Abstract
Given a certain severity of crash and of injury, it is unclear whether acute and/or chronic alcohol use leads to increased morbidity, mortality or a more complicated hospital course after motor vehicle collisions. 496 patients admitted to a trauma service were retrospectively evaluated to assess the effects of acute alcohol ingestion and chronic alcohol use on outcome. Results suggest that patients with acute or chronic alcohol abuse have increased needs for nursing services in the hospital. Alcohol use did not play a role in modifying other outcome measures.
It is well established that acute and chronic alcohol abuse are important factors in motor vehicle collisions (MVC’s). The awareness of this relationship has increased over the past 20 years. In 1982, 54% of driver fatalities and 16% of driver survivors of motor vehicle collisions were tested for alcohol. This increased to 67% and 25% respectively in 1997 [NHTSA, 1997a]. Seven percent of MVC’s involve a driver who has alcohol in his or her blood [NHTSA, 1997a]. While the percentage of fatalities from MVC’s involving a driver with a measured blood alcohol concentration (BAC) greater than 0 decreased from 57% in 1982 to 39% in 1997 [NHTSA, 1997b], alcohol associated MVC’s continue to be an important public health problem.
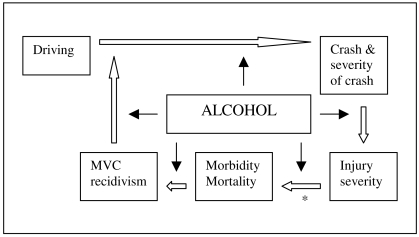
Alcohol has a potential role in many aspects of MVC’s (see Figure). Although it is clear that drivers who have an elevated BAC are more likely to get into a crash [McMarroll, 1961] [NHTSA, 1998] [Secretary of the Department of Health and Human Services, 1997] and are more likely to suffer a repeat MVC [Rivara, 1993], the other points in the flow chart are less definitively known.
Figure.
Schematic showing points where alcohol may play a role in motor vehicle collisions and subsequent patient care.
We hypothesized that MVC patients with a lifetime history of chronic alcohol abuse would have a more complicated hospital course than controls. This paper describes a retrospective cohort study of patients admitted to a general surgery trauma service between May 1, 1992 and August 30, 1994. By controlling for injury severity, we attempted to evaluate the independent effects of both acute alcohol ingestion and chronic alcohol abuse on clinical outcomes of subjects who sustained a MVC and were admitted to an inpatient trauma surgery service. The outcome measures include mortality, ICU admission, number of operations, presence of complications, utilization of nursing services, volume of blood transfusions, length of stay and functional status at discharge.
METHODS
SAMPLE
Subjects were patients >= 18 years old who were occupants of automobiles or small trucks involved in a MVC and who presented directly from the scene to the Emergency Department within six hours of the crash, and who were admitted to the inpatient general surgery trauma service. Pregnant patients, transfer patients and institutionalized patients were excluded. Subjects were enrolled from one academic, tertiary, American College of Surgeons (ACS) verified Level I trauma center and from one community hospital not designated by the ACS as a trauma center. The subjects were enrolled from 1992 to 1994 as part of a prospective study to examine the potentiating effect of alcohol on injury [Waller, 1999]. The current study describes secondary analysis in a retrospective manner performed on these data.
MEASURES
Chronic alcohol abuse/dependence (AA/AD) was determined using the alcohol section of the Diagnostic Interview Schedule of the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM III-R) [American Psychiatric Association, 1987]. Lifetime severity of AA/AD is broken down into five categories: none, alcohol abuse, mild dependence, moderate dependence and severe dependence. This study defines none as AA/AD− and all other categories of AA/AD as AA/AD+. Acute alcohol ingestion was determined by serum analysis, whole blood analysis or breath analysis to evaluate for BAC. Blood or breath samples were obtained within six hours from the time of injury. Subjects are classified as BAC+ if they had a BAC > 0, and BAC- if they had a BAC = 0. Cannabis, cocaine and opiate information were based on whole blood samples drawn within six hours of the crash and sent to Compuchem Laboratories, Inc. (now LABCORPS) in the Research Triangle Park, North Carolina. Injury severity was defined by the Injury Severity Score (ISS) [Baker, 1974] using the Abbreviated Injury Scale, 1985 version (which correlates 0.98 with AIS-90), and Tri-Code injury scoring software (Tri-analytics R, Bel Air, MD). Mean corpuscular volume (MCV) and gammaglutamyl transferase (GGT) were also determined, with levels of greater than 95 femtoliters and greater than 85 IU/L respectively being suggested as additional indicators of chronic alcohol abuse [Jurkovich, 1993].
