Abstract
Background
This study compared six of the briefest screening instruments for detecting DSM-IV-defined Alcohol Use Disorder (AUD) among older adolescents treated in Emergency Departments (ED).
Methods
The AUDIT-C, the RAPS4-QF, the FAST, the CRAFFT, the RUFT-Cut, and 2-Items from the Diagnostic and Statistical Manual IV of the American Psychiatric Association (APA, 1994) criteria for AUD (heretofore referred to as the DSM-IV 2-Item Scale) were evaluated against the criterion of a current DSM-IV diagnosis of either alcohol abuse or dependence. The instruments were administered to 181 alcohol-using older adolescents (57% males; age range 18–20 years) in an ED and compared using Receiver Operator Characteristic (ROC) analyses against the criterion of a current DSM-IV diagnosis of alcohol abuse or dependence.
Results
Of these instruments, the DSM-IV 2-Item Scale performed best for identifying AUD (88% sensitivity and 90% specificity), followed by the FAST and the AUDIT-C.
Conclusions
Two items from the DSM-IV criteria for AUD performed best for identifying ED-treated older adolescents with alcohol use disorders. The FAST and AUDIT-C performed well, but are longer and more difficult to score in the hectic environment of the Emergency Department.
Keywords: alcohol screening, adolescent, alcohol use disorders, emergency department
1.0 Introduction
Until the mid-1980’s, the 4-item CAGE (Ewing, 1984) was the only brief alcohol screening instrument available. In the early-1990’s, the Alcohol Use Disorders Identification Test (AUDIT) was developed and was found to be the best “brief” screening instrument for use among adults (Saunders et al., 1993). However, the AUDIT is relatively long and uses a relatively complicated scoring system (10 questions, range 0=40 points). During the last 20 years, alcohol research has seen a burgeoning of that focus on the development of very brief screening instruments for the identification of hazardous drinking and alcohol use disorders (AUD) in primary care settings studies (e.g., Cherpitel, 1999; Hodgson et al., 2003; Knight et al., 1999; Russell et al., 1989, Saunders et al., 1993). ). Ease and brevity in administration are assets for alcohol screens used in the ED, yet few studies have directly compared the performance of the briefest of these alcohol screens to determine their suitability for use with young adults in an ED setting. Evaluation of these instruments usually focuses on their sensitivity (ability to identify true positive cases) and their specificity (ability to identify true negative cases).
Recently, a short version of the AUDIT (the AUDIT-C) that uses only the consumption items (Items 1–3; range 0–12) (AUDIT-C) was found to accurately identify 84% of ED patients with a DSM-IV defined alcohol abuse or alcohol dependence disorder, while correctly classifying 74% of those patients without an AUD, using a cut-point of 4 (Dawson et al., 2005). At a cut-point of 5, the AUDIT-C was 78% sensitive and 79% specific for identifying AUD among people in the 18–29 year old age group. Although the AUDIT-C is much shorter than the full AUDIT, its 12-point scoring system is still somewhat unwieldy.
A screening instrument developed for use in ED, the RAPS4 assesses remorse over drinking, alcoholic blackouts, impairment in completing responsibilities, and drinking in the morning. The RAPS4 has been shown to be effective for identifying adult ED patients with alcohol dependence, but was less useful for detecting alcohol abuse (Cherpitel, 1995; 2000). A version of the RAPS4, the 6-item RAPS4-QF, which also assesses alcohol consumption, however, can identify 90% of alcohol abuse cases while correctly identifying 82% of alcohol abuse non-cases among adults treated in emergency departments (Cherpitel, 2002).
The CRAFFT (Knight et al., 1999) is a mnemonic for six items that describe use of drugs to relax, use of drugs when alone, driving using drugs or riding with a drug using driver, family or friends concern about drug use, and experiencing negative consequences of drinking or use of drugs. The CRAFFT has been found to have good discriminative properties for determining the presence of substance use disorders among 14–18 year old adolescents in primary care (Knight et al., 2002).
The 4-item Fast Alcohol Screening Test (FAST), developed by Hodgson and colleagues (2002) in an Accident and Emergency Department using items borrowed from the AUDIT (see section 2.5 for item descriptions). The FAST was found to be 93% sensitive and 88% specific for identifying alcohol “misuse” when a cut-point of 3 or higher is used.
Our own previous work identified a 5-item screening instrument based on selected items from the AUDIT, CRAFFT, and CAGE called the RUFT-Cut. The RUFT-Cut performed as well as the full scale AUDIT (sensitivity = 82%, specificity = 78%; Kelly et al, 2004). The RUFT-Cut was validated in a small sample, however, and these findings were considered preliminary. The current study uses a sample size that increases the original sample by 95%.
Other research efforts using a minimal number of questions have found that such very brief screens can still be sensitive for identifying patients with alcohol use disorders, but may sacrifice some degree of specificity for identifying non-cases (Canagasaby & Vinson, 2005; Dawson et al., 2005; Vinson et al., 2007). Vinson and colleagues (2005), for example, found over 90% sensitivity but only 77% specificity for identifying AUD cases using just two-items from the larger set used to define DSM-IV alcohol abuse or dependence, specifically, “recurrent drinking in hazardous situations” and “drinking more tan intended, or over a longer period than intended.”
Although many efforts to develop screening instruments have included young adult patients (aged 18–24 years), few have focused on young adult under-aged drinkers aged 18–20 years treated in emergency departments. Nationally, 89,000 young adults between 18 and 20 years of age were treated in ED for alcohol-related illness or injury in the last six months of 2005 (Drug Abuse Warning Network, 2007). Research shows that the earlier young patients who are experiencing AUD are identified, the more quickly treatment is provided and negative outcomes are prevented in this high-risk population (Godley and White, 2005). Furthermore, cost-effectiveness research indicates that intervention is beneficial in primary care clinics where specific sub-groups such as patients with mild to moderate alcohol abuse can be efficiently targeted (Chisholm et al., 2004).
