Abstract
Background
While knowledge has accumulated regarding health care seeking in several functional gastrointestinal disorders (FGIDs), little is know about health care seeking in those with bloating and distention. We aimed to identify predictors of health care seeking for bloating and distention.
Methods
The validated Talley Bowel Disease Questionnaire was mailed to a cohort selected at random from the population of Olmsted County, Minnesota; 2,259 subjects (53% females; mean age 62 yr) answered questions about bloating and distention. The complete medical record of each respondent was reviewed. Logistic regression was used to compare consulting for bloating and distention to consulting for other GI symptoms, and non-consulters.
Results
A total of 131 (6%) subjects in the community consulted a physician for bloating or distention. Older age (odds ratio(OR), 1.8; 95% confidence interval (CI): 1.5, 2.1), higher somatic symptom scores (OR, 2.0; CI: 1.4, 2.8), lower education level (OR, 2.7; CI: 1.2, 5.6), early satiety (OR, 2.0; CI: 1.1, 3.8), and abdominal pain (OR, 2.4; CI: 1.6, 3.7) were associated with people seeking health care for bloating or distention vs. non-consulters. Similarly, older age (OR, 1.4; CI: 1.2, 1.7), chronic constipation (OR, 2.0; CI: 1.2, 3.2) and visible distention (OR, 3.0; CI: 1.8, 4.9) had greater odds of presenting for bloating or distention compared to presenting for other GI symptoms; somatic symptoms were not a predictor (OR, 1.1; CI: 0.8, 1.5).
Conclusions
Factors that lead people to present for bloating and distention are similar to those for other GI symptoms visits; however, specific biologic rather than somatic features may predict visits for bloating and distention.
Keywords: Large intestine Organ-based, Abdominal pain Topics, Epidemiology Topics, Motility Topics
INTRODUCTION
A sensation of abdominal bloating and objective visible distention are common symptoms in the general population (1, 2). We have reported that 19% of the subjects in a US community experienced bloating, and about half of them believed this was accompanied by visible abdominal distension (3). Notably, Sandler et al (4) observed that more than 75% of patients with bloating and distention rated their symptoms as moderate to severe, and 54% of them reported these symptoms affected their daily activities; 43% had resorted to the use of medications. However, while much is known about health care seeking in several functional gastrointestinal disorders (FGIDs) (5–11), little is know about health care seeking behavior for bloating and distention.
Few studies have adequately separated bloating /distention (B/D) from irritable bowel syndrome (IBS) and other functional disorders (7, 12, 13). Lembo et al (14) reported that bloating-type symptoms were listed by 60% of patients with IBS as most bothersome, whereas only 29% rated abdominal pain as their most bothersome symptom; however, subjects with bloating-type predominant IBS had similar consulting behavior compared with those with pain-predominant IBS. Others also have observed that bloating and distention are common and particularly intrusive (14, 15); these complaints appear to negatively impact on quality of life(16), especially visible distention (17). However, factors that lead subjects to seek medical care especially for bloating and distention remain unclear and partly as a result, management remains unsatisfactory.
Lifetime rates of affective and anxiety disorders in the general population are higher in subjects with gastrointestinal symptoms compared with subjects without gastrointestinal symptoms (18). Heaton (19) reported that patients with IBS have truly abnormal bowel function (based on transit), though they were also more anxious and more depressed. Whether psychological factors including somatization drive health care seeking in IBS and functional dyspepsia remains controversial (20–24), even when symptom severity has been controlled for in the analysis (25). It has been reported that people who have gastrointestinal symptoms but do not trouble their doctors are less anxious and better at coping with the problems of life than consulters (24, 25). To our knowledge, no other studies have investigated the link between psychological factors and bloating/distention symptoms in consulters versus non-consulters in the general population, though bloating and distention may be closely related to somatization (3).
In the present study, we aimed to identify predictors of health care seeking for bloating and distention. We hypothesized that the predictors of healthcare seeking for bloating and distention are different from other GI syndromes, and in particular specific biologic rather than psychological features predict visits for bloating and distention. Further, we hypothesized that subjects with visible distention will seek more health care compared with those with bloating alone.
METHODS
This study was approved by the Institutional Review Board of Mayo Clinic. Subjects were randomly selected resident of Olmsted County, Minnesota. The Olmsted County, Minnesota is isolated from other urban centers and sociodemographicaly is similar to the United States white population (26). Over 95% of County residents receive their long term medical care from one of the two group practices (Mayo Medical Center and Olmsted Medical Center). Recorded diagnoses and surgical procedures are indexed, including the diagnoses made for outpatients seen in office or clinic consultations, emergency room visits or nursing home care, as well as the diagnoses recorded for hospital inpatients, at autopsy examination or on death certificates for more than 90 years. This system was further developed by Rochester Epidemiology Project (REP). Annually, over 80% of the entire population is attended by one or both of these two practices, and nearly everyone is seen at least once during any given 3–4 year period (26). The REP medical records linkage system provides what is essentially an enumeration of the population from which random samples can be drawn.
