Abstract
Purpose
Serial transverse enteroplasty (STEP) is a novel technique to lengthen and taper bowel in patients with intestinal failure. First described in 2003, initial data and reports have demonstrated favorable short-term outcomes, but there is limited published data on long-term outcomes of the procedure. Our aim was to assess clinical and nutritional outcomes after the STEP procedure.
Methods
After obtaining institutional review board approval, we reviewed all records of patients (n = 16) who underwent the STEP procedure at our institution from February 2002 to February 2008. Patients were observed for a median time of 23 months (range, 1–71) postoperatively. Analyses of z scores for weight, height, and weight-for-height, and progression of enteral calories were performed using longitudinal linear models with random effects.
Results
Of the 16 patients (10 male), the median age at time of surgery was 12 months (interquartile range, 1.5–65.0). The mean increase in bowel length was 91% ± 38%. After the STEP procedure, patients had increased weight-for-age z scores of 0.03 units per month (P = .0001), height for age z scores of 0.02 units per month (P = .004), and weight-for-height z scores of 0.04 units per month (P = .02). Patients had improved enteral tolerance of 1.4% per month (P < .0001). Six patients (38%) transitioned off parenteral nutrition (median, 248 days). Long-term complications included catheter-related bacteremia (n = 5), gastrointestinal bleeding (n = 3), and small bowel obstruction (n = 1). Two patients ultimately underwent transplantation. There were no deaths.
Conclusions
In pediatric patients with intestinal failure, the STEP procedure improves enteral tolerance, results in significant catch-up growth, and is not associated with increased mortality.
Keywords: Short bowel syndrome, Intestinal failure, Serial transverse enteroplasty (STEP), Autologous intestinal reconstruction surgery (AIRS)
First described in 2003 [1], the serial transverse enteroplasty (STEP) is a method of autologous intestinal reconstruction surgery (AIRS) designed to both lengthen and taper the bowel in patients with intestinal failure. Serial transverse enteroplasty is a surgical alternative to other AIRS methods, including the longitudinal intestinal lengthening and tapering procedure described by Bianchi [2]. Compared to the longitudinal intestinal lengthening and tapering procedure, the advantages of the STEP include the technical ease and simplicity of the procedure, the ability to use it in cases of nonuniform bowel dilation, and the ability to repeat the procedure should redilation occur [3–5]. Commonly reported indications for the STEP procedure have included short bowel syndrome, failure to advance enteral feeds, neonatal intestinal atresias [6], and severe bacterial overgrowth [7].
Because the first STEP procedure was performed in 2002, there have yet to be reports on its long-term efficacy and outcomes. There have been several reports on short-term outcomes after the STEP procedure [9–12]. These reports demonstrate the safety and efficacy of the procedure in increasing bowel length, tapering dilated bowel, and facilitating weaning patients off parenteral nutrition (PN). However, none of these reports, including the first report from the International STEP Data Registry [10], contains detailed nutritional data, and this type of data is difficult to collect in a large data registry. We present the first detailed long-term nutritional analysis in patients after the STEP procedure at our institution.
1. Methods
After obtaining institutional review board approval, we reviewed the charts and medical records of all patients who underwent the STEP procedure at our institution from February 2002 to February 2008. The mean follow-up period was 23 months (range, 1–71 months). We estimated mean postoperative trajectories of the 16 patients’ z scores for weight, height, and weight-for-height, as well as their percentage of enteral calories. These trajectories were measured as a function of time using a linear mixed model with a random intercept.
We compared the model-based estimate with mean over all available measures obtained in specified intervals before starting the analysis. One patient, who underwent the STEP for bacterial overgrowth, and who was receiving full enteral nutrition at the time of surgery, was excluded from our enteral tolerance analysis. Results were considered statistically significant when the P value was < .05. All analyses were performed in S-plus 8 (Insightful, Seattle, WA).