Efforts for identifying alcohol-related problems in EDs often involve a brief intervention component for reducing use (e.g., Monti et al., 1999). Such efforts often include assessment of what is considered hazardous use or risk drinking, i.e., males drinking more than 14 drinks a week, females drinking more than 7 drinks, or males drinking more than 4 drinks at a time once a month or more, females drinking more than 3 drinks at a time once a month or more (US Department of Health and Human Services, 2005). Our project did not include conducting brief treatment in the emergency department. Rather it consisted of collecting screening data in the ED with recommendations for a full psychiatric evaluation within the next week. Because we were not providing brief interventions in the ED we did not focus on hazardous or risk drinking. Conversely, because the feedback we provided to the participant at the time of the follow-up study was related to the findings on the SCID-IV (Spitzer et al, 1992), we did focus on assessment of alcohol use disorders.
The objective of the current study is to test the utility of six very brief screening instruments for identifying AUD in a sample of 181 young adults in the hectic environment of an emergency department. The instruments included in this study are the RUFT-Cut, the CRAFFT, the FAST, the RAPS4-Q, the AUDIT-C, and the DSM-IV-2-Item Scale.
2.0 Materials and Methods
2.1 Emergency Department Procedures
The study protocol was approved by the University of Pittsburgh Institutional Review Board. Participants were recruited at two ED on weekend nights (Friday-Saturday and Saturday-Sunday) from 3 PM to 7AM. Both ED are within a multi-hospital university medical system and serve as regional resource trauma centers, i.e., centers approved by the Pennsylvania Trauma Systems Foundation as Level-1 facilities caring for the most severely injured patients. Inclusion criteria for patients in the study consisted of: 1) age 12 through 20 years (inclusive); and 2) clearance by medical staff to participate. Exclusion criteria were: 1) Glasgow Coma Score < 15 (Jennet & Bond, 1975), i.e., no serious head injury; 2) patient not accompanied by parent or legal guardian (if under 18 years of age) or patient admitted due to suspected child abuse or neglect; or 3) patient unable to read and complete a self-report questionnaire.
Research technicians who were not ED medical personnel staffed the ED and reviewed admission information for patients meeting the above age criterion. The technicians approached ED nurses regarding the potential eligibility of patients. Eligible patients (or the parents of eligible patients) were approached first by the nurse to determine their interest in learning about the study. Interested patients were then approached by the research technician to obtain written informed consent prior to performing any research procedures. Intoxicated patients who were not oriented to time and place, or who could not explain the major risks of the study following the informed consent process, were excluded from participation (n=8).
The ED study involved completion of a questionnaire containing five brief alcohol screening instruments. Findings on the performance of some of these instruments have been published elsewhere (see Kelly and Donovan, 2001; Kelly et al., 2002; Kelly et al., 2004). The screening instruments were kept together as item sets as much as possible except where logic dictated otherwise. For example, RAPS4-QF items were placed immediately before AUDIT items that request more detailed information on the frequency of a behavior within the past year because it is logical to ask the RAPS4QF “yes/no” item before the AUDIT item. This is similar to the method used by Cherpitel (1998) for integrating multiple instruments in a single questionnaire.
The last question on the ED questionnaire asked if participants were willing to be contacted to learn about a follow-up study, and contact information was taken from those who agreed. Medical staff members were not informed of any research results, and research data were not entered into participants' medical records. Participants were given a $10 gift certificate as compensation for participation.
2.2 Sample in the ED
Nine hundred-eighty five patients aged 12–20 were screened. Two hundred thirty-two patients (23.4%) could not be approached due to the severity of their illness or injury. Another 137 patients (13.8%) were not approached regarding participation for several other reasons, including the following: 1) absence of a parent to provide consent for participation of a minor child, n=46 (38%); 2) discharge from the ED before they could be recurited, n=42 (34%); or 3) various other reasons, e.g., illiteracy, lack of privacy for the interview, or failure of the medical staff to introduce the study to the patient, n=34 (28%). Data that specify why 15 patients were not approached are missing.
2.3 Participants in the ED
Six hundred-sixteen patients were approached in the ED, and 419 (68%) agreed to participate in the study. This participation rate is comparable to similar studies conducted in EDs (see Cherpitel & Bazargan, 2003; Longabaugh et al., 2001; Monti et al., 1999). There were no significant gender or racial group differences between participants and patients who refused to participate. However, participants were older than non-participants (18.8±1.6 years vs. 18.0±2.0 years, respectively; t=5.0, df=613, p<.001). Whereas 72% (360 of 499) of the patients aged 18 years and over who were approached consented to participate, only half (59 of 117) of the parents of minor patients consented to their child’s participation. This tendency for parents to refuse to allow their minor children to participate in studies of alcohol use has been noted in other emergency department studies as well (Gregor et al., 2003). Consistent with our inclusion criteria, the sample is comprised of patients who were not severely ill or injured. Only 11 of the participants (less than 3%) were admitted to the hospital following their ED treatment.
2.4 Sample for the Follow-Up Study Outside of the ED
Of the 419 patients who participated in the ED research study, 340 (81%) also agreed to be contacted regarding participation in a follow-up study. Of these, 234 (69%) participated in the follow-up study which included an evaluation for DSM-IV defined psychiatric disorders (APA, 1994). These interviews took place at the Pittsburgh Adolescent Alcohol Research Center (PAARC). There were no significant differences on age, gender, or racial/ethnic group between patients who participated in the ED study only and those who participated in both the ED study and the follow-up study. Although we did not systematically press patients to tell us why they declined to participate, interviewers often asked patients and many responded, or spontaneously stated, that they did not have enough time, or they did not want to take the time to participate.
