Abstract
The difference between the ISS and NISS scores was determined for 1,533 inpatients consecutively admitted in 1998 in the Emergency Department of a University Hospital in São Paulo, Brazil. The average ISS was 12.49 ± 12.72, and the average NISS was 16.99 ± 17.60. The two predictive scores were identical in 47.75% of the patients and discrepant in 52.25%. In all cases of discrepant scores, the NISS was greater than ISS. NISS identified significantly more (42.47%) major trauma patients (score ≥ 16) than ISS (34.18%) (p<0.001). For nonsurvivors the percentage of discrepant score was higher (75.68%) than for the survivors group (48.28%).
In the last four decades, methods named systems, indices or scales, based upon the nature of the injury, were developed and improved to rate the degree of injury damage. However, the complex and multiple variables of trauma, which influence the outcomes of trauma care, make the creation of an ideal model for graduating injury severity difficult.
The Abbreviated Injury Scale (AIS) is still widely used to rate the severity of each injury in the body. The AIS code for each injury ranges from 1 (minor injuries) to 6 (maximum injuries, almost always fatal). Therefore, the evaluation of cumulative effect of multiple injuries in many body regions, characteristically found in trauma patients, is not simply obtained by using AIS.
By recognizing AIS’s fragility as a prognostic measure for patients with multiple injuries, and the needs of a method to summarize the severity, Baker, O’Neill, Haddon et al. (1974) introduced the Injury Severity Score (ISS) based on AIS and this index has become the most widely applied score for evaluating trauma.
The ISS consists of the result of the sum of the squares of the highest AIS scores for the three most severely different injured body regions. The six defined body regions for ISS are: head and neck, face, chest, abdominal and external. The ISS scores range from 1 to 75, being one the least severe and 75 the most severe trauma injury. Any injury coded AIS 6 implies an ISS of 75.
In spite of its widespread application, ISS is associated with a series of limitations pointed out throughout time by several researchers [Cayten, Stahl, Murphy et al, 1991;Osler, Baker, Long, 1997; Sacco, Mackenzie, Champion et al., 1999]. Aiming at overcoming some ISS limitations, Osler et al. (1997) proposed a modification to the original ISS with the objective of increasing its predictive power and simplifying its calculation. They named this innovative method New Injury Severity Score (NISS), whose score results from the sum of the squares of the three highest AIS scores regardless of the body region affected.
The NISS proposition was based, by its creators, on two aspects [Osler et al.1997]. First, the ISS usually excludes some injuries from measurement process, because it takes into account only a single injury per body region. Therefore, when patients have multiple injuries in the same body region, ISS considers only the most severe injury in this region. Second, for the patients who have many injuries in many body regions, ISS needs an injury from a second region to be considered for its calculation. This way, sometimes, an injury less severe than the second one from the first body region will contribute to ISS score. For this reason, it often fails by considering less severe injuries, instead of other more severe injuries affecting other body regions.
Scoring systems also have been used in Brazil to quantify injury severity. The limitations of AIS/ISS systems, observed in studies conducted in our setting and the necessity to know the NISS performance in Brazilian trauma patients, contributed to the decision to develop this study. Then, the purpose was to determine the differences between the ISS and NISS scores among trauma inpatients in a university hospital in Brazil.
METHODS
Data related to trauma patients, consecutively admitted in the Emergency Department of the “Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HCFMUSP)” Brazil, from January to December 1998, were gathered retrospectively.
The HCFMUSP data set consisted of 1,533 trauma inpatients. It mainly included young male-sex patients (80.24%), in average aged 30 years (sd 16.27). The external-cause types were classified as blunt trauma (67.06%), followed by penetrating trauma (26.81%), burn (4.04%) and other (2.09%). Hospital mortality reached 14.48 %.
For each patient the ISS (sum of the squares of the highest AIS score in each of the three most severely injured body regions) and the NISS (the sum of the squares of the highest AIS score regardless of the body region in which they occur) were calculated.
Data sources applied to the ISS and NISS calculations included the patients’ charts and the autopsy findings. The injury severity measurement was made by using Abbreviated Injury Scale 1990 revision - update 98.
The difference and agreement between ISS and NISS scores were verified by applying intraclass correlation coefficient, MacNemar’s test and Kappa’s coefficient [Agresti, 1990]. The comparison was made for the data set as a whole as well as for the mechanism of trauma and between survivors and nonsurvivors.
RESULTS
Among the 1,533 patients studied, ISS and NISS scores were identical for 47.75% and significantly discrepant for 52.25% (p=0.0002). In all cases of discrepant scores, NISS was greater than ISS. The NISS average was higher than ISS average, respectively, 16.99 (sd 17.60) and 12.49 (sd 12.79).
