Abstract
Approximately one-half of vehicle occupants with traumatic brain injury (TBI) have a mild TBI (admission Glasgow Coma Scale (GCS) score of 13–15 with transient loss of consciousness). However, despite the label of “mild”, many of these injuries result in long-term consequences; frequently these sequelae go unrecognized, as the patients are lost to medical follow-up. The Crash Injury Research Engineering Network (CIREN) project affords us the opportunity to examine the crash circumstances, injury sources and outcomes of mild TBI cases in greater detail.
The incidence rate of fatal and hospitalized TBI was estimated to be 91/100,000 population in 1994 (Thurman et al., 1999). Each year in the U.S., for every person who dies of a brain injury, five are admitted to hospitals, and an additional 26 seek outpatient medical treatment (Kraus, 1993). More than 75% of brain injuries are considered mild (Evans, 1992), and many of these result from motor vehicle collisions. However, few studies have focused on the characteristics of crashes associated with these injuries.
Although the majority of patients with mild TBI improve within three months of injury, it is estimated that approximately 20% experience symptoms, such as memory problems, depression, or cognitive difficulties that may continue for six months or longer (Alexander, 1995; Jacobson, 1995; Gronwall, 1991). Such problems impact not only the patients themselves but also their families and society.
In a previous analysis of injuries among drivers admitted to Maryland hospitals following car crashes, it was noted that 37.7% incurred a TBI (Dischinger, 1999). Among this group, the majority of injuries (79.2%) were minor in nature, as defined by a maximum Abbreviated Injury Scale score (MAIS) of 1 or 2 for the head. As contrasted with more serious TBIs, minor TBIs were found to be more prevalent among women, younger drivers, and those who were wearing seatbelts at the time of the collision. They were also more prevalent in frontal, as compared to lateral, crashes. No differences were noted in either the incidence or severity of brain injury in association with airbags, but the number of airbags was relatively small, as the analysis was based on drivers hospitalized between 1994 and 1996. Also, in that study, based on police crash reports, detailed crash circumstances were not available, as crash reconstruction analyses were not conducted.
In a 2003 Canadian study of head injuries in severe motor vehicle crashes by Stewart et al., it was reported that airbag deployment did not significantly lower a driver’s odds of incurring a head injury, but did significantly lower the severity of head injury. Their study, however, was based on trauma registry data and did not include data on the actual forces, contact points, intrusions and other biomechanical factors associated with these injuries.
The National Highway Traffic Safety Administration’s (NHTSA) CIREN project allows for a more detailed analysis of injury circumstances and sources. Loo et al. examined CIREN crash reconstruction and injury data to identify the pattern of injuries resulting from crashes and the role of airbag protection. The authors suggest that “the most important effect of the airbag, used either as a supplemental or primary restraint system in the absence of seatbelts, is to reduce the severity of brain injury.” However, they also noted that the total incidence of brain injuries remained slightly higher in airbag cases, perhaps because of the mild concussions induced by the airbag itself (Loo et al., 1996).
The purpose of this study is to focus on the question of mild TBI from two separate perspectives. First, we examine the CIREN database for all network centers and compare driver and crash circumstances for patients with mild vs moderate/severe brain injuries. For this part of the analysis, mild TBIs are defined as a GCS score of 13–15 with a transient loss of consciousness and no identifiable lesions on computed tomography (CT) scan. Secondly, we examine the long-term follow-up data, obtained from patient interviews, for all patients admitted to the Baltimore center with a GCS of 15 (13s and 14s were excluded due to small numbers) comparing those with and without mild TBI (as defined by loss of consciousness, identified from either the patient’s chart or interview, and a negative CT scan).
The impact of mild TBIs upon patients, their families, and society, is often overlooked since patients may be lost to the medical care system following hospital discharge. Physicians who treat trauma patients in follow-up clinics after their discharge from the hospital are well aware of the potential residual effects of these injuries, but the magnitude and impact of this problem has not been well documented, at least in terms of motor vehicle-related trauma and current vehicle safety standards. The opportunity to obtain such information about long-term outcomes is a valuable aspect of the CIREN project, and one that is not available from other datasets such as NHTSA’s National Accident Sampling System (NASS), or Crash Outcome Data Evaluation System (CODES).