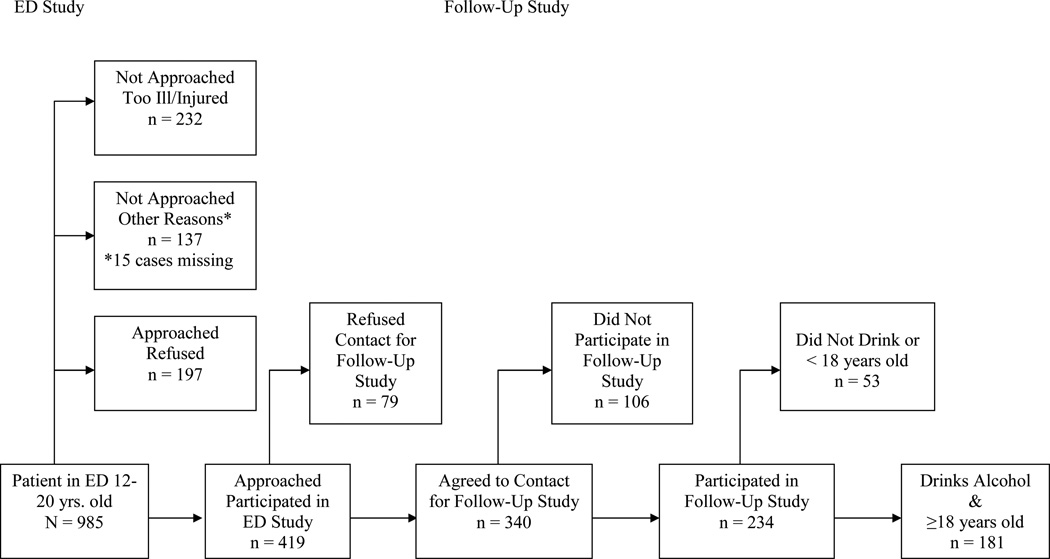
Of the 234 participants who were interviewed for the follow-up study, 39 (17%) had never used alcohol and were therefore not included in the following analyses. It was necessary to remove non-drinkers from these analyses because including them would have artificially increased the specificity of the tested instruments. Of the remaining 195 participants who reported that they drink alcohol, all but 14 participants were aged 18 or older. Epidemiologic research finds that adolescents drink substantially less than young adults (see Johnston et al. 2005). These 14 younger adolescents were excluded because it would be difficult to agree that results based on a small number of 12–17 year olds would generalize to the larger population. Instead, we restricted the present analyses to the 181, 18–20 year old participants who use alcohol. With the close proximity of the participating ED to several college campuses, the majority (89%) of our 18–20 year old participants were college students. Figure 1 provides a schematic of the recruitment process for this study.
Figure 1.
Patient Flow Chart for ED Study and Follow-Up Study
2.5 Brief Screens for Alcohol Use Disorders-Emergency Department
The RAPS4-QF and the FAST use similar items from the AUDIT. The RAPS4 (Cherpitel, 2000) assesses feelings of guilt or Remorse due to drinking, drinking related Amnesia, role failure as a result of drinking (Performance), and drinking first thing in the morning (Starter). The RAPS4-QF (scale range=0–6) also includes one item on binge drinking at least once (Q) in the last year and one item on drinking at least once a month (F) in the last year (Cherpitel, 2002). In order to avoid presenting the same items twice, for the current study, two AUDIT items were re-scored to represent these items from the RAPS4-QF. The dichotomy on frequency (AUDIT Item 1) is slightly different from that in the original RAPS4-QF items because the AUDIT item assesses drinking monthly or less often versus more than once a month. AUDIT item 3 was dichotomized to indicate whether participants drank six or more drinks on at least one occasion in the last year or less than this.
The FAST consists of: AUDIT Item 3, “How often do you have six or more drinks on one occasion?”; AUDIT Item 5, “How often during the last year have you failed to do what was normally expected of you because of drinking?”; AUDIT Item 8, “How often during the last year were you unable to remember what happened the night before because you had been drinking?”; and AUDIT Item 10, “Has a relative or friend, or a doctor or other health care worker been concerned about your drinking or suggested you cut down?” Due to the young age of our sample, we used the FAST scale described in Hodgson and colleagues (2002). The modifications made to the questions in Hodgson and colleagues (2003) regarding binge drinking (male binge drinking =8+ drinks), sets an inappropriately high threshold for binge drinking in this age group. Furthermore, again due to the younger age of our sample, we did not ask about the frequency with which family, friends, or health care workers showed concern about drinking in the last year, as suggested in Hodgson and colleagues (2003). We scored this positively for any occasion that such concern was voiced in the past because it should count as a risk at any time it is brought up in the life of an underage drinker. The FAST was scored using the 16-point scoring method, described in Hodgson et al. (2003).
The RUFT-Cut (Kelly et al., 2004) was developed by combining 2 items from the AUDIT (Saunders et al. 1993), 2 items from the CRAFFT (Knight et al., 1999), and 1 item from the CAGE (Ewing, 1984) that were predictive of alcohol abuse or dependence in a sample of 15–20 year old emergency department patients. The RUFT-Cut consists of Riding with an intoxicated driver, being Unable to stop drinking, Family, friends, health care worker showing concern, getting into Trouble while drinking, and feeling the need to Cut-down. Two items use a 5-point scale and the other three use a 0–1 scale (scale range=0–11. The RUFT-Cut was most efficient at a cut-score of 3 in the original study (82% sensitivity; 78% specificity).
