Abstract
The olfactory mucosa, located in the nasal cavity, is in charge of detecting odours. It is also the only nervous tissue that is exposed to the external environment and easily accessible in every living individual. As a result, this tissue is unique for anyone aiming to identify molecular anomalies in the pathological brain or isolate adult stem cells for cell therapy.
Molecular abnormalities in brain diseases are often studied using nervous tissue samples collected post-mortem. However, this material has numerous limitations. In contrast, the olfactory mucosa is readily accessible and can be biopsied safely without any loss of sense of smell1. Accordingly, the olfactory mucosa provides an "open window" in the adult human through which one can study developmental (e.g. autism, schizophrenia)2-4 or neurodegenerative (e.g. Parkinson, Alzheimer) diseases4,5. Olfactory mucosa can be used for either comparative molecular studies4,6 or in vitro experiments on neurogenesis3,7.
The olfactory epithelium is also a nervous tissue that produces new neurons every day to replace those that are damaged by pollution, bacterial of viral infections. This permanent neurogenesis is sustained by progenitors but also stem cells residing within both compartments of the mucosa, namely the neuroepithelium and the underlying lamina propria8-10. We recently developed a method to purify the adult stem cells located in the lamina propria and, after having demonstrated that they are closely related to bone marrow mesenchymal stem cells (BM-MSC), we named them olfactory ecto-mesenchymal stem cells (OE-MSC)11.
Interestingly, when compared to BM-MSCs, OE-MSCs display a high proliferation rate, an elevated clonogenicity and an inclination to differentiate into neural cells. We took advantage of these characteristics to perform studies dedicated to unveil new candidate genes in schizophrenia and Parkinson's disease4. We and others have also shown that OE-MSCs are promising candidates for cell therapy, after a spinal cord trauma12,13, a cochlear damage14 or in an animal models of Parkinson's disease15 or amnesia16.
In this study, we present methods to biopsy olfactory mucosa in rats and humans. After collection, the lamina propria is enzymatically separated from the epithelium and stem cells are purified using an enzymatic or a non-enzymatic method. Purified olfactory stem cells can then be either grown in large numbers and banked in liquid nitrogen or induced to form spheres or differentiated into neural cells. These stem cells can also be used for comparative omics (genomic, transcriptomic, epigenomic, proteomic) studies.
Keywords: Neuroscience, Issue 54, stem cell, nose, brain, neuron, cell therapy, diagnosis, sphere
Protocol
1. Collection of Olfactory Mucosa in Rats
Begin by preparing three 35 mm Petri dishes filled with DMEM/HAM F12 culture medium in a clean culture hood.
Any method of euthanasia must be approved in advance by the institution's animal care and use committee and carried out by qualified personnel. After the rat has entered deep anesthesia with sodium pentobarbital or other injectable forms of anesthesia such as ketamine/xylazine, decapitate and remove the skin. Inhalant anesthetics should be avoided. Adequacy of anesthesia will be assessed by toe pinch prior to decapitation. Remove the lower jaw with scissors and with the help of a rongeur, eliminate the facial muscles on both sides.
Starting from the back of the incisors, remove with a rongeur the bone covering the nasal cavity, one side at a time. The olfactory turbinates come into sight as orange/brown organs located in the back of the nose.
Delicately discard the turbinates with a forceps. Using a 26 gauge needle, isolate the olfactory mucosa lying on the septum by cutting the tissue along three lines: the arc of the perpendicular plate, the cribriform plate and the ceiling of the nasal cavity.
Collect biopsies on both sides and transfer them in a DMEM/HAM F12-filled Petri dish. This procedure should not take longer than 10 minutes from the onset euthanasia.
Now, in order to remove the mucus, transfer the biopsies two times in medium-filled Petri dishes.
2. Collection of Olfactory Mucosa in Humans
This procedure should be carried out by an Ear Nose and Throat (ENT) surgeon, in accordance with the relevant local ethical committee(s), and every outpatient should sign an informed consent form.
Using a 0° or 30° rigid endoscope (4 mm diameter), inspect both nasal cavities and assess the putative presence of polyps or any inflammatory lesion. Choose the best nasal cavity, taking into account the deviation of the septum.
Using a cotton applicator, apply a local anesthetic, such as lidocaine with epinephrine, for 10 minutes.
