Abstract
Wound healing is the process of repair that follows injury to the skin and other soft tissues. Following injury, an inflammatory response occurs and the cells below the dermis (the deepest skin layer) begin to increase collagen (connective tissue) production. Later, the epithelial tissue (the outer skin) is regenerated. There are three stages to the process of wound healing: inflammation, proliferation, and remodeling. Traditionally, Ficus benghalensis is used for wound healing. Since no detailed scientific data are available regarding the wound-healing activity of F. benghalensis, the present study was designed to explore the same. The wound-healing efficacy of ethanolic and aqueous extracts of F. benghalensis was evaluated in excision and incision wound models. The parameters studied include rate of wound contraction, period of complete epithelialization, and tensile strength of incision wound. Student's t test was used to analyze the results obtained from the present study and P<0.05 was considered significant. Both the ethanolic and aqueous extracts of F. benghalensis were found to possess significant wound-healing activity, which was evidenced by decrease in the period of epithelialization, increase in the rate of wound contraction and skin-breaking strength. The present study has demonstrated that the ethanolic and aqueous extracts of F. benghalensis have properties that render them capable of promoting accelerated wound-healing activity compared with placebo control.
Keywords: Excision wound model, Ficus benghalensis, incision wound model, tensile strength
INTRODUCTION
Wound healing is the process of repair that follows injury to the skin and other soft tissues. Following injury, an inflammatory response occurs and the cells below the dermis (the deepest skin layer) begin to increase collagen (connective tissue) production. Later, the epithelial tissue (the outer skin) is regenerated. There are three stages to the process of wound healing: inflammation, proliferation, and remodeling.
The proliferative phase is characterized by angiogenesis, collagen deposition, granulation tissue formation, epithelialization, and wound contraction. Angiogenesis involves new blood vessel growth from endothelial cells. In fibroplasia and granulation tissue formation, fibroblasts excrete collagen and fibronectin to form a new, provisional extracellular matrix. Subsequently, epithelial cells crawl across the wound bed to cover it and the wound is contracted by myofibroblasts, which grip the wound edges and undergo contraction using a mechanism similar to that in smooth muscle cells.[1]
Plants or chemical entities derived from plants need to be identified and formulated for treatment and management of wounds. In this direction, a number of herbal products are being investigated at present. Various herbal products have been used in management and treatment of wounds over the years.[2]
Ficus benghalensis Linn. (Family: Moraceae) is a reputed plant in ayurvedic medicine and commonly known as “banayan tree” in ayurvedic literature. Milky juice from stem, seeds, or fruits of the plant is applied externally in rheumatism and to the soles of feet when inflamed, internally used in dysentery and diarrhea. All the parts of the plant have astringent, anti-inflammatory, antiarthritic, and antidiarrheal activities. The latex is useful in hemorrhage, diarrhea, and dysentery, as well as in hemorrhoid and inflammation.[3]
Traditionally, it is used for wounds, fever, swollen joints, inflammations, and ulcers.[4]
Various scientific studies have been carried out on F. benghalensis and various pharmacological activities have been reported. It has been reported to possess immunomodulatory,[5] hypoglycemic,[6] antioxidant,[7] antistress and antiallergic,[8] and anthelmintic[9] activities. A glucoside, bengalenoside was isolated from F. benghalensis and evaluated for hypoglycemic activity.[10] Efforts are being made all over the world to discover agents that can promote healing and thereby reduce the cost of hospitalization and save the patient from amputation or other severe complications. The need for safer and effective wound-healing agents and the lack of enough scientific data to support the claims made in ancient literature prompted the present study.
MATERIALS AND METHODS
The bark of F. benghalensis was collected in the month of August, 2006 from the local area of Meerut district and identified and authenticated by Dr. Anjula Pandey, Taxonomist, National Herbarium of Cultivated Plants, New Delhi. Voucher specimens (No. NHCP/NBPGR/2006/94/51/8929) have been kept in National Herbarium of Cultivated Plants, New Delhi, and Department of Pharmaceutical Technology, Meerut Institute of Engineering and Technology (MIET), Meerut, for future reference.