By comparing the percentage of blunt trauma patients in each bracket of ISS and NISS scores (Tables 1 and 2), a lower percentage of patients in NISS scores ranging from 1 to 24 and a higher percentage of patients in NISS scores ranging from 25 to 75 were observed. The frequency of patients in the NISS scores up to 41 was 2.83 times higher than the one observed in the ISS brackets. For blunt trauma patients, the ISS average was 13.08 and NISS was 17.66.
Table 1.
ISS scores according to trauma mechanisms
| Blunt | Penetrating | Burn | Others | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ISS | n | % | n | % | n | % | n | % | n | % |
| 1 – 8 | 425 | 41.4 | 183 | 44.5 | 33 | 53.2 | 23 | 71.9 | 664 | 43.4 |
| 9 – 15 | 216 | 21.0 | 110 | 26.8 | 15 | 24.2 | 4 | 12.5 | 345 | 22.5 |
| 16 – 24 | 199 | 19.4 | 41 | 10.0 | 7 | 11.3 | - | - | 247 | 16.1 |
| 25 – 40 | 135 | 13.1 | 59 | 14.4 | 6 | 9.7 | 3 | 9.4 | 203 | 13.2 |
| 41 – 49 | 30 | 2.9 | 7 | 1.7 | - | - | 2 | 6.2 | 39 | 2.5 |
| 50 – 74 | 21 | 2.0 | 7 | 1.7 | 1 | 1.6 | - | - | 29 | 1.9 |
| 75 | 2 | 0.2 | 4 | 0.9 | - | - | - | - | 6 | 0.4 |
| Total | 1028 | 100.00 | 411 | 100.00 | 62 | 100.00 | 32 | 100.00 | 1533 | 100.00 |
Table 2.
NISS scores according to trauma mechanisms
| Blunt | Penetrating | Burn | Others | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NISS | n | % | n | % | n | % | n | % | n | % |
| 1 – 8 | 400 | 38.9 | 172 | 41.8 | 33 | 53.2 | 22 | 68.8 | 627 | 40.9 |
| 9 – 15 | 163 | 15.9 | 74 | 18.0 | 15 | 24.2 | 3 | 9.4 | 255 | 16.6 |
| 16 – 24 | 175 | 17.0 | 55 | 13.4 | 7 | 11.3 | 2 | 6.2 | 239 | 15.6 |
| 25 – 40 | 140 | 13.6 | 49 | 11.9 | 6 | 9.7 | 3 | 9.4 | 198 | 12.9 |
| 41 – 49 | 66 | 6.4 | 16 | 3.9 | - | - | 2 | 6.2 | 84 | 5.5 |
| 50 – 74 | 75 | 7.3 | 39 | 9.5 | 1 | 1.6 | - | - | 115 | 7.5 |
| 75 | 9 | 0.9 | 6 | 1.5 | - | - | - | - | 15 | 1.00 |
| Total | 1028 | 100.00 | 411 | 100.00 | 62 | 100.00 | 32 | 100.00 | 1533 | 100.00 |
In the ISS and NISS score brackets, related to penetrating trauma, the distribution of patients was different as well (Tables 1 and 2). The percentage of patients from NISS 1 to 15 and from 25 to 40 was lower than in ISS, but it was higher in the 16 to 24 and 41 to 75 brackets. The patients’ frequency was 3.39 times higher in the NISS brackets, from the 41 score on.
The ISS and NISS scores in the burn group were the same. For the group named others, the frequency of patients was lower in the brackets from 1 to 24 NISS scores. Two patients scored with ISS from 1 to 15 were included in NISS scores from 15 to 24.
According to Table 3, the agreement among ISS and NISS scores was high in all types of trauma studied. Blunt and penetrating trauma showed the same level of agreement.
Table 3.
NISS and ISS scores agreement coefficient by trauma mechanisms
| Trauma mechanisms | Coefficient | Confidence interval* |
|---|---|---|
| Blunt | 0.82 | 0.80–0.84 |
| Penetrating | 0.81 | 0.77–0.84 |
| Burn | 1 | |
| Others | 0.99 | 0.97–0.99 |
95% CI
In general, NISS identified significantly more (42.47%) major trauma patients (score ≥ 16) than ISS (34.18%) (p<0.001).
