Abstract
Hypothesis: A second injury in the same body region is associated with lower mortality than a second injury in a different body region, independently of injury severity and body region.
Methods: The population consisted of 15,200 patients with two or more injuries from level I trauma centers in Quebec. The mortality odds ratio of having a same-region second injury (SR) as opposed to a different-region second injury (DR) was assessed.
Results: Patients with a SR had 43% lower odds of mortality when compared to patients with a DR.
Conclusion: A second injury in the same body region is associated with lower mortality than a second injury in a different body region.
The Abbreviated Injury Scale (AIS) coding system was first introduced in 1971 and has been updated regularly since [Copes, Sacco, Champion, 1971]. The Injury Severity Score (ISS) was introduced in 1974 to summarize AIS severity codes for patients with multiple injuries [Baker, O’Neill, Haddon, 1974]. The ISS, calculated as the sum of squares of the highest AIS severity codes of three worst injured body regions, has been criticized for many reasons but particularly because it does not account for more than one injury in the same body region [Champion, Sacco, Copes, 1995]. In 1997, Osler et al. introduced the New Injury Severity Score (NISS) to overcome this limitation (1997). It is calculated as the sum of squares of the AIS severity code of the three worst injuries, regardless of body region. The NISS appeared to be clinically more logical as, for example, a patient with two head injuries of AIS=5 and one extremity injury of AIS=2 would have an ISS of 29 but a NISS of 54. The NISS has been reported to produce very different severity scores to the ISS (62% of a trauma registry population with NISS>ISS)5. However, surprisingly, the NISS has been found to be equivalent or only slightly superior to the ISS at predicting mortality in a general trauma population [Lavoie, Moore, Lesage, 2004] [Meredith, Evans, Kilgo, 2002] [Sacco, MacKenzie, Champion, 1999]. We hypothesized that this was because a second injury in the same body region is associated with less mortality than a second injury in a different body region, independent of injury severity.
METHODS
The study population was drawn from the trauma registries of the four level I trauma centers in the province of Quebec, Canada; Sacré-Coeur Hospital, Montreal General Hospital and Charles-Lemoine hospital in the region of Montreal, and Enfant-Jésus Hospital in Quebec City. Patients are included in these registries according to the following criteria; hospital stay of 3 or more days, admission to the Intensive Care Unit (ICU), death following trauma or transfer from another hospital. Deaths on arrival, isolated hip fractures and patients under 16 years of age were excluded. Patients with penetrating injuries were also excluded since their small number (3.5% of patients) precluded analyses in this particular subgroup. Between April 1998 and March 2004, 20,462 patients were available for analyses.
AIS coding was performed by trained medical archivists from patient files using the 1990 version of the AIS coding system [Association for the Advancement of Automotive Medicine, 1990]. Loss of consciousness AIS codes were only considered if a patient had no coded anatomic head injury of equal or greater severity. This project was approved by the ethics review board of the CHAUQ and by the ‘Commission d’accès à l’information du Québec’.
Analyses were performed among patients with at least two injuries. Injuries were ranked by injury severity with the most severe first. The two worst injuries were considered. Patients with a first or second external injury were excluded as external injuries can occur in any body region. A binary variable was created to identify patients with their two worst injuries in the same body region (SR) and to those with their two worst injuries in different body regions (DR). AIS codes were divided into seven body regions for creation of this variable as follows: Head, face, thorax, abdomen, spine, upper extremities and lower extremities. Only 20 patients had their worst injury in the neck region. Neck injuries were therefore combined with head injuries. Multiple logistic regression models were then built to assess the odds of mortality among patients with a SR compared to those with a DR, while adjusting for confounding variables. The following variables were considered as possible confounders: Severity of the first and second injury (AIS), age (0–64, 65–74,75–84, ≥85) and region of the first and second injury. The effect of the severity and body region of additional injuries was also assessed.
The possibility of effect modification due to injury body region, injury severity, age (as a proxy for co-morbidities) and injury mechanism was explored by performing sensitivity analysis in sub groups. Finally, mortality proportions in SR and DR groups were compared according to all specific first/second region/AIS combinations with at least 50 subjects in each exposure group. All analyses were performed with SAS software.
RESULTS
A total of 15,330 patients (75%) had two or more injuries. One hundred and thirty patients (0.8%) were excluded since they had a first or second external injury. Of the remaining 15,200 patients, 9,331 (61%) had a SR.