METHODS
The data presented were generated as part of the NHTSA CIREN project. The mission of the CIREN study is to improve the prevention, treatment, and rehabilitation of motor vehicle crash injuries to reduce deaths, disabilities, and human and economic costs. The CIREN approach is multidisciplinary in scope, involving the efforts of physicians, engineers, epidemiologists, social workers, and others, whose collective goal is a better understanding of the causes and outcomes of crash related injury. Such insights can lead to more focused and effective prevention measures as well as an improved understanding of the medical consequences, both immediate and long-term.
CIREN investigators focus on patients admitted to trauma centers following a motor vehicle crash and give special attention to those who are injured despite the availability of newer vehicles and modern occupant restraints, including airbags. Patients eligible for selection include those in vehicles aged 6 years or newer. The crash investigation utilizes physical evidence such as skid marks, vehicular damage measurements, and occupant contact points coupled with the investigator’s expert knowledge and experience of vehicle dynamics and occupant kinematics in order to determine the pre-crash, crash, and post-crash movements of involved vehicles and occupants. Medical experts and engineers go over the evidence for each case, including documentation of crash forces, contact points and intrusions; in addition, photographs, x-rays and CT scans of the patient’s injuries are presented. Detailed information on the causes of injuries is obtained from this case review. Patients are also interviewed in the hospital to obtain a pre-injury psychosocial history (based on perceptions of their pre-injury status) and provide additional information on the circumstances of the crash, if known. They are again interviewed at 6 and 12 months post-crash so that the long term consequences of injuries can be more fully understood, in terms of their impact on cognitive, physical, psychosocial and economic factors.
Data from all ten of the CIREN centers is entered into a centralized database maintained by the United States Department of Transportation. Thus, in addition to utilizing their own data, each of the centers has the ability to access CIREN-wide data. Although the “core” data for each of the centers, including reconstruction and injury documentation, is standardized, some centers have specific research interests, and thus, may augment their data with other information. For example, at the Baltimore center, patients are interviewed by a clinical social worker following their discharge from the hospital. While all centers obtain data using the SF-36, a widely used measure for assessing patient-reported health outcomes, the Baltimore center also obtains more detailed information regarding various psychosocial factors, including post-injury cognitive and behavioral problems.
Each interview requires approximately 30–40 minutes and includes the following aspects: 1) pre-injury health information and trauma history, 2) two questions that measure depression (Whooley, 1997), 3) questions regarding cognitive function, 4) questions diagnostic of post-traumatic stress disorder (PTSD), and 5) measurement of the impact of injury on general health status (Short Form 36 Health Survey [SF-36]).
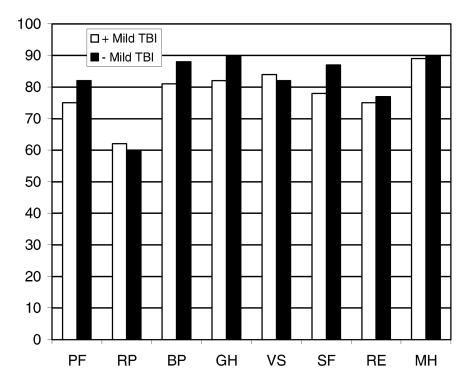
The SF-36 includes multi-item scales that measure eight dimensions of health: physical function (PF), role physical (RP), body pain (BP), general health perception (GH), vitality (VS), social function (SF), role emotional (RE), and mental health (MH). Although the presence of mild TBI may be revealed by the mental health scores of the SF-36, these questions need to be supplemented with additional measures of cognitive function, as the SF-36 has been shown to be deficient in this regard (Mackenzie, 2002). These additional questions improve the identification of problems associated with TBI, especially in patients with multiple trauma issues. Finally, other questions address return to employment, inpatient and outpatient rehabilitation therapy, persistence of legal issues, and costs associated with rehabilitation.