Survey Methodology
We have been conducting population based research in Olmsted County since 1988 (27–32). Using the REP, we have drawn random samples of county residents and mailed them valid GI symptom questionnaires on several occasions. We subsequently linked the data from these surveys together to create a database of survey responses from these questionnaires. In 2003, a total of 4,194 subjects who were a subset of the original random samples of Olmsted County residents were mailed a modified version of the validated bowel disease questionnaire (Talley-BDQ) (33, 34), The Talley-BDQ consists of 46 gastrointestinal symptoms, including separate questions to define bloating (Do you often feel bloated?) and visible distention (Do you often feel bloated and actually see your belly swell up?), plus a 17-item validated Somatic Symptom Checklist (SSC) (35), a measure of somatization. Subjects, who had died, moved from Olmsted County or had denied authorization for use of their medical records for research, as required by Minnesota law, were excluded from the subset.
A total of 2,298 (aged 18–95 years) subjects returned a completed questionnaire, giving an overall response rate of 55%. No significant differences were found between responders and non-responders in terms of sex, educational level, body mass index (BMI, kg m−2) and previous surgery (e.g. cholecystectomy); only a weak association with age was detected (Odds Ratio (OR) for responding, per year of age = 1.02 (95% confidence interval (95%CI):1.01–1.02) (36). The complete (inpatient and outpatient) medical records of the responders to this survey were abstracted using a standard form. A total of 2,259 responders answered the bloating/distention questions. The number of subjects with IBS, dyspepsia or chronic constipation in the survey period as previously defined were also collected(3). We used these data in the present study.
From both the questionnaire and chart review, we obtained data on health care seeking for GI symptoms; by chart review we collected information on physician visits including for abdominal bloating and distention: Subjects were considered consulters for bloating or distention if they had visited any physician for one or both these symptoms at least once in the medical history (including subjects with mixed GI symptomatology who reported bloating/distension). Subjects that had visited a physician for other GI symptoms (abdominal pain/discomfort, diarrhea, constipation, mucus, urgency, gas, borborygmi, vomiting, nausea, incontinence, heartburn, acid regurgitation, dysphagia, chest pain, change in bowel habits) at least once (aside from bloating and distention) in the medical history were considered as consulters for other GI symptoms. “Non-consulters” (reference group) were subjects that had not sought medical care for any GI symptoms documented in their medical history.
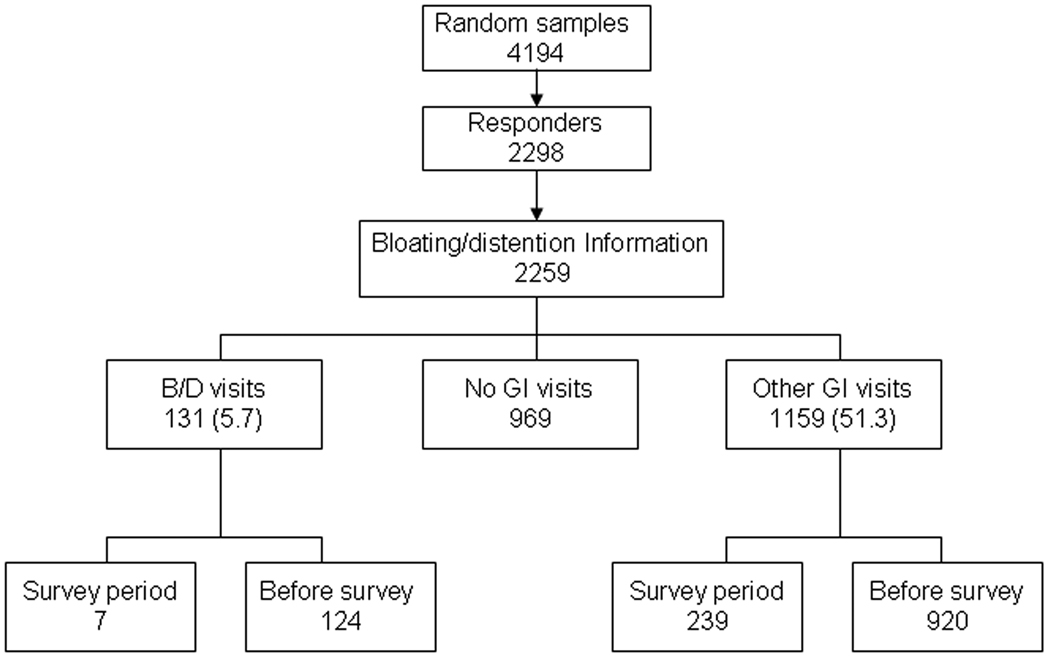
Thus, subjects (2,259 cases) were divided into three groups according to the type of consulting behavior as having bloating/distention visits (B/D visits, 131 cases), other GI visits (1,159 cases), and no GI visits (969 cases) based on the comprehensive and independent medical history. Figure 1 illustrates the sample method and the number and percentage of persons who consulted a physician for bloating and distention or other GI symptoms in the medical history and in the previous 12 months (survey period). Predictors of visit type that were considered included age, gender, somatic symptom checklist (SSC) score, marital status, educational level, current smoking (Yes/No), alcohol use (Yes/No), GI symptoms (chronic diarrhea, chronic constipation, heartburn, early satiety, loss of appetite, vomiting, nausea, blood in stools, chest pain), abdominal pain severity and frequency, site of bloating, and past abdominal surgery, using both questionnaire and chart review data.