2. Results
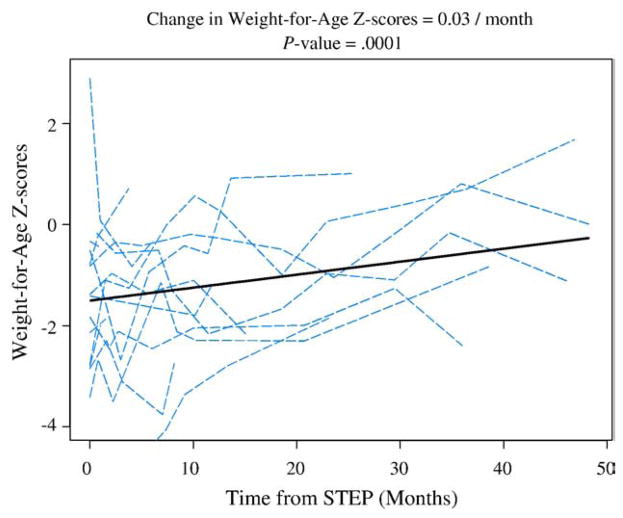
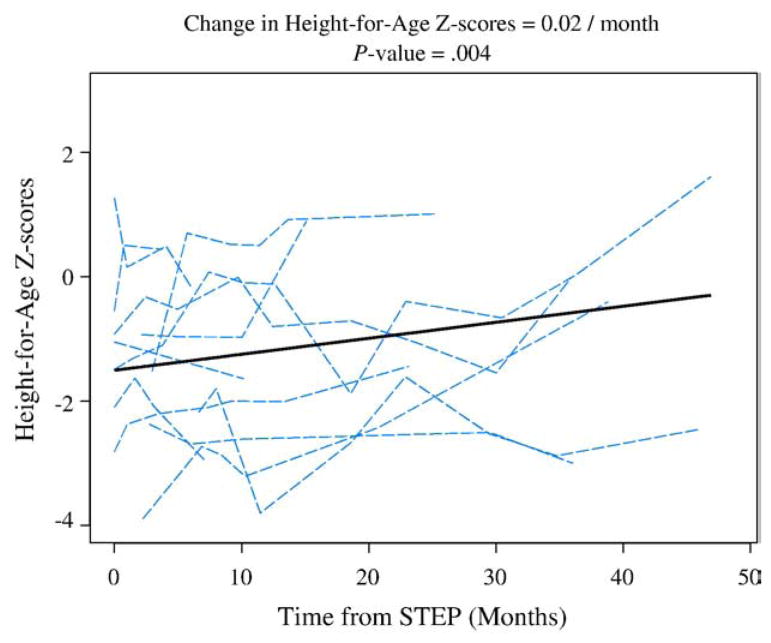
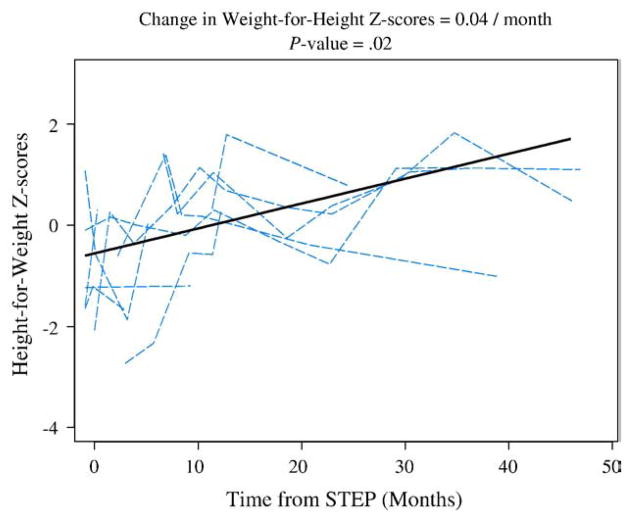
Of the 16 patients (10 male), the median age at time of surgery was 12 months (interquartile range, 1.5–65.0). The most common indication for the STEP procedure was failure to advance on enteral feeds (Table 1). Other indications included complications arising from bacterial overgrowth and the desire to lengthen and taper selected neonatal intestinal atresias with marginal residual intestine length. As seen in Table 2, there was a mean increase in bowel length of 91% (SD, 38%) and a mean decrease in bowel width of 70% (SD, 6%). Weight-for-age z scores improved 0.36 units per year (P = .0001) as seen in Fig. 1. Fig. 2 illustrates the height-for-age z scores of patients after the STEP procedure. There was an increase of 0.24 units per year (P = .004). The weight-for-height for age z scores, in Fig. 3, demonstrated an increase of 0.48 units per year (P = .02).
Table 1.
Patient demographics (n = 16)
| n (%) | |
|---|---|
| Male | 10 (63%) |
| Mean age at time of STEP, median (IQR) | 12 (1.5–65) |
| Primary diagnosis | |
| Gastroschisis | 6 (38%) |
| Intestinal atresia | 4 (25%) |
| Midgut volvulus | 3 (19%) |
| Necrotizing enterocolitis | 2 (13%) |
| Hirschprung’s disease | 1 (6%) |
| Indication for STEP | |
| Failure to advance enteral feedings | 11 (69%) |
| Bacterial overgrowth | 3 (19%) |
| Neonatal atresia | 2 (13%) |
IQR indicates interquartile range.
Table 2.
Operative results (n = 16)
| Pre-STEP | Post-STEP | % change mean ± SD | |
|---|---|---|---|
| Small bowel length (cm), median (IQR) | 60 (30, 108) | 117 (62, 209) | 91 ± 38 |
| Small bowel width (cm), median (IQR) | 6.5 (4.5, 8.0) | 2.0 (1.0, 2.6) | −70 ± 6 |
IQR indicates interquartile range.
Fig. 1.
Dashed lines represent individual trajectories, and the solid line represents mean trajectory as estimated in a linear mixed effects model.
Fig. 2.
Dashed lines represent individual trajectories, and the solid line represents mