Abstract
Objective
Although bowel length is an important prognostic variable used in the management of children with short bowel syndrome (SBS), reliable measurements can be difficult to obtain. Plasma citrulline (CIT) levels have been proposed as surrogate markers for bowel length and function. We sought to evaluate the relationship between CIT and parenteral nutrition (PN) independence in children with SBS.
Study Design
A retrospective chart review performed for all patients seen in a multidisciplinary pediatric intestinal rehabilitation clinic with a recorded CIT between January 2005 and December 2007 (n = 27).
Results
Median age at time of CIT determination was 2.4 years. Diagnoses included necrotizing enterocolitis (26%), intestinal atresias (19%), and gastroschisis (22%). Citrulline levels correlated well with bowel length (R = 0.73; P < .0001) and was a strong predictor of PN independence (P Wilcoxon = 0.002; area under the receiver operating characteristic curve = 0.88; 95% confidence interval, 0.75–1.00). The optimal CIT cutoff point distinguishing patients who reached PN independence was 15 μmol/L (sensitivity = 89%; specificity = 78%).
Conclusion
Plasma CIT levels are strong predictors of PN independence in children with SBS and correlate well with a patient’s recorded bowel length. A cutoff CIT level of 15 μmol/L may serve as a prognostic measure in counseling patients regarding the likelihood of future PN independence.
Keywords: Citrulline, Parenteral nutritional, Enteral tolerance, Short bowel syndrome
Long-term dependence on parenteral nutrition (PN) is a potentially life-threatening consequence of short bowel syndrome (SBS) in children. The ability to reliably predict a child’s potential to successfully wean from PN based upon a unique biomarker would be of significant benefit to the clinician. Ideally, such a biomarker would distinguish patients with likely long-term PN requirements, offer an assessment of intestinal rehabilitation potential, and help with the early identification of children who may ultimately benefit from intestinal transplantation. Furthermore, this marker would be easily measured, allowing it to be followed on a serial basis. Preliminary investigation into the plasma level of citrulline suggests that it could serve as such a biomarker.
Citrulline is a free amino acid found in human plasma. Almost all of the circulating citrulline in plasma is produced by the metabolism of glutamine and proline in small bowel enterocytes [1]. In adults, the level of circulating plasma citrulline has been correlated with small bowel enterocyte mass and small bowel absorptive capacity [2,3], and this correlation appears to be independent of intestinal inflammation [4]. Fewer data exist regarding the significance of plasma citrulline levels in the pediatric population with SBS [5].
Cholestasis in patients receiving PN can develop fairly rapidly, presenting within the first month of exposure [6]. The time course of enteral advancement can therefore be critical. We sought to investigate the relationship between plasma citrulline levels and enteral tolerance by retrospectively reviewing our data on children with SBS and a history of PN dependence. Our aim was to confirm existing reports on the correlation between plasma citrulline levels, small bowel length, and PN independence, as well as to further define the role of citrulline as a possible biomarker of the rate of a patient’s progression to full enteral tolerance.
1. Methods
1.1. Study population
Medical records were reviewed for all children cared for by the Center for Advanced Intestinal Rehabilitation Clinic, Children’s Hospital Boston (Mass), in whom serum citrulline levels were obtained between January 2005 and March 2008. Patients seen by the Center for Advanced Intestinal Rehabilitation Clinic encompass children managed at a tertiary care center for intestinal failure because of SBS. These children have been exposed in the past or are currently being treated with PN. Patients who were purposefully kept on full PN at the time of citrulline testing (eg, patients with a diagnosis of duodenal atresia) were excluded from the study.
1.2. Data collection
Data collected included baseline demographic information as well as clinical and nutritional variables. Baseline demographics included gestational age and sex. Clinical variables included the patient’s primary diagnosis, date and type of operation, and recorded pre and postoperative small bowel length. If the reviewed operative note only specified the amount of bowel resected, the approximate pre and postsurgical bowel lengths were calculated using previously published age-based estimates of small intestinal length [7,8].
Finally, nutritional variables included the type of enteral feed, the route of its administration, and the rate of enteral advancement. The rate of enteral advancement was calculated by recording 4 separate data points (the dates at which the patient reached 25%, 50%, 75%, and 100% enteral intake). A patient was identified as having successfully reached full enteral feeding if he or she maintained 100% enteral energy intake for longer than 2 months.
1.3. Analysis methods
Descriptions of demographic, clinical, and nutritional baseline characteristics were based on means (and SDs), or medians (and interquartile ranges) when variables were skewed, and proportions for categorical variables. For subjects who had several citrulline levels, we studied the reliability of these measurements using an intraclass correlation coefficient.
To assess whether bowel length affected citrulline levels, we estimated Pearson correlation coefficients and fitted linear regression models, with P values obtained via F tests. Only the citrulline level closest to a bowel length measurement was analyzed when patients had more than one citrulline level referred to the same bowel length measurement. Because a few patients had 2 citrulline levels linked to different bowel length measurements, we compared results of linear regression models assuming independence across all records with results of a linear regression model using the generalized estimating equation to account for the repeated measures (assuming an identity working correlation). Results of the simple linear regression and multivariate linear regression with generalized estimating equation were comparable; thus, we reported results of the linear regression model. The association between citrulline levels and the closest percentage of enteral intake was also studied through Pearson correlation and linear regression models. For these analyses, we also selected the citrulline level tested closest to the recorded percentage of enteral calories.
To study the prognostic value of citrulline to identify subjects who attained PN independence during the follow-up period (vs subjects who continued receiving PN), we first estimated the association between these 2 variables via odds ratios in a logistic model with P values obtained through likelihood ratio tests. Considering that our focus was on determining the clinical relevance of using citrulline testing, we a priori chose to include in this analysis only the first available citrulline level for each patient. Furthermore, we estimated the area under the receiver operating characteristic (ROC) curve of citrulline nonparametrically. The area under the ROC curve is a function of the ability of a predictor to discriminate subjects with and without the outcome of interest because it is a function of the sensitivity and false-positive fractions of a test. It varies from 0.5 (for the poorest predictors) to 1 (for perfect predictors). An optimal cutoff point for the test was identified based on the point at which the sensitivity and specificity were simultaneously maximized (or the point that minimized the square root of [{1 − sensitivity}2 + {1 − specificity}2]).
All P values were 2-tailed and 95% confidence intervals were 2-sided. Statistical analyses were performed using SAS version 9 (SAS Institute, Cary, NC) and S-Plus 8 for Windows (Insightful, Seattle, Wash).
2. Results
A total of 27 patients seen in our clinic had citrulline levels drawn between January 2005 and December 2007. Four patients had citrulline levels drawn and bowel lengths recorded but had no corresponding enteral advancement information, leaving 23 patients eligible for our analysis of citrulline levels and enteral tolerance.
The median patient age was 2.4 years (interquartile range, 0.6, 6.7) at the time of citrulline testing. The most common diagnosis was necrotizing enterocolitis (26%) followed by intestinal atresia (19%) and gastroschisis (22%). A review of the operative notes used to obtain bowel lengths revealed that most patients underwent either an exploratory laparotomy with bowel resection or a serial transverse enteroplasty procedure (Table 1).
Table 1.
Patient characteristics (n = 27)
| Patient characteristics | |
|---|---|
| Age at the first recorded citrulline (y), median (IQR) | 2.4 (0.6, 6.7) |
| Gestational age (wk), mean ± SD | 33 ± 3.6 |
| Male, n (%) | 18 (66) |
| Diagnosis, n (%) | |
| Necrotizing enterocolitis | 7 (26) |
| Intestinal atresia | 5 (19) |
| Gastroschisis | 6 (22) |
| Volvulus | 4 (15) |
| Malrotation | 2 (7) |
| Other | 3 (11) |
| Original surgery, n (%) | |
| Exploratory laparotomy and bowel resection | 13 (48) |
| Serial transverse enteroplasty (STEP) | 9 (33) |
| Longitudinal instestinal lengthening (Bianchi) | 2 (7) |
| Other | 3 (11) |
| Bowel length recorded at surgery (cm), median (IQR) a | 61 (36, 131) |
| Bowel length (cm; recorded at surgery or imputed b), median (IQR) | 101 (40, 231) |
IQR indicates interquartile range.
A total of 21 subjects had bowel length recorded at surgery.
Imputed bowel length calculated from reported age-related norms.