Figure 1.
Flow chart of sampling techniques used in the study.
Statistical Analysis
A summary of demographics was compiled for the three groups (consulters for bloating/distention, consulters for other GI symptoms and those with no GI visits). Quantitative data are expressed as mean ± standard error and categorical data summarized as proportions (%).
Polychotomous logistic regression models (generalized logit link function) were used to assess the potential predictors of type of health care visit (i.e. a three category dependent variable). These models were used to estimate the odds for bloating/distention visits and for other GI visits (each compared to no GI visits) and for bloating/distension visits compared to other GI visits. The odds ratios (and corresponding 95% Confidence Intervals) of each potential predictor were estimated in separate logistic regression models from the corresponding coefficients in the model, in each case adjusting for age, gender, SSC score and bloating/distension symptom status as reported on the questionnaire. A two-sided α level of 0.05 was used to assess statistical significance.
RESULTS
Demographic Data
Table 1 illustrates the distribution of demographic characteristics across the study subjects with bloating and distention visits, other GI visits and no GI visits in the medical charts. There was no significant association of group status with gender, though age (mean± standard deviation SD: 68 ± 11, 64±12, 60 ±12, respectively), and less so, SSC scores (mean± SD: 0.7 ±0.6, 0.7 ±0.5, 0.5 ±0.5, respectively), were associated with group status.
Table 1.
Descriptive information for consulting behavior in n=2259 subjects in whom bloating/distention symptom questionnaire responses were obtained
| Characteristic |
Total N=2259 |
Bloating/distention visits N=131 % (n) |
Other GI visits N=1159 % (n) |
No GI visits N=969 % (n) |
|---|---|---|---|---|
| Age | <50 (n=418) | 2.6 (11) | 43.3 (181) | 54.1 (226) |
| >=50 (n=1841) | 6.5 (120) | 53.1 (978) | 40.4 (743) | |
| SSC | < 0.47 (n=1061) | 4.5 (48) | 45.9 (488) | 49.6 (528) |
| >= 0.47 (n=1112) | 6.8 (76) | 57.3 (637) | 35.9 (399) | |
| Gender | Male (n=1071) | 5.0 (54) | 49.9 (534) | 45.1 (483) |
| Female (n=1188) | 6.5 (77) | 52.6 (625) | 40.9 (486) | |
| Married | Yes(n=1788) | 5.6 (100) | 50.8 (908) | 43.6 (780) |
| No (n=471) | 6.6 (31) | 53.3 (251) | 40.1 (189) | |
| Current smoker | Yes (n=168) | 6.5 (11) | 53.6 (90) | 39.9 (67) |
| No (n=2091) | 5.7 (120) | 51.1 (1069) | 43.1 (902) | |
| Current alcohol user | Yes (n=1028) | 6.2 (64) | 49.8 (512) | 44.0 (452) |
| No (n=1231) | 5.4 (67) | 52.6 (647) | 42.0 (517) | |
| Education | < high school (n=123) | 12.2 (15) | 68.3 (84) | 19.5 (24) |
| High school or some college (n=1195) | 6.3 (75) | 53.6 (640) | 40.2 (480) | |
| College or professional training (n=919) | 3.9 (36) | 46.4 (426) | 49.7 (457) | |
| Chronic diarrhea | n=332 | 6.0 (20) | 55.1 (183) | 38.9 (129) |
| No chronic diarrhea | n=1910 | 5.8 (111) | 50.5 (965) | 43.7 (834) |
| Chronic constipation | n=238 | 10.5 (25) | 50.4 (120) | 39.1 (93) |
| No chronic constipation | n=2004 | 5.3 (106) | 51.3 (1028) | 43.4 (870) |
| Heartburn | n=366 | 7.1 (26) | 58.2 (213) | 34.7 (127) |
| No heartburn | n=1883 | 5.5 (104) | 49.8 (937) | 44.7 (842) |
| Early satiety | n=163 | 9.2 (15) | 62.6 (102) | 28.2 (46) |
| No early satiety | n=2092 | 5.5 (116) | 50.4 (1054) | 44.1 (922) |
| Loss of appetite | n=184 | 9.2 (17) | 53.8 (99) | 37.0 (68) |
| No loss of appetite | n=2068 | 5.5 (114) | 51.1 (1057) | 43.4 (897) |
| Vomiting | n=9 | 0 | 77.8 (7) | 22.2 (2) |
| No vomiting | n=2231 | 5.8 (129) | 51.1 (1141) | 43.1 (961) |
| Nausea | n=70 | 4.3 (3) | 65.7 (46) | 30.0 (21) |
| No nausea | n=2182 | 5.8 (127) | 50.8 (1108) | 43.4 (947) |
| Blood in stools | n=246 | 7.3 (18) | 54.5 (134) | 38.2 (94) |
| No blood in stools | n=2007 | 5.6 (113) | 50.9 (1022) | 43.5 (872) |
| Chest pain | n=98 | 8.2 (8) | 65.3 (64) | 26.5 (26) |
| No chest pain | n=2116 | 5.5 (116) | 50.4 (1067) | 44.1 (933) |
| Abdominal pain | n=761 | 7.5 (57) | 61.0 (464) | 31.5 (240) |
| No abdominal pain | n=1481 | 5.0 (74) | 46.2 (684) | 48.8 (723) |
| Severity abdominal pain | No/mild (n=1668) | 5.3 (89) | 47.7 (795) | 47.0 (784) |
| Moderate (n=482) | 7.3 (35) | 60.4 (291) | 32.3 (156) | |
| Severe (n=79) | 5.1 (4) | 68.3 (54) | 26.6 (21) | |
| Frequency of abdominal pain | No pain (n=1476) | 5.0 (73) | 46.0 (680) | 49.0 (723) |
| About Once a month (n=494) | 5.3 (26) | 58.9 (291) | 35.8 (177) | |