Patients in the SR group were slightly younger and had greater injury severity than those in the DR group (Table 1). Motor vehicle collisions were the most frequent injury mechanism in the SR group whereas falls were most frequent in the DR group.
Table 1.
Description of the study population
| Variable | N | SR (%) | DR (%) | |
|---|---|---|---|---|
| Age | <65 | 11,006 | 70.2 | 73.8 |
| 65–74 | 1,666 | 10.7 | 11.1 | |
| 75–84 | 1,671 | 12.1 | 10.3 | |
| ≥85 | 857 | 7.0 | 4.8 | |
| AIS worst injury | 1/2 | 3,478 | 21.2 | 25.6 |
| 3 | 6,279 | 36.7 | 48.7 | |
| 4 | 2,554 | 17.1 | 16.3 | |
| 5/6 | 2,889 | 25.0 | 9.4 | |
| Injury mechanism | Motor vehicle collision | 6,519 | 52.3 | 37.1 |
| Fall | 6,490 | 38.4 | 45.4 | |
| Firearm / stab | 73 | 0.6 | 0.40 | |
| Blunt | 1,356 | 6.2 | 10.6 | |
| Other | 762 | 2.7 | 6.5 |
SR: same region second injury; DR: different region second injury; AIS: Abbreviated Injury Scale, MVC: motor vehicle collision
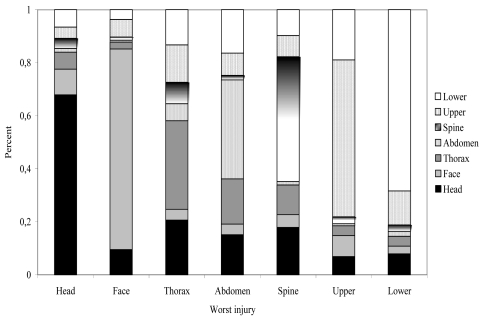
The most frequent body region of the first (worst) injury was the head (39%), followed by the lower extremities (25%), upper extremities (11%), the spine (10%), the thorax (9%), the face (4%) and the abdomen (2%). Patients with a first injury of the head, face, lower and upper extremities were more likely to have their second injury in the same region whereas patients with a first thoracic, abdominal or spinal injury were less likely to have their second injury in the same region (Figure 1). The most frequent second region for each first region was the head for the face (10%), thorax (21%) and spine (18%), the face for the head (10%), the thorax for the abdomen (17%) the upper extremities for the lower extremities (13%) and the lower extremities for the upper extremities (19%), (Figure 1).
Figure 1.
Body regions for first and second injuries.
Mortality was 8.8% globally, 10.3% among patients with a SR and 6.4% among patients with a DR. Table 2 shows the results of logistic regression models with and without adjustment for possibly confounding variables. The crude OR indicates an increased risk of mortality for patients with a SR compared to those with a DR. However, after adjustment for the severity of the first two injuries, age and the region of the first and second injury those with a SR had a 43% lower risk of mortality than those with a DR (OR=0.57 95% CI 0.46–0.71). Adding the severity and region of additional injuries to the model did not change the effect estimate.
Table 2.
Crude and adjusted Odds Ratios (OR) of mortality associated with having a same region as opposed to a different region second injury
| Model | OR | 95% CI |
|---|---|---|
| Crude | 1.68 | 1.48–1.90 |
| Adjusted* | 0.57 | 0.46–0.71 |
OR: Odds Ratio, CI: Confidence Interval
Adjusted for are adjusted for age and the severity and the region of first and second injuries
Analyses performed in population sub-groups are shown in Table 3. A SR had a significantly lower risk of mortality than a DR in the sub group of patients with two severe injuries (AIS≥4) and the sub group with no additional injuries. When analyses were stratified for the region of the first injury, OR indicated lower mortality for a SR in 5 out of seven first injury regions. For the abdomen and lower extremities, an OR greater than one was observed but was not statistically significant. Analyses stratified for the severity of the first injury revealed OR consistently lower than one for moderate to severe injuries but no effect for minor injuries (AIS=1/2). Results were consistent for patients under 65 years old and those 65 years old or older. OR were also homogeneous for the two most important injury mechanisms in our population: Motor Vehicle Collisions and falls.
Table 3.
