Abstract
Studies highlight a higher involvement of drivers with diabetes in motor vehicle accidents. Extensive debate, though, exists over the most appropriate approach to license these drivers. Risk factors for crashes in persons with diabetes are not well defined. In this report, motor vehicle crash involvement was identified in two cohorts of persons with type 1 diabetes to identify if crash patterns and characteristics differ by age. Overall, reported crashes decline with age in persons with and without diabetes, but the crash risk remained higher for persons with diabetes throughout the age span. No relationship was observed between diabetes complications, blood glucose control, and diabetes treatment patterns and motor vehicle crashes. Severe hypoglycemia, though, was consistently and strongly related to crashes at all ages. The findings suggest that the crash risk related to hypoglycemia does not diminish markedly in persons with Type 1 diabetes, despite changes in health and age.
Several reports highlight the involvement of drivers with diabetes in motor vehicle crashes [Charlton, 2004]. Extensive debate exists, though, over the role of diabetes in these crashes and licensing policy differs, worldwide, for these drivers. The natural history of type 1 diabetes (worsening health outcomes over time) indicates that factors influencing crashes in persons with diabetes may change over time. Few reports, though, have examined the factors related to crashes in persons with diabetes by age.
BACKGROUND
Diabetes mellitus is a health condition that is comprised of a heterogeneous group of disorders which all result in persistently high blood glucose levels [Harris, 1995]. The most common forms of diabetes include type 1 and type 2 diabetes. Type 1 diabetes mellitus is generally characterized by abrupt onset during childhood or young adulthood. Individuals with type 1 diabetes are dependent upon injected insulin to sustain life [Harris, 1997]. The onset of type 2 diabetes typically occurs later in adulthood, although recently, increased prevalence of this form of diabetes in children and adolescents has been observed. Type 2 diabetes mellitus is often related to obesity, with its associated insulin resistance, and a progressive beta cell defect in the pancreas, such that the body cannot properly utilize available insulin and cannot produce sufficient insulin to maintain proper blood glucose levels. Most persons with diabetes (90–95%) have type 2 diabetes [Harris, 1995]. Most individuals with type 2 diabetes are not treated with insulin, but may require insulin in the later stages of the disease to maintain blood glucose control.
Several factors may influence the risk for crash among persons with diabetes. Most of the focus in the literature has been on persons with insulin-treated diabetes. The primary concern among these individuals is their capacity to develop sudden impairment in judgment or consciousness while driving. This arises primarily from hypoglycemia, or extremely low levels of blood glucose, which occurs more commonly among persons using insulin to treat their diabetes. Mild forms of hypoglycemia can result in altered judgment. Some individuals have described this alteration as being similar to that observed among fatigued drivers. Severe hypoglycemia, if not detected, can result in sudden impairment, and in some situations, a loss of consciousness.
Table 1 outlines our current understanding of how the frequency of crash compares between persons with and without diabetes. These listed studies and others in the literature [Cox, 2003; Koepsell, 1994] indicate that the risk for crash is probably higher for a person with diabetes compared to someone without diabetes. While the studies listed in Table 1 are not directly comparable, the rate ratio information is remarkably consistent. Further, it indicates that the risk related to diabetes is not extraordinarily high, approximately on the order of 30% higher than the non-diabetic population.
Table 1.
Crash Risks Among Persons with Insulin-Treated Diabetes
| Study | Rate Ratio |
|---|---|
| Waller, 1965 | 1.8 |
| Songer, 1988 | 2.0 unadjusted |
| 0.99 adjusted | |
| Eadington, 1989 | 0.54 |
| Stevens, 1989 | 1.0 |
| Hansotia, 1991 | 1.32 |
| McGwin, 1999 | 1.3 |
| Laberge-Nadeau, 2000 | 1.07 |
| Vernon, 2001 | 1.30 |
| Kennedy, 2002 | 1.29 |
There remain many debates, though, around the licensing of persons with insulin-treated diabetes, particularly with regard to occupational licenses. The debate centers on the issue of whether the increased risk is acceptable. Some argue that this level of risk is already accepted with regards to the licensing of other drivers. Others argue that safety is compromised due to the heightened risk.