| About Once a week (n=110) | 11.8 (13) | 64.6 (71) | 23.6 (26) | |
| Several times a week/daily (n=146) | 11.0 (16) | 65.7 (96) | 23.3 (34) | |
| Bloating/Distention | Bloating alone (n=343) | 6.1 (21) | 59.5 (204) | 34.4 (118) |
| Distention +/− bloating (n=272) | 13.6 (37) | 55.5 (151) | 30.9 (84) | |
| No B/D (n=1644) | 4.4 (73) | 48.9 (804) | 46.7 (767) | |
| Site of bloating | No bloating or distention OR unspecified location (n=1378) | 4.4 (61) | 49.0 (675) | 46.6 (642) |
| Above the navel (n=243) | 9.5 (23) | 53.5 (130) | 37.0 (90) | |
| Below the navel (n=294) | 7.1 (21) | 54.1 (159) | 38.8 (114) | |
| Both above and below the navel (n=267) | 9.0 (24) | 59.9 (160) | 31.1 (83) |
Of the 2,259 subjects providing data on the questionnaire in response to the bloating and distension items, 131(6%) reported having seen a physician in the past for bloating and distention, while only 7 (0.3%) subjects indicated seeing a physician for bloating and distention in the prior year. On the other hand, 1,159 (51%) subjects reported having seen a physician for other GI symptoms in the past and 232 (10%) reported a visit for other GI symptoms occurred in the prior year. Of note, there were 73 subjects that did not report bloating or distension on the survey but had seen a physician in the past for bloating / distension (most of them [n=55] greater than 5 years prior to the survey).
Based on the questionnaire, we found that 615/2259 (27%) subjects reported bloating/distention in the survey period; out of them, 44% (272/615) had visible distention, and 99% (609/615) of the bloaters reported at least one other GI complaint. On the other hand, we defined 281/2259 (12%) IBS cases in the survey period, with 69% (195/281) of them reporting bloating (30% (84/281) bloating alone cases, 40% (111/281) distention cases). Table 2 illustrated the percentage of bloating alone and distention symptoms in the community and in the common disorders (IBS, dyspepsia and functional constipation) during the survey period.
Table 2.
The percentage of bloating alone and distention symptoms in community and in several common disorders (IBS, dyspepsia and functional constipation) during the survey period
| % (n) of the total sample N=2259 |
%(n) meeting IBS criteria N=281 |
%(n) meeting Dyspepsia criteria N=110 |
%(n) meeting Functional constipation criteria N=238 |
|
|---|---|---|---|---|
| Bloating alone | 15% (343) | 40% (84) | 25% (27) | 28% (66) |
| Distention | 12% (272) | 40% (111) | 44% (48) | 11% (26) |
| No bloating/distention | 73% (1644) | 31% (86) | 32% (35) | 61% (146) |
Considering bloaters, we found that only 1% (6/615) of them had consulted a doctor for bloating like symptoms, while 18% (108/615) had seen a doctor for other GI symptoms in the survey period. Table 3 illustrated the consulting behavior in the year prior to the survey by subject group based on questionnaire responses to the bloating and distention questions.
Table 3.
Consulting behavior in the year prior to the survey by subject group based on questionnaire responses to bloating and distention questions.
| Symptoms Reported |
n of cases |
With other GI symptoms %(n) |
B/D visits %(n) |
other GI visits %(n) |
No GI visit %(n) |
|---|---|---|---|---|---|
| Bloating alone | 343 | 99% (340) | 1% (2) | 14% (49) | 85% (292) |
| Distention | 272 | 99% (269) | 2% (4) | 22% (59) | 77% (209) |
| No B/D | 1644 | 81% (1326) | 0.1% (1*) | 8% (124) | 92% (1519) |
| Total | 2259 | 86% (1935) | 0.3% (7) | 10% (232) | 89% (2020) |
one subject answered ‘no’ to the bloating and distention questions but had seen a physician for B/D in the year prior to the survey based on chart review of their medical history.
Predictors for bloating visits and other GI visits vs. no GI visits
The logistic regression analysis estimated ORs (95% CIs) of predictors for bloating/ distention visits, and other GI visits (each vs. no GI visits) are illustrated in Table 4, adjusted for age, gender, SSC score, and bloating/distension symptom status. Older age, lower education, and abdominal pain were associated with increased odds for bloating/ distention visits as well as for other GI visits, compared to no GI visits. Moreover, chronic constipation and frequent abdominal pain increased the odds for people to seek health care for bloating and distention vs. no GI visits. Higher SSC score severity, and the frequency of abdominal pain were associated with other GI visits compared to no GI visits. Overall, females had similar odds for type of physician visit relative to males.