The CRAFFT (Knight et al., 1999) is a mnemonic for: 1) driving or riding in a Car with an intoxicated driver; 2) using drugs or alcohol to Relax; 3) using drugs or alcohol while Alone; 4) Forgetting things while using; 5) having Friends or family say you should cut down; and 6) getting into Trouble while using drugs or alcohol. The CRAFFT has been found to have good discriminative properties for determining the presence of substance use disorders among 14–18 year old adolescents in primary care (Knight et al., 2002).
As presented above, two DSM-IV items, the alcohol abuse item reflecting drinking in hazardous situations and the alcohol dependence item reflecting drinking more or over a longer period than intended, were coded as present (range 0–2) if the patient reported them in the diagnostic interview conducted as part of the follow-up study. Vinson et al. (2007) have shown that these two items are highly predictive of a diagnosis of either alcohol abuse or alcohol dependence.
2.6 Follow-Up Study-PAARC
A modified version of the Substance Use Disorders section of the Structured Clinical Interview for DSM-IV disorders (SCID) was used to determine the presence of an AUD among participants (Spitzer et al., 1992; Martin et al., 1995). The interviews were administered by the first author or by Masters-level clinical assessors who achieved very high inter-rater reliability for detection of AUD (κ=0.92, Martin et al., 2000). The clinical assessors were kept blind regarding the reasons participants were treated in the emergency department. Diagnoses were formulated in clinical consensus conferences chaired by two psychiatrists (one Board-certified in child psychiatry [OGB] and one Board-certified in addiction psychiatry [JRC]).
In addition to the diagnostic interview, the follow-up study included completion of some self-report questionnaires, including questionnaires on risk-taking activities, family functioning, self-esteem, impulsiveness, and sensation seeking. Other than the diagnostic data from the SCID interview, no data from the follow-up study were used in this report.
2.7 Data Analysis
The scale properties of the six alcohol screening measures were determined using the RELIABILITIES procedure in SPSS 11.0, including alpha estimates of the inter-item consistency of the scales (Cronbach, 1951) and total scale score means and standard deviations. MedCalc (www.medcalc.be) was used to compute Receiver Operator Characteristic (ROC) curves and to determine the sensitivity (percentage of “true positives,” participants who screened positive diagnosed with an AUD) and specificity (percentage of “true negatives,” participants who screened negative and not diagnosed with an AUD) for each scale at various cut-points. The ROC curves for the six brief screens were compared to determine whether they were significantly different using the method of Hanley and McNeil (1983) for both correlated samples (i.e., multiple tests within the same sample) and independent samples (e.g., gender differences).
For this study, any current (i.e., past 6 months) DSM-IV defined AUD diagnosis, i.e., either alcohol abuse or alcohol dependence, was treated as a single dichotomous criterion.
3.0 Results
The present analyses focus on the data from one hundred eighty-one participants between the ages of 18.0 and 20.9 years of age who use alcohol and who were treated in emergency department. Sixty-five participants (36%) were diagnosed with current alcohol abuse or dependence. Higher rates of AUD were found among males than females (46% vs. 22% respectively; χ2 =11.1, df=1, p<.002). We found no significant difference between college students and non-college students on rates of AUD (36% vs. 32%, respectively; χ2=0.2, df=1, p=.68).
3.1 Comparison of Screening Instruments
The mean(SD) for the screening instruments were as follows: AUDIT-C = 5.0(2.7); CRAFFT = 2.3(1.7); FAST = 3.4(3.2); RAPS4-QF = 2.5(1.5); DSM-IV Items = 0.50(0.7); and RUFT-Cut = 3.0(2.7). The internal consistency alphas of the scales were as follows: AUDIT-C= .81; RAPS4-QF= .68; FAST= .64; RUFT-Cut= .64; CRAFFT=.61; and DSM-IV Items=.41.
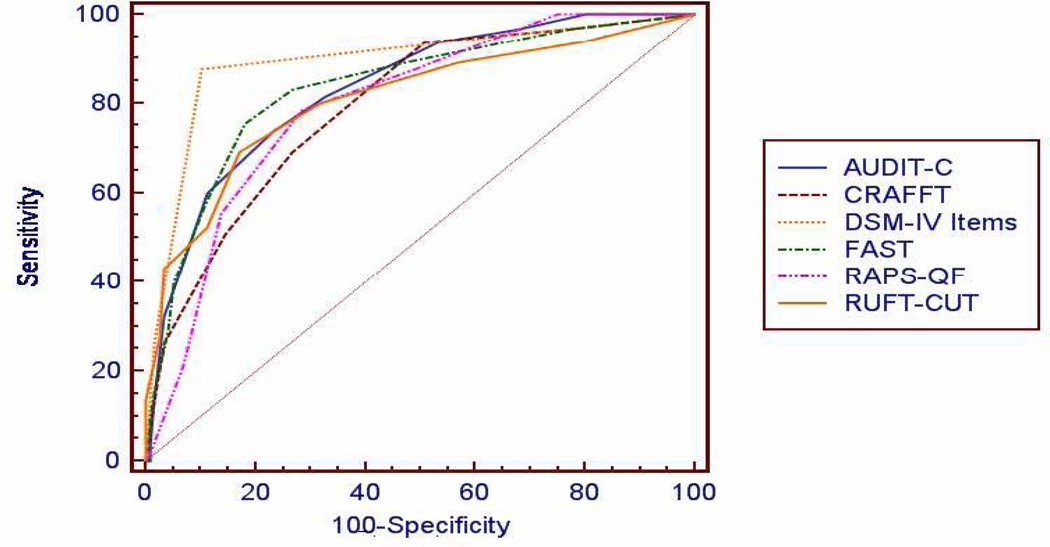
Receiver Operator Characteristics (ROC) analyses indicated that the DSM-IV Item scale had the highest Area Under the Curve (AUC=.89, SE=0.03), followed by the FAST and AUDIT-C (AUC=.83, SE=0.03 for both), RUFT-Cut (AUC=.81, SE=0.04), RAPS4-QF (AUC=.80, SE=0.04) and CRAFFT (AUC=.79, SE=0.04). Figure 2 presents total sample ROC curves for each of these instruments.
