Abstract
While there is a great deal of data documenting the etiologic role alcohol use plays in crash culpability, there is a dearth of data for other drugs. The purpose of this study was to assess crash culpability for single drug use among injured drivers admitted to a regional trauma center. This study is the largest of its kind involving trauma center patients. Clinical toxicology results obtained for patient care were linked to police crash reports containing a field attributing crash culpability. Drugs studied were alcohol, cocaine, and marijuana. As expected crash culpability was strongly associated with pre-crash alcohol use. In contrast, for both men and women, this study did not find an association between crash culpability and marijuana use. The data documents a significant association between cocaine use and crash culpability for both sexes and for drivers 21 to 40 years of age. This is the first large study to assess for crash culpability among injured drivers relative to cocaine use.
Each year approximately 42 to 43,000 people die annually as the result of vehicular crashes. (NHTSA, 2005) For the decade 1994 through 2003, alcohol was a factor in 40–43% fatal injury crashes - the fatally injured person being either a vehicular occupant or pedestrian. Specifically 25 to 29% of drivers of cars and light trucks involved in those crashes were alcohol positive. Further, it is estimated that 80% or more of those drivers had blood alcohol concentrations (BAC) of 80 mg/dl or greater. (NHTSA, 2005)
In 1964 Borkenstein and colleagues compared BAC data for drivers involved in crashes (300 drivers were killed or injured) with drivers who had not crashed. That seminal study and others (AMA, 1986; Zador et al, 2000) clearly documented the etiologic role alcohol plays in the causation of both fatal and non-fatal vehicular crashes. This is true at BAC levels ≥80 mg/dl – which defines impaired driving in the United States – and lower levels.
Almost 50% of patients admitted to the 405 trauma centers in the American College of Surgeons’ National Trauma Data Bank were occupants of vehicular crashes, of whom over two-thirds were drivers. (ACS, 2005) Among injured drivers admitted to these centers, 26% to 52% have a positive BAC test at the time of admission (Soderstrom et al,1997; Rivara et al, 1994; Maio et al, 1997; Cornwell et al, 1999).
Among injured drivers treated in emergency departments (EDs), 34–53% of BAC negative drivers were assessed to be crash culpable, compared with 54–90% of BAC+ drivers. (Terhune, 1982; Lowenstein et al, 2001; Longo et al, 2000). In contrast high crash culpability rates have been documented among select groups of injured drivers admitted to trauma centers. Among 52 drivers admitted to a Virginia trauma center, police indicated that 98% were crash culpable (Maull et al, 1984). In a subsequent study of 58 drivers admitted to the trauma center involved with this current project, we found that 65% of drivers who were not alcohol impaired, i.e., BAC <80 mg/dl, were crash culpable, while drivers with higher levels were crash culpable 93% of the time (Soderstrom et al, 1990).
Compared to alcohol, much less is known about the use of “other drugs” among vehicular crash victims admitted to trauma centers. Only a few studies provide information about injured drivers and pre-crash drug use. A 1992 report (Kirby et al) found the following percentages of toxicology positive test results for 201 drivers: alcohol, 32%; benzodiazepines, 20%; cocaine, 5%; opiates, 5%; amphetamines, 2%; and barbiturates, 1%. In an earlier report, (Soderstrom et al, 1988) we documented that 32% of 393 automobile and 39% of 70 motorcycle drivers admitted to the R Adams Cowley Shock Trauma Center tested positive for delta-9-tetrahydrocannabinol (delta-9-THC), the active marijuana ingredient detected in the serum. In a later study (Soderstrom et al, 1995), we found that 2.7% of automobile drivers and 32% of motorcycle drivers tested positive for delta-9-THC activity. Further, urine toxicology tests for 1077 automobile and motorcycle drivers yielded the following test positive results: cocaine, 5% automobile vs. 8% motorcycle; phencyclidine, 1.5% automobile vs. 3.1% motorcycle.
To our knowledge the only studies assessing crash culpability and substance use all involve patients treated in EDs. In Terhune’s 1982 study of 497 drivers, crash culpability was assessed relative to marijuana (serum tests of delta-9-THC) and other drugs. Culpability rates were: 34% for drug negative patients, 53% for marijuana, and 50% for those with alcohol in combination with another drug. Findings were limited by the small number of patients who tested positive for drugs: delta-9-THC, 6.3% (n=31); and ≤2% for other drugs. In a recent study (Lowenstein et al, 2001) of injured drivers treated in an ED, crash culpability rates were: toxicology negative, 48%; alcohol alone, 74%; non-alcohol drugs, 51%; marijuana alone, 50%; alcohol and a non-alcohol drug, 76%. In that study only 23 patients were BAC+, only 67 tested positive for non-alcohol drugs, and cocaine and opiates “were seldom found.” Another recent study, (Longo et al, 2000) assessed crash culpability among 2500 injured drivers admitted to Australian Accident and Emergency Units. While high rates of culpability were found for BAC+ patients (90%) and those using other drugs alone or in combination with alcohol (70%–94%), sample sizes for drugs other than alcohol were small, with the highest number being 46 drivers testing positive for benzodiazepines. Patients were not tested for cocaine and opiates.
STUDY OBJECTIVE AND HYPOTHESES
The goal of this study was to assess crash culpability in a large cohort of injured vehicular crash drivers admitted to a regional trauma center who tested positive for at least one drug of abuse. The drugs studied were alcohol, cocaine, and marijuana.
Culpability among patients with positive toxicology test results were compared with patients who had negative results. Further analyses examined culpability relative to sex and age. Our hypothesis was that injured drivers with positive toxicology results would more often be crash culpable. Further, the youngest drivers, because of inexperience, who were toxicology positive would more often be culpable compared to older toxicology positive patients.
METHODS
IRB
This study was approved by the Institutional Review Board of the University of Maryland School of Medicine.
Clinical Study Site
The R Adams Cowley Shock Trauma Center (STC) of the University of Maryland Medical Center, is the hub of the emergency medical system in Maryland. Maryland is one of five states meeting all of the criteria for a fully developed system of trauma care. (Bass et al, 1998) The Center, located in Baltimore, MD, serves as a regional adult trauma center for Central Maryland, the most populated region of the state, and as an area wide trauma center for a quadrant of Baltimore City. Hence, the Center’s patients are transported from rural and suburban (usually by helicopter) and urban (transport by ambulance) settings. The center’s patient profile, relative to age, sex, and mechanism of injury, reflects that of the aggregate of patients treated in U.S. trauma centers. (ACS, 2005)
Alcohol/Other drug testing
For over three decades alcohol and other drug testing has been performed routinely for patients admitted to the trauma center. Testing results are used for patient management, not for legal reasons, e.g., identification of drunk drivers. Drug tests are conducted for a number of licit and illicit drugs. According to clinical protocols in the trauma center, alcohol use is determined by measurement of a BAC and drug use is determined from a urine specimen. Alcohol testing rates are higher than other drug testing rates because, while an admitting blood specimen is needed for clinical management of almost all patients, the same is not true relative to urine samples.
A positive blood test result for alcohol documents use at the time of injury. In contrast, a positive drug test result does not necessarily document use in close proximity to the time of injury.
Research Center and Clinical Toxicology Database
The Charles McC. Mathias, Jr., National Study Center (NSC) for Trauma and EMS of the University of Maryland, Baltimore serves primarily as a research support arm for the Shock Trauma Center. The NSC houses and maintains a confidential Clinical Toxicology Database of STC patients, the largest active one of its kind. A previous analysis of toxicology results from 1985 through 2000 for almost 60,000 patients indicated that the most commonly used drugs were alcohol, marijuana, opiates and cocaine (Soderstrom et al, 2001). For this study we assessed culpability only for alcohol (expressed as a BAC level), cocaine (COC) and marijuana (MAR). In the mid-1990s the practice of giving opiates for pain management shortly after admission was begun. It was not possible to distinguish pre-injury opiate use from therapeutically administered opiates after admission without an extensive time consuming chart by chart audit. Hence, opiates were not assessed in this study.
Statewide Hospital Discharge Data (HSCRC)
For all patients admitted to the 51 acute care hospitals in Maryland, information on diagnoses, length of stay, mechanism of injury, and hospital charges are detailed in the Health Services Cost Review Commission (HSCRC) database. The HSCRC data is available for research and evaluation purposes in both confidential and non-confidential (without patient identifiers) formats. The NSC has been granted access to the confidential state data.
Maryland Automated Accident Reporting System (MAARS)
Data on all police-reported motor vehicle crashes as well as pedestrian and motorcycle incidents occurring in traffic are included in the MAARS database. MAARS data are compiled by crash, vehicle type and person type (e.g., driver, pedestrian) and encompass a broad scope of information regarding circumstances surrounding the crash and characteristics of the vehicles and occupants involved. Occupant information collected by the police includes age, sex, date of birth, and address. In addition, a field is reserved for an indication of the party determined by the attending policeman to be “at fault”.
According to the Maryland State Police Department, officers are specifically instructed to consider all possible evidence and information pertaining to the investigation of the crash before ascertaining who should be deemed at fault, or culpable, for the incident. Such information should include, but is not limited to, that which is collected regarding drivers, witnesses, vehicle condition, and the surrounding environment (e.g., roadway, weather, traffic).
For MAARS reports that did not contain a determination of who was at fault, driver culpability was scored by applying the “culpability scale” advocated by Terhune (1982) as a modification of the one developed by Perchonok (1978). These determinations were made by members of the study team as per the methodology which was used in our prior study (Soderstrom et al, 1990). Initially, there were 867 records with missing culpability, encompassing 13.3% of all linked data. To reduce the percentage of missing culpability cases, we utilized multiple sources to assist in the determination of culpability. We were able to determine culpability for 292 cases by reviewing hard copies of police reports, and 31 by obtaining driver citation information from the Maryland Motor Vehicle Administration. For all of the 867 cases, only drivers having the most definitive determination of culpability (i.e., obviously culpable or clearly not responsible for the crash) were included in the analysis. As a result of these efforts, the total of missing culpability cases was reduced from 867 to 372 (5.7%).
Data Management
Linkage and Identification of Study Subjects
Five years (1997 through 2001) of HSCRC and MAARS data were linked, using probabilistic linkage techniques (Jaro, 1995; Jaro, 1998), to obtain information on all drivers admitted to the STC in Baltimore. The data linkage technique is based on a computation of odds ratios for variables common to both files; thus, some variables (e.g., sex) may have a smaller weight than other more specific variables (e.g., date of birth) when computing the probability of a match. Successful linkage is associated with the trade-off between an effective weighting scheme and the application of match probabilities. As weights and probabilities of a match among specific key variables are increased, accuracy is increased at the expense of incurring a smaller linkage rate. Conversely, as the linkage criteria are broadened, by a reduction of variable weights and probabilities, the percent match between the two databases will increase.
Probabilistic linkage of two unique databases that were created for entirely different purposes may not result in 100% one-toone match of corresponding records (Cook et al, 2000) The lack of unique identifiers that are common to both databases, the large number of injured drivers who are transported to hospitals other than the STC, and the unknown number of injury crashes that are not reported to the police are several reasons as to why this is so. However, for this report, the data linkage was enhanced by linking on non-unique key variables such as date of birth, age, gender, date, time, county and driver type (e.g., automobile, motorcycle).
Following the linkage effort, two approaches were taken to validate the resulting database and determine false positives (records that matched but should not have) and false negatives (records that did not match but should have) among the injured drivers admitted to the STC. First, hard copies of police crash reports and medical charts were examined for randomly sampled patients, and second, the final linked database was merged with the Maryland Trauma Registry and the drivers’ license file provided by the state Motor Vehicle Administration to compare agreements on key linkage variables. Both the sensitivity rate of the linkage effort (the proportion of true matches) and the specificity rate (the proportion of true non-matches) were determined to be 92%. These findings confirmed the validity of the probabilistic data linkage.
Data Analysis
Positive and negative toxicology test results were indicated by BAC+ (i.e., 20 mg/dl or higher) and BAC− (< 20 mg/dl) for alcohol, COC+ and COC− for cocaine, and MAR+ and MAR− for marijuana, respectively. Age groups to be analyzed were defined as less than 21 years, 21 to 40 years, 41 to 60 years, and 61 years or older. Percentages and unadjusted odds ratios (OR) for crash culpability, along with corresponding 95% confidence intervals (CI), were calculated.
RESULTS
Following linkage, the resulting database included information on 6,518 drivers who were hospitalized at the STC during the five-year period. Approximately 85% (n = 5,573) of the 6,518 STC patients were drivers of automobiles, limousines, pick-up trucks, vans and recreational vehicles. These drivers were the basis of this report.