With a throughcut ethmoid forceps, collect a two square millimeter biopsy either at the root of the medial aspect of the middle turbinate or on the septum in the dorsomedial area.
The olfactory biopsy is then transferred, using a sterile needle, into a sterile 2 ml tube filled with 1 ml of DMEM/HAM F12. Tip the tube upside down to make sure that the biopsy is immersed in the culture medium.
Insert the tube in a refrigerated container and transport it to the research laboratory. At this stage, the biopsy can be used per se for comparative molecular studies focused on specific brain diseases or processed for generating stem cells.
3. Isolation of Olfactory Stem Cells from Human and Rat Mucosa
Wash the biopsies in DMEM/HAM F12. Incubate the biopsies in a Petri dish filled with 1 ml of dispase II solution (2.4 IU/ml), for 1 hour at 37°C.
Next, under a dissecting microscope with a diffracted inverted light, the olfactory epithelium is removed from the underlying lamina propria using a micro spatula.
The olfactory epithelium is thinner and looks translucent over a black background compared to the lamina propria which is striped orange/brown. Over a white background, the epithelium looks gray and the lamina propria, brown.
Once purified, transfer the lamina propria into a Petri dish filled with DMEM/HAM F12.
If the tissue is from a rodent, then cut the lamina propria into small pieces with two 25 gauge needles. Then, transfer the pieces to a 15 ml tube filled with 1 ml of collagenase IA.
In the tube, using a sterile plastic pipette, dissociate the tissue. Then, incubate the tube for 10 minutes at 37°C.
To terminate the dissociation, gently rock the tube and add 9 ml of Ca-free and Mg-free PBS and centrifuge at 200 g for 5 minutes.
Resuspend the cell pellet in DMEM/HAM F12 culture medium supplemented with 10% fetal calf serum, antibiotics and plate on plastic culture dishes.
Now, if the tissue is human, then slice the lamina propria into 3 to 4 pieces with a thickness ranging from 200 to 500 μm.
Insert each strip into its own 2 cm diameter culture dish and cover the tissue with sterile 1.3 cm diameter glass cover slips.
Then, add 500 μl of culture medium (DMEM/HAM F12 supplemented with 10% fetal calf serum and antibiotics) to each culture dish.
For either tissue type, renew the culture medium every 2 to 3 days.
Five to seven days after, stem cells will begin to invade the culture dish and after two weeks they should be confluent. When confluency is reached, passage and transfer the cells to culture flasks.
4. Sphere Formation and Neuronal Differentiation of Olfactory Stem Cells
To generate stem cell spheres, incubate the flasks for two hours at 37°C with poly-L-lysine. (TEXT: 5 g/cm2).
Plate the cells at a density of 16,000 cells per square centimeter in the treated flasks.
Every two days, feed the cells with 0.2ml per square centimeter of supplemented medium (DMEM/HAM F12 supplemented with insulin, transferrin, selenium (ITS-X, 1%), EGF (50 ng/ml) and FGF2 (50 ng/ml)).
Two to five days later, collect floating cell spheres and either re-plate or dissociate them before grafting in animal models of cell therapy.
To differentiate olfactory stem cells into neuron-like cells, cultivate them for 21 days in Neurobasal medium containing B-27, penicillin, streptomycin, glutamine and glutamate.
Then make medium changes every 3 days. Neuron-like cells should appear after two to three weeks.
5. Representative Results:
Nasal human explant-outgrowing stem cells (Figure 2A) are dividing rapidly and confluency can be reached within one to two weeks. One key feature of stemness, nestin expression, was evaluated (Figure 2B). When grown on poly-L-lysine with a serum-free culture medium supplemented with EGF (50 ng/ml) and FGF2 (50 ng/ml), olfactory stem cells give rise to spheres (figure 2C). When grown in serum-containing culture medium newly plated spheres give rise to GFAP-expressing cells (˜50%), tubulin-expressing cells (˜10-15%) and O4-expressing cells (˜2-5%)9 (Figures 2D-F). However, the fate of the sphere-derived cells can be modified. For example, when grown in a Neurobasal culture medium supplemented with B27 and glutamate, most of the nasal olfactory stem cells into neuron-like cells expressing β-III tubulin (Figure 2G) and MAP2 (Figure 2H).