Extraction
The bark of F. benghalensis was dried under shade, crushed into small pieces, and powdered. The powder was loaded into Soxhlet extractor and was subjected to successive extraction with petroleum ether, benzene, chloroform, ethanol, and water to get different extracts. The ethanolic and aqueous extracts were concentrated to dryness using Rotary evaporator, giving yield as 4.10% w/v and 4.42%, respectively, and preserved in a refrigerator. Aliquot portions of the ethanolic and aqueous extracts of F. benghalensis were weighed and suspended in an appropriate volume of Tween 80 (2% v/v) for use on each day.
Acute Toxicity Study of the Extract
Female Albino Wistar rats weighing 200 to 220 g were used in the study. Acute oral toxicity was performed as per OECD-423 guidelines.[11] The animals were fasted overnight with water ad libitum. The starting dose of 5 mg/kg of both ethanolic and aqueous extracts was administered orally to three animals in each group. If mortality was observed in two or three animals, then the dose administered was assigned as a toxic dose. If mortality was observed in one animal, then the same dose was repeated again in three animals to confirm the toxic dose. If mortality was not observed, the procedure was repeated for further higher doses such as 50, 300, and 2 000 mg/kg body weight. Animals were observed individually after dosing at least once during the first 30 minutes, periodically during the first 24 hours, with special attention given during the first 4 hours and daily thereafter, for a total of 14 days.
Preliminary Phytochemical Studies
The different extracts were then subjected to qualitative phytochemical screening for the identification of the phytoconstituents. Although petroleum ether, benzene, and chloroform does not show any appreciable tests for the presence of different phytoconstituents, ethanolic and aqueous extracts showed positive tests for the presence of glycosides and flavonoids.
In order to follow the reasonable method of isolation of active ingredients from the plants, “activity guided” fractionation was followed. To achieve this, wound-healing activity of ethanolic and aqueous extracts was carried out at a dose level of 200 mg/kg.
Experimental Animals
The Institutional Animal Ethics Committee approved the use of animals for the present study (Ethical clearance number: 711/02/a/CPCSEA).
Healthy Wistar albino rats of both sexes weighing 200 to 220 g was used for the study. They were individually housed and were allowed free access to standard pellet diet and water ad libitum. Animals were periodically weighed before and after the experiment. The rats were anesthetized prior to and during infliction of the experimental wounds.
The surgical interventions were carried out under sterile conditions using ketamine anesthesia (120 mg/kg). Animals were closely observed for any infection and those which showed signs of infection were separated and excluded from the study and were replaced.
Wound-healing Activity
Excision and incision wound models were used to evaluate the wound-healing activity of aqueous and ethanolic extracts of F. benghalensis.
Excision Wound Model
Animals were anesthetized prior to and during creation of the wounds. The rats were inflicted with excision wounds as described by Morton and Malone.[12] The dorsal fur of the animals was shaved with an electric clipper and the anticipated area of the wound to be created was outlined on the back of the animals with methylene blue using a circular stainless steel stencil. A full thickness of the excision wound of circular area 500 mm2 and 0.2 cm depth was created along the markings using toothed forceps, a surgical blade, and pointed scissors. The entire wound was left open.[13] The animals were divided into two groups of six each. Group 1 animals were topically treated with the simple ointment base I.P. as a placebo control. The animals of group 2 were topically treated with the 10% ointment of the aqueous extract of F. benghalensis formulated in simple ointment base I.P. till complete epithelialization.[14] The wound closure rate was assessed by tracing the wound on days 0, 2, 4, 8, 12, 16, 18, and 20 post-wounding using transparency sheets and a permanent marker. The wound areas recorded were measured using a graph paper. Number of days required for falling of eschar without any residual raw wound gave the period of epithelialization.
Incision Wound Model
As with the above model, rats were anesthetized prior to and during creation of the wound. The dorsal fur of the animals was shaved with an electric clipper. A longitudinal paravertebral incision, 6 cm in length, was made through the skin and cutaneous muscle on the back, as described by Ehrlich and Hunt.[15] After the incision, surgical sutures were applied to the parted skin at intervals of 1 cm. The wounds were left undressed. The rats were given F. benghalensis extract (dissolved in tween-80, 0.5%) orally at a dose of 200 mg kg-1 day-1. The controls were given with tween-80 0.5% only. The sutures were removed on the eight post-wound day and the treatment was continued. The skin-breaking strength was measured on the 10th day by the method described by Lee.[16]
The anesthetized animal was secured to the table, and a line was drawn on either side of the wound 3 mm away from the line. This line was gripped using forceps one at each end opposed to each other. One of the forceps was supported firmly, whereas the other was connected to a freely suspended light-weight metal plate. Weight was added slowly and the gradual increase in weight, pulling apart the wound edges. As the wound just opened up, addition of weight was stopped and the weights added was noted as a measure of breaking strength in grams. Three readings were recorded for a given incision wound. The mean reading for the group was taken as an individual value of breaking strength. The mean value gives the breaking strength for a given group.
Statistical Analysis[17]
All the results obtained from various activities, as described above, were analyzed statistically by using Student's t test and P<0.05 were considered significant.
RESULT
Acute Toxicity Studies
In the acute toxicity studies, no signs of toxicity or mortality were observed at 2 000 mg/kg dose level. So, 200 mg/kg b.w. dose was taken as the therapeutic dose.
Excision Wound Model
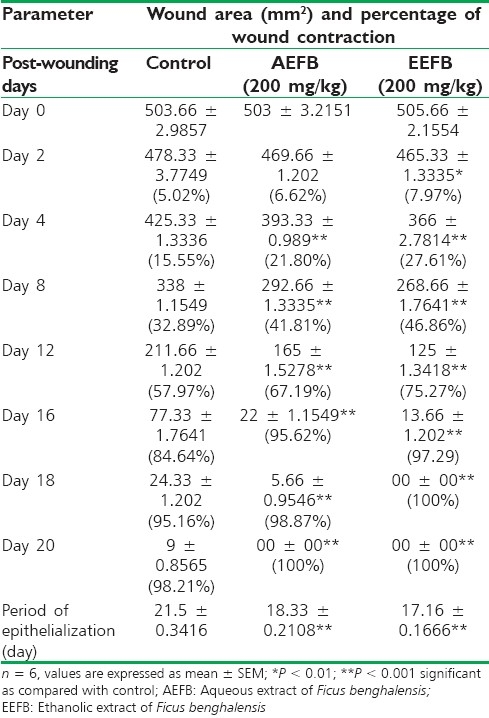
The significant increase in the wound-healing activity was observed in the animals treated with the F. benghalensis extracts compared with those who received the placebo control treatments. In the excision wound model, F. benghalensis-treated animals showed a significant reduction in the wound area (P<0.001) [Figure 1] and epithelialization period [Table 1]. The ethanolic extract showed healing in 17.16 days, whereas the aqueous extract showed healing in 18.33 days as compared with 21.50 days of control.
Figure 1.
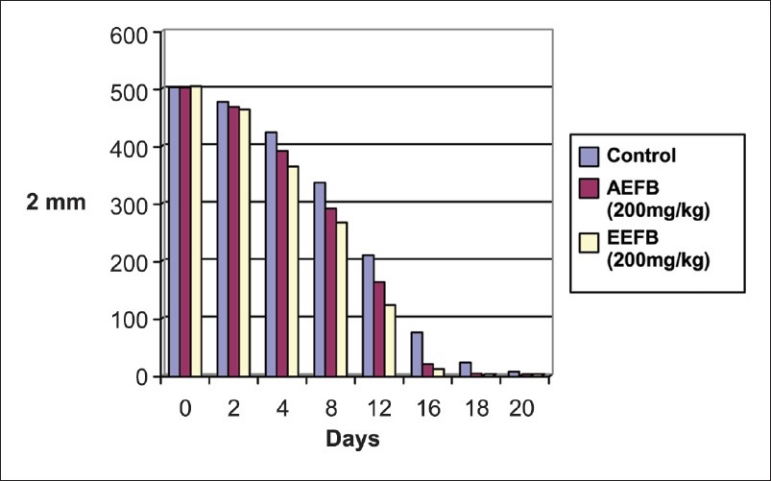
Wound-healing effect of Ficus benghalensis in excision wound model
Table 1.