The current study addresses the issue of TBI, specifically that of mild brain injury. For the purpose of this analysis, mild TBI is defined as injury to the head with a total GCS between 13 and 15, no identifiable lesions and associated symptoms such as loss of consciousness. There were 133 mild TBI patients included in the CIREN database; approximately 77% experienced a loss of consciousness of less than one hour, 6% had cerebral concussion, and the remainder reported amnesia, headache or dizziness, etc. Moderate or severe TBI cases thus include patients with a GCS of less than 13, with or without findings of a brain lesion on CT scan (n=155). The GCS included in the analysis was based on the earliest determination available, which may have been at the scene, in transit, or upon arrival at the trauma center.
Point of impact was based on the number one rank as determined from the Collision Deformation Classification (CDC), a program used by the crash reconstructionists (SAE, 1980). The change in velocity at the time of the collision (delta v) was also determined in this manner, from the first ranked delta v, based on the CDC. Airbag deployment was defined as any airbag deployed in association with the driver’s seating position; that is, some drivers may have had two airbags, with only one deployed during the crash.
In addition to an analysis of CIREN-wide data on the circumstances associated with mild TBI, we also examined the long-term outcomes among a population of 96 CIREN patients who were admitted to the R Adams Cowley Shock Trauma Center in Baltimore and had baseline GCS scores of 15 (13s and 14s were excluded due to small numbers of cases). A comparison was made between those with (N= 56) and without (N=40) mild TBI, based on a reported loss of consciousness either from the patient interview or chart review.
RESULTS
There were a total of 1,409 CIREN cases in the database at the time of this analysis. Of those, 288 were drivers, aged 16 or older, who were involved in a frontal or left lateral crash, and had a TBI. Of the 288 cases with TBI, 133 (46.2%), had a mild TBI.
The demographic and crash characteristics of the 288 CIREN cases with TBI are shown in Table 1. Patients with mild TBIs are compared to those with moderate/severe TBIs. There were no differences with regard to gender. However, those with mild TBIs were significantly more likely to be between the ages of 20 and 59, as compared to those with more severe injuries; approximately 19% of those with mild TBI were either 16–19 or 60 or older, as compared to 40% of the group with moderate/severe TBI. In addition, those with more serious TBI injuries had more multiple trauma; Injury Severity Scores (ISS) were significantly higher for the cases with moderate/severe injuries as compared to those with mild TBI (34.0 vs. 14.0, p<.001).
Table 1.
Demographic and Crash Characteristics (All CIREN Centers, N=288)
| Mild TBI (N=133) % | Moderate/Severe TBI (N=155) % | P-Value | |
|---|---|---|---|
| Age: 16–19 | 9.0 | 18.1 | |
| 20–39 | 48.9 | 43.2 | |
| 40–59 | 32.3 | 17.4 | |
| 60+ | 9.8 | 21.3 | <0.001 |
| Male | 54.9 | 56.8 | NS |
| Median ISS | 14 | 34 | <0.001 |
| Died | 0.0 | 42.2 | <0.001 |
| Point of Impact: Frontal | 82.0 | 65.2 | |
| Left Lateral | 18.1 | 34.8 | <0.001 |
| Belted | 50.0 | 54.1 | NS |
| Airbag Deployed | 90.9 | 83.1 | 0.06 |
| Delta V < 30 miles | 56.6 | 58.9 | NS |
| Median Delta V | 28.7 | 28.1 | NS |
Patients with mild TBIs were significantly more likely to have been injured in frontal vs. lateral collisions (82.0% vs. 65.2%, p<.001). There were no differences between the two groups with respect to seatbelt use, airbag deployment or delta v.
Table 2 ranks the injury sources associated with mild vs. moderate/severe TBIs. For mild TBI, 24.8% of cases were attributable to the airbag, while another 10.9% were due to “non-contact” sources. Injury source was listed as “unknown” for an additional 11.6%.
Table 2.