BAC levels were available for 95.9% (n = 5,342) and illicit drug test results were available for 45.5% (n = 2,537) of hospitalized drivers. Complete toxicology findings (i.e., alcohol, cocaine and marijuana) were obtained for 2,537 drivers. A comparison was conducted between those with and without complete toxicology screens to ascertain selection bias among the injured drivers over the five-year period. The proportion of drivers tested for alcohol, cocaine and marijuana use averaged approximately 45% over the 5-year period, with a low of 40.8% in 1997 and a high of 52.1% in 1998. Drivers with injuries of moderate to serious severity (Injury Severity Score [ISS] of 16 or higher) (AAAM, 1990) were more likely to be tested than were drivers with milder injuries (ISS < 16; 52.3% vs. 44.3%, respectively). However, the testing rates for males (45.4%) and females (45.7) were virtually identical and testing rates were similar within the four age groups: 42.6% (< 21 years), 46.7% (21 to 40 years), 45.4% (41 to 60 years), and 46.1% (> 60 years).
Positive Toxicology Results - overall
Approximately 40% of drivers with complete toxicology findings tested positive for some combination of the drugs studied. However, drivers were more likely to be positive for a single substance (30.2%) than for multiple substances (9.9%). The proportion of documented alcohol and cocaine positive cases were fairly consistent throughout the study period, ranging from 20.3% and 23.1% per year for alcohol, and 8.3% and 10.0% each year for cocaine. Marijuana use was substantially higher in the last two years of the study period, averaging 11.4% for 1998 and 1999, and 17.4% during 2000 and 2001.
Single substance use
Alcohol alone had the highest prevalence (19.1%), followed by marijuana alone (7.3%) and the combination of alcohol and marijuana (4.8%). The prevalence of cocaine use alone was 3.8%.
Crash culpability - overall
Information regarding the culpability of the driver was available for 94.8% of those with complete toxicology screens; almost three-quarters (73.8%) of drivers with available data were deemed to be at fault for their crash. In an effort to ascertain the culpability of drivers who tested positive for a specific drug, analyses of culpability were conducted in terms of each individual drug alone (i.e., among drivers who tested negative for the two remaining substances).
Crash culpability for single drugs of abuse
BAC+ drivers were significantly more likely to be culpable for their crash than were BAC− drivers (93.1% vs. 64.5%, OR = 7.45, 95% CI = [5.12–10.84]). COC+ drivers were also significantly more likely to be culpable for their crash than were COC− drivers (80.9% vs. 64.5%, OR = 2.33, 95% CI = [1.36–3.99]). MAR+ drivers, however, were no more likely than MAR− drivers to be at fault for their crash (68.2% vs. 64.5%, OR = 1.18, 95% CI = [0.84–1.64]).
Culpability by Sex
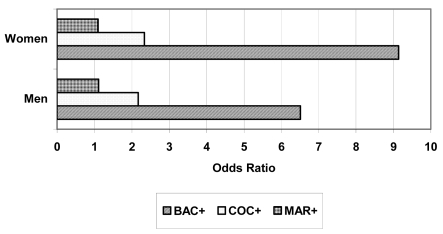
The odds of being culpable for BAC+ relative to BAC− were significantly high among both male and female drivers (Figure 1 and Table 1). However, these odds were about 40% higher for women than for men. In contrast, there was little difference between male and female culpability relative to cocaine or marijuana use. While the 95% confidence interval for females relative to cocaine use covered an odds ratio of 1.00, the skewness of the interval and the high upper limit of 6.35 indicate that women who are COC+, as well as men, are a crash risk.
Figure 1.
Odds of Culpability by Gender and Substance Use
Table 1.