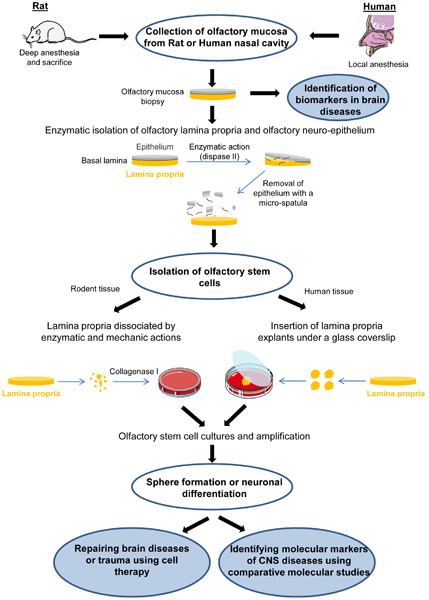 Figure 1. Overall scheme of the experiment. Olfactory mucosa biopsies are excised from rat or human nasal cavity. Explants can be used per se for comparative molecular studies aiming to identify biomarkers in brain diseases. For isolating olfactory stem cells, the interactions between the lamina propria and the neuro-epithelium are disrupted with the dispase II enzyme and, after 45 minutes, the epithelium is removed with a micro-spatula. Rodent olfactory stem cells are further selected by dissociating the lamina propria with collagenase IA. For human tissue, pieces of olfactory lamina propria are cultured under glass coverslip until outgrowing stem cells invade the whole well. After proliferation, using an appropriate culture medium, olfactory stem cells can generate spheres or differentiate into neuron-like cells. Olfactory stem cells can be used to i) repair brain diseases or trauma or ii) identify molecular markers of central nervous system diseases. Illustrations are made with the help of Servier Medical Art.
Figure 1. Overall scheme of the experiment. Olfactory mucosa biopsies are excised from rat or human nasal cavity. Explants can be used per se for comparative molecular studies aiming to identify biomarkers in brain diseases. For isolating olfactory stem cells, the interactions between the lamina propria and the neuro-epithelium are disrupted with the dispase II enzyme and, after 45 minutes, the epithelium is removed with a micro-spatula. Rodent olfactory stem cells are further selected by dissociating the lamina propria with collagenase IA. For human tissue, pieces of olfactory lamina propria are cultured under glass coverslip until outgrowing stem cells invade the whole well. After proliferation, using an appropriate culture medium, olfactory stem cells can generate spheres or differentiate into neuron-like cells. Olfactory stem cells can be used to i) repair brain diseases or trauma or ii) identify molecular markers of central nervous system diseases. Illustrations are made with the help of Servier Medical Art.
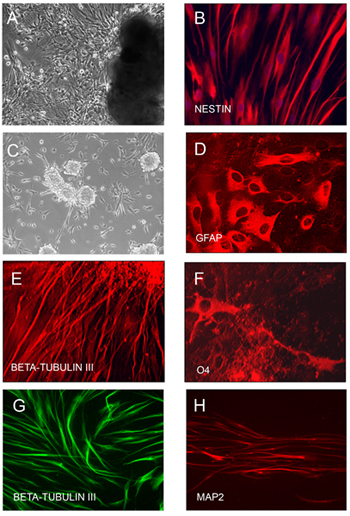 Figure 2. Culture and differentiation of nasal human olfactory stem cells. Human stem cells growing out of the lamina propria explant (A) are dividing rapidly, when cultivated in a serum-containing medium. Stem cells express the stemness marker nestin (B). When plated on poly-L-lysine-coated plastic and cultivated in a serum-free culture medium supplemented with EGF and FGF2, olfactory stem cells generate spheres (C). Sphere-derived cells, when plated in serum-containing culture medium, give rise to GFAP-expressing cells (˜50%), tubulin-expressing cells (˜10-15%) and O4-expressing cells (˜2-5%)9 (D-F). When grown in a Neurobasal culture medium supplemented with B27 and glutamate, they differentiate into neuron-like cells expressing β-III tubulin (G) and MAP2 (H).
