KL, et al. Behavioral compliance with dialysis prescription in hemodialysis patients. J Am Soc Nephrol. 1995;5:1826–1834. doi: 10.1681/ASN.V5101826. [DOI] [PubMed] [Google Scholar]
- 96.Everett KD, Brantley PJ, Sletten C, et al. The relation of stress and depression to interdialytic weight gain in hemodialysis patients. Behav Med. 1995;21:25–30. doi: 10.1080/08964289.1995.9933739. [DOI] [PubMed] [Google Scholar]
- 97.Safdar N, Baakza H, Kumar H, et al. Non-compliance to diet and fluid restrictions in haemodialysis patients. J Pak Med Assoc. 1995;45:293–295. [PubMed] [Google Scholar]
- 98.Sensky T, Leger C, Gilmour S. Psychosocial and cognitive factors associated with adherence to dietary and fluid restriction regimens by people on chronic haemodialysis. Psychother Psychosom. 1996;65:36–42. doi: 10.1159/000289029. [DOI] [PubMed] [Google Scholar]
- 99.Brownbridge G, Fielding DM. Psychosocial adjustment and adherence to dialysis treatment regimes. Pediatr Nephrol. 1994;8:744–749. doi: 10.1007/BF00869109. [DOI] [PubMed] [Google Scholar]
- 100.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 101.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psych. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 102.Hedayati SS, Minhajudin AT, Toto RD, Morris DW, Rush AJ. Validation of depression screening scales in patients with CKD. Am J Kidney Dis. 2009 Jun 2; doi: 10.1053/j.ajkd.2009.03.016. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Alpert JE, Biggs MM, Davis L, et al. STAR*D Investigators: Enrolling research subjects from clinical practice: Ethical and procedural issues in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial. Psychiatry Res. 2006;141:193–200. doi: 10.1016/j.psychres.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 104.Micromedex® Healthcare Series [intranet database]. Version 5.1. Greenwood Village, CO: Thomson Reuters Health-care, Inc; 2008. [Google Scholar]
- 105.Cohen LM, Tessier EG, Germain MJ, Levy NB. Update on psychotropic medication use in renal disease. Psychosomatics. 2004;45:34–48. doi: 10.1176/appi.psy.45.1.34. [DOI] [PubMed] [Google Scholar]
- 106.Cohen SD, Perkins V, Kimmel PL. Psychosocial issues in ESRD patients. In: Daugirdas J, Ing T, editors. Handbook of Dialysis. 4. Boston, MA: Little Brown; 2007. pp. 455–461. [Google Scholar]
- 107.Yuan Y, Tsoi K, Hunt RH. Selective serotonin reuptake inhibitors and the risk of upper gastrointestinal bleeding: Confusion or confounding? Am J Med. 2006;119:719–727. doi: 10.1016/j.amjmed.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 108.Wessinger S, Kaplan M, Choi L, et al. Increased use of selective serotonin reuptake inhibitors in patients admitted with gastrointestinal hemorrhage: A multi-center retrospective analysis. Aliment Pharmacol Ther. 2006;23:937–944. doi: 10.1111/j.1365-2036.2006.02859.x. [DOI] [PubMed] [Google Scholar]
- 109.Dalton SO, Johansen C, Mellemkjaer L. Use of selective serotonin reuptake inhibitors and risk of gastrointestinal bleeding: A population-based cohort study. Arch Intern Med. 2003;163:59–64. doi: 10.1001/archinte.163.1.59. [DOI] [PubMed] [Google Scholar]
- 110.Serebruarny VL. Selective serotonin reuptake inhibitors and increasing bleeding risk: Are we missing something? Am J Med. 2006;119:113–116. doi: 10.1016/j.amjmed.2005.03.044. [DOI] [PubMed] [Google Scholar]
- 111.Spigset O. Adverse reactions of selective serotonin reuptake inhibitors. Drug Saf. 1999;29:277–287. doi: 10.2165/00002018-199920030-00007. [DOI] [PubMed] [Google Scholar]
- 112.Ueda N, Yoshimura R, Shinkai K, et al. Higher plasma 5-hydroxyindoleacetic acid levels are associated with SSRI-induced nausea. Neuropsychobiology. 2003;48:31–34. doi: 10.1159/000071826. [DOI] [PubMed] [Google Scholar]
- 113.Finkelstein FO, Finkelstein SH. Depression in chronic dialysis patients: Assessment and treatment. Nephrol Dial Transplant. 2000;15:1911–1913. doi: 10.1093/ndt/15.12.1911. [DOI] [PubMed] [Google Scholar]
- 114.Wuerth D, Finkelstein SH, Finkelstein FO. The identification and treatment of depression in patients maintained on dialysis. Semin Dial. 2005;18:142–146. doi: 10.1111/j.1525-139X.2005.18213.x. [DOI] [PubMed] [Google Scholar]
- 115.Wuerth D, Finkelstein SH, Ciarcia J, et al. Identification and treatment of depression in a cohort of patients maintained on chronic peritoneal dialysis. Am J Kidney Dis. 2001;37:1011–1017. doi: 10.1016/s0272-6386(05)80018-6. [DOI] [PubMed] [Google Scholar]
- 116.Kennedy SH, Craven JL, Rodin GM. Major depression in renal dialysis patients: An open trial of antidepressant therapy. J Clin Psychiatry. 1989;50:60–63. [PubMed] [Google Scholar]
- 117.Levy NB, Blumenfield M, Beasley CM, Jr, et al. Fluoxetine in depressed patients with renal failure and in depressed patients with normal kidney function. Gen Hosp Psychiatry. 1996;18:8–13. doi: 10.1016/0163-8343(95)00073-9. [DOI] [PubMed] [Google Scholar]
- 118.Blumenfield M, Levy NB, Spinowitz B, et al. Fluoxetine in depressed patients on dialysis. Int J Psychiatry Med. 1997;27:71–80. doi: 10.2190/WQ33-M54T-XN7L-V8MX. [DOI] [PubMed] [Google Scholar]
- 119.Sesso R, Miyasaki MC, Duarte PS, et al. Effectiveness of cognitive behavioral therapy in hemodialysis patients with depression. J Am Soc Nephrol. 2008;19:52A. (abstr) [Google Scholar]
- 120.Ouzouni S, Kouidi E, Sioulis A, Grekas D, Deligiannis A. Effects of intradialytic exercise training on health-related quality of life indices in haemodialysis patients. Clin Rehabil. 2009;23:53–63. doi: 10.1177/0269215508096760. [DOI] [PubMed] [Google Scholar]
- 121.Levendog lu F, Altintepe L, Okudan N, et al. A twelve week exercise program improves the psychological status, quality of life and work capacity in hemodialysis patients. J Nephrol. 2004;17:826–832. [PubMed] [Google Scholar]
- 122.Finkelstein FO, Finkelstein SH, Wuerth D, Shirani S, Troidle L. Effects of home hemodialysis on health-related quality of life measures. Semin Dial. 2007;20:265–268. doi: 10.1111/j.1525-139X.2007.00287.x. [DOI] [PubMed] [Google Scholar]
- 123.Reynolds JT, Homel P, Cantey L, et al. A one year trial of in-center daily hemodialysis with an emphasis on quality of life. Blood Purif. 2004;22:320–328. doi: 10.1159/000079186. [DOI] [PubMed] [Google Scholar]
- 124.Finkelstein FO, Collins A, Glickan J, et al. Daily home hemodialysis improves the quality of life measures, depressive symptoms and recovery time: Interim results from the FREEDOM Study. J Am Soc Nephrol. 2008;19:52A. (abstr) [Google Scholar]
- 125.Suri RS, Garg AX, Chertow GM, et al. Frequent Hemodialysis Network Trial Group: Frequent Hemodialysis Network (FHN) randomized trials: Study design. Kidney Int. 2007;71:349–359. doi: 10.1038/sj.ki.5002032. [DOI] [PubMed] [Google Scholar]
- 126.Cukor D, Coplan J, Brown C, et al. Anxiety disorders in adults treated by hemodialysis: A single-center study. Am J Kidney Dis. 2008;52:128–136. doi: 10.1053/j.ajkd.2008.02.300. [DOI] [PubMed] [Google Scholar]
- 127.Strine TW, Kroenke K, Dhingra S, et al. The associations between depression, health-related quality of life, social support, life satisfaction, and disability in community-dwelling US adults. J Nerv Ment Dis. 2009;197:61–64. doi: 10.1097/NMD.0b013e3181924ad8. [DOI] [PubMed] [Google Scholar]
- 128.Maratos AS, Gold C, Wang X, Crawford MJ. Music therapy for depression. Cochrane Database Syst Rev. 2006:CD004517. doi: 10.1002/14651858.CD004517.pub2. [DOI] [PubMed] [Google Scholar]
- 129.Gallagher LM, Lagman R, Walsh D, Davis MP, Legrand SB. The clinical effects of music therapy in palliative medicine. Support Care Cancer. 2006;14:859–866. doi: 10.1007/s00520-005-0013-6. [DOI] [PubMed] [Google Scholar]
- 130.Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]