Most Common Injury Source of TBI (All CIREN Centers, N=288)
| Rank | Mild TBI (N=133) | Moderate/Severe TBI (N=155) | ||
|---|---|---|---|---|
| % | % | |||
| 1 | Driver side air bag | 24.8 | Driver side air bag | 14.8 |
| 2 | Injury source unknown | 11.6 | Left A (A1/A2) - pillar | 9.0 |
| 3 | Other non-contact source | 10.9 | Other non-contact source | 8.4 |
| 4 | Left A (A1/A2) - pillar | 7.0 | Injury source unknown | 5.8 |
| 5 | Windshield | 5.4 | Windshield | 5.8 |
| 6 | Steering wheel rim | 4.7 | Front header | 5.2 |
| 7 | Sun visor | 4.7 | Left B-pillar | 5.2 |
| 8 | Front header | 3.9 | Other vehicle object | 5.2 |
| 9 | Left B-pillar | 3.1 | Roof left side rail | 5.2 |
| 10 | Roof or convertible top | 3.1 | Left side window glass | 3.9 |
As shown in Figure 1, based on the SF-36, there were no major differences in the percentage change from baseline (based on the patient’s perceptions of their pre-injury status) to one-year post injury among the eight domains measured. It is apparent that, with the exception of “role physical” and “vitality”, those with mild TBI had slightly lower recovery rates, but the differences were very small. This may be due, in part, to the fact that trauma patients have multiple injuries and that the SF-36 is not designed to measure cognitive and other outcomes, often quite subtle, associated with mild TBI. However, the small sample size might also limit the detection of small differences between the two groups.
Figure 1.
Percentage Return to Pre-Injury Functioning at One Year Patients with a GCS of 15: Findings from the SF-36. (Baltimore Center, N=96)
Table 3 shows outcomes at six months and one-year post-injury for all Baltimore CIREN cases with an admission GCS of 15 (i.e. a normal score) and at least one year of follow-up. In contrast to the earlier analyses shown in Tables 1 and 2, this group includes drivers and occupants and is not necessarily limited to frontal and left lateral impacts. Among this group 58% had a mild TBI as reflected by a reported loss of consciousness identified either from the patient’s chart or in-hospital interview. A comparison of outcomes at 6 and 12 months post-trauma is made for those with and without a mild TBI. Those with mild TBI had higher rates of cognitive problems, behavioral changes, and depression at 6 and 12 months post-injury, as compared to patients without TBI. For PTSD, on the other hand, rates appeared to be higher among those without mild TBI at 6 months, but not significantly different at 12 months.
Table 3.
Psychosocial Outcomes for those with and without Mild TBI (Baltimore Center, N=96)
| Mild TBI | |||
|---|---|---|---|
| Yes (%)(N=56) | No (%)(N=40) | P-Value | |
| Cognitive Problems | |||
| - 6 months | 39.3 | 17.5 | 0.02 |
| -12 months | 32.1 | 17.5 | NS |
| Behavioral Changes | |||
| - 6 months | 39.3 | 27.5 | NS |
| - 12 months | 26.8 | 7.5 | 0.02 |
| PTSD | |||
| - 6 months | 19.6 | 27.5 | NS |
| - 12 months | 21.4 | 17.5 | NS |
| Depression | |||
| - 6 months | 57.1 | 42.5 | NS |
| - 12 months | 50.0 | 30.0 | 0.05 |
Further analyses (not shown) revealed that the difference in the rates of depression between patients with and without mild TBI was especially apparent for those patients with no reported pre-injury depression. For this group of 57 patients, the incidence of depression at one year among those with a mild TBI was 43.8%, compared to 20% among those without TBI (p=.06).
DISCUSSION
In a 1999 report from the Institute of Medicine on “Reducing the Burden of Injury”, the authors note that “despite significant strides in the past decade, the biomechanical properties of the brain and the biologic response of the brain to injury are not well characterized.” This would seem to be especially so for mild brain injuries, which frequently do not involve contact with the vehicle interior and may occur in both high and low delta v collisions.