Figure 2. Culture and differentiation of nasal human olfactory stem cells. Human stem cells growing out of the lamina propria explant (A) are dividing rapidly, when cultivated in a serum-containing medium. Stem cells express the stemness marker nestin (B). When plated on poly-L-lysine-coated plastic and cultivated in a serum-free culture medium supplemented with EGF and FGF2, olfactory stem cells generate spheres (C). Sphere-derived cells, when plated in serum-containing culture medium, give rise to GFAP-expressing cells (˜50%), tubulin-expressing cells (˜10-15%) and O4-expressing cells (˜2-5%)9 (D-F). When grown in a Neurobasal culture medium supplemented with B27 and glutamate, they differentiate into neuron-like cells expressing β-III tubulin (G) and MAP2 (H).
Discussion
The techniques presented here make the rodent and human olfactory mucosa a useful model for clinical research into the causes of neurodevelopmental and neurodegenerative diseases as well as a tool for repairing the pathological or traumatized brain. The protocol is relatively straightforward and can be easily carried out by an experienced cell biologist. The success rate for the biopsy and culture techniques is high.
Critical steps
For the collection of rodent olfactory mucosa, it is recommended not to exceed a time limit of 10 minutes between euthanasia and the final excision of the olfactory tissue.
The dissociation of the rodent olfactory lamina propria is usually achieved after 10 min. incubation in collagenase IA. If not, we recommend to collect the day after the supernatant in which undissociated bits of lamina propria float, centrifuge it at 200 g and mechanically dissociate the floating lamina using a Pasteur pipette before replating the cells in a new well. The first well containing the already attached cells is filled with fresh culture medium.
For the human lamina propria, which is more compact than the rodent tissue, we do not recommend an enzymatic dissociation. The tissue is sliced and each explant is inserted between the bottom of the plastic dish and a glass coverslip. Successful cultures include explants whose thickness range from 200 to 500 μm.
Possible modifications
The current protocol can be slightly modified in order to generate olfactory neurons in vitro. For that purpose, the neuro-epithelium is not removed and the whole olfactory mucosa is sliced with a McIlwain chopper (200 μm thickness). Each explant is plated in a dish, partially dried for one hour and then rehydrated with FCS-containing culture medium. During the first days post plating, epithelial and mesenchymal cells grow out of the explant. Then, neuron progenitors will migrate on the top of this cell layer and differentiate into neurons.
Purification of olfactory stem cells can be achieved using flow cytometry. Specific surface markers can be retrieved from the list published in the characterization paper11.
For transplantation experiments, it is possible to use a strain of rats whose olfactory stem cells are GFP-positive. This rat strain (Sprague Dawley, eGFP driven by the PGK promoter) is available at ITERT (Nantes, France). For inserting the GFP gene in human olfactory stem cells, we use a method based on lentivirus infection.
This paper is focused on olfactory ecto-mesenchymal stem cells. However, another cell type of interest, the olfactory ensheathing cells, can be purified from the same tissue. We described a method for their collection and purification1,17 and we used human nasal ensheathing cells for a phase I/IIa clinical trial in paraplegic patients18.
As a member of the mesenchymal stem cell superfamily, OE-MSCs are able, under appropriate culture conditions, to differentiate into adipocytes, osteocytes and myocytes11.
Future applications
We have already used human olfactory biopsies to study cellular and molecular anomalies in patients with autism, bipolar disorder, familial dysautonomia, Parkinson's disease, Alzheimer's disease and schizophrenia2-7. Theoretically, all brain diseases can be studied using nasal biopsies or peripheral olfactory stem cells.
Rodent and human nasal olfactory stem cells have already been grafted in animal models of amnesia, Parkinson's disease, cochlear damage and spinal cord trauma12-16. It is conceivable to transplant these cells into animal models of Alzheimer's disease, brain ischemia, Multiple sclerosis.
Disclosures
No conflicts of interest declared.
Acknowledgments
This work was financially supported by ANR (Agence nationale de la Recherche), AFM (Association Française contre les Myopathies), FEDER in PACA and IRME (Institut de Recherche sur la Moelle épinière et l'Encéphale). We greatfully thank Marie Pierre Blanchard (Jean Roche Institute) for her efficient help during time lapse recording.