Figure 2.
ROC Curves for the AUDIT-C, the CRAFFT, the FAST, the RUFT-Cut, the RAPS-QF, and the DSM-IV 2-Item Scale
Table 1 presents the sensitivity and specificity of each of the instruments for predicting a diagnosis of AUD (either abuse or dependence) at several different cut-points for the total sample as well as for each gender. Cut-points for the “best” performance are indicated by a caret (>) and are based on a joint consideration of both optimum sensitivity and specificity levels for each instrument. The best cut-point for the AUDIT-C was 6 for males and 5 for females. The best cut-point was 3 for the FAST, the CRAFFT, the RUFT-Cut and the RAPS-QF and 1 for the DSM IV 2-Item Scale for both genders.
Table 1.
Sensitivity and Specificity of the AUDIT-C, the FAST, the RAPS4QF, the RUFT-Cut, the CRAFFT, and the DSM-IV-2 Scale for Classifying Alcohol Use Disorder at Various Cut-Points Among 181, 18–20 Year-Olds Treated in Emergency Departments
| Total Sample (n=181) | Males (n=104) | Females (n=77) | |||||
|---|---|---|---|---|---|---|---|
| Cut-point | Sensitivity | Specificity | Sensitivity | Specificity | Sensitivity | Specificity | |
| AUDIT-C | 3 | .97 | .32 | .96 | .23 | 1.00 | .40 |
| 4 | .94 | .47 | .94 | .36 | .94 | .57 | |
| 5 | .82 | .67 | .83 | .55 | >.77 | .78 | |
| >6 | .74 | .77 | >.77 | .68 | .65 | .85 | |
| 7 | .60 | .89 | .65 | .86 | .47 | .92 | |
| FAST | 2 | .89 | .53 | .88 | .39 | .94 | .65 |
| >3 | .83 | .73 | .79 | .68 | .94 | .78 | |
| 4 | .75 | .82 | .73 | .75 | .82 | .88 | |
| 5 | .59 | .89 | .54 | .86 | .71 | .92 | |
| RAPS4-QF | 1 | 1.00 | .25 | 1.00 | .14 | 1.00 | .30 |
| 2 | .87 | .51 | .85 | .43 | .94 | .58 | |
| >3 | .79 | .72 | .79 | .66 | .77 | .77 | |
| 4 | .55 | .86 | .54 | .82 | .59 | .90 | |
| RUFT-Cut | 1 | .94 | .21 | .92 | .12 | 1.00 | .28 |
| 2 | .89 | .43 | .88 | .37 | .94 | .48 | |
| >3 | .80 | .68 | .77 | .68 | .88 | .68 | |
| 4 | .69 | .83 | .69 | .79 | .71 | .87 | |
| CRAFFT | 1 | .97 | .22 | .96 | .16 | 1.00 | .28 |
| 2 | .94 | .49 | .94 | .44 | .94 | .52 | |
| >3 | .69 | .73 | .71 | .68 | .65 | .78 | |
| 4 | .51 | .85 | .52 | .82 | .47 | .88 | |
| DSM-IV-2 | >1 | .88 | .90 | .85 | .87 | .94 | .92 |
| 2 | .26 | .98 | .25 | .82 | .29 | .98 | |
> Indicates cut-point at which the instrument performs best for classifying AUD.
Pairwise comparisons of the ROC curves found that the DSM-IV 2 Item Scale performed significantly better than the CRAFFT (AUC difference = 0.100, SE=0.42, p=<.02), the RAPSQF (AUC difference = 0.97, SE=0.42, p=<.03), and the RUFT-Cut (AUC difference = 0.084, SE=0.42, p=<.05). No other comparisons were significantly different.
No significant gender differences were found for the performance of the AUDIT-C (male AUC=.80, female AUC=.86, SE of difference=.07, z=0.9, p=.38), the CRAFFT (male AUC=.76, female AUC=.82, SE of the difference=.09, z=0.7, p=.46), the DSM 2-Item Scale (male AUC=.87, female AUC=.93, SE of the difference =.06, z=1.1, p=.29), the RAPSQF (male AUC=.76, female AUC=.84, SE of the difference =.08, z=1.1, p=.29), or the RUFT-Cut (male AUC=.76, female AUC=.89, SE of the difference=.07, p=.08). The FAST performed marginally better among females in this sample (male AUC=.78, female AUC=.92, SE of the difference =.07, z=2.0, p=.05).
4.0 Discussion
In the current study of brief screens for AUD, the shortest screen (i.e., two-item DSM-IV test) performed best in identifying young adult patients in the ED who have an AUD and those who do not. While this may seem counterintuitive, the two-item DSM-IV scale has the greatest conceptual overlap with the diagnosis of AUD among adolescents and young adults. The dependence item of “drinking larger amounts or drinking over longer periods than intended,” for example, reflects a lack of control over one’s own drinking, and is one of two DSM-defined AUD symptoms most often endorsed by adolescents who are diagnosed with an alcohol use disorder (tolerance for alcohol is the other) (Chung et al., 2005). Our own work in the ED found that drinking larger/longer is associated with being treated for an alcohol-related injury, and that males who drink larger/longer are at particularly high risk for an alcohol-related injury (Kelly et al., 2005).