Table4.
Odds Ratios (OR) from logistic regression models† for type of consulting behavior in n=2259 subjects in whom questionnaire responses were obtained.
| B/D§ visit vs. no GI visit OR (95% CI) |
Other GI visit vs. no GI visit OR (95% CI) |
B/D visit vs. other GI visit OR (95% CI) |
|
|---|---|---|---|
| Age per 10 years | 1.9 (1.6,2.3) | 1.3 (1.2,1.4) | 1.5 (1.2,1.7) |
| Female vs. male | 1.1 (0.7,1.6) | 1.0 (0.9,1.2) | 1.1 (0.7,1.6) |
| SSC per 1 unit | 1.4 (0.9,2.0) | 1.6 (1.3,1.9) | 0.9 (0.6,1.3) |
| Bloating/Distention# | |||
| Bloating alone | 1.8 (1.0,3.1) | 1.5 (1.1,1.9) | 1.2 (0.7,2.1) |
| Distention +/−bloating | 4.8 (2.9,8.2) | 1.6 (1.2,2.2) | 3.0 (1.8,4.9) |
| Married vs. not married | 1.2 (0.7,1.9) | 1.1 (0.8,1.3) | 1.1 (0.7,1.8) |
| Current smoker vs. not current smoker | 1.2 (0.6,2.6) | 1.1 (0.8,1.6) | 1.1 (0.5,2.3) |
| Current alcohol user vs. not current alcohol user | 1.2 (0.8,1.8) | 1.0 (0.8,1.2) | 1.2 (0.8,1.8) |
| Education | |||
| < high school vs. High school or some college | 2.6 (1.2,5.6) | 2.3 (1.4,3.9) | 1.1 (0.6,2.2) |
| College or professional training vs. High school or some college | 0.7 (0.4,1.1) | 0.9 (0.7,1.1) | 0.8 (0.5,1.2) |
| Chronic diarrhea# | 1.2 (0.7,2.0) | 1.2 (0.9,1.5) | 1.0 (0.6,1.7) |
| Chronic constipation# | 1.9 (1.1,3.2) | 0.9 (0.7,1.3) | 2.0 (1.2,3.4) |
| Heartburn# | 1.2 (0.7,2.0) | 1.2 (0.9,1.6) | 1.0 (0.6,1.6) |
| Early satiety# | 1.3 (0.6,2.6) | 1.4 (0.9,2.0) | 0.9 (0.5,1.8) |
| Loss of appetite# | 1.2 (0.7,2.3) | 1.0 (0.7,1.4) | 1.2 (0.7,2.2) |
| Nausea# | 0.4 (0.1,1.9) | 1.5 (0.8,2.7) | 0.3 (0.1,1.2) |
| Blood in stools# | 1.6 (0.9,2.8) | 1.2 (0.9,1.6) | 1.3 (0.8,2.3) |
| Chest pain# | 1.6 (0.7,3.8) | 1.6 (1.0,2.6) | 1.0 (0.4,2.2) |
| Abdominal pain# | 1.8 (1.2,2.8) | 1.9 (1.6,2.4) | 0.9 (0.6,1.4) |
| Severity of pain | |||
| Moderate ‡ | 1.4 (0.8,2.3) | 1.7 (1.3,2.1) | 0.8 (0.5,1.3) |
| Severe‡ | 1.2 (0.4,3.9) | 2.4 (1.4,4.1) | 0.5 (0.2,1.5) |
| Frequency of pain# | |||
| About Once a month | 1.3 (0.8,2.3) | 1.8 (1.4,2.3) | 0.7 (0.4,1.3) |
| About Once a week | 4.0 (1.8,8.7) | 2.8 (1.7,4.7) | 1.4 (0.7,2.8) |
| Several times a week/daily | 2.4 (1.2,5.1) | 2.3 (1.5,3.6) | 1.0 (0.5,2.0) |
| Site of bloating/distention* | |||
| Above navel | 1.7 (0.8,3.8) | 0.9 (0.6,1.3) | 1.9 (0.9,4.2) |
| Below navel | 1.2 (0.5,2.8) | 1.0 (0.7,1.4) | 1.3 (0.6,2.9) |
| Above and below navel | 1.7 (0.7,3.9) | 1.2 (0.8,1.8) | 1.4 (0.6,3.3) |
Models adjusted for age, gender, somatic symptom checklist (SSC) score and reporting bloating or distention on the survey.
B/D: bloating or distention.
SSC: somatic symptoms checklist scores
symptom versus absence of the symptom (reference level)
vs. none/mild pain (reference level)
No bloating/distention or unspecified site as the reference level.