Vehicle occupant position, restraint use and severity of crash were determined from the Michigan Uniform Crash Report (UD-10). Severity of the crash was determined using the Traffic Accident Data (TAD) system, where no visible damage to the vehicle scores zero points with a maximum of seven points for the most severe collision. The scale was developed by the National Safety Council and relies on investigating police officers comparing the state of the vehicle to standard photographs of damaged vehicles, then assigning a collision rating. Reliability problems of the TAD system include the subjective nature of the scoring and the non-uniformity of the system in different geographic areas [Compton, 1993]. Glasgow Coma Score (GCS), a measure of central nervous system function and graded on a scale from 3 (coma) to 15 (normal) was determined from nursing flow sheets and the medical record. Volume of packed red blood cells transfused, in cubic centimeters (cc’s) was determined from nursing flow sheets. Utilization of nursing care was determined by the Therapeutic Intervention Scoring System (TISS), which was calculated from nursing flow sheets and review of medical records. The TISS was calculated during the initial 24 hours after the injury and after the Emergency Medical Service arrived on the scene. In the TISS, interventions are scored from one point for a minimal intervention such as the use of a urinary catheter or the use of IV antibiotics to four points for complicated interventions such as use of a pulmonary artery catheter, controlled ventilation, or the management of a cardiac arrest [Cullen, 1974] [Silverman, 1975]. Other outcome measures such as discharge functional status, number of operations, number of days in ICU, length of stay (LOS), mortality, and number of complications were determined from the medical record.
ANALYSIS
We selected eight dimensions of hospital course: mortality, ICU admission, number of operations, presence of complications, TISS, volume of blood transfusions, length of stay and functional status at discharge. Acute effects of alcohol were analyzed using the sample of 496 subjects who had BAC data. The effects of chronic use were analyzed in the sub-sample of 339 subjects who completed the Diagnostic Interview Schedule. Statistical significance was defined as an alpha of 0.05. The numerical values for the p-values are explicitly stated if p < 0.1.
The primary aim of the study was to determine the role of acute and chronic alcohol use on hospital course. We first evaluated the effects of acute alcohol ingestion. We used univariate analysis to compare descriptively subject characteristics between BAC+ (n = 192) and BAC- (n = 304) for the entire sample of 496 subjects who had blood alcohol concentrations drawn, using two tailed t-tests for continuous variables and chi-square for categorical variables. We then analyzed outcome data for the entire sample, evaluating for the effects of BAC+ and BAC- on clinical outcomes, after controlling for ISS.
To control for other variables that might have affected hospital course, we utilized Analysis of Covariance (ANCOVA) and linear or logistic regression, depending on the distribution of the dependent variable, to model outcome measures. ISS was entered as a predictor and the role of acute alcohol ingestion was evaluated after accounting for ISS on outcome. Other well-known predictors of worse outcome were evaluated as potential covariates (i.e. age and sex). These were not significantly related to outcome so they were not used in the final analysis. Because the ISS is a dependent on TAD, we chose to use only the ISS in our analysis as a covariant. For continuous variables, p values were computed using univariate ANCOVA and means were computed after adjusting for ISS. For categorical variables, p values were calculated using logistic regression and proportions were calculated after adjusting for ISS.
Next, we evaluated the individual effects of BAC and AA/AD as well as their joint effect. We analyzed the subset of subjects who completed the Diagnostic Interview Schedule for AA/AD (n = 339), dividing them into four groups: BAC+:AA/AD+ (n = 89), BAC+:AA/AD− (n = 30), BAC−:AA/AD+ (n = 43) and BAC−:AA/AD− (n = 177). Continuous subject characteristics were analyzed using univariate ANOVA; categorical characteristics were analyzed using logistic regression.
Finally, using the same four groups, we analyzed the clinical outcome measures. For continuous variables, we used ANCOVA (Type I Sum of Squares) BAC X AA/AD with ISS as the covariate. The effects of BAC, AA/AD and the interaction of BAC+ with AA/AD were tested. Categorical variables were analyzed with logistic regression. For continuous variables, means were computed after adjusting for ISS. For categorical variables, proportions were calculated after adjusting for ISS.
Thirty two percent of the subjects had missing data regarding their AA/AD diagnosis. Preliminary analyses revealed that subjects with missing data were more likely to have a positive BAC on admission (46%) than subjects who had completed the DSM III-R Diagnostic Interview Schedule (35% BAC+), p = 0.017. This would introduce selection bias, as these subjects would be more likely to be AA/AD positive.