The current findings are consistent with those of Vinson and colleagues (2005) who also used the 2-Item DSM-IV scale to predict AUD diagnosis, thereby, increasing the applicability of using this scale for screening young adults in emergency departments. The method in the present research includes some degree of circularity between the predictor and the criterion and this circularity may “stack the deck” in favor of this brief two-item screen. Nevertheless, prevention of recurrent injury demands that screening for AUD be conducted in emergency departments and such screening is burdensome. It is, therefore, critically important to advise clinicians in emergency departments on the briefest, valid screening instrument available for diagnosing alcohol use disorders. While our findings suggest that a two-item instrument is a useful indicator of AUD, it is important to note that our sample included only participants who drink alcohol and, in practice, it is necessary to ask the most important screening question, i.e., “Do you drink alcohol?” before proceeding to the two-item scale.
The AUDIT-C likely performed well in this young sample despite its focus on levels of alcohol consumption rather than negative consequences of drinking. This is not surprising because Hill and colleagues (2000) found that higher levels of binge drinking during adolescence are predictive of later AUD, even when it does not begin until late adolescence. Binge drinking is associated with very high rates of negative outcomes such as hangovers, withdrawal-related illness, and fights or arguments among adolescents and young adults (Windle, 2003), any one of which elevates the potential need for emergency treatment.
In studies using the CRAFFT, Knight and colleagues (1999; 2003) found that “riding with a driver who is using drugs or alcohol” is the single most important question for assessing problematic substance use among adolescents. This behavior was associated with using alcohol in dangerous situations, and under the current DSM-IV nosological system recurrent alcohol use in dangerous situations alone fulfills the criterion for a diagnosis of alcohol abuse. Low levels of endorsement (<25%) of two of the CRAFFT items, “using alcohol while alone” and “family and friends concerned,” may have contributed to the lower level of criterion-validity found in the current study for this instrument.
The FAST performed as well as the AUDIT-C in identifying AUD cases (sensitivity=.85) but performed less well in determining AUD non-cases (specificity=.73). It also takes more time to administer and is more difficult to score than the AUDIT-C because its preferred scoring system uses a 0–16 score range (Hodgson et al., 2003).
The RAPS4-QF and RUFT-Cut did not perform well enough in the present study to justify their use with adolescents and young adults in health care settings such as ED, where accuracy and brevity are of paramount importance. The RAPS4-QF may not have performed well in this sample because its items require a longer history of problem alcohol use than is typically experienced by adolescents and young adults. For example, only 25% of the alcohol-using adolescents in this sample had ever experienced alcohol-related role failure, and just 11% indicated that this had occurred monthly or more often. Even more salient in this regard, less than 7% (n=13) of this young adult sample reported ever having had a drink first thing in the morning. Drinking in the morning most often reflects drinking to avoid withdrawal, a sign of severe alcohol dependence.
The RUFT-Cut also includes two items that are symptomatic of more severe problem alcohol use than is often found among adolescents and young adults (inability to stop drinking and feeling the need to cut-down). The smaller sample and/or use of a different outcome variable (lifetime AUD rather than the present focus on current AUD) may have contributed to their inclusion in our earlier study (Kelly et al., 2004).
4.1 Limitations
One limitation of this study is that it was conducted in a single ED system in the Northeast, as findings on problematic drinking can vary by region and even by individual ED populations (Cherpitel & Clark, 1995). Experienced investigators have noted that the population under investigation is an important consideration in choosing an appropriate screening instrument (Cherpitel, 1998; Maisto et al., 1995). Low numbers of African-American participants and other minority participants precluded examination of racial differences in the performance of the instruments. The present findings also may not generalize beyond the population of young adults treated in emergency departments on weekends. Furthermore, although ED participants who agreed to the follow-up interview were not different on age, race, and gender from those who declined, it is possible that they differ on some unspecified variable(s), thereby introducing some selection bias. We presented some anecdotal evidence that the only difference between participants in our ED–only study and participants in both the ED and the follow-up study is that participants who declined the follow-up study did not want to take the time to participate.
Our method included embedding several screening instruments into one single questionnaire. Our method kept screening items together as much as possible, except where logic dictated otherwise. This procedure has been used by other investigators (Cherpitel, 1998) for integrating multiple instruments in a single questionnaire. However, it is possible that this method would not reproduce results obtained by administration of each instrument in a single, unique format because responses to items from one instrument may contribute to variation in responses to items from other instruments.
Another possible limitation is related to the timing of different aspects of the study. Since the full psychiatric evaluation was not conducted at the point of care in the ED, it is possible that factors between the ED visit and the follow-up interview, including the ED visit itself, might have caused the participant to respond differently in the diagnostic interview. If, for example, the ED visit constituted a “teachable moment” (Leist & Kristofco, 1990) leading to a reduction in drinking behavior, this may have attenuated the relationship of the screening instruments to AUD, making the current results more conservative estimates of that relationship.
Even considering certain study limitations, the current findings are important for determining the most efficient method of diagnosing AUD in the emergency department. Research continues to consistently find that brief treatment is effective for mild to moderate alcohol problems in ED and primary care settings (e.g., Ockene et al., 1999; Senft et al., 1997; D’Onofrio et al., 2005). Therefore, the paradigm for screening and treating alcohol problems in ED is shifting from that of research-oriented substance abuse specialists providing such interventions (Monti et al., 1999; Longabaugh et al., 2003) to the training of ED personnel and other health care providers who can screen and provide brief treatment for their own patients (D’Onofrio et al., 2005; US DHHS, 2005). The major obstacle to this shift is that ED medical personnel believe that too much time is required to screen and provide brief treatment of alcohol use disorders (Graham et al., 2000). Busy ED practitioners are more likely to screen patients and possibly provide treatment only if both are truly brief. Reviews of treatment efforts for alcohol problems in the ED have reported that effective interventions can be delivered in less than 30 minutes (D’Onofrio and Degutis, 2002). In fact, effective interventions of less than 10 minutes have been developed for use with hazardous drinkers in emergency departments (D’Onofrio et al., 2005).