Predictors for bloating visits vs. other GI visits
The analyses of predictors of consulting for bloating and distention visits vs. visits for other GI symptoms indicated that older age (OR, 1.5; CI: 1.2, 1.7), and chronic constipation (OR, 2.0; CI: 1.2, 3.4) were associated with greater odds for presenting for bloating and/or distention compared to seeking care for other GI symptoms. Interestingly, SSC scores (OR, 1.1; CI: 0.8, 1.5) and female gender (OR, 1.2; CI: 0.8, 1.8)) were not significantly associated with visits for bloating/distension vs. for other GI visits (Table 4).
As might be expected, reporting visible distention on the survey was also positively associated with more bloating/distention visits vs. other GI visits (OR, 3.0; CI: 1.8, 4.9), however reporting bloating alone was not (OR, 1.2; CI: 0.7, 2.1).
DISCUSSION
Little has been know about consulting behavior for functional bloating or distention. The present results provide a profile of the consulting behavior of those who saw a physician for bloating/distention in a community population.
It may be assumed that patients’ rating of a symptom as most bothersome will result in a strong expectation and motivation to obtain relief from the particular symptom. Bloating and distention are very common (1–3, 13) and often rank as the most bothersome GI symptom (14, 15). However, the consulting rates for bloating and distention in the community are much lower than other GI symptoms (6% vs. 51%). The possible explanation might be that the majority of subjects (99%) suffering from bloating and distention had accompanying other GI symptoms. Others have observed that both bloating and abdominal distention worsened when other abdominal symptoms were present (17). Patients (and physicians) may also perceive sensations such as bloating as being bothersome and annoying, rather than life threatening. Other GI symptoms such as abdominal pain are likely perceived as warning or alarm signs of a more serious process, resulting in a greater likelihood of attention by patients themselves and the treating physician.
We found that factors leading people to consult for bloating and distention were similar to those leading people to consult for other GI symptoms. Those who had consulted doctors specifically for bloating and distention as well as for other GI symptoms tended to be older and with lower education levels compared to subjects with no GI visits. Consulting a physician more for bloating and distention also seemed to be explained by co-morbid chronic constipation, which may induce more pronounced bloating and distention. Houghton et al reported that there was a strong correlation between bloating scores and distention in those subjects with constipation, whereas this does not appear to be the case in those individuals with diarrhea; furthermore, the higher the pain thresholds(hyposensitivity) experienced by the patients, the more they distended during the course of the day (37). Of interest, people with objective distention seem to seek more health care. These findings are consistent with the concept that visible abdominal distension is present in subjects with more severe bloating symptoms and may suggest that people weigh this symptom as then more important (17).
There is preliminary evidence to support a role for mental stress, depression, sleeping difficulties, problems coping, and the use of analgesics in the pathogenesis of bloating like symptoms (12). However, our present study does not suggest that somatization was related to greater health care seeking of bloating and distention compared to other GI symptoms, which may reflect that biologic features rather than psychological morbidity drive visits for bloating and distention versus other gastrointestinal problems. Previous studies have suggested that females not only have more FGIDs, including bloating and distention symptoms but also consult health care more frequently (3, 5, 38), however, this was not consistent with our findings.
Our population data resource was derived from Olmsted County, Minnesota, a place uniquely positioned to perform high quality population-based research in the USA (26). We believe that the results from this study are valid and generalizable to the American white population (38). Our response rate was adequate and additional data comparing respondents and non-respondents suggests non-response bias is unlikely (36). On the other hand, the population assessed in the survey was somewhat older and this data might not apply to younger people, where indeed a female predominance of bloating might be seen. Moreover, we used self-report data, which may be subject to recall bias with respect to occurrence of symptoms and in particular, health care use over the past one year, however, because we aimed to assess health care use for bloating and distention in a large community sample, the use of a survey was the only practical methodology available. The present study asked only about physician visits and therefore failed to assess the broad range of alternative health services that may be used by persons with bloating and distention, such as pharmacists or chiropractors. This area requires close attention in the future studies.
There are certain clinical implications resulting from this study. We demonstrated many with bloating and distention do not seek care for these complaints. Many patients presenting for care for other GI symptoms will have bloating and distention, although treatment of the latter remains challenging. Overall, factors that lead people to present for bloating and distention are similar to those for other GI symptom visits; however, some specific biologic (e.g. chronic constipation) rather than psychological features appear to predict visits for bloating and distention. Our date imply that better management of constipation might reduce physician visits for bloating and distention.
Abbreviations
- FGIDs
functional gastrointestinal disorders
- GI
gastrointestinal
- OR
odds ratio
- CI
confidence interval
- SSC
somatic symptom checklist score
- B/D
bloating or distention
- REP
Rochester Epidemiology Project
- BDQ
Bowel Disease Questionnaire
- BMI
body mass index
- IBS
irritable bowel syndrome
Footnotes
Conflicts of interest: none to declare.