RESULTS
A total of 1833 subjects who met the study criteria fell into the sampling frame. Of these, 1705 were approached and provided written consent to provide a blood or breath sample for analysis of alcohol and other drugs. Of these, 496 subjects who were in passenger cars were admitted to the inpatient trauma surgery service of the hospitals. This subsample was the focus of the present analysis. 39% of these were BAC+. Of the 496 subjects, 68% completed the Diagnostic Interview Schedule, of whom 39% screened positive for AA/AD. Of the BAC+ subjects, 75% screened positive for AA/AD while 20% of the BAC− subjects screened positive for AA/AD, p < 0.001. Of the AA/AD+ subjects, 67% were BAC+ on admission while 15% of the AA/AD− subjects were BAC+ on admission, p < 0.001. For subjects with BAC > 0, the average BAC for AA/AD+ subjects was significantly higher than for AA/AD negative subjects (180 vs. 137, p = 0.003).
I. EFFECTS OF ACUTE ALCOHOL INGESTION
Subjects
A univariate analysis of characteristics of all 496 subjects comparing BAC+ with BAC− subjects can be found in Table 1. BAC+ subjects had a higher probability of being male, younger, more likely to not wear a seatbelt and a higher probability of cannabis in the blood on admission. The BAC+ group had a lower GCS by 0.7 points, p = 0.015. The BAC+ group had a larger proportion with an elevated MCV, although only 11% of that group had an elevated MCV. BAC+ subjects had significantly higher levels of baseline alcohol use including increased number of drinks needed to have an effect (4 vs. 2), number of drinks per week (16 vs. 2), maximum number of drinks in recent history (13 vs. 4), and increased proportion of screening positive on the Diagnostic Interview Schedule for AA/AD (75% vs. 20%), all p values less than 0.001. However, ISS did not differ between groups.
Table 1.
Subject characteristics for entire data set (n = 496).
| BAC+ (n = 192) | BAC− (n = 304) | p value | |
|---|---|---|---|
| age (SD) | 31.6 (11.0) | 38.8 (18.0) | <.001 |
| TAD score (SD) | 5.6 (1.3) | 5.4 (1.5) | NS |
| ISS (SD) | 10.0 (9.7) | 11.0 (10.4) | NS |
| GCS (SD) | 13.5 (3.1) | 14.2 (2.4) | 0.015 |
| male (%) | 148 (80%) | 152 (51%) | <.001 |
| driver (%) | 156 (81%) | 239 (79%) | NS |
| no seatbelt (%) | 103 (60%) | 97 (34%) | <.001 |
| MCV>95 (%) | 20 (11%) | 15 (5%) | .021 |
| GGT>85 (%) | 18 (13%) | 17 (8%) | NS |
| cocaine (%) | 7 (5%) | 3 (1%) | .051 |
| cannabis (%) | 40 (27%) | 22 (9%) | <.001 |
| opiates (%) | 2 (1%) | 4 (2%) | NS |
SD = standard deviation.
% = proportion of BAC+ or BAC− with associated characteristic.
ISS = Injury Severity Score, GCS = Glasgow Coma Score, MCV = mean corpuscular volume, GGT = gammaglutamyl transferase, NS = not significant.
Outcomes
Apart from the TISS, no statistically significant outcome differences were present between BAC+ subjects and BAC− subjects. The TISS for the initial 24 hours after injury was 2.9 points higher in the BAC+ group, p = 0.044. ICU admission, LOS, operations performed, complications present, blood transfusions, mortality, and discharge functional status all had statistically similar outcomes comparing the two groups. These results can be found in Table 2.
Table 2.
Outcome analysis for entire data set adjusted for ISS (n=496).
| BAC+ n = 192 | BAC− n = 304 | p value | |
|---|---|---|---|
| ICU admission | 70 (38%) | 129 (41%) | NS |
| days in ICU (SE) | 2.0 (0.32) | 2.1 (0.25) | NS |
| TISS 24 (SE) | 21.7 (0.73) | 19.8 (0.58) | 0.044 |
| LOS (SE) | 6.0 (0.55) | 5.9 (0.44) | NS |
| operation performed (adj %) | 61 (33%) | 89 (28%) | NS |
| number of operations (SE) | 0.71 (0.11) | 0.79 (0.09) | NS |
| presence of complication (adj %) | 27 (15%) | 49 (16%) | NS |
| number of complications (SE) | .31 (0.07) | .36 (0.05) | NS |
| PRBC 24 hours (cc) (SE) | 278 (120) | 413 (93) | NS |
| mortality (adj %) | 2 (1.4%) | 14 (4.2%) | .080 |
| independent at discharge (adj %) | 128 (76%) | 198 (76%) | NS |
| ambulatory at discharge (adj %) | 145 (87%) | 223 (85%) | NS |
Mean is adjusted for ISS for continuous variables.
adj. % = adjusted percent. For categorical variables, proportion with associated outcome within BAC− or BAC+ group is adjusted for ISS.
SE = standard error of the mean.
ICU = Intensive Care Unit, TISS 24 = Therapeutic Intervention Scoring System for first 24 hours, LOS = Length of stay, PRBC = Packed red blood cells, cc = cubic centimeters.