An emerging component to the debate regarding licensing is the heterogeneity found between individuals in their risk for crash. In other words, not all individuals carry the same risk despite having a disease or other health condition. Some persons will have more crashes, and others very few. Identifying the risk factors related to motor vehicle crashes among persons with diabetes is an important endeavor. Surprisingly, few reports have examined the risk factors for crashes among persons with diabetes in much detail.
One area that has received attention is the relationship between hypoglycemia and crashes [Frier, 2000]. Several case reports note hypoglycemia involvement in motor vehicle crashes. Evidence from controlled experiments in a driving simulator also shows decrements in performance as a person becomes hypoglycemic [Cox, 2000]. Defining and attributing the risk for crash due to hypoglycemia, though, is a thorny issue. It is extremely difficult, for example, to document blood glucose levels at the time of a crash. These values can change quickly (depending upon the person’s and the body’s response to a hypoglycemic event), and individuals may have differing thresholds triggering hypoglycemia. Thus, most large-scale studies do not directly examine the role of hypoglycemia in crashes. However, indirect evidence does exist showing a relationship between a history of hypoglycemic events while driving and reported crashes [Cox, 2003] and a relationship between past severe hypoglycemia events and reported crashes [Songer, 2002].
Another issue receiving recent attention is the role of diabetes treatment in motor vehicle crash occurrence. The aggressive treatment of diabetes, with frequent insulin administration and regular blood glucose monitoring, is now standard practice and an important component to improve the long-term health of a person with diabetes and prevent future health problems. Many individuals believe that an intensified treatment regimen may lead to more accidents because of a greater potential for hypoglycemia. Available evidence, however, has not yet documented that intensified treatment regimens are a risk factor for crashes. One study [Harsch, 2002] found no relationship between hypoglycemia-related accidents and intensive treatment. Another study [Cox, 2003] found the opposite effect, where persons using an insulin pump (one form of intensified management) had fewer crashes.
Yet another issue that draws attention is the potential role of diabetes complications in motor vehicle crashes. The natural history of diabetes is well established and indicates a pattern of worsening health over time. Common chronic health conditions related to diabetes include eye, kidney, and heart problems. Past research demonstrates a strong link between poor vision and motor vehicle crashes, as well as heart disease and crashes [Charlton, 2004]. Thus, there is the potential that the factors related to crashes in persons with diabetes may change over time.
OBJECTIVE
The role of age in motor vehicle crashes in persons with insulin-treated diabetes has not received much prior study. As treatment patterns have changed over time, and longer disease duration is typically linked with worsening health in persons with diabetes, one could hypothesize that the crash frequency and characteristics related to crashes in drivers with diabetes may change with age. In this light, the following report examines two issues; (a) if crash risks differ by age in persons with type 1 diabetes compared to persons without diabetes, and (b) if the risk factors related to crashes among persons with diabetes differ by age.
METHODS
This report is based upon information gathered from two studies; (1) a case-control study of the self-reported crash experience of individuals with type 1 diabetes and siblings without diabetes, and (2) a longitudinal study of the reported crash and health experience identified from a large cohort of persons with type 1 diabetes. The case-control study will be used to identify how crash risks, overall, differ by age. The longitudinal study provides more depth to assess if and how risk factors related to crashes change with advancing age.
Case-Control Study
In the case-control study, reported crash frequency was compared between persons with type 1 diabetes and non-diabetic sibling controls. Person with diabetes were recruited from two cohorts which differed primarily by age. The first cohort included older subjects with type 1 diabetes (age range: 45–64 years) who were identified from 169 eligible individuals who were listed in the Children’s Hospital of Pittsburgh type 1 diabetes registry and participated in a prior study in 1985. Individuals listed in the registry were less than 17 years of age at the diagnosis of diabetes, were diagnosed between 1950–65, were discharged from the hospital at diagnosis on insulin therapy, and received medical care at Children’s Hospital at diagnosis or within 1 year of diagnosis.