Wound-healing effect of Ficus benghalensis in excision wound model
Incision Wound Model
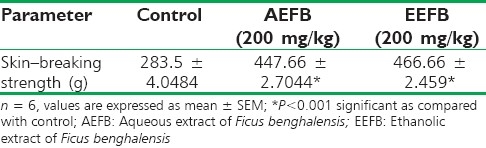
Table 2 shows the effects of the ethanolic and aqueous extracts of F. benghalensis administered orally at a dose of 200 mg kg-1 day-1 for 10 days on wound-healing activity in rats inflicted with incision wound. In the incision wound model, a significant increase in the wound-breaking strength was observed with the ethanolic and aqueous extracts of F. benghalensis when compared with the control.
Table 2.
Wound-healing effect of Ficus benghalensis in incision wound model
DISCUSSION
Wound healing is a highly complex, but orchestrated cascade of events that can roughly be divided into three overlapping phases—inflammation, granulation tissue formation, and remodeling of the extracellular matrix. These events involve several cellular phenomena such as migration, proliferation, adhesion, phenotypic differentiation, etc. Immediately after injury, there is clot formation and the earlier phases of wound repair involve inflammation and synthesis of ground substance. The ground substance mainly consists of proteoglycans, which are heterogeneous, nonfibrillar components of the extracellular matrix. These complex macromolecules are made up of a protein core linked covalently to linear heteropolysaccharides, the glycosaminoglycans (GAGS). Proteoglycans and GAGS have been shown to play important roles in all the above-mentioned events of wound healing.[18]
Biological activities in skin are due to its interaction with various binding proteins. In the tissue repair process, inflammatory cells promote the migration and proliferation of endothelial cells leading to neovascularization of connective tissue cells which synthesize extracellular matrices including collagen resulting in re-epithelialization of wounded tissue.[19] The increased tensile strength may be due to increased collagen concentration and stabilization of fibers.
The wound-healing property of F. benghalensis may be attributed to the phytoconstituents present in the plant, and the quicker process of wound healing could be a function of either the individual or the additive effects of the phytoconstituents. The early tissue approximation and increased tensile strength of the incision wound observed in our study may have been contributed by the phytoconstituents of F. benghalensis.
CONCLUSION
The present study has demonstrated that the ethanolic and aqueous extracts of F. benghalensis have properties that render them capable of promoting accelerated wound-healing activity compared with placebo control. Wound contraction and increased tensile strength support further evaluation of F. benghalensis in the topical treatment and management of wounds.