Estimated Unadjusted Odds Ratios of Culpability For Effect of Substance Use Among Women and Men
| Effect | Sex | Odds Ratio | 95% CI for OR |
|---|---|---|---|
| BAC + vs BAC− | Women | 9.14 | 3.94 – 21.19 |
| BAC + vs BAC− | Men | 6.51 | 4.25 – 9.99 |
| COC+ vs COC− | Women | 2.34 | 0.86 – 6.35 |
| COC+ vs COC− | Men | 2.17 | 1.14 – 4.13 |
| MAR+ vs MAR− | Women | 1.10 | 0.56 – 2.15 |
| MAR+ vs MAR− | Men | 1.11 | 0.75 – 1.64 |
Culpability by Age
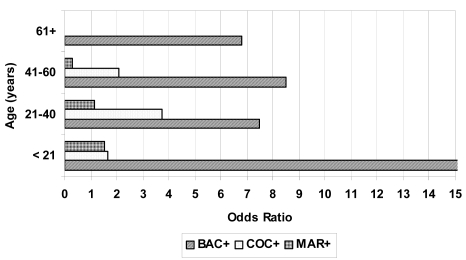
For each age group, however, alcohol was the primary substance responsible for crash causation. The odds of being culpable for BAC+ relative to BAC− was highest among drivers younger than age 21, as everyone in that age group who was BAC+ was at fault for their crash (Figure 2 and Table 2). In addition, the large upper confidence limit for elderly drivers suggests that those who are BAC+ may also be a crash risk. Drivers of age 21 to 40 had the highest odds of culpability for COC+ relative to COC−, and the odds for MAR+ relative to MAR− were not statistically significant for drivers aged 40 or younger. However, within the 41 to 60 year age group, drivers who were positive for marijuana were significantly less likely than those who tested negative for the drug to be considered at fault in a crash. Elderly drivers were not found to be either COC+ or MAR+; hence, no odds ratios were calculated for who were over 60.
Figure 2.
Odds of Culpability by Age Group and Substance Use
Table 2.
Estimated Unadjusted Odds Ratios of Culpability For Effect of Substance Use According to Age Group
| Effect | Age Group | Odds Ratio | 95% CI for OR |
|---|---|---|---|
| BAC + vs BAC− | <21 yrs | INF | ----- |
| BAC + vs BAC− | 21–40 yrs | 7.46 | 4.67 – 11.93 |
| BAC + vs BAC− | 41–60 yrs | 8.49 | 4.16 – 17.30 |
| BAC + vs BAC− | 61+ yrs | 6.81 | 0.90 – 51.75 |
| COC+ vs COC− | <21 yrs | 1.64 | 0.19 – 13.93 |
| COC+ vs COC− | 21–40 yrs | 3.76 | 1.74 – 8.13 |
| COC+ vs COC− | 41–60 yrs | 2.08 | 0.89 – 4.82 |
| COC+ vs COC− | 61+ yrs | ---- | ------ |
| MAR+ vs MAR− | <21 yrs | 1.53 | 0.76 – 2.98 |
| MAR+ vs MAR− | 21–40 yrs | 1.13 | 0.69 – 1.84 |
| MAR+ vs MAR− | 41–60 yrs | 0.31 | 0.12 – 0.81 |
| MAR+ vs MAR− | 61+ yrs | --- | ------ |
Culpability by Age and Sex
Although no statistically significant interactions between age and sex were documented, important non-significant differences between males and females were apparent for several age groups. The odds of being culpable for BAC+ relative to BAC− within the 41 to 60 year age group were much higher among women (OR=23.28, 95% CI=[3.09–175.21]) than among men (OR=6.21, 95% CI=[2.83–13.60]). However, men were almost solely responsible for the high odds of culpability for BAC+ within the oldest age group (see Table 2). Similarly, men were largely responsible for the inverse relationship of culpability found within the 41 to 60 year age group for MAR+ relative to MAR−.
DISCUSSION
This is the first study we believe to assess crash culpability relative to several drugs of abuse in a population of trauma center patients. A total of 2,537 patients had complete testing results available for the three substances under study. Because of the large cohort linked to crash reports, substantial numbers of patients were available to assess for crash culpability relative to single drug use.
Alcohol - overall
The overall proportion of patients testing BAC+, which ranged from 20–23% throughout the study period, is lower than the 33% prevalence noted from a 1988 Shock Trauma Center study (Soderstrom et al) and other trauma center studies (Rivara et al, 1989; Maio et al, 1997). As in the case of other studies of injured drivers treated in EDs or trauma centers, alcohol was found to be the most commonly used substance prior to crashing (Terhune, 1982; Kirby et al, 1992, Longo et al, 2000, Lillis et al, 1999) These studies are in contrast to the Lowenstein and colleagues’ 2001 ED report which found 17% testing positive for marijuana and 14% testing positive for alcohol.