The second cohort included younger subjects with type 1 diabetes (age range: 18–31 years) who were identified from 197 individuals who were listed in the Allegheny County type 1 diabetes registry between 1965–85 and whose parents participated in a prior study in 1989. These individuals were <17 years of age at diagnosis and were residents of Allegheny County, PA at diagnosis. Family members of the individuals with diabetes in both cohorts were identified as a comparison group in the analysis. Selected brothers, sisters, and first cousins who did not have diabetes were eligible. These subjects were known from their participation in prior studies.
Both diabetes case and sibling control subjects interested in the study were sent a questionnaire by mail. Survey responses were collected from the participants from November 2002 to June 2005. Survey questions examined if the research subjects drove, their annual mileage driven, current health, and their involvement in motor vehicle crashes in the past three years. In addition, persons with diabetes were asked about the frequency in which they developed hypoglycemia. Self-reported hypoglycemia was classified as mild hypoglycemia in the last year (noted by the symptoms of sweating, shaking, or trembling), hypoglycemia without recognition of symptoms in the last year, or severe hypoglycemia in the last two years (noted by an episode where the person lost consciousness).
Longitudinal Study
Persons enrolled in the Pittsburgh Epidemiology of Diabetes Complications (EDC) study were also examined to identify patterns in crashes by age among persons with diabetes, and to identify the factors related to these crashes. The EDC study is an ongoing prospective study of the factors related to the development of the long-term complications of type 1 diabetes. The study is compromised of adults with type 1 diabetes who were diagnosed or seen within one year of diagnosis at the Children’s Hospital of Pittsburgh between 1950–1980.
Clinical exams were given in the EDC study biannually from 1986–98 to document health and complication status. Motor vehicle crash frequency and related factors have been examined as one part of the EDC study since 1990. Thus, information from four clinical exams was available for analysis. Data on crashes, hypoglycemia, and driving patterns were queried from participants by self-report questionnaires during the clinical exam schedules. In 2000–01, subjects were sent an additional survey (similar to those completed in earlier years) by mail, but these individuals did not receive a clinical exam. In all surveys, motor vehicle crashes and driving characteristics were identified over the prior one year period.
The frequency of hypoglycemia was also captured in the surveys. Hypoglycemia events were again defined from three perspectives; the frequency of mild hypoglycemia in the last year, hypoglycemic reactions in the last year without recognition of the warning symptoms of hypoglycemia, and severe hypoglycemia within the last 2 years.
STATISTICAL ANALYSIS
The survey data in both the case-control and longitudinal studies were first examined to identify the demographic characteristics (age, gender, health conditions) of the respondents. Subsequent analyses were confined to subjects reporting possession of a driver’s license. Motor vehicle crash risks were examined using the Chi-square statistic, where crash involvement (yes/no) was assessed relative to the demographic, health, and hypoglycemia characteristics reported by the participants. Multivariate analysis was conducted to identify the independent contribution of diabetes to motor vehicle crashes in the case-control study, and the independent role of hypoglycemia and other factors in the crash risk of diabetes drivers in the longitudinal study.
RESULTS
PARTICIPATION
Overall, surveys were received from 67 persons with type 1 diabetes and 136 siblings without diabetes in the case-control study. Data was available from all individuals participating in the clinical exam and survey structure of the EDC study. The number of participants at each clinical exam in the longitudinal study varied slightly over time; 397 persons at the first data collection point in 1990–92, 404 persons at the second data point in 1992–94, 352 persons examined in 1994–96, and 395 persons from the 1996–98 exam. Fewer subjects (n=293) participated in the survey conducted in 2000–01.
Table 2 outlines the demographic characteristics of the respondents in both studies. In the case-control study, case subjects did not differ from controls by gender, mileage driven, or marital status, but were slightly older (43.8 yrs. vs. 38.5 yrs, p=0.01). Also, more case subjects were older than age 45 years (54.0% vs. 40.6%, p<0.05) when compared to control subjects. Slightly fewer cases (88.9% vs. 96.5%) reported driving in the last year compared to controls.