It is apparent that mild TBIs resulting from motor vehicle collisions are common and that they may occur even in new vehicles with modern occupant restraint systems. Numerous studies have now shown that airbags are associated with a decrease in serious TBIs; (Pintar et al., 2000; Loo, 1996) at the same time, however, they have been associated with an increase in mild TBIs. While this trade-off is a beneficial one, attention needs to be given to the magnitude of the problem of mild TBI, and the long-term consequences of injuries which are often overlooked, even in the trauma center setting. In 1996, Dischinger et al, in an analysis of linked hospital and police report records, noted that “the airbag group had a lower incidence of spinal, thoracic, abdominal and serious facial injuries; however, that group also had a higher incidence of brain injuries and upper and lower extremity fractures.” However, this analysis did not include data on GCS Scores, which provide important detail concerning the severity of the injury. Also, no data were available on the delta v’s associated with the collisions.
Segui-Gomez, in an analysis based on NASS data in 2000, pointed out the fact that “airbag deployment exerts a net injurious effect in low-severity crashes and a net protective effect in high-severity crashes.” That is, at lower delta v’s airbags may cause injuries, whereas at higher delta v’s these injuries may be prevented. Based on the CIREN data in Table 2, it is apparent that a significantly greater proportion of mild vs. moderate/severe TBIs had airbag ranked as the primary cause of injury (24.8% vs. 14.8%, p=0.03), in part because the mild injuries are more likely to result from frontal impacts. However, there was no significant difference in the median delta v for those crashes resulting in mild vs. moderate/severe TBIs, perhaps because patients admitted to trauma centers tend to be involved in crashes at the higher end of the range of delta v’s. Nor was there a difference in the proportion of injuries attributable to the airbag when comparing patients in crashes with high and low velocity changes (data not shown). For mild TBIs almost one fourth (22.5%) were assigned an injury source of “unknown” or “other non-contact source”, as compared with 14.2% of the moderate/severe group. Thus, many of these injuries result from movement of the head during the crash, frequently without contact with components of the vehicle interior.
CIREN affords us an important opportunity to focus on this issue and to gain a better understanding of the causes and outcomes of mild TBI. Despite the advances made in vehicle safety and the reduction of serious TBI injuries, it is apparent that mild TBIs are still prevalent. Parents and coaches are often acutely aware of the consequences of a concussion in student athletes, and may be alert to subsequent signs and symptoms. However, following a car crash, especially when there may be multiple injuries, attention is frequently diverted to the ankle fracture, ruptured spleen, or other more apparent injury, with no expectation of future problems that might be associated with mild TBI. Trauma clinicians who see patients in “follow-up” clinics are acutely aware of this problem, as family members frequently voice concerns over the patient’s changes in behavior or other issues.
It may be safely assumed that patients such as the ones enrolled in the CIREN study represent only the “tip of the iceberg” with respect to the problem of TBI. As estimated by Guerrero et al. in 2000, the TBI-related Emergency Department (ED) visit incidence rate of 329 per 100,000 population per year was more than 4 times the rate of fatal and hospitalized TBI in 1994. In addition to ED visits, patients with isolated TBI, i.e. no other injuries, might be seen by their own physicians or even not at all, if they walked away from the collision. Sometimes the assumption that no injury has occurred is based on the fact that the GCS score is 15; however, other studies have shown that GCS scores within the range of 13–15 are not clearly predictive of neuropsychiatric sequelae at follow-up (McCullagh et al., 2001).
Thus, physicians and families need to be more aware of the consequences of mild TBI following motor vehicle crashes. Patients with mild TBI, in addition to multisystem trauma, may have more difficulty returning to pre-injury levels of functioning. Even those with normal GCS scores may exhibit cognitive problems and be at risk of depression and behavioral changes. Conversely, patients who experience depression and/or PTSD post-trauma, may also develop cognitive problems such as poor attention and concentration. Once these problems are identified, counseling and education may be helpful in mitigating these adverse effects, and preventing more long-term problems.
ACKNOWLEDGMENTS
The authors would like to acknowledge the collaborating CIREN Centers for their data, which were included in Tables 1 and 2.