Sensitivity analysis: Is the odds ratio of mortality associated with a same region compared to a different region second injury consistent in all population sub-groups?
| Population | OR* | 95% CI | |
|---|---|---|---|
| AIS1 ≥4, AIS2 ≥4† | 0.59 | 0.45–0.77 | |
| No more than two injuries‡ | 0.58 | 0.36–0.94 | |
| Region of first injury | Head | 0.30 | 0.20–0.43 |
| Face | 0.69 | 0.14–3.35 | |
| Thorax | 0.79 | 0.36–1.76 | |
| Abdomen | 1.23 | 0.30–5.07 | |
| Spine | 0.20 | 0.07–0.57 | |
| Upper extremities | 0.33 | 0.10–1.15 | |
| Lower extremities | 1.10 | 0.41–2.91 | |
| AIS of first injury | 1/2 | 1.00 | 0.53–1.69 |
| 3 | 0.58 | 0.42–0.81 | |
| 4 | 0.47 | 0.32–0.71 | |
| 5/6 | 0.72 | 0.58–0.89 | |
| Age | <65 | 0.52 | 0.35–0.76 |
| ≥65 | 0.58 | 0.44–0.75 | |
| Injury mechanism | MVC | 0.50 | 0.35–0.72 |
| Fall | 0.60 | 0.45–0.80 |
OR: Odds Ratio, CI: Confidence Interval, AIS: Abbreviated Injury Scale, MVC: motor vehicle collision.
OR are adjusted for age and the severity and the region of first and second injuries when appropriate
n=2,825,
n=3,863
Table 4 presents mortality proportions for all region*AIS subgroups with AIS≥3 and at least 50 patients in each SR/DR group. SR mortality was significantly lower than DR mortality for 7/9 subgroups. This difference was statistically significant for 6 sub-groups. Contradictory results observed for head/spine and lower/upper extremity combinations were not statistically significant.
Table 4.
Mortality according to combinations of body region and AIS.
| First region, (second region)* | AIS1, AIS2 | N | Mortality SR (%) | Mortality DR (%) | p-value |
|---|---|---|---|---|---|
| Head, (head/thorax) | 4,4 | 581 | 4.5 | 12.5 | 0.01 |
| Head, (head/thorax) | 5,4 | 1081 | 28.5 | 42.1 | 0.01 |
| Head, (head/thorax) | 5,3 | 3199 | 25.1 | 72.7 | <0.0001 |
| Head, (head/thorax) | 5,5 | 848 | 46.6 | 80.0 | 0.0003 |
| Head, (head/spine) | 5,5 | 834 | 46.6 | 25.0 | 0.1 |
| Head, (head/lower extremities) | 5,3 | 399 | 25.1 | 45.5 | 0.01 |
| Thorax, (thorax/lower extremities) | 4,3 | 676 | 4.9 | 10.2 | 0.2 |
| Lower extremities, (lower/upper extremities) | 3,3 | 898 | 4.6 | 3.9 | 0.7 |
| Lower extremities, (lower/upper extremities) | 3,2 | 1106 | 0.9 | 6.9 | <0.0001 |
Cases with a high probability of mortality are used (AIS ≥3). All combinations providing over 50 patients in each SR/DR group are shown.
DISCUSSION
A second injury in the same body region is associated with less mortality than a second injury in a different body region. Patients with a SR have higher crude mortality but this is explained by the fact that SR are associated with higher injury severity, probably because more than one injury in the same region is synonym of greater impact on injury. Therefore, for the same injury severity, a patient with two injuries in the same body region has 40% lower probability of dying than a patient with two injuries in different body regions.
The results of this study give an explanation as to why the NISS offers only limited improvement over the ISS in terms of mortality prediction. The ISS only accounts for the worst injury per body region whereas the NISS considers all injuries in a body region. This study does not endorse the use of the ISS over the NISS. While the improvement of the NISS over the ISS has been shown to be modest or even null in a general trauma population, it is considerably better in high-severity sub-populations such as head-injured patients [Lavoie et al, 2004].
Two possible weaknesses of the study are worth discussion. Firstly, results cannot necessarily be generalized to trauma populations with penetrating trauma. Unfortunately, our population did not include enough penetrating injury for analyses to be carried out in this important subgroup. Secondly, misclassification due to differing regions of additional injuries could have biased our results. If a large proportion of patients in the SR group had additional severe injuries in a different body region, the OR observed in our study would tend to underestimate the true effect. In fact, among 9,331 SR patients, 1,540 (16.5%) had additional moderate to severe (AIS>2) injuries in a different body region. Despite this, we decided to present injuries based on the worst two injuries only because of the difficulty of controlling for the severity and the region of up to ten injuries and the complexity of stratified analysis when more than two injuries were considered. We performed sensitivity analysis to evaluate the impact of the misclassification problem in three specific subpopulations; 1) Patients with only two injuries, 2) Exclusion of all SR patients with additional different-region injuries of AIS>2, 3) SR patients with additional different-region injuries of AIS>2 transferred to the DR group. Results were as follows (OR (95% CI)); 1) 0.58 (0.36–0.94), 2) 0.58 (0.47–0.72), 3) 0.68 (0.59–0.79). Results of sensitivity analysis therefore support the study hypothesis and indicate that misclassification bias was not a problem in our analyses.