Table 2.
Demographic and Driving Characteristics of the Study Participants
| Case-Control Study | Longitudinal Study of Drivers with Diabetes | ||||||
|---|---|---|---|---|---|---|---|
| Cases (n=67) | Controls (n=136) | Exam A (1990–92) (n=397) | Exam B (1992–94) (n=404) | Exam C (1994–96) (n=352) | Exam D (1996–98) (n=395) | Survey E (2000–01) (n=293) | |
| Gender | |||||||
| Males | 51.6% | 44.0% | 51.1% | 49.3% | 50.3% | 49.4% | 43.7% |
| Females | 48.4% | 56.0% | 48.9% | 50.7% | 49.7% | 50.6% | 56.3% |
| Mean Age (yrs ± SD) | 43.8 ± (13.1) | 38.5 ± (14.3)* | 32.0 ± (7.3) | 34.0 ± (7.7) | 35.8 ± (7.6) | 37.5 ± (7.8) | 39.7 ± (8.3) |
| Age Category | |||||||
| <25 years | 3.2% | 22.3%* | 14.8% | 12.4% | 7.7% | 5.1% | 1.7% |
| 25–34 years | 38.1% | 28.5% | 47.6% | 43.8% | 41.8% | 35.4% | 25.3% |
| 35–44 years | 4.8% | 10.0% | 32.5% | 34.2% | 38.1% | 40.8% | 45.9% |
| 45–54 years | 25.4% | 23.8% | 5.0% | 9.7% | 12.5% | 18.2% | 24.3% |
| 55–64 years | 28.6% | 15.4% | - | - | - | 0.5% | 2.7% |
| Health Conditions | |||||||
| Retinopathy | 50.0% | - | 40.6% | 45.5% | 50.2% | 53.5% | - |
| Heart Disease | - | - | 11.3% | 14.9% | 18.8% | 21.0% | - |
| Mean Miles Driven (per year) | 10, 532 mi | 14,456 mi | 11,107 mi | 11,106 mi | 11,011 mi | 11,985 mi | 11,311 mi |
p<0.05
In the longitudinal study, the mean age of the participants increased over time by design, from 32.0 years at the time of the first data collection point (1990–92) to 39.7 years in 2000–01. The participants were evenly split by gender over the time of the study, and reported mileage driven (per year) and the percentage that drove were also similar over time. Clinical exam data was available to document the health conditions of the participants. The presence of diabetes complications increased over time, reflecting the natural history identified for type 1 diabetes. Retinopathy (eye disease) was very common in this study cohort. The prevalence of coronary heart disease increased from 11.3% to 21.0% from 1990–98. Other conditions were also frequent. At the time of the 1992–94 clinical exam, 27.3% of the individuals had nephropathy (kidney disease) and 17.2% had neuropathy (nerve disease). The mean HbA1c level in this group (an indicator of glucose control) was 9.05.
CRASH RISKS AND AGE
The first objective of this report was to identify if crash risks differ by age in persons with type 1 diabetes compared to persons without diabetes. In the case-control study, the reported crash frequency of persons with diabetes was significantly higher than that reported by the sibling controls. Overall, persons with diabetes reported more crash involvement in the previous 3 years compared to controls (27.4% vs. 13.4%, p=0.02). The characteristics of the reported crashes among the diabetic subjects were as follows; 58% involved two vehicles, 47% were reported to the police, 37% involved an injury, and in 37%, the vehicle was towed from the scene. Reported crashes among the control subjects were as follows; 75% involved two vehicles, 62% were police reported, 25% involved an injury, and in 25%, a vehicle was towed from the scene.