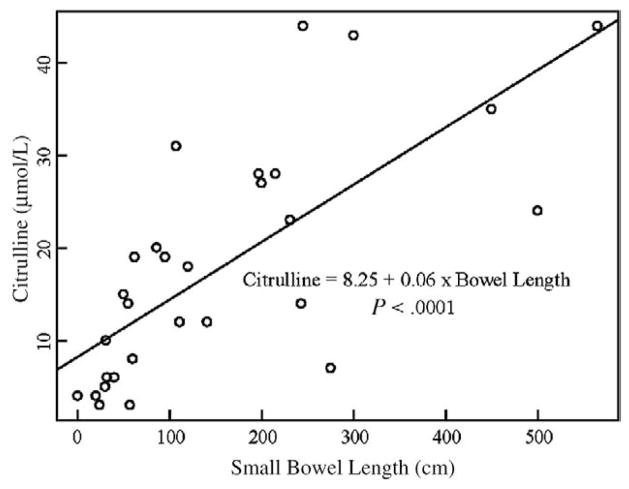
Citrulline levels ranged from 2.0 to 50 μmol/L (mean, 17; SD, 13). For those 11 subjects who had multiple citrulline levels drawn (maximum of 4), citrulline proved to be a reliable test (intraclass correlation coefficient = 0.87). Citrulline levels correlated well with bowel length (Pearson correlation coefficient = 0.73; P < .0001; Fig. 1). This correlation coefficient remained unchanged when the analysis was performed after excluding 6 patients for whom bowel lengths were imputed from historical norms.
Fig. 1.
Association between bowel length and plasma citrulline level. Scatterplot with the fitted regression line (solid line), equation with estimated coefficients, and P value of F test for the coefficient of bowel length (n = 27 patients with 30 citrulline levels).
2.1. Citrulline and percentage of enteral intake
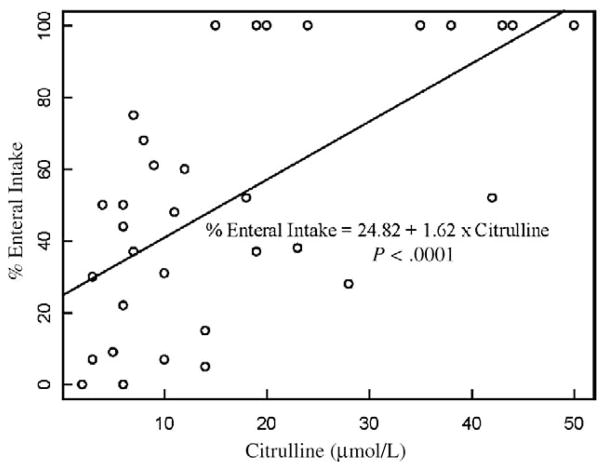
The median elapsed time between the recorded plasma citrulline level and the closest recorded percentage of enteral intake was 2 days (interquartile range, 0, 22 days). Citrulline was associated with percentage of enteral intake (Pearson r = 0.63; P < .0001; Fig. 2) with a 1.6% increase in percentage of enteral tolerance for each 1-μmol/L increment of plasma citrulline (P < .0001).
Fig. 2.
Association between plasma citrulline levels and recorded percentage of enteral intake (% enteral intake). Scatterplot with the fitted regression line (solid line), equation with estimated coefficients, and P value of F test for the coefficient of citrulline level (n = 23 patients with 33 citrulline levels).
2.2. Citrulline and progression to PN independence
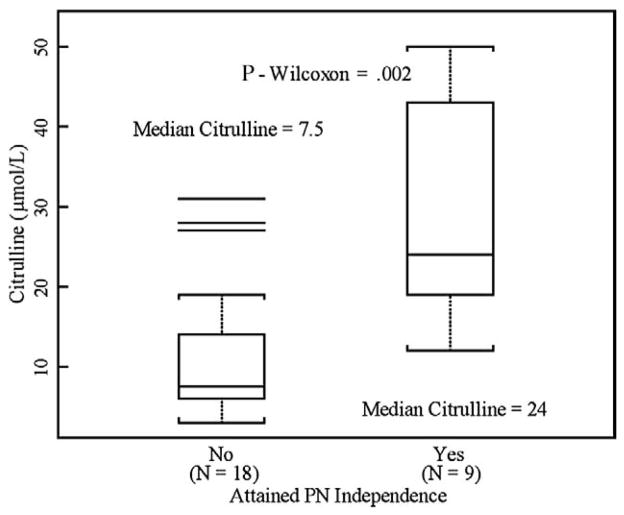
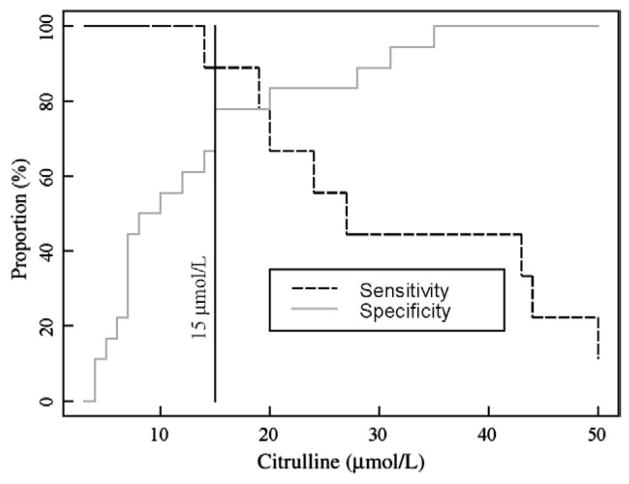
Seven patients had only one data entry point for enteral intake and were thus excluded from the analysis of the rate of enteral advancement. Citrulline levels were significantly associated with attainment of PN independence (odds ratio, 1.9/5 μmol/L citrulline; 95% confidence interval [CI], 1.2–3.1; P = .01; Fig. 3). The area under the ROC curve was close to 1 (0.88; 95% CI, 0.75–1.00), suggesting that citrulline was a good prognostic factor. The citrulline level that maximized the test’s sensitivity and specificity for future PN independence was 15 μmol/L, with a sensitivity of 89% and a specificity of 78% (Fig. 4). At a plasma citrulline concentration of 12 μmol/L or less no patient weaned completely from PN.
Fig. 3.
Distribution of plasma citrulline levels comparing patients who attained PN independence to those who did not. The solid bar within the box represents the median value; upper boundary, 75th percentile; lower boundary, 25th percentile; whiskers extend to the most extreme observation within 1.5 interquartile range units of the 25th and 75th percentiles.
Fig. 4.