The finding in this study that BAC+ patients had significantly higher crash culpability than BAC− patients (93% vs 65%) is consistent with other studies assessing crash culpability among patients treated in emergency departments (Terhune, 1982; Longo et al, 2000; Lowenstein et al, 2001) and our previous report (Soderstrom et al, 1990) from the trauma center involved in this study.
Non-alcohol drugs – testing and study limitations
A BAC+ state at the time of admission to the trauma center documents alcohol use immediately prior to injury. Further, a body of scientific study has clearly established that all individuals are impaired to some degree at levels of 80 mg/dl (AMA, 1986; Zador et al, 2000). The same cannot be said about other drugs of abuse, including cocaine and marijuana, which came under study in the current project.
Before discussing cocaine and marijuana findings from this study it is important to consider the limitations of urine tests. As noted in a recent review by Jones, Shinar and Walsh (2003), while blood samples allow direct measurement of the “parent” drug (the active drug) – as opposed to a urine test which usually detects metabolites – there is generally no agreement on plasma concentrations of drugs other than alcohol which can be designated as evidence of impairment. Urine tests detect metabolites of cocaine and marijuana use and do not provide evidence of a close temporal relationship between use and the crash necessitating admission to a trauma center. While the metabolites appear in the urine shortly after use, they are detectable for a number of days. In the case of cocaine, after cessation of use, urinary metabolites can be detected for about 48 hours (Ambre, 1985; Preston et al, 2002). In the case of chronic cocaine use, metabolites can be detected for up to an average of 3.4 days (Preston et al, 2002). Relative to marijuana, metabolites are detectable in the urine generally for at least three days or more even after smoking a single marijuana cigarette (Huestis et al. 1996).
In summary, while the current study does not provide evidence of cocaine and marijuana impairment, or use at the time of injury, it provides information about culpability relative to users of cocaine and marijuana admitted to a trauma center.
Cocaine
This is the first study to assess for crash culpability among injured drivers relative to cocaine use. Other studies of crash culpability of injured patients treated in EDs did not assess for crash culpability relative to cocaine either because the testing was not done (Longo et al, 2000), or very few patients were available for study (Terhune, 1982; Lowenstein et al, 2001). While only 3.8% of patients tested positive for cocaine use alone, 96 patients were available for study because of the large patient database.
The data document a significant association between cocaine use and crash culpability for males and for drivers of 21 to 40 years of age. Our study results are consistent with a Dutch prospective observational case-control study (Movig et al, 2004) in which the OR for personal injury in a crash was 2.04 for cocaine using drivers compared with non-cocaine using drivers.
While this study did not verify cocaine use proximal to the time of injury, the “window of time” during which cocaine is detectable is only about 48 hours. Hence, use proximal to the time of injury could have taken place in a substantial number of instances.
Marijuana
For both mean and women, this study did not find an association between crash culpability and marijuana use among male and female drivers. However, drivers of age 41 to 60 who were MAR+ were less likely to be crash culpable.
Our findings are consistent with other studies of injured drivers in which urine test results were studied (Longo et al, 2000; Lowenstein et al, 2001; Movig et al, 2004). Terhune’s 1982 crash culpability study which utilized δ-9-THC blood test results – and documented marijuana use at the time of injury – found a slightly higher percentage of MAR+ patients were crash culpable compared to patients who were both BAC+ and other drug positive, being 53% and 50%, respectively. (It is interesting that the patients in that study who tested negative for substance use had an overall crash culpability of only 34%, whereas in other studies, including the present one, crash culpability in toxicology negative patients ranged from 48–64% [Longo et al, 2000; Lowenstein et al, 2001]). In an Australian ED study, in which marijuana was confirmed in the blood of injured drivers, Longo and colleagues (2000) did find a significant increase in culpability among drivers testing positive for marijuana alone.
The lack of association between pre-injury marijuana use and crash culpability among injured drivers treated in acute care settings appears to contradict experimental and epidemiologic studies (Jones et al, 2003; Ramaekers et al, 2004). Indeed, one would expect them to be consistent with Drummer and associates’ (2004) case-control study of fatally injured drivers using blood test results for δ-9-THC. They found a strong association between marijuana use and crash culpability. This association was even stronger when alcohol was a factor in crashes. To clarify the role of marijuana use in crash culpability, a large study of injured patients treated in acute care settings using blood tests to assess for marijuana use proximal to time of injury would be quite useful.