The reported crash experience did not differ among males with and without diabetes (cases: 25.8% vs. controls: 15.3%), but approached significance in females (cases: 26.7% vs. controls: 12.0%, p=0.06). Marital status was also related to crash risk where case subjects who were not married had a markedly higher reported crash frequency than unmarried sibling controls (36.4% vs. 15.5%, p=0.045). No difference was observed among married cases and controls. In diabetic subjects, the frequency of hypoglycemia was not associated with the reported crashes. However, among those who reported a crash, having a history of hypoglycemia without warning symptoms in the past year was significantly related to involvement in a single vehicle crash (78% of persons with hypoglycemia unawareness reported a single vehicle crash vs. 0% of those without hypoglycemia unawareness, p=0.002).
In multivariate analysis, diabetes status and age were the strongest factors independently related to reported crashes. Persons with diabetes were 2.67 more likely to report a crash compared to their sibling controls (p=0.019) after adjusting for the contributions of gender, age, mileage driven, and marital status to this experience.
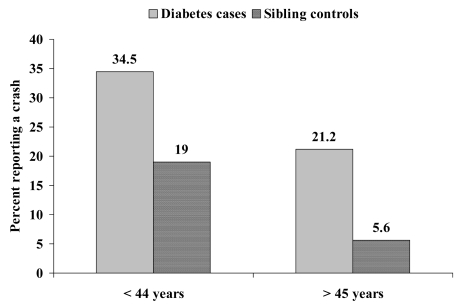
Age was also an independent factor explaining crashes in the case-control study. Reported crashes declined with age in both cases and controls. However, crash risks remained higher for persons with diabetes when stratified by age group, particularly so for persons over age 45 years (Figure 1)(age 17–44:34.5% vs. 19.0%, p=0.08; aged 45–66 years: 21.2% vs. 5.6%, p=0.03).
Figure 1.
Reported Crash Involvement by Diabetes Status and Age
DO RISK FACTORS DIFFER BY AGE
Given that higher risks for crashes have been observed for both young and older individuals with diabetes, the second research question sought to identify if the factors contributing to motor vehicle crashes differ by age in persons with diabetes.
The frequency of involvement in a crash reported by persons with diabetes in the longitudinal study was fairly consistent over time, ranging from 11.7% to 15.3% in the five survey points. However, when considering driving exposure, the reported mean crash rates (number of crashes per million miles driven) were much more variable (1990–92 exam: 48.3 crashes per million miles driven, 1992–94 exam: 133.0, 1994–96 exam: 16.9, 1996–98 exam, 63.6 crashes per million miles driven).
The characteristics of the reported crashes were next examined at each time point in the longitudinal study. Significant influences for crashes at each time point included age and hypoglycemia (both severe hypoglycemia and hypoglycemia without recognition of symptoms). Table 3 displays the accident data of the EDC study group over time by age category. When stratified by age group, there was a trend towards fewer reported crashes among those in older ages (particular for those over age 45 years).
Table 3.
Percent Reporting Involvement in a Motor Vehicle Crash in the Last Year by Age Group and Survey Period
| Exam A | Exam B | Exam C | Exam D | Survey E | |
|---|---|---|---|---|---|
| < 21 years | 11.1% | 33.3% | 14.3% | 33.3% | - |
| 21–24 years | 17.1% | 14.3% | 15.0% | 18.8% | 0.0 |
| 25–34 years | 15.9% | 18.1% | 10.2% | 15.1% | 20.3% |
| 35–44 years | 10.1% | 13.8% | 15.7% | 10.6% | 10.6% |
| 45–54 years | 5.0% | 2.6% | 6.8% | 5.6% | 8.6% |
| 55–64 years | - | - | - | 0.0 | 12.5 |
Hypoglycemia was consistently and strongly related to the reported crashes over each survey point. This pattern was not evident for mild hypoglycemia, but was marked for both hypoglycemia without warning (no recognition of the symptoms of hypoglycemia) and severe hypoglycemia (Table 4). This relationship appeared to be more pronounced for severe hypoglycemia, where the reported frequency of crash was 1.5–2.0 times higher in persons with a history of severe hypoglycemia in the last two years (compared to those with no history of severe episodes).
Table 4.