II. JOINT EFFECTS OF ACUTE ALCOHOL INGESTION AND CHRONIC ABUSE
Subjects
Table 3 displays the descriptive characteristics of the sub-sample who completed the Diagnostic Interview Schedule, stratified for BAC and AA/AD. The BAC+ subject characteristic was associated with younger age and lower GCS. Both BAC+ and AA/AD+ characteristics were independently associated with subjects having higher alcohol use indicators including more drinks needed to have an effect, higher average number of drinks per week and higher maximum number of drinks in current history.
Table 3.
Analysis of joint effects of BAC and AA/AD on subject characteristics (n = 339).
| BAC+ | BAC− | Factor p-values | |||||
|---|---|---|---|---|---|---|---|
| AA/AD + n = 89 | AA/AD − n = 30 | AA/AD + n = 43 | AA/AD − n = 177 | BAC | AA/AD | Interaction | |
| age (SD) | 30.5 (9.6) | 33.6 (12.8) | 37.4 (15.8) | 39.1 (18.2) | 0.004 | NS | NS |
| TAD score (SD) | 5.7 (1.3) | 5.6 (1.6) | 5.5 (1.4) | 5.5 (1.5) | NS | NS | NS |
| ISS (SD) | 10.1 (8.4) | 10.3 (12.7) | 10.6 (8.0) | 10.2 (9.4) | NS | NS | NS |
| GCS (SD) | 13.8 (2.63) | 13.8 (2.87) | 14.9 (0.35) | 14.5 (1.55) | 0.001 | NS | NS |
| # drinks needed for effect (SD) | 4.0 (2.9) | 3.1 (2.0) | 3.1 (5.0) | 1.8 (1.6) | <.001 | 0.005 | NS |
| # drinks per week, current (SD) | 19.3 (26.9) | 3.9 (3.9) | 3.1 (5.7) | 1.1 (2.2) | <.001 | <.001 | 0.001 |
| max number of drinks (SD) | 14.3 (7.1) | 8.2 (4.5) | 5.8 (8.6) | 3.1 (4.2) | <.001 | <.001 | 0.06 |
| MCV>95 (%) | 9 (11%) | 1 (3.7%) | 1 (2.4%) | 7 (4.2%) | NS | NS | NS |
| GGT>85 (%) | 9 (14%) | 1 (4.2%) | 4 (11%) | 5 (4.1%) | NS | NS | NS |
SD = standard deviation.
ISS = Injury Severity Score, GCS = Glasgow Coma Score, AA/AD = Alcohol abuse/alcohol dependence, MCV = mean corpuscular volume, GGT = gammaglutamyl transferase, NS = not significant.
% = Proportion within BAC:AA/AD group.
Outcomes
Table 4 displays the outcome variables for the four subject groups. The TISS for the 24 hours after injury was significantly higher in both the BAC+ group (20.4 vs. 19.5) and the AA/AD positive group (21.2 vs. 18.6), suggesting effects on increased use of nursing services of both acute ingestion of alcohol and chronic alcohol abuse.
Table 4.
Analysis of joint effects of BAC and AA/AD on outcomes, controlling for ISS (n = 339).
| BAC + | BAC − | Factor p-values** | |||||
|---|---|---|---|---|---|---|---|
| AA/AD+ n = 89 | AA/AD− n = 30 | AA/AD+ n = 43 | AA/AD− n = 177 | BAC | AA/AD | Inter action | |
| Mortality (adj. %) | 0(0%) | 0(0%) | 1(0%) | 1(0%) | NS | NS | NS |
| TISS 24 (SE) | 21.3 (1.1) | 19.5 (1.8) | 21.1 (1.5) | 17.8 (0.8) | 0.035 | 0.037 | NS |
| LOS (SE) | 5.1 (0.6) | 5.4 (1.1) | 6.4 (0.9) | 5.1 (0.4) | NS | NS | NS |
| ICU admission (adj. %) | 32 (36%) | 9 (30%) | 23 (53%) | 71 (40%) | NS | NS | NS |
| days in ICU (SE) | 1.4 (0.27) | 1.8 (0.43) | 1.5 (0.38) | 1.4 (0.19) | 0.068 | NS | NS |
| operation performed (adj. %) | 32 (36%) | 9 (30%) | 14 (32%) | 45 (25%) | 0.063 | NS | NS |
| number of operations (SE) | 0.8 (0.16) | 0.4 (0.28) | 0.7 (0.23) | 0.7 (0.11) | NS | NS | NS |
| presence of complication (adj. %) | 9 (10%) | 3 (10%) | 9 (20%) | 21 (12%) | NS | 0.08 | NS |
| number of complications (SE) | 0.21 (0.09) | 0.33 (0.16) | 0.38 (0.13) | 0.28 (0.07) | NS | NS | NS |
| PRBC 24 hours (cc) (SE) | 184 (169) | 498 (288) | 185 (247) | 327 (118) | NS | NS | NS |
| independent at discharge (adj. %) | 64 (80%) | 16 (69%) | 31 (78%) | 126 (79%) | NS | NS | NS |
| ambulatory at discharge (adj. %) | 70 (87%) | 21 (89%) | 32 (80%) | 140 (87%) | NS | NS | NS |
SE = standard error of the mean.
adj. % = adjusted percent. Proportion with associated outcome within BAC:AA/AD group is adjusted for ISS.