References
- 1.Houghton LA, Whorwell PJ. Towards a better understanding of abdominal bloating and distension in functional gastrointestinal disorders. Neurogastroenterol Motil. 2005;17(4):500–511. doi: 10.1111/j.1365-2982.2005.00666.x. [DOI] [PubMed] [Google Scholar]
- 2.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional Bowel Disorders. In: Drossman DA, editor. ROME III The Functional Gastrointestinal Disorders. Third ed. Mclean, Virginia: DeGNON ASSOCIATES; 2006. pp. 487–555. [Google Scholar]
- 3.Jiang X, Locke GR, 3rd, Choung RS, Zinsmeister AR, Schleck CD, Talley NJ. Prevalence and risk factors for abdominal bloating and visible distention: a population-based study. Gut. 2008;57(6):756–763. doi: 10.1136/gut.2007.142810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandler RS, Stewart WF, Liberman JN, Ricci JA, Zorich NL. Abdominal pain, bloating, and diarrhea in the United States: prevalence and impact. Dig Dis Sci. 2000;45(6):1166–1171. doi: 10.1023/a:1005554103531. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38(9):1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 6.Hungin AP, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003;17(5):643–650. doi: 10.1046/j.1365-2036.2003.01456.x. [DOI] [PubMed] [Google Scholar]
- 7.Kay L, Jorgensen T, Jensen KH. The epidemiology of irritable bowel syndrome in a random population. Prevalence, incidence, natural history and risk factors. J Intern Med. 1994;236:23–30. doi: 10.1111/j.1365-2796.1994.tb01115.x. [DOI] [PubMed] [Google Scholar]
- 8.Koloski NA, Talley NJ, Boyce PM. Epidemiology and health care seeking in the functional GI disorders: a population-based study. Am J Gastroenterol. 2002;97(9):2290–2299. doi: 10.1111/j.1572-0241.2002.05783.x. [DOI] [PubMed] [Google Scholar]
- 9.Longstreth GF, Wilson A, Knight K, Wong J, Chiou CF, Barghout V, et al. Irritable bowel syndrome, health care use, and costs: a U.S. managed care perspective. Am J Gastroenterol. 2003;98(3):600–607. doi: 10.1111/j.1572-0241.2003.07296.x. [DOI] [PubMed] [Google Scholar]
- 10.Talley NJ, Boyce P, Jones M. Dyspepsia and health care seeking in a community: How important are psychological factors? Dig Dis Sci. 1998;43(5):1016–1022. doi: 10.1023/a:1018878717715. [DOI] [PubMed] [Google Scholar]
- 11.Talley NJ, Boyce PM, Jones M. Predictors of health care seeking for irritable bowel syndrome: a population based study. Gut. 1997;41(3):394–398. doi: 10.1136/gut.41.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnsen R, Jacobsen BK, Forde OH. Associations between symptoms of irritable colon and psychological and social conditions and lifestyle. Br Med J (Clin Res Ed) 1986;292(6536):1633–1635. doi: 10.1136/bmj.292.6536.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Castillo EJ, Camilleri M, Locke GR, Burton DD, Stephens DA, Geno DM, et al. A community-based, controlled study of the epidemiology and pathophysiology of dyspepsia. Clin Gastroenterol Hepatol. 2004;2(11):985–996. doi: 10.1016/s1542-3565(04)00454-9. [DOI] [PubMed] [Google Scholar]
- 14.Lembo T, Naliboff B, Munakata J, Fullerton S, Saba L, Tung S, et al. Symptoms and visceral perception in patients with pain-predominant irritable bowel syndrome. Am J Gastroenterol. 1999;94(5):1320–1326. doi: 10.1111/j.1572-0241.1999.01009.x. [DOI] [PubMed] [Google Scholar]
- 15.Schmulson M, Lee OY, Chang L, Naliboff B, Mayer EA. Symptom differences in moderate to severe IBS patients based on predominant bowel habit. Am J Gastroenterol. 1999;94(10):2929–2935. doi: 10.1111/j.1572-0241.1999.01440.x. [DOI] [PubMed] [Google Scholar]
- 16.Cain KC, Headstrom P, Jarrett ME, Motzer SA, Park H, Burr RL, et al. Abdominal pain impacts quality of life in women with irritable bowel syndrome. Am J Gastroenterol. 2006;101(1):124–132. doi: 10.1111/j.1572-0241.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- 17.Chang L, Lee OY, Naliboff B, Schmulson M, Mayer EA. Sensation of bloating and visible abdominal distension in patients with irritable bowel syndrome. Am J Gastroenterol. 2001;96(12):3341–3347. doi: 10.1111/j.1572-0241.2001.05336.x. [DOI] [PubMed] [Google Scholar]
- 18.Walker EA, Katon WJ, Jemelka RP, Roy-Bryne PP. Comorbidity of gastrointestinal complaints, depression, and anxiety in the Epidemiologic Catchment Area (ECA) Study. Am J Med. 1992;92(1A):26S–30S. doi: 10.1016/0002-9343(92)90133-v. [DOI] [PubMed] [Google Scholar]
- 19.Heaton KW, Ghosh S, Braddon FE. How bad are the symptoms and bowel dysfunction of patients with the irritable bowel syndrome? A prospective, controlled study with emphasis on stool form. Gut. 1991;32(1):73–79. doi: 10.1136/gut.32.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith RC, Greenbaum DS, Vancouver JB, Henry RC, Reinhart MA, Greenbaum RB, et al. Psychosocial factors are associated with health care seeking rather than diagnosis in irritable bowel syndrome. Gastroenterology. 1990;98(2):293–301. doi: 10.1016/0016-5085(90)90817-k. [DOI] [PubMed] [Google Scholar]