Percent Reporting Involvement in a Motor Vehicle Crash in the Last Year, Overall, and by Reported Type of Hypoglycemia
| Exam A | Exam B | Exam C | Exam D | Survey E | |
|---|---|---|---|---|---|
| Overall | 13.4% | 15.3% | 12.2% | 11.7% | 12.8% |
| Mild hypoglycemia | 14.1% | 15.2% | 12.7% | 12.4% | 13.0% |
| Hypoglycemia without recognition | - | 18.1% | 17.0%* | 17.7%* | 12.6% |
| Severe hypoglycemia | 22.7%** | 20.5% | 14.7% | 22.1%** | 16.2% |
p<0.05
p<0.01
There also were several consistent non-relationships observed over time between motor vehicle crash involvement and demographic, treatment, and health factors in persons with diabetes. No relationship was observed between gender and crashes over time, although males reported involvement in more crashes than females. Many individuals have hypothesized in the past that the presence of diabetes complications may increase crash risk. However, in this analysis, retinopathy, coronary heart disease, and symptomatic autonomic neuropathy were not associated with crash frequency. Blood glucose control and the use of an insulin pump are two factors that define the level of treatment for a person with type 1 diabetes. Both were not related to the reported crash experience of this group over time. As an example, at the 1996–98 exam, no difference in mean HbA1c levels was noted by crash status (crash: 8.75 ± 1.5, no crash: 9.05 ± 1.6).
Multivariate analysis was conducted to examine the influence of these potential risk factors over time (or advancing age). Overall, age was related to reported crashes (declining crashes with advancing age), but severe hypoglycemia remained the strongest variable related to crashes independent of age (Table 5). The odds of being involved in a crash were 2–4 times higher for someone reporting severe hypoglycemia than for someone with no severe events. Diabetes complications (retinopathy and coronary heart disease) were not related to crashes.
Table 5.
Multivariate Models of Factors Related to Motor Vehicle Crashes in Drivers with Type 1 Diabetes over Ten Years (data shown as odds ratios)
| Factor | Exam A | Exam B | Exam C | Exam D | Survey E |
|---|---|---|---|---|---|
| Gender (female:male) | 0.99 | 0.96 | 1.98 | 0.70 | |
| Age (per year) | 0.97 | 0.96 | 0.99 | 0.95 | 0.95 |
| Severe hypoglycemia (yes:no) | 2.78** | 1.96* | 1.23 | 4.20** | 2.0 |
| Annual mileage driven (per mile) | 1.01* | 1.01 | 1.01 | 1.01** | 1.01* |
| Retinopathy (yes:no) | 1.36 | 0.99 | 0.99 | 1.33 | - |
| Coronary Artery Disease (yes:no) | 0.95 | 1.39 | 1.90 | 0.64 | - |
p<0.05
p<0.01
DISCUSSION
Debate has existed for several years over the proper licensing policy for persons with insulin-treated diabetes. Many jurisdictions place restrictions on occupational licenses for persons with diabetes, because of the perception that the crash risk is higher for drivers requiring insulin. Current events have led to a re-examination of the licensing policy debate. These include the rising prevalence of diabetes, advances in diabetes treatment agents and technologies that improve health, changes in diabetes treatment patterns where more persons with type 2 diabetes are now treated with insulin, and an overall shortage of occupational drivers.
This report examined the motor vehicle crash experiences of persons with Type 1 diabetes mellitus over large age range. Several observations were noted in the study. First, the results suggest that motor vehicle crash frequency decline with age in persons with diabetes as it does in the general population. However, the crash risk level remains elevated for persons with type 1 diabetes compared to persons without diabetes at all age categories up to age 65 years. Second, while diabetes complications increase in prevalence with advancing age for a person with diabetes, the primary factor related to motor vehicle crashes is hypoglycemia, particularly severe hypoglycemia. Third, elements of diabetes treatment and blood glucose control were not major determinants of crash risk among these study participants.
This study expands upon the scientific understanding of how diabetes influences motor vehicle crash risk. It is one of the first reports to examine crash patterns and risk factors at differing ages among persons with diabetes. The findings suggest that crashes related to hypoglycemia are not just a phenomenon of the young, but are also quite frequent among older persons with Type 1 diabetes; many of whom also have existing co-morbid health conditions.