ACKNOWLEDGMENT
The authors are thankful to Dr. Anjula Pandey, Senior Scientist, Taxonomic Division, National Herbarium of Cultivated Plants, National Bureau of Plant Genetic and Resources, New Delhi, for plants identification and its authentication and also to the Department of Pharmaceutical Technology, Meerut Institute of Engineering and Technology (MIET), Meerut, for providing research facilities to carry out the work.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Nayak BS, Anderson M, Pereira LMP. Evaluation of wound-healing potential of Catharanthus roseus leaf extract in rats. Fitoterapia. 2007;78:540–4. doi: 10.1016/j.fitote.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Raina R, Prawez S, Verma PK, Pankaj NK. Medicinal plants and their role in wound healing. VetScan. 2008;3:1–7. [Google Scholar]
- 3.Patel MA, Patel PK, Patel MB. Effects of ethanol extract of Ficus bengalensis (bark) on inflammatory bowel disease. Indian J Pharmacol. 2010;42:214–8. doi: 10.4103/0253-7613.68420. Available from: http://www.ijp-online.com/text.asp?2010/42/4/214/68420 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.West Lafayette: Purdue University; 2003. [updated on 2003 Jan 01; cited in 2004]. Available from: http://www.hort.purdue.edu/newcrop/default.html . Available from: http://www.hort.purdue.edu/newcrop/cropfactsheets/ficus.html . [Google Scholar]
- 5.Gabhe SY, Tatke PA, Khan TA. Evaluation of the immunomodulatory activity of the methanol extract of Ficus benghalensis roots in rats. Indian J Pharmacol. 2006;38:271–5. [Google Scholar]
- 6.Deshmukh VK, Shrotri DS, Aiman R. Isolation of a hypoglycemic principle from the bark of Ficus bengalensis. Indian J Physiol Pharmacol. 1960;4:182–5. [PubMed] [Google Scholar]
- 7.Shukla R, Gupta S, Gambhir JK, Prabhu KM, Murthy PS. Antioxidant effect of aqueous extract of the bark of Ficus bengalensis in hypercholesterolaemic rabbits. J Ethnopharmacol. 2004;92:47–51. doi: 10.1016/j.jep.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 8.Taur DJ, Nirmal SA, Patil RY, Kharya MD. Antistress and antiallergic effects of Ficus bengalensis bark in asthma. Nat Prod Res. 2007;21:1266–70. doi: 10.1080/14786410701757330. [DOI] [PubMed] [Google Scholar]
- 9.Aswar M, Aswar U, Watkar B, Vyas M, Wagh A, Gujar KN. Anthelmintic activity of Ficus benghalensis. Int J Green Pharma. 2008;2:170–2. [Google Scholar]
- 10.Augusti KT. Hypoglycemic action of bengalenoside: A glucoside isolated from Ficus benghalensis Linn.in normal and alloxan diabetic rabbits. Indian J Physiol Pharmacol. 1975;19:218–20. [PubMed] [Google Scholar]
- 11.2002. [updated on 2002 Feb 8]. Available from: http://www.oecd-ilibrary.org. OECD, Test No. 423: Acute Oral toxicity - Acute Toxic Class Method, OECD Guidelines for the Testing of Chemicals, Section 4: Health Effects, OECD Publishing http://www.oecd-ilibrary.org/environment/oecd-guidelines-for-thetesting-of-chemicals-section-4-health-effects_20745788;jsessionid=473a34p6eq17.delta .
- 12.Morton JJP, Malone MH. Evaluation of vulnerary activity by an open wound procedure in rats. Arch Int Pharmacodyn. 1972;196:117–26. [PubMed] [Google Scholar]
- 13.Diwan PV, Tilloo LD, Kulkarni DR. Influence of Tridax procumbens on wound healing. Indian J Med Res. 1982;75:460–4. [PubMed] [Google Scholar]
- 14.The Indian Pharmacopoeia. 2nd ed. Delhi: Ministry of health, Government of India; 1966. [Google Scholar]
- 15.Ehrlich HP, Hunt TK. Effect of cortisone and vitamin A on wound healing. Ann Surg. 1968;167:324–8. doi: 10.1097/00000658-196803000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee KH. Studies on mechanism of action of salicylates II Retardation of wound healing by aspirin. J Pharm Sci. 1968;57:1042–3. doi: 10.1002/jps.2600570633. [DOI] [PubMed] [Google Scholar]
- 17.Kulkarni SK. 2nd ed. New Delhi: Vallabh Prakashan; 1993. Handbook of Experimental Pharmacology. [Google Scholar]
- 18.Chithra P, Sajithlal GB, Chandrakasan G. Influence of Aloe vera on the glycosaminoglycans in the matrix of healing dermal wounds in rats. J Ethnopharmacol. 1998;59:179–86. doi: 10.1016/s0378-8741(97)00112-8. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal PK, Singh A, Gaurav K, Goel S, Khanna HD, Goel RK. Evaluation of wound healing activity of extracts of plantain banana (Musa sapientum var.paradisiaca) in rats. Indian J Exp Biol. 2009;47:32–40. [PubMed] [Google Scholar]