- 21.Colgan S, Creed F, Klass H. Symptom complaints, psychiatric disorder and abnormal illness behaviour in patients with upper abdominal pain. Psychol Med. 1988;18(4):887–892. doi: 10.1017/s003329170000982x. [DOI] [PubMed] [Google Scholar]
- 22.Zuckerman MJ, Guerra LG, Drossman DA, Foland JA, Gregory GG. Health-care-seeking behaviors related to bowel complaints. Hispanics versus non-Hispanic whites. Dig Dis Sci. 1996;41(1):77–82. doi: 10.1007/BF02208587. [DOI] [PubMed] [Google Scholar]
- 23.Gomborone J, Dewsnap P, Libby G, Farthing M. Abnormal illness attitudes in patients with irritable bowel syndrome. J Psychosom Res. 1995;39(2):227–230. doi: 10.1016/0022-3999(94)00126-p. [DOI] [PubMed] [Google Scholar]
- 24.Whitehead WE, Bosmajian L, Zonderman AB, Costa PT, Jr, Schuster MM. Symptoms of psychologic distress associated with irritable bowel syndrome. Comparison of community and medical clinic samples. Gastroenterology. 1988;95(3):709–714. doi: 10.1016/s0016-5085(88)80018-0. [DOI] [PubMed] [Google Scholar]
- 25.Drossman DA, McKee DC, Sandler RS, Mitchell CM, Cramer EM, Lowman BC, et al. Psychosocial factors in the irritable bowel syndrome. A multivariate study of patients and nonpatients with irritable bowel syndrome. Gastroenterology. 1988;95(3):701–708. doi: 10.1016/s0016-5085(88)80017-9. [DOI] [PubMed] [Google Scholar]
- 26.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71(3):266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 27.Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ., 3rd Dyspepsia and dyspepsia subgroups: a population-based study. Gastroenterology. 1992;102(4 Pt 1):1259–1268. [PubMed] [Google Scholar]
- 28.Talley NJ, Weaver AL, Zinsmeister AR, Melton LJ., 3rd Onset and disappearance of gastrointestinal symptoms and functional gastrointestinal disorders. Am J Epidemiol. 1992;136(2):165–177. doi: 10.1093/oxfordjournals.aje.a116483. [DOI] [PubMed] [Google Scholar]
- 29.Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ., 3rd Smoking, alcohol, and analgesics in dyspepsia and among dyspepsia subgroups: lack of an association in a community. Gut. 1994;35(5):619–624. doi: 10.1136/gut.35.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., 3rd Gastrointestinal tract symptoms and self-reported abuse: a population-based study. Gastroenterology. 1994;107(4):1040–1049. doi: 10.1016/0016-5085(94)90228-3. [DOI] [PubMed] [Google Scholar]
- 31.Locke GR, 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., 3rd Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112(5):1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 32.Locke GR, 3rd, Weaver AL, Melton LJ, 3rd, Talley NJ. Psychosocial factors are linked to functional gastrointestinal disorders: a population based nested case-control study. Am J Gastroenterol. 2004;99(2):350–357. doi: 10.1111/j.1572-0241.2004.04043.x. [DOI] [PubMed] [Google Scholar]
- 33.Talley NJ, Phillips SF, Melton J, 3rd, Wiltgen C, Zinsmeister AR. A patient questionnaire to identify bowel disease. Ann Intern Med. 1989;111(8):671–674. doi: 10.7326/0003-4819-111-8-671. [DOI] [PubMed] [Google Scholar]
- 34.Talley NJ, Phillips SF, Wiltgen CM, Zinsmeister AR, Melton LJ., 3rd Assessment of functional gastrointestinal disease: the bowel disease questionnaire. Mayo Clin Proc. 1990;65(11):1456–1479. doi: 10.1016/s0025-6196(12)62169-7. [DOI] [PubMed] [Google Scholar]
- 35.Attanasio V, Andrasik F, Blanchard EB, Arena JG. Psychometric properties of the SUNYA revision of the Psychosomatic Symptom Checklist. J Behav Med. 1984;7(2):247–257. doi: 10.1007/BF00845390. [DOI] [PubMed] [Google Scholar]
- 36.Choung RS, Locke GR, 3rd, Zinsmeister AR, Schleck CD, Talley NJ. Epidemiology of slow and fast colonic transit using a scale of stool form in a community. Alimentary pharmacology & therapeutics. 2007;26(7):1043–1050. doi: 10.1111/j.1365-2036.2007.03456.x. [DOI] [PubMed] [Google Scholar]
- 37.Houghton LA, Lea R, Agrawal A, Reilly B, Whorwell PJ. Relationship of abdominal bloating to distention in irritable bowel syndrome and effect of bowel habit. Gastroenterology. 2006;131(4):1003–1010. doi: 10.1053/j.gastro.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 38.Talley NJ, Zinsmeister AR, Van Dyke C, Melton LJ., 3rd Epidemiology of colonic symptoms and the irritable bowel syndrome. Gastroenterology. 1991;101(4):927–934. doi: 10.1016/0016-5085(91)90717-y. [DOI] [PubMed] [Google Scholar]