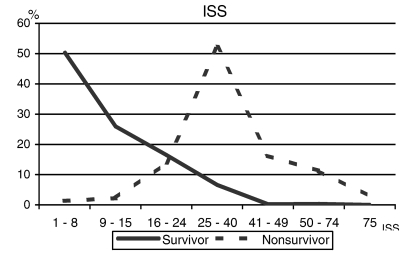
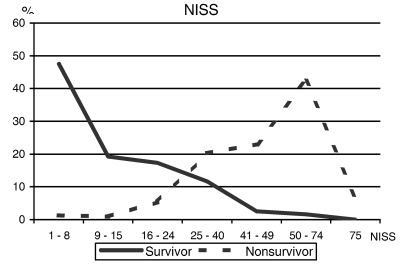
The ISS and NISS averages of survivors were 9.01 and 11.91, and for nonsurvivors were 33.06 and 47.02, respectively. According to Figure 1, the greatest death concentration (52.25%) occurred between 25 – 40 ISS scores. The distribution with NISS was different, presenting high nonsurvivor frequency in the high score brackets: from 25 until 74, the greatest concentration occurred between 50 – 74 (42.34%) (Figure 2).
Figure 1.
ISS scores according to discharge status.
Figure 2.
NISS scores according to discharge status.
For both blunt trauma as well as penetrating trauma a similar distribution pattern between survivors and nonsurvivors in the ISS and NISS brackets was observed.
For nonsurvivors the percentage of discrepant score was higher (75.68%) than for the survivors group (48.28%). Table 4 shows low agreement between ISS and NISS scores for nonsurvivors and high agreement for survivors.
Table 4.
NISS and ISS scores agreement coefficient by hospital discharge
| Hospital discharge | Coefficient | Confidence interval* |
|---|---|---|
| Nonsurvivor | 0.29 | 0.17–0.41 |
| Survivor | 0.84 | 0.82–0.85 |
95%CI
DISCUSSION
Professionals involved in trauma care have interest in measuring the effectiveness of patient management, mainly, the ability to maximize patient survival after serious injury
The difference between ISS and NISS in a series of trauma patients has not been established in Brazil to date.
The worldwide ISS utilization among several trauma populations during many years has made the observation of its performance and limitations possible.
The creation of NISS with the perspective of a better predictive capacity than the one applying ISS has led researchers to study its performance in different trauma populations [Brenneman, Boulanger, McLellan et al., 1998; Balogh, Offner, Moore et al., 2000; Husum, Strada, 2002; Stephenson, Langley, Civil, 2002; Meredith, Evans, Kilgo et al., 2002]. In the several studies as well as in this one, the frequency of discrepancy, a higher NISS value than an ISS one, varied from 52.25% to 82.5%.
In the Balogh et al. study (2000), the discrepancy between the ISS and NISS scores was higher among penetrating trauma patients, a fact not found in the present study and by Husum, Strada (2002).
The percentage of ISS and NISS scores discrepancy verified by Campos (2001) in Brazil among 63 outpatients who suffered blunt brain injury was high, 82.5%. Those victims presented mostly one or two body regions affected, several wounds in the head/neck regions and severe or critical wounds always found in this region. Therefore, the head wounds were crucial to the NISS calculation. In 74.6% of the victims only wound scores from this region were used to figure out this index.
NISS calculation methodology will enable a more adequate rating of the severity of a patient presenting multiple wounds and a high AIS score in the same body region, since it will add up points. This factor adds to the NISS performance in predicting mortality.
Sacco et al.’s study (1999) about comparison of alternative methods for assessing injury severity based on anatomic descriptors showed that NISS is better than ISS to predict hospital mortality.
The analysis of a blunt trauma patient group with discrepant ISS and NISS scores has revealed that the larger the score difference, the smaller the survival probability.
In Balogh’s study (2000), patients presenting discrepant NISS and ISS scores suffered higher mortality and related more often to a multiple organ failure.
The ISS limitation in quantifying trauma severity has important implications. When age and physiological variables are added to ISS, it composes the Trauma and Injury Severity Score (TRISS), a methodology for determining the probability of survival that has been used to evaluate trauma care. In fact, the analysis of unexpected deaths using TRISS, oftentimes reveals that in some cases the measurement of trauma anatomical severity remains underestimated due to the ISS calculation process [Osler, Rogers, Badger et al., 2002].
In this present study’s data set, initially Gennari (2000) studied the 222 nonsurvivors, out of whom 79, who had complete data to calculate TRISS, were analyzed. The study revealed 10 patients, out of 79, with unexpected deaths. When comparing the ISS and NISS scores for these 10 patients it was verified that in two cases scores were identical, 48 and 50. In the eight remaining cases, NISS values were much higher; in four cases the difference ranged from 3 to 8 points, in three from 16 to 25 and in one from 49 points. The distribution of specific injuries analysis in those 10 patients revealed multiple injuries in the head were responsible for more discrepants scores. (Whitaker, 2000)
In this study, the increase of NISS score, in case of multiple injuries, has enabled a better adjustment in trauma severity, which could be observed among nonsurvivors. In this group the degree of agreement between the scores was low (0.2930). The shift of nonsurvivors’ curve (Figure 2), because of the increase in NISS scores, better classified severe patients and more accurately distinguished between survivors and nonsurvivors. Even analyzing all patients, the proportion of major trauma (score ≥ 16) was statistically greater in the NISS group.