Sensitivity and specificity curves of citrulline testing to predict attainment of parenteral nutrition independence as a function of test levels. The vertical line was drawn at the point in which sensitivity and specificity are optimal (ie, 15 μmol/L that corresponds to the citrulline level that minimizes the square root of [{1 − sensitivity}2 + {1 − specificity}2]).
In addition, the plasma citrulline concentration cutoff point of 15 μmol/L could also be used to better predict the rate at which patients reached PN independence. The rate of enteral advancement for patients with a citrulline level greater than 15 μmol/L was 2.4% per day as compared to the rate of 0.1% per day seen in patients with citrulline levels below this cutoff. Thus, patients with a citrulline level more than 15 μmol/L progressed in their enteral intake at a rate of 2.3% per day faster than patients with a citrulline level of 15 μmol/L or less (95% CI, −0.2% to 4.9% per day; P = .09).
3. Discussion
The use of plasma citrulline levels as a biomarker for future enteral tolerance in children with SBS is potentially of significant clinical use. It is easy to obtain and reflects viable small bowel surface area. Its importance may be particularly accentuated if accurate cotemporal operative measurements of bowel length are unavailable.
Although small bowel length is a predictive indicator of enteral tolerance [9,10], the precise determination of intestinal length is at times difficult. This is often the case if the bowel is inflamed (ie, necrotizing enterocolitis) or extensively adhesed (ie, gastroschisis). Furthermore, the pediatric population is noteworthy in its ability for some longitudinal bowel growth and rapid bowel adaptation. Increased surface area from adaptation would not be reflected in the static measure of length obtained during a single operation. Together, the technical difficulty of precise measurements and the potential for changing intestinal surface areas, inherent in small bowel adaptation, potentially limit the use of length as a completely reliable biomarker.
In this study, we sought to investigate the relationship between plasma citrulline levels and enteral tolerance in children with SBS and a history of PN dependence. The correlation we observed between documented small bowel length and plasma citrulline levels was consistent with past reports [5]. The difficulty in obtaining reliable bowel measurements was underscored in this study, as several operative notes failed to mention the total pre and postsmall bowel length.
When bowel length was available, plasma citrulline concentrations did correlate with this measure (Pearson correlation coefficient = 0.73; P < .0001). Perhaps, more important, plasma citrulline concentrations significantly correlated with the physiologic variable of enteral tolerance (Pearson r = 0.63; P < .0001).