ICU = Intensive Care Unit, TISS 24 = Therapeutic Intervention Scoring System for first 24 hours, LOS = Length of stay, PRBC = Packed red blood cells, cc = cubic centimeters.
DISCUSSION
With a given crash extent, there are data to suggest that alcohol has a potentiating effect on the injury severity incurred in the collision. This research has been performed using epidemiological methods of large databases [Waller, 1986], as well as using case control studies on local populations [Tulloh, 1994] [Pories, 1992] [Waller, 1989]. Other researchers have suggested that confounding factors, such as decreased seatbelt use in intoxicated drivers caused the increased ISS and were more significant than the effect of alcohol itself [Andersen, 1990] [Li, 1997].
Researchers have also investigated the effects of both acute alcohol ingestion and chronic alcohol use on clinical outcome after an injury of a given severity has occurred, with conflicting results. There are physiological data that would explain why trauma patients with an elevated BAC would have worse outcomes. These include decreased myocardial response to hypovolemia, EKG changes associated with intoxication, cell membrane changes, immunosuppressive effects and others [Li, 1997] [Gentilello, 1993]. Similarly, chronic alcohol abuse can lead to diminished liver function, nutritional status, mental status, and generally poorer health, thus possibly leading to a worse outcome after trauma.
Gentilello et al. found that the acute effects of alcohol caused increased complications among penetrating abdominal trauma patients, with no differences in outcome associated with chronic alcohol abuse [Gentilello, 1993]. Jurkovich and colleagues found that the chronic use of alcohol increased complications among blunt and penetrating trauma patients, showing increased infections among patients with a positive behavioral screen for alcohol abuse (Short Michigan Alcohol Screening Test) and an elevated GGT [Jurkovich, 1993]. An elevated BAC was not associated with increased complications in their study. However, one study that found improved outcomes among intoxicated patients attributed the results to possible increased catecholamine production among intoxicated patients [Ward, 1982].
Consistent with these previously published works, our study of subjects injured in MVC’s revealed a significant proportion of subjects with a positive BAC (39%), and a substantial proportion of patients with chronic alcohol problems (39% overall with a lifetime diagnosis of AA/AD, 75% among BAC+ subjects.) Given results of previous research showing that alcohol does increase the risk of a motor vehicle driver getting into a collision, and given the finding that over one third of our subjects tested positive for alcohol, we can infer that alcohol played a significant role in causing a significant number of injuries in our study population, and is likely the major factor that, if modified, could prevent a significant proportion of serious collisions.
Our study found that, after controlling for injury severity, both BAC and lifetime chronic alcohol use were associated with modestly higher TISS. Importantly, however, no other outcome measures differed between either of the groups. After controlling for injury severity, the TISS scores were three points higher in AA/AD+ subjects than AA/AD− subjects, and were two points higher in BAC+ than BAC− subjects. A difference of three points over 24 hours could be the result of one moderate intervention, such as the administration of a bolus of fluid or the use of three or more intravenous catheters. We think this difference is of minimal clinical significance. The effect of the increased nursing utilization as it relates to overall health care costs could be further studied. A more detailed breakdown of which nursing services were utilized more in the AA/AD positive subjects and what kinds of injuries those subjects sustained would be interesting.
Our research differed from others investigating the same research question [Gentilello, 1993] [Jurkovich, 1993] in that we found that both acute alcohol level and chronic alcohol use were associated with higher TISS. Gentilello found that BAC was associated with increased infectious complications among penetrating trauma patients while Jurkovich found that chronic alcohol abuse was associated with increased infectious complications among blunt and penetrating trauma patients. The differences could be due to the fact that we studied only MVC patients, found a difference in a measure not used by the other investigators, or used a different standardized measure to evaluate for alcohol abuse.
We also think that the spectrum of alcohol related problems among MVC patients on trauma services needs to be more precisely defined. As noted above, comparing our results to previous studies would suggest that the manner in which chronic alcohol use is defined might impact on the studies’ findings and conclusions. For example, perhaps when the broad spectrum of alcohol use is considered, only MVC patients admitted to the trauma service with an biochemical evidence of chronic alcohol abuse will have problems that can be attributed to their alcohol use, as Jurkovich found [Jurkovich, 1993].