The study population in this report was drawn from two large and representative registries of persons with type 1 diabetes. The study subjects have also been active participants in prior research on diabetes epidemiology issues. Both of these issues pose strengths to the current study in terms of the population sample and participation rates. The structure of the registries and the timing of our prior research, though, also posed limitations in the study. Foremost, it was not possible to examine persons over age 65 in the study. Crash frequency and patterns may differ in these individuals. Prior reports in the literature are conflicting; with reports indicating a higher crash risk in older diabetes drivers, and other reported indicating no difference. These reports, though, were based largely on persons with type 2 diabetes.
Prior research participation also adversely affected the expected participation for the case-control study in this report. All subjects in the older cohort and the parents of individuals in the younger cohort had participated in prior research from 1985–89. Given the long time lag between studies, it was not possible to locate 35% of the original participants. An additional 16% of the original group had died. Among subjects that were located, the participation rate of case subjects in the case-control study was low; 37% of those subjects who were alive. Many individuals declined (29%) or refused (27%) to participate in the case-control study because of participation in prior research studies and because of the changing research environment. In particular, several parents of the younger cohort subjects declined to grant permission to contact the diabetes case. The low participation rate in the case-control study may introduce a bias that affects the results, particularly if the crash experience of those participating differs from those not participating.
The low sample size available in the case-control study may also account for some of the findings that approached, but did not reach statistical significance. On the other hand, the ability to tap into an existing longitudinal study to examine the risk factors for crashes was a noted strength of the report. Participation rates in the EDC study have been very good. In addition, clinical measures of complications allowed for the assessment of the role of chronic disease in crashes.
The crash experience identified in this study was based upon the self-report of the participants. While this is not the gold standard for identifying crashes, it represents a reasonable approximation for event frequency and captures events of differing severity. In this report, for example, there was evidence that nearly half of the reported crashes were reported to the police and one-third involved an injury. The limitation of identifying crashes by self-report, though, is that respondents may not accurately recall the number of crashes or injuries incurred. They may also withhold information if they believe that it would adversely affect their licensing status.
A key finding of this report was the link between hypoglycemia and motor vehicle crashes. There also was preliminary evidence to suggest an association between hypoglycemia without warning symptoms and involvement in a single vehicle crash. These links found between reported hypoglycemia history and reported crashes, though, are indirect in nature. It was not possible, in this report, to determine the extent to which hypoglycemia actually contributed to the reported crashes, only the association of prior hypoglycemia and crashes. Further, the number of single vehicle crashes among persons with diabetes identified in this report was low, and further study is necessary to establish the relationship between hypoglycemia and the severity of crashes.
This report supplements existing research in the field by examining how crash frequency and patterns differ by age. This information may aid future decisions regarding licensing policy, particularly decisions regarding the risk associated with licensing drivers requiring insulin. In addition, the results may lay the foundation for efforts to develop of screening tools or strategies to reduce the risks faced by drivers with insulin-treated diabetes.
ACKNOWLEDGEMENT
This work was supported by a grant award from the National Institutes of Health (RO1-DK58353). We would like to thank Kathy Fadgen and Jamie Knotts for their excellent support on data collection and data entry on the project.