Citrulline determinations also correlated well with eventual PN independence (area under the ROC = 0.88; 95% CI, 0.75–1.00). The identified cutoff of 15 μmol/L proved to be the point at which this distinction could be made with the most sensitivity (89%) and specificity (78%). Alternatively, a plasma citrulline threshold of 12 μmol/L provided a sensitivity of 100%, eliminating all false-negative results (ie, none of the patients with a plasma citrulline level of ≤12 μmol/L were successfully weaned from PN). Hence, the use of these cutoffs could aid the clinician in identifying patients with a low likelihood of reaching PN independence and warranting consideration for small bowel transplantation.
Finally, we investigated the correlation between citrulline levels and the rate of enteral advancement. At our institution, the question of how quickly to advance a given child’s feeds is often determined by an empiric strategy. Our data demonstrate that the cutoff point of 15 μmol/L could also be used to distinguish those patients who had a greater tendency to tolerate a more rapid rate of enteral advancement. In our study population, children with a plasma citrulline level less than 15 μmol/L advanced at a rate of approximately 0.1% per day, whereas those with a level more than 15 μmol/L advanced at the more rapid rate of 2.4% per day. Although a clear trend appeared to be evident, it did not attain statistical significance (P = .09).
4. Conclusion
Plasma citrulline concentrations offer clinicians a valuable biomarker for the likelihood of intestinal rehabilitation in children with SBS and PN dependence. Citrulline levels correlate well with enteral feeding tolerance, future PN independence, and tend to correlate with the rate at which enteral feeds can be successfully advanced. Larger scale prospective evaluations of the use of plasma citrulline concentrations are certainly warranted.
Footnotes
Presented at the 40th Annual CAPS Meeting, August 21–24, 2008, Toronto, Ontario, Canada.
References
- 1.Rabier D, Kamoun P. Metabolism of citrulline in man. Amino Acids. 1995;9:299–316. doi: 10.1007/BF00807268. [DOI] [PubMed] [Google Scholar]
- 2.Crenn P, Coudray-Lucas C, Thuillier F, et al. Postabsorptive plasma citrulline concentration is a marker of absorptive enterocyte mass and intestinal failure in humans. Gastroenterology. 2000;119:1496–505. doi: 10.1053/gast.2000.20227. [DOI] [PubMed] [Google Scholar]
- 3.Jianfeng G, Weiming Z, Ning L, et al. Serum citrulline is a simple quantitative marker for small intestinal enterocytes mass and absorption function in short bowel patients. J Surg Res. 2005;127:177–82. doi: 10.1016/j.jss.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Papadia C, Sherwood R, Kalantzis C, et al. Plasma citrulline concentration: a reliable marker of small bowel absorptive capacity independent of intestinal inflammation. Am J Gastroenterol. 2007;102:1474–82. doi: 10.1111/j.1572-0241.2007.01239.x. [DOI] [PubMed] [Google Scholar]
- 5.Rhoads J, Plunkett E, Galanko J, et al. Serum citrulline levels correlate with enteral tolerance and bowel length in infants with short bowel syndrome. J Pediatr. 2005;146:542–7. doi: 10.1016/j.jpeds.2004.12.027. [DOI] [PubMed] [Google Scholar]
- 6.Beath S, Davies A, Papadopoulou A, et al. Parenteral nutrition-related cholestasis in postsurgical neonates: multivariate analysis of risk factors. J Pediatr Surg. 1996;31(4):604–6. doi: 10.1016/s0022-3468(96)90507-2. [DOI] [PubMed] [Google Scholar]
- 7.Siebert JR. Small-intestine length in infants and children. Am J Dis Child. 1990;134:593–5. doi: 10.1001/archpedi.1980.02130180051015. [DOI] [PubMed] [Google Scholar]
- 8.Touloukian RJ, Walker Smith GJ. Normal intestinal length in preterm infants. J Pediatr Surg. 1983;18(6):720–3. doi: 10.1016/s0022-3468(83)80011-6. [DOI] [PubMed] [Google Scholar]
- 9.Kaufman S, Loseke C, Lupo J, et al. Influence of bacterial overgrowth and intestinal inflammation on duration of parenteral nutrition in children with short bowel syndrome. J Pediatr. 1997;131:356–61. doi: 10.1016/s0022-3476(97)80058-3. [DOI] [PubMed] [Google Scholar]
- 10.Sondheimer J, Cadnapaphornchai M, Sontag M, et al. Predicting the duration of dependence on parenteral nutrition after neonatal intestinal resection. J Pediatr. 1998;132:80–4. doi: 10.1016/s0022-3476(98)70489-5. [DOI] [PubMed] [Google Scholar]