Before concluding our study we need to address several limitations. There are many well known confounders to studies looking at the effects of alcohol on injury, and this study suffers from many of them [Waller, 1988]. This study looks at patients admitted to a surgical service of either a community or tertiary hospital, thus leading to selection bias of the study population. However, the study only includes patients admitted directly from the scene, and does not include transfers from outside hospitals. Certainly, the injury severity of these patients would likely be higher than MVC victims who were not sent to a hospital, who were triaged to a different hospital, or who were released from the Emergency Department. Secondly, the average GCS in the BAC+ patients was 0.7 points lower than in the BAC− group, and this may contribute to higher ISS in the BAC+ solely as a result of the BAC status of the subject, thus leading to more bias. Third, we did not take into account the mechanics of the crash, which may be different comparing BAC+ and BAC− groups, although the TAD scores were similar. This study, however is a clinical study looking at clinical outcomes of MVC victims admitted to a surgery service; it is not investigating the potentiating effect of alcohol on outcomes.
The TISS was developed for use in the intensive care unit, while in our study we used the TISS system as a means of measuring interventions performed from the initial injury until 24 hours later, regardless of whether the subjects were admitted to the intensive care unit. It may be that the TISS does not adequately measure intensity of service given in the non-ICU setting. Also, the p values for TISS, although less than 0.05, must be interpreted in light of the fact that 7 other outcome measures were also evaluated.
Although this study uses a structured diagnostic instrument, the DSM III-R Diagnostic Interview Schedule, to screen for AA/AD, one third of the subjects had missing data in this area. Missing data were due to death, inability to understand or answer the questions, patient refusal, or inability of researchers to approach subjects prior to discharge. This significant amount of missing data could contribute a bias to the results, because subjects with missing AA/AD data were more likely to have a positive BAC, and were therefore more likely to have a diagnosis of AA/AD. Selection bias may be a pervasive issue in medical studies such as this one that involve interviews with potentially critically ill patients.
Finally, other systems of controlling for injury severity such as the Anatomic Profiling system, TRISS or body adjusted MAIS may, when used as a covariant in analyses, provide more information about the effects of alcohol than using the ISS alone.
Although our findings suggest that the impact of acute and chronic alcohol use on the acute episode of care for the MVC patient admitted to a trauma service is minimal, we feel that trauma surgeons should still evaluate their patients for both acute and chronic alcohol abuse. This information is critical for identifying patients who will benefit from interventions for their alcohol abuse, possibly resulting in less likelihood of alcohol related injury in the future [Gentilello, 1999]. Furthermore, the role of acute and chronic alcohol use in long term outcomes from trauma is not well defined and needs more research. Treating alcohol problems may not only prevent trauma recidivism but may also result in better long term trauma outcomes. If alcohol use does indeed impact adversely on long term outcomes, this factor would need to be considered when comparing different interventions or systems.
Our study reiterates the importance of both acute alcohol ingestion and chronic alcohol use as major preventable factors in MVC’s. We found modest effects of acute or chronic alcohol use on intensity of therapeutic interventions needed and no effect on seven other clinical outcomes. Referring back to the Figure, we found additional evidence that suggests that alcohol will have a negative effect on a patient’s hospital course after a given level of injury has been sustained. While alcohol may play a role in worse outcomes or increasing costs given a severity of injury, both acute alcohol ingestion and chronic alcohol abuse have a much clearer role in precipitating a motor vehicle driver getting into a collision, as well as having repeat collisions. Health care providers who care for patients involved in motor vehicle collisions should take that into account during their interactions with these patients, and more research needs to be done to improve treatment options for patients with alcohol abuse/dependence to prevent MVC’s.
(Presenter: David Melnick)
Jeff Runge: Thank you for a nice, crisp presentation. It’s really not the AAAM way though (audience laughter). Does the TISS reflect things like nursing intensity, physician interactions or does it relate to the degree of illness, or is it simply the number of patient interactions or the difficulty treating a patient?
D. Melnick: It was developed to stratify for outcome in the intensive care unit and what it looks at is actual interventions. For instance, not nursing time, not physician time, but how many IVs did patients have. If they had one IV, they would get one point; three IVs, they may get two points. Did they need to be intubated? Do they have a cardiac arrest? Do they need a Swan- Ganz catheter? Those are all more invasive and would give you more points. After 24 hours you would add up all the interventions like CPR, chest tubes, IVs, Foley catheters, the need for ventilation, you would add up those in 24 hours and you would arrive at a score. TISS does not reflect nursing or physician time spent with a patient. That might be something that could be measured in this population. Maybe nurses do spend more time with patients who are intoxicated or who have chronic alcohol problems.