REFERENCES
- Alexander, MP. Mild traumatic brain injury: pathophysiology, natural history, and clinical management. Neurology. 1995;45:1253–1260. doi: 10.1212/wnl.45.7.1253. [DOI] [PubMed] [Google Scholar]
- Collision Deformation Classification. Society of Automotive Engineers; Mar, 1980. Paper J224. [Google Scholar]
- Cushman JG, Agarwal N, Fabian TC, Garcia V, et al. Practice Management Guidelines for the Management of Mild Traumatic Brain Injury: The EAST Practice Management Guidelines Work Group. J Trauma. 2001;51(5):1016–1026. doi: 10.1097/00005373-200111000-00034. [DOI] [PubMed] [Google Scholar]
- Dischinger PC, Ho SM, Kerns TJ, Brennan P. Patterns of Injury in Frontal Collisions With and Without Airbags. Proceedings of IRCOBI. 1996:311–319. [Google Scholar]
- Dischinger PC, Ho SM, Kufera JA. The epidemiology of traumatic brain injury: a statewide study of hospitalized Maryland drivers. Proceedings of the AAAM. 1999:71–88. [Google Scholar]
- Evans RW. The postconcussion syndrome and the sequelae of mild head injury. Neurol Clin. 1992;10:815–847. [PubMed] [Google Scholar]
- Gronwall D. Minor head injury. Neuropsychology. 1991;5:253–265. [Google Scholar]
- Guerrero JL, Thurman DJ, Sniezek JE. Emergency department visits associated with traumatic brain injury: United States, 1995–1996. Brain Injury. 2000;14(2):181–186. [PubMed] [Google Scholar]
- Jacobson RR. The post-concussion syndrome: physiogenesis, psychogenesis and malingering. An integrative model. Journal of Psychosomatic Research. 1995;39:675–693. doi: 10.1016/0022-3999(95)00006-5. [DOI] [PubMed] [Google Scholar]
- Kraus JF. Epidemiology of Head Injury. In: Paul R, editor. In Head Injury. Cooper: Williams and Wilkins; 1993. [Google Scholar]
- Loo GT, Siegel JH, Dischinger PC, Rixen DR, Burgess AR, et al. Airbag protection versus compartment intrusion effect determines the pattern of injuries in multiple trauma motor vehicle crashes. J Trauma. 1996;41(6):935–951. doi: 10.1097/00005373-199612000-00001. [DOI] [PubMed] [Google Scholar]
- MacKenzie EJ, McCarthy ML, Ditunno JF, Forrester-Staz C, Gruen GS, Marion DW, Schwab WC. Using the SF-36 for characterizing outcome after multiple trauma involving head injury. J Trauma. 2002;52(3):527–34. doi: 10.1097/00005373-200203000-00018. [DOI] [PubMed] [Google Scholar]
- McCullagh S, Ouchterlony D, Protzner A, Blair N, Feinstein A. Prediction of neuropsychiatric outcome following mild trauma brain injury: an examination of the Glasgow Coma Scale. Brain Injury. 2001;15(6):489–497. doi: 10.1080/02699050010007353. [DOI] [PubMed] [Google Scholar]
- Pintar FA, Yognandan N, Gennarelli TA. Airbag Effectiveness on Brain Trauma in Frontal Crashes. Proceedings of the AAAM. 2000:149–170. [PMC free article] [PubMed] [Google Scholar]
- Segui-Gomez M. Driver air bag effectiveness by severity of crash. AJPH. 2000;90(10):1575–1581. doi: 10.2105/ajph.90.10.1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart TC, Girotti MJ, Nikore V, Williamson J. Effect of airbag deployment on head injuries in severe motor vehicle crashes in Ontario, Canada. J Trauma. 2003;54:266–272. doi: 10.1097/01.TA.0000038699.47295.2D. [DOI] [PubMed] [Google Scholar]
- Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14(6):602–15. doi: 10.1097/00001199-199912000-00009. [DOI] [PubMed] [Google Scholar]
- Ware JJ, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Whooley M, Avins A, Miranda J, Browner W. Case finding instruments for depression. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]