Nevertheless, it is important to note that brief interventions alone are not effective for treating alcohol dependence and severe alcohol abuse. Positive results on screening instruments for more severe alcohol use disorders generally indicate the need for treatment by a specialist. Furthermore, sub-threshold levels of misuse may also indicate the need for treatment outside of the emergency department. For example, by themselves, neither recurrent binge-drinking nor drinking larger amounts or over longer periods of time reach the threshold for an alcohol use disorder. However, each of these is a serious problem and represents considerable risk for illness or injury. The decision to limit treatment to those interventions that can be conducted in the ED versus referring patients for specialized treatment elsewhere should not rest solely on the results of any brief screening instrument. It should also reflect sound clinical judgment. Knowledgeable practitioners should err on the side of conservatism and refer patients to a specialist whenever they believe that a brief intervention is not adequate for the level of alcohol problems identified through the screening and other treatment-related findings.
In this regard, the DSM-IV Two-Item scale is a brief screening instrument for current alcohol use disorder that may help ED personnel to quickly identify which older adolescents are in need of further evaluation for the presence of an alcohol use disorder. Future research should focus on its use in ED and other primary care settings with larger and more diverse samples of adolescents and young adults.
Acknowledgments
This work was supported by NIAAA Grant No. K08-AA-00280.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen JP, Litten RZ, Fertig JB, Babor T. A review of research on the Alcohol Use Disorders Identification Test (AUDIT) Alcoholism: Clinical & Experimental Research. 1997;21:613–619. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Psychiatric Disorders, (1994) (DSM-IV) 4th ed. Washington D.C.: American Psychiatric Association; 1994. [Google Scholar]
- Canagasaby A, Vinson DC. Screening for hazardous or harmful drinking using one or two quantity-frequency questions. Alcohol & Alcoholism. 2007;40:208–213. doi: 10.1093/alcalc/agh156. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Screening for alcohol problems in the emergency room: A rapid alcohol problems screen. Drug and Alcohol Dependence. 1995;40:133–137. doi: 10.1016/0376-8716(95)01199-4. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Performance of screening instruments for identifying alcohol dependence in the general population, compared with clinical populations. Alcoholism: Clinical & Experimental Research. 1998;22:1399–1404. doi: 10.1111/j.1530-0277.1998.tb03926.x. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. A brief screening instrument for problem drinking in the emergency room: the RAPS4, Rapid Alcohol Problems Screen. Journal of Studies on Alcohol. 2000;61:447–449. doi: 10.15288/jsa.2000.61.447. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Screening for alcohol problems in the U.S. general population: Comparison of the CAGE, RAPS4, and RAPS4-QF by gender, ethnicity, and service utilization. Alcoholism: Clinical & Experimental Research. 2002;26:1686–1691. doi: 10.1097/01.ALC.0000036300.26619.78. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Bazargan S. Screening for alcohol problems: Comparison of the AUDIT, RAPS4 and RAPS4-QF among African-American and Hispanic patients in an inner city emergency department. Drug and Alcohol Dependence. 2003;71:275–280. doi: 10.1016/s0376-8716(03)00140-6. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Clark WB. Ethnic differences in performance of screening instruments for identifying harmful drinking and alcohol dependence in the emergency room. Alcoholism: Clinical & Experimental Research. 1995;19:628–634. doi: 10.1111/j.1530-0277.1995.tb01559.x. [DOI] [PubMed] [Google Scholar]
- Chisholm D, Rehm J, Van Ommeren M, Monteiro M. Reducing the global burden of hazardous alcohol use: A comparative cost-effectiveness analysis. Journal of Studies on Alcohol. 2004;65:782–793. doi: 10.15288/jsa.2004.65.782. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS, Winters KC. Diagnosis, course, and assessment of alcohol abuse and dependence in adolescents. In: Galenter M, editor. Recent Developments in Alcoholism, Volume 17: Alcohol Problems in Adolescents and Young Adults: Epidemiology, Neurobiology, Prevention, Treatment. New York: Kluwer Academic/Plenum; 2005. pp. 5–27. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism: Clinical & Experimental Research. 2005;29:844–854. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operator characteristic curves: A non-parametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- D’Onofrio GD, Degutis LC. Preventive care in the emergency department: Screening and brief intervention for alcohol problems in the emergency department: A systematic review. Academy of Emergency Medicine. 2002;6:627–638. doi: 10.1111/j.1553-2712.2002.tb02304.x. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G, Pantalon MV, Degutis LC, Fiellin DA, O’Conner PG. Development and implementation of an emergency practitioner-performed brief intervention for hazardous and harmful drinkers in the emergency department. Alcoholism: Clinical & Experimental Research. 2005;12:249–256. doi: 10.1197/j.aem.2004.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drug Abuse Warning Network (DAWN) Alcohol-Related Emergency Department Visits. 2005 http://dawninfo.samhsa.gov/.