J. Runge: It seems that that score is rather nonspecific. I mean CPR is a big thing, intubation is a big thing, urinary catheter is not a big thing. Frequently, it’s put into people who are drunk so they don’t pee in the bed. So I’m not sure what that really tells us.
D. Melnick: It probably tells us outcome in the intensive care unit.
J. Runge: I also noticed that people who did not have alcohol abuse or alcohol dependency, their average alcohol level or mean alcohol level was 137 milligrams percent.
D. Melnick: For those who tested BAC positive.
J. Runge: BAC positive, alcohol abuse/alcohol dependence negative, a BAC of 137 is pretty high. I wonder about the sensitivity of your AA/AD tests.
D. Melnick: I don’t know the sensitivity of our tests. I know it’s the DSM III-R standard for it. One of the problems is that we only got the data from that test for two thirds of our patients. That is high and maybe we were missing some patients who had a diagnosis of alcohol abuse.
Carl Soderstrom: You cited the seminal paper by Jurkovich and colleagues from Seattle. One of the things they noticed was that the major outcome they found was that chronic alcoholics or chronic alcohol abusers had a higher risk of having infections and, particularly, pneumonia. You list in your tables complications. What are those complications? Did you analyze for infection?
D. Melnick: In a subset analysis we did. The numbers weren’t really high enough so I don’t think we had enough power to see everything. We looked hard. Going in, our hypothesis was that chronic alcohol use or abuse would have worse outcomes and maybe it was because our numbers weren’t big enough or we didn’t have enough power. We certainly didn’t have enough power to break down complications. Jurkovich had many more points than we had.
C. Soderstrom: He had 2500+ patients.
D. Melnick: He found those patients who had both the behavioral definition of alcohol abuse, i.e. they tested positive for the SMAST but they also had to have a biochemical indicator as well so they had an elevated GGT. We certainly did not have enough subjects to break it down that far.
C. Soderstrom: I’m a little confused. How did you define chronic alcohol abuse?
D. Melnick: I don’t have here the DSM III-R basic diagnostic but there are questions asked: such as quantity and frequency of drinking, have you had negative consequences of social drinking, have you got into fights because of drinking; ever arrested because of drinking, and it’s scaled from zero (no history); history of alcohol abuse and then 3 levels of alcohol dependence mild, moderate, severe. In our study we lumped everything from abuse up to severe dependency into one category, and no history in another category.
C. Soderstrom: So you didn’t use bioechemical markers.
D. Melnick: We looked at it, but it wasn’t helpful.
C. Soderstrom: Because your previous work showed they weren’t helpful and everyone else’s work including ours show they are not helpful. In this instrument that you used to make AA/AD, is there a way to separate the AAs from the ADs because I think that’s really critical.
D. Melnick: It probably is critical and that is probably something that would be worthwhile doing. I don’t think we had the power. In the Seattle study, they were looking at all patients admitted to emergency room as well as patients who died in the field – and they have a lot of trauma there so they had a large number of patients. Ours is a very clinical study – surgeons looking at trauma patients, not even an emergency physician, because these are patients submitted to the surgery service. So our numbers are really quite small and when we tried to break it down into gradations of alcohol abuse, the numbers got very small.
C. Soderstrom: Did you have to be interviewed to be in this study?
D. Melnick: You did. In the study, they tried to get proxy interviews with family members, but the final results only deal with actual patient interviews.
C. Soderstrom: I think another limitation that has to be listed is that this is limited to patients who are cognizant and therefore giving you very different results.
D. Melnick: Absolutely.
C. Soderstrom: I applaud you for doing this work. This is an extremely important subject and, as I said, we would all agree that the seminal paper is the Jurkovich paper but still that has some very serious limitations so I think we have to keep plugging away. I don’t think we’re getting the answers that we anticipate because we haven’t quite designed the studies completely right, but I do applaud you for going the extra mile. Thank you.
Footnotes
This work was supported by grants from the National Institute on Alcohol Abuse and Alcoholism, numbers T32 AA07477 and R01 AA09110-01.