The results of subgroup analyses suggest that the effect observed in this study is not due to a foible in the AIS severity scoring system caused by differing mortality for different body regions. OR were less than one for all but two body regions. An OR close to one for the lower extremities and the abdomen indicates that these regions may be the exception to the rule. Nor is the observed effect due to patients with a DR having more frequent or more severe additional injuries, as adjustment for the number and severity of additional injuries didn’t alter OR estimates. OR were also consistent when stratified for the severity of the first injury, with one exception; no effect was observed among patients with minor injuries (AIS=1/2). This was to be expected however, as mortality among these patients is generally due to factors other than the injury itself (e.g. co morbidities). Analysis repeated for each of the four trauma centers also revealed consistent results between centers (results not shown). The effect observed could, at least in part, be due to severity misclassification inherent to AIS coding, especially present in early deaths in the absence of autopsy. If injuries were missed or underestimated more frequently in patients with DR than those with SR (the description of a second injury in the same region could be an indicator of better injury description), the effect observed would overestimate the true effect. However, it is equally likely that injuries were missed or underestimated more frequently in patients with SR (SR being more severe could have more early deaths), which would lead to an underestimation of the effect.
The phenomenon observed in this study is therefore likely to be due to physiological, clinical or organizational factors. From a physiological point of view, compensation may be better for two same-region injuries than for two different-region injuries. This could be due to the fact that the two injuries are not truly independent: adjacent injuries (i.e. is a comminuted fracture of the lower third of the shaft of the femur truly a separate injury from a supracondylar fracture on the same side?), or one injury being the result of another (i.e. brain haematoma followed by brain oedema or head injury followed by loss of consciousness). This latter hypothesis would apply to few injury combinations, however, and is therefore unlikely to entirely explain the large effect observed in our study. From a clinical point of view, it is easier to treat two injuries that are physically close as interventionists can concentrate on one area. From an organizational point of view, injuries in two body areas often require very different care approaches. This entails relying on the availability of different specialists and equipment, and often leads to one of the injuries being left unattended.
CONCLUSION
A second injury in the same body region has a lower risk of mortality than a second injury in a different body region. The results of this study explain, at least in part, why the NISS offers little improvement over the ISS for predicting mortality in a general trauma population. Our work suggests that the reasons behind this mortality difference could be physiological, clinical or organizational. Apart from its use in the development of anatomical injury severity measures, this study may therefore have clinical and/or organizational implications for the improvement of treatment strategies among patients with multiple injuries.
REFERENCES
- Association for the Advancement of Automotive Medicine. Abbreviated Injury Scale - 1990 revision. Des Plains, IL. USA: [Google Scholar]
- Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- Champion HR, Sacco WJ, Copes W. Injury severity scoring again. J Trauma. 1995;38:94–95. doi: 10.1097/00005373-199501000-00024. [DOI] [PubMed] [Google Scholar]
- Copes WS, Sacco WJ, Champion HR, Bain LW. Progress in Characterizing Anatomic Injury. 33rd annual proceedings, Association for the Advancement of Automotive Medicine; October 1989. [Google Scholar]
- Lavoie A, Moore L, Lesage N, et al. The new injury severity score - a more accurate predictor of in-hospital mortality than the Injury Severity Score. J Trauma. 2004;56:1312–1320. doi: 10.1097/01.ta.0000075342.36072.ef. [DOI] [PubMed] [Google Scholar]
- Meredith JW, Evans MS, Kilgo PD, et al. A Comparison of the Abilities of Nine Scoring Algorithms in Predicting Mortality. J Trauma. 2002;53:621–629. doi: 10.1097/00005373-200210000-00001. [DOI] [PubMed] [Google Scholar]
- Osler T, Baker SP, long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43:922–926. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
- Sacco WJ, MacKenzie EJ, Champion HR, et al. Comparison of alternative methods for assessing injury severity based on anatomic descriptors. J Trauma. 1999;47(3):441–446. doi: 10.1097/00005373-199909000-00001. [DOI] [PubMed] [Google Scholar]