- Ewing JA. Detecting alcoholism – the CAGE questionnaire. Journal of the American Medical Association. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Godley MD, White WL. A brief history and some current dimensions of adolescent treatment in the United States. Recent Developments in Alcohol. 2005;17:367–382. doi: 10.1007/0-306-48626-1_17. [DOI] [PubMed] [Google Scholar]
- Graham DM, Maio RF, Blow FC, Hill EM. Emergency physician attitudes concerning intervention for alcohol abuse/dependence delivered in the emergency department: A brief report. Journal of Addictive Diseases. 2000;19:45–53. doi: 10.1300/J069v19n01_04. [DOI] [PubMed] [Google Scholar]
- Gregor MA, Shope JT, Blow FC, Maio RF, Weber JE, Nypaver MM. Feasibility of using an interactive laptop program in the emergency department to prevent alcohol misuse among adolescents. Annals of Emergency Medicine. 2003;42:276–284. doi: 10.1067/mem.2003.265. [DOI] [PubMed] [Google Scholar]
- Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristics curves derived from the same cases. Radiology. 1983;148:839–843. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- Hodgson RJ, Alwyn xT, John B, Thom B, Smith A. The FAST alcohol screening test. Alcohol and Alcoholism. 2002;37:61–66. doi: 10.1093/alcalc/37.1.61. [DOI] [PubMed] [Google Scholar]
- Hodgson R, Waller S, Thom B, Newcombe RG. Fast screening for alcohol misuse. Addictive Behaviors. 2003;28:1453–1463. doi: 10.1016/s0306-4603(02)00246-0. [DOI] [PubMed] [Google Scholar]
- Jennet B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Shulenburg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2004. Volume II: College Students and Adults Ages 19–45 (NIH Publication No. 05-5728) Bethesda, MD: National Institute on Drug Abuse; 2005. [Google Scholar]
- Kelly TM, Donovan JE. Confirmatory factor analyses of the Alcohol Use Disorders Identification Test (AUDIT) among adolescents treated in emergency departments. Journal of Studies on Alcohol. 2001;62:838–842. doi: 10.15288/jsa.2001.62.838. [DOI] [PubMed] [Google Scholar]
- Kelly TM, Donovan JE, Chung T, Cook RL, Delbridge TR. Alcohol use disorders among ED-treated older adolescents: A new brief screen (RUFT-Cut) using the AUDIT, CAGE, CRAFFT, and RAPS-QF. Alcoholism: Clinical & Experimental Research. 2004;28:746–753. doi: 10.1097/01.alc.0000125346.37075.85. [DOI] [PubMed] [Google Scholar]
- Kelly TM, Donovan JE, Cornelius JR, Bukstein OG, Delbridge TR, Kinnane JM. Alcohol use disorder symptoms and risk-taking behavior as predictors of alcohol-related medical events among young adults treated in emergency departments. Addictive Behaviors. 2005;30:1674–1689. doi: 10.1016/j.addbeh.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Kelly TM, Donovan JE, Kinnane JM, Taylor DM. A comparison of alcohol screening instruments among under-aged drinkers treated in emergency departments. Alcohol & Alcoholism. 2002;37:444–450. doi: 10.1093/alcalc/37.5.444. [DOI] [PubMed] [Google Scholar]
- Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shaffer HJ. A new brief screen for adolescent substance abuse. Archives of Pediatric & Adolescent Medicine. 1999;153:591–596. doi: 10.1001/archpedi.153.6.591. [DOI] [PubMed] [Google Scholar]
- Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Archives of Pediatric & Adolescent Medicine. 2002;156:607–614. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- Leist JC, Kristofco RE. The changing paradigm for continuing medical education: impact of information on the teachable moment. Bulletin of the Medical Library Association. 1990;78:172–179. [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Woolard RF, Nirenberg TD, Minugh AP, Becker B, Clifford PR, Carty K, Sparadeo F, Gogineni A. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Connors GJ, Allen JP. Contrasting self-report screens for alcohol problems: A review. Alcoholism: Clinical & Experimental Research. 1995;19:1510–1516. doi: 10.1111/j.1530-0277.1995.tb01015.x. [DOI] [PubMed] [Google Scholar]
- Martin CS, Kaczynski NA, Maisto SA, Bukstein OG, Moss HB. Patterns of DSM-IV alcohol abuse and dependence symptoms in adolescent drinkers. Journal of Studies on Alcohol. 1995;56:672–680. doi: 10.15288/jsa.1995.56.672. [DOI] [PubMed] [Google Scholar]
- Martin CS, Pollock NK, Bukstein OG, Lynch KG. Inter-rater reliability of the SCID alcohol and substance use disorders section among adolescents. Drug and Alcohol Dependence. 2000;59:173–176. doi: 10.1016/s0376-8716(99)00119-2. [DOI] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Woolard R, Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Ockene JK, Adams A, Hurley TG, Wheeler EV, Hebert JR. Brief physician-and nurse practitioner-delivered counsel high-risk drinkers: Does it work? Archives of Internal Medicine. 1999;159:2198–2205. doi: 10.1001/archinte.159.18.2198. [DOI] [PubMed] [Google Scholar]
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): A review of recent research. Alcoholism: Clinical & Experimental Research. 2002;26:272–279. [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fluente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Senft RA, Polen MR, Freeborn DK, Hollis JF. Brief intervention in a primary care setting for hazardous drinkers. American Journal of Preventive Medicine. 1997;13:464–470. [PubMed] [Google Scholar]
- Smith GT, McCarthy DM, Goldman MS. Self-reported drinking and alcohol-related problems among early adolescents: Dimensionality and validity over 24 months. Journal of Studies on Alcohol. 1995;56:383–394. doi: 10.15288/jsa.1995.56.383. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID) I: history, rationale, and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Helping patients who drink too much: A clinician’s guide. National Institute on Alcohol Abuse and Alcoholism; 2005. [Accessed: January 28, 2009]. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. [Google Scholar]
- Vida S. A computer program for non-parametric receiver operating characteristic analysis. Computer Methods and Programs in Biomedicine. 1993;40:95–101. doi: 10.1016/0169-2607(93)90004-5. [DOI] [PubMed] [Google Scholar]
- Vinson DC, Kruse RL, Seale JP. Simplifying alcohol assessment: two questions to identify alcohol use disorders. Alcohoisml: Clinical & Experimental Research. 2007;31:1392–1398. doi: 10.1111/j.1530-0277.2007.00440.x. [DOI] [PubMed] [Google Scholar]
- Windle M. Alcohol use among adolescents and young adults. Alcohol Research & Health. 2003;27:79–85. [PMC free article] [PubMed] [Google Scholar]