Limitations of the Study
There are a number of limitations to this study. As previously noted, as opposed to alcohol test results, urine drug test results may not represent a close temporal relationship between use and the injury event. We were not able to study opiates because we could not distinguish whether positive opiate test results were from pre-injury use, or therapeutically administered opiates after admission. Finally, the research team had to rely on the crash culpability assessments of police officers.
CONCLUSIONS
This study documents for the first time that there is an association with pre-injury cocaine use and crash culpability in a large population of injured drivers admitted to a trauma center among males and drivers of 21 to 40 years of age. The study provides further documentation that crash culpability is linked to pre-injury alcohol use among both sexes and in all age groups. Finally, the study adds to the clinical body of literature suggesting that pre-injury marijuana alone is not associated with an increase in crash culpability.
ACKNOWLEDGEMENT
This project was supported by a Robert Wood Johnson Foundation Substance Abuse Policy Research Program grant (#04848).
REFERENCES
- Ambre J. The urinary excretion of cocaine and metabolites in humans; a kinetic analysis of published data. J Anal Toxicol. 1985;9:241–245. doi: 10.1093/jat/9.6.241. [DOI] [PubMed] [Google Scholar]
- American College of Surgeons Committee on Trauma. National Trauma Data Bank Report 2004. Chicago, Illinois: Available on the web at: http://www.facs.org/trauma/ntdb.html. [Google Scholar]
- Association for the Advancement of Automotive Medicine. The Abbreviated Injury Scale. Des Plaines; Illinois: 1990. [Google Scholar]
- Bass RR, Gainer PS, Carlini AR. Update on trauma system development in the United States. J Trauma. 1999;47:S15–S21. doi: 10.1097/00005373-199909001-00005. [DOI] [PubMed] [Google Scholar]
- Borkenstein RF, Crowther RF, Shumate RP, et al. The role of the drinking driver in traffic accidents. Bloomington, IN: Indiana University, Department of Police Administration; 1964. [Google Scholar]
- Cook LJ, Knight S, Olson LM, et al. Motor vehicle crash characteristics and medical outcomes among older drivers in Utah, 1992–1995. Ann Emerg Med. 2000;35:585–591. [PubMed] [Google Scholar]
- Cornwell EE, III, Belzberg H, Velhamos G, et al. The prevalence and effect of alcohol and drug abuse on cohort-matched critically injured patients. Am Surg. 1998;64:461–465. [PubMed] [Google Scholar]
- Council on Scientific Affairs of the American Medical Association. Alcohol and the driver. JAMA. 1986;255:522–527. [PubMed] [Google Scholar]
- Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36:239–248. doi: 10.1016/s0001-4575(02)00153-7. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Mitchell JM, Cone EJ. Urinary excretion profiles of 11- nor-9-carboxy-delta-9-tretrahydocannabinol in humans after single smokes doses o marijuana. J Anal Toxicol. 1996;20:441–452. doi: 10.1093/jat/20.6.441. [DOI] [PubMed] [Google Scholar]
- Jaro MA. Advances in record-linkage methodology as applied to matching the 1985 census of Tampa, Florida. Journal of the American Statistical Association. 1989;84:16–22. [Google Scholar]
- Jaro MA. Probabilistic linkage of large public health data files. Statistics in Medicine. 1995;14:491–498. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- Jones RK, Shinar D, Walsh JM. State of Knowledge of Drug- Impaired Driving. National Highway Traffic Safety Administration. NHTSA, U.S. Department of Transportation; Washington, DC: Sep, 2003. Report No. DOT HS 809 642. [Google Scholar]
- Kirby JM, Maull KI, Fain W. Comparability of alcohol and other drug use in injured drivers. J South Med Association. 1992;85:800–802. doi: 10.1097/00007611-199208000-00003. [DOI] [PubMed] [Google Scholar]
- Lillis RP, Good RG, Kwong T, et al. Incidence of drug use among drivers treated in emergency departments. (Poster abstract.) 43rd Annual Proceedings, Association for the Advancement of Automotive Medicine; September 20–21, 1999; pp. 469–470. [Google Scholar]