REFERENCES
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed, Revised. Washington, DC: 1987. [Google Scholar]
- Andersen JA, McLellan BA, Pagliarello G, Nelson WR. The relative influence of alcohol and seatbelt usage on severity of injury from motor vehicle crashes. Journal of Trauma. 1990;30:415–417. [PubMed] [Google Scholar]
- Baker SP, O’Neil B, Haddon W, Jr, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- Compton CP. The use of public crash data in biomechanical research. In: Nahum AM, Melvin JW, editors. Accidental Injury Biomechanics and Prevention. New York, NY: Springer-Verlag New York Inc; 1993. pp. 49–65. [Google Scholar]
- Cullen DJ, Civetta JM, Briggs BA, Ferrara LC. Therapeutic intervention scoring system: a method for quantitative comparison of patient care. Critical Care Medicine. 1974;2:57–60. [PubMed] [Google Scholar]
- Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daranciang E, Dunn CW, Villaveces A, Copass M, Ries RR. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Annals of Surgery. 1999;230:473–483. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentilello LM, Cobean RA, Walker AP, Moore EE, Wertz MJ, Dellinger EP. Acute ethanol intoxication increases the risk of infection following penetrating abdominal trauma. The Journal of Trauma. 1993;34:669–675. doi: 10.1097/00005373-199305000-00009. [DOI] [PubMed] [Google Scholar]
- Li G, Keyl PM, Smith GS, Baker SP. Alcohol and injury severity: reappraisal of the continuing controversy. Journal of Trauma. 1997;42:562–569. doi: 10.1097/00005373-199703000-00032. [DOI] [PubMed] [Google Scholar]
- Jurkovich GJ, Rivara FP, Gurney JG, Fligner C, Ries R, Mueller BA, Copass M. The effect of acute alcohol intoxication and chronic alcohol abuse on outcome from trauma. JAMA. 1993;270:51–56. [PubMed] [Google Scholar]
- Maio RF, Waller PF, Blow FC, Hill EM. Alcohol abuse/dependence in motor vehicle crash victims presenting to the emergency department. Academic Emergency Medicine. 1997;4:256–262. doi: 10.1111/j.1553-2712.1997.tb03545.x. [DOI] [PubMed] [Google Scholar]
- McMarroll JR, Haddon W., Jr A controlled study of fatal automobile accidents in New York City. Journal of Chronic Disease. 1961;14:655. doi: 10.1016/0021-9681(62)90051-6. [DOI] [PubMed] [Google Scholar]
- National Highway Transportation Safety Administration, U.S. Department of Transportation. Alcohol Traffic Safety Facts 1997. 1997a. http://www.nhtsa.dot.gov/people/ncsa/FactPrev/Alcohol97.html.
- National Highway Transportation Safety Administration, U.S. Department of Transportation. State Alcohol Estimates Traffic Safety Facts 1997. 1997b. http://www.nhtsa.dot.gov/people/ncsa/FactPrev/StAlc97.html.
- National Highway Traffic Safety Administration, U.S. Department of Transportation. Final Report. Alcohol Highway Safety: Problem Update. Apr, 1998. http://www.nhtsa.dot.gov/people/injury/alcohol/alcupdate/alcprobupd.html.
- Pories SE, Gamelli RL, Vacek P, Goodwin G, Shinozaki T, Harris F. Intoxication and Injury. Journal of Trauma. 1992;32:60–64. doi: 10.1097/00005373-199201000-00013. [DOI] [PubMed] [Google Scholar]
- Rivara FP, Koepsell TD, Jurkovich GJ, Gurney JG, Soderberg R. The effects of alcohol abuse on readmission for trauma. JAMA. 1993;270:1962–1964. [PubMed] [Google Scholar]
- Secretary of Health and Human Services, Ninth Special Report to the U.S. Congress on Alcohol and Health. June 1997.
- Silverman DG, Goldiner PL, Kaye BA, Howland WS, Turnbull AD. The therapeutic intervention scoring system. Critical Care Medicine. 1975;3:222 – 225. doi: 10.1097/00003246-197511000-00003. [DOI] [PubMed] [Google Scholar]
- Tulloh BR, Collopy BT. Positive correlation between blood alcohol level and ISS in road trauma. Injury. 1994;25:539–541. doi: 10.1016/0020-1383(94)90097-3. [DOI] [PubMed] [Google Scholar]
- Waller PF, Hansen AR. The potentiating effects of alcohol on injury: a clinical study. 33rd Annual Proceedings of the Association for the Advancement of Automotive Medicine; 1 – 15, 1989. [Google Scholar]
- Waller JA. Methodologic issues in hospital-based injury research. Journal of Trauma. 1988;28:1632–1636. doi: 10.1097/00005373-198812000-00003. [DOI] [PubMed] [Google Scholar]
- Waller PF, Hill EM, Maio RF, Blow FC, Singer K, Schaeffer N. Abstract: Alcohol Potentiates Motor Vehicle Crash Injury. Academic Emergency Medicine. 1999;6:490. [Google Scholar]
- Waller PF, Stewart JR, Hansen AR, Stutts JC, Popkin CL, Rodgman EA. The potentiating effects of alcohol on driver injury. JAMA. 1986;256:1461–1466. [PubMed] [Google Scholar]
- Ward RE, Flynn TC, Miller PW, Blaisdell WF. Effects of Ethanol ingestion on the severity and outcome of trauma. The American Journal of Surgery. 1982;144:153–157. doi: 10.1016/0002-9610(82)90617-1. [DOI] [PubMed] [Google Scholar]