REFERENCES
- Charlton J, Koppel S, O’Hare M, et al. Influence of chronic illness on crash involvement of motor vehicle drivers. Monash University Accident Research Center Report No. 213; Melbourne, Australia, Monash University. April 2004.pp. 146–179. [Google Scholar]
- Cox DJ, Gonder-Frederick L, Kovatchev BP, et al. Progressive hypoglycemia’s impact on driving simulation performance: occurrence, awareness, and correction. Diabetes Care. 2000;23:163–170. doi: 10.2337/diacare.23.2.163. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Penberthy JK, Zrebiec J, et al. Diabetes and driving mishaps. Diabetes Care. 2003;26(8):2329–2334. doi: 10.2337/diacare.26.8.2329. [DOI] [PubMed] [Google Scholar]
- Eadington DW, Frier BM. Type 1 diabetes and driving experience: an eight year cohort study. Diabetic Medicine. 1989;6:137–141. doi: 10.1111/j.1464-5491.1989.tb02101.x. [DOI] [PubMed] [Google Scholar]
- Frier BM. Hypoglycemia and driving performance. Diabetes Care. 2000;23(2):148–150. doi: 10.2337/diacare.23.2.148. [DOI] [PubMed] [Google Scholar]
- Hansotia P, Broste SK. The effect of epilepsy or diabetes mellitus on the risk of automobile accidents. NEJM. 1991;324:22–26. doi: 10.1056/NEJM199101033240105. [DOI] [PubMed] [Google Scholar]
- Harris MI. Diabetes in America, National Institutes of Health Pub. No. 95-1468. 2. Bethesda, MD: National Institutes of Health, National Diabetes Data Group; 1995. Chapter 1 Summary; pp. 1–13. [Google Scholar]
- Harris MI, Zimmet P. International Textbook of Diabetes Mellitus. 2. New York, NY: John Wiley & Sons; 1997. Classification of Diabetes Mellitus and Other Categories of Glucose Intolerance; pp. 13–16. [Google Scholar]
- Harsch IA, Stocker S, Radespiel-Troger M, et al. Traffic hypoglycemias and accidents in patients with diabetes mellitus treated with different antidiabetic regimens. J Internal Med. 2002;252:352–360. doi: 10.1046/j.1365-2796.2002.01048.x. [DOI] [PubMed] [Google Scholar]
- Kennedy RL, Henry J, Chapman AJ, et al. Accidents in patients with insulin-treated diabetes: increased risk of low-impact falls but not motor vehicle crashes. J Trauma. 2002;52:660–666. doi: 10.1097/00005373-200204000-00008. [DOI] [PubMed] [Google Scholar]
- Koepsell TD, Wolf ME, McCloskey L, et al. Medical conditions and motor vehicle collision injuries in older adults. J Amer Geriatrics Soc. 1994;42:695–700. doi: 10.1111/j.1532-5415.1994.tb06526.x. [DOI] [PubMed] [Google Scholar]
- Laberge-Nadeau C, Dionne G, Ekoe JM, et al. Impact of diabetes on crash risks of truck-permit holders and commercial drivers. Diabetes Care. 2000;23(5):612–7. doi: 10.2337/diacare.23.5.612. [DOI] [PubMed] [Google Scholar]
- McGwin G, Sims RV, Pulley L, Roseman JM. Diabetes and automobile crashes in the elderly. Diabetes Care. 1999;22:220–227. doi: 10.2337/diacare.22.2.220. [DOI] [PubMed] [Google Scholar]
- Songer TJ, LaPorte RE, Dorman JS, et al. Motor vehicle accidents and IDDM. Diabetes Care. 1988;11:701–707. doi: 10.2337/diacare.11.9.701. [DOI] [PubMed] [Google Scholar]
- Songer TJ. Low blood sugar and motor vehicle crashes in persons with type 1 diabetes. Annu Proc Assoc Adv Automotive Med. 2002;46:424–427. [PubMed] [Google Scholar]
- Stevens AB, Roberts M, McKane R, et al. Motor vehicle driving among diabetics taking insulin and non-diabetics. Brit Med J. 1989;299:591–595. doi: 10.1136/bmj.299.6699.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon DD, Diller EM, Cook LJ, Reading JC, Deane JM. NHTSA Technical Report No. DOT-HS-809211. Washington, DC: US Dept. of Transportation, National Highway Traffic Safety Administration; Mar, 2001. Further analysis of drivers licensed with medical conditions in Utah. [Google Scholar]
- Waller JA. Chronic medical conditions and traffic safety: review of the California experience. NEJM. 1965;273:1413–1420. doi: 10.1056/NEJM196512232732605. [DOI] [PubMed] [Google Scholar]