As expected, the agreement between ISS and NISS scores observed in the burn group was perfect (Table 3), since this type of trauma only affected the external body region.
In conclusion, NISS scores were different from ISS scores in 52.25% of the trauma inpatients studied and enabled the identification of a higher amount of major trauma.
The limitation of this study refers to the analysis conducted in only one hospital in Brazil. Further studies including more patients and hospitals should be conducted to verify the NISS effect in the evaluation of trauma care in our setting.
REFERENCES
- Agresti A. Categorical data analysis. New York: Wiley Interscience; 1990. [Google Scholar]
- Baker SP, O’Neill B, Haddon W, Jr, Long WB. The Injury Severity Score: a Method for Describing Patients with Multiple Injuries and Evaluating Emergency Care. J Trauma. 1974;14(3):187–96. [PubMed] [Google Scholar]
- Balogh Z, Offner PJ, Moore EE, Biffl WL. NISS Predicts Postinjury Multiple Organ Failure Better than the ISS. J Trauma. 2000;48(4):624–7. doi: 10.1097/00005373-200004000-00007. [DOI] [PubMed] [Google Scholar]
- Brenneman FD, Boulanger BR, McLellan BA, Redelmeier DA. Measuring Injury Severity: Time for a Change? J Trauma. 1998;44(4):580–2. doi: 10.1097/00005373-199804000-00003. [DOI] [PubMed] [Google Scholar]
- Campos MA. Master of Nursing Thesis, Universidade de São Paulo, Brazil. 2001. The Injury Severity Score and its New Propose in Traumatic Brain Injury Victms: Differences in Outcome and Predictive Value Effectiveness. [Google Scholar]
- Cayten CG, Stahk WM, Murphy JG, Agarwal N, Bryne DW. Limitations of the TRISS Method for interhospital compariosons: a Multihospital Study. J Trauma. 1991;31(4):471–82. doi: 10.1097/00005373-199104000-00005. [DOI] [PubMed] [Google Scholar]
- Gennari TD. Injury Severity Analyzed by Means of Clinical Diagnosis and Autopsy. Doctoral of Nursing Dissertation; Universidade de São Paulo, Brazil. 2000. [Google Scholar]
- Hussum H, Strada G. Injury Severity Score Versus New Injury Severity Score for Penetrating Injuries. Prehospital Disaster Med. 2002;17(1):27–32. doi: 10.1017/s1049023x0000008x. [DOI] [PubMed] [Google Scholar]
- Meredith JW, Evans G, Kilgo PD, MacKenzie E, Osler T, McGwin G, Cohn S, Esposito T, Gennarelli T, Hawkins M, Lucas C, Mock C, Rotondo M, Rue L. A Comparison of the Abilities of Nine Scoring Algorithms in Predicting Mortality. J Trauma. 2002;53(4):621–8. doi: 10.1097/00005373-200210000-00001. [DOI] [PubMed] [Google Scholar]
- Osler T, Baker S, Long W. A Modification of the injury Severity Score that Both Improves Accuracy and Simplifies Scoring. J Trauma. 1997;43(6):922–6. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
- Osler T, Rogers FB, Badger GJ, Healey M, Vane DW, Shackford SR. A Simple Mathematical Modification of TRISS Markedly Improves Calibration. J Trauma. 2002;53(4):630–4. doi: 10.1097/00005373-200210000-00002. [DOI] [PubMed] [Google Scholar]
- Sacco W, MacKenzie E, Champion HR, Davis EG, Buckman RF. Comparison of Alternative Methods for Assessing Injury Severity Based on Anatomic Descriptors. J Trauma. 1999;47(3):441–6. doi: 10.1097/00005373-199909000-00001. [DOI] [PubMed] [Google Scholar]
- Stephenson SCR, Langley JD, Civil ID. Comparing Measures of Injury Severity for Use with Large Databases. J Trauma. 2002;53(4):326–32. doi: 10.1097/00005373-200208000-00023. [DOI] [PubMed] [Google Scholar]
- Whitaker IY. Injury Severity and Survival Probabilities in Inpatients. Doctoral of Nursing Dissertation; Universidade de São Paulo, Brazil. 2000. [Google Scholar]