- Longo MC, Hunter CE, Lokan RJ, et al. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability – Part II: the relationship between drug prevalence and drug concentration, and driver culpability. Accid Anal Prev. 2000;32:623–632. doi: 10.1016/s0001-4575(99)00110-4. [DOI] [PubMed] [Google Scholar]
- Lowenstein SR, Koziol-McLain J. Drugs and traffic crash responsibility: a study of injured motorists in Colorado. J Trauma. 2001;50:313–320. doi: 10.1097/00005373-200102000-00019. [DOI] [PubMed] [Google Scholar]
- Maio RF, Waller PF, Blow FC, et al. Alcohol abuse/dependence in motor vehicle crash victims presenting to the emergency department. Acad Emerg Med. 1997;4:256–262. doi: 10.1111/j.1553-2712.1997.tb03545.x. [DOI] [PubMed] [Google Scholar]
- Maull KI, Kinning LS, Hickman JK. Culpability and accountability of hospitalized injured alcohol-impaired drivers. JAMA. 1984;252:1880–1883. [PubMed] [Google Scholar]
- Movig KLL, Mathijssen MPM, Nagel PHA, et al. Psychoactive substance use and the risk of motor vehicle accidents. Accid Anal Prev. 2004;36:631–636. doi: 10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration (NHTSA) Traffic Safety Facts 2003. NHTSA, U.S. Department of Transportation; Washington, DC: Jan, 2005. Report No. DOT HS 808 775. [Google Scholar]
- Perchonok K. Identification of Specific Problems and Countermeasures: Targets for Reducing Alcohol Related Casualties. National Highway Traffic Safety Administration, U.S. Department of Transportation; Washington, DC: 1978. Report No. DOT HS 803 716. [Google Scholar]
- Preston KL, Epstein DH, Cone EJ, et al. Urinary elimination of cocaine metabolites in chronic cocaine users during cessation. J Anal Toxicol. 2002;26:393–400. doi: 10.1093/jat/26.7.393. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of Motor vehicle crashes after cannabis use. Drug Alcohol Dependence. 2004;73:109–119. doi: 10.1016/j.drugalcdep.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Rivara FP, Jurkovich GJ, Gurney JG, et al. The magnitude of acute and chronic abuse in trauma patients. Arch Surg. 1994;128:907–913. doi: 10.1001/archsurg.1993.01420200081015. [DOI] [PubMed] [Google Scholar]
- Soderstrom CA, Kerns TJ, Ho SM, et al. Alcoholism at the time of injury among trauma center patients: Vehicular crash victims compared with other patients. Accid Anal Prev. 1997;29:715–721. doi: 10.1016/s0001-4575(97)00040-7. [DOI] [PubMed] [Google Scholar]
- Soderstrom CA, Birschbach J, Dischinger PC. Injured drivers and alcohol use: culpability, convictions, pre- and post-crash driving history. J Trauma. 1990;30:1208–1214. [PubMed] [Google Scholar]
- Soderstrom CA, Dischinger PC, Kerns TJ, et al. Marijuana and other drug use among automobile and motorcycle drivers treated at a trauma center. Accid Anal & Prev. 1995;27:131–135. doi: 10.1016/0001-4575(94)00043-l. [DOI] [PubMed] [Google Scholar]
- Soderstrom CA, Trifillis AL, Shankar BS, et al. Marijuana and alcohol use among 1023 trauma patients: A prospective study. Arch Surg. 1988;123:733–737. doi: 10.1001/archsurg.1988.01400300079013. [DOI] [PubMed] [Google Scholar]
- Soderstrom CA, Dischinger PC, Kerns TJ, et al. Epidemic increases in cocaine and opiate use by trauma center patients. Documentation with a large clinical toxicology database. J Trauma. 2001;51:557–564. doi: 10.1097/00005373-200109000-00024. [DOI] [PubMed] [Google Scholar]
- Terhune KW. The Role of Alcohol, Marijuana, and Other Drugs in the Accidents of Injured Drivers. Vol. 1. National Highway Traffic Safety Administration, U.S. Department of Transportation; Springfield, VA: Jan, 1982. Report No. DOT HS 806 199. [Google Scholar]
- Terhune KW. Problems and methods in studying drug crash effects. Alcohol Drugs and Driving, Abstracts and Reviews. 1986;2:1–13. [Google Scholar]
- Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: an update using 1996 data. J Stud on Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]