References
- Feron F, Perry C, McGrath JJ, Mackay-Sim A. New techniques for biopsy and culture of human olfactory epithelial neurons. Arch Otolaryngol Head Neck Surg. 1998;124:861–866. doi: 10.1001/archotol.124.8.861. [DOI] [PubMed] [Google Scholar]
- Ronnett GV. Olfactory biopsies demonstrate a defect in neuronal development in Rett's syndrome. Ann Neurol. 2003;54:206–218. doi: 10.1002/ana.10633. [DOI] [PubMed] [Google Scholar]
- Feron F, Perry C, Hirning MH, McGrath J, Mackay-Sim A. Altered adhesion, proliferation and death in neural cultures from adults with schizophrenia. Schizophr Res. 1999;40:211–218. doi: 10.1016/s0920-9964(99)00055-9. [DOI] [PubMed] [Google Scholar]
- Matigian N. Disease-specific, neurosphere-derived cells as models for brain disorders. Dis Model Mech. 2010;3:11–12. doi: 10.1242/dmm.005447. [DOI] [PubMed] [Google Scholar]
- Arnold SE. Olfactory epithelium amyloid-beta and paired helical filament-tau pathology in Alzheimer disease. Ann Neurol. 2010;67:462–469. doi: 10.1002/ana.21910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone N. Olfactory stem cells, a new cellular model for studying molecular mechanisms underlying familial dysautonomia. PLoS One. 2010. [DOI] [PMC free article] [PubMed]
- McCurdy RD. Cell cycle alterations in biopsied olfactory neuroepithelium in schizophrenia and bipolar I disorder using cell culture and gene expression analyses. Schizophr Res. 2006;82:163–173. doi: 10.1016/j.schres.2005.10.012. [DOI] [PubMed] [Google Scholar]
- Roisen FJ. Adult human olfactory stem cells. Brain Res. 2001;890:11–22. doi: 10.1016/s0006-8993(00)03016-x. [DOI] [PubMed] [Google Scholar]
- Murrell W. Multipotent stem cells from adult olfactory mucosa. Dev Dyn. 2005;233:496–515. doi: 10.1002/dvdy.20360. [DOI] [PubMed] [Google Scholar]
- Tome M, Lindsay SL, Riddell JS, Barnett SC. Identification of nonepithelial multipotent cells in the embryonic olfactory mucosa. Stem Cells. 2009;27:2196–2208. doi: 10.1002/stem.130. [DOI] [PubMed] [Google Scholar]
- Delorme B. The human nose harbors a niche of olfactory ectomesenchymal stem cells displaying neurogenic and osteogenic properties. Stem Cells Dev. 2010;19:853–866. doi: 10.1089/scd.2009.0267. [DOI] [PubMed] [Google Scholar]
- Xiao M. Human adult olfactory neural progenitors rescue axotomized rodent rubrospinal neurons and promote functional recovery. Exp Neurol. 2005;194:12–30. doi: 10.1016/j.expneurol.2005.01.021. [DOI] [PubMed] [Google Scholar]
- Xiao M. Human adult olfactory neural progenitors promote axotomized rubrospinal tract axonal reinnervation and locomotor recovery. Neurobiol Dis. 2007;26:363–374. doi: 10.1016/j.nbd.2007.01.012. [DOI] [PubMed] [Google Scholar]
- Pandit SR, Sullivan JM, Egger V, Borecki AA, Oleskevich S. Functional Effects of Adult Human Olfactory Stem Cells on Early-Onset Sensorineural Hearing Loss. Stem Cells. 2011. [DOI] [PubMed]
- Murrell W. Olfactory mucosa is a potential source for autologous stem cell therapy for Parkinson's disease. Stem Cells. 2008;26:2183–2192. doi: 10.1634/stemcells.2008-0074. [DOI] [PubMed] [Google Scholar]
- Nivet E. Engraftment of human nasal olfactory stem cells restores neuroplasticity in mice. The Journal of Clinical Investigation. 2011. Forthcoming. [DOI] [PMC free article] [PubMed]
- Bianco JI, Perry C, Harkin DG, Mackay-Sim A, Feron F. Neurotrophin 3 promotes purification and proliferation of olfactory ensheathing cells from human nose. Glia. 2004;45:111–123. doi: 10.1002/glia.10298. [DOI] [PubMed] [Google Scholar]
- Mackay-Sim A. Autologous olfactory ensheathing cell transplantation in human paraplegia: a 3-year clinical trial. Brain. 2008;131:2376–2386. doi: 10.1093/brain/awn173. [DOI] [PMC free article] [PubMed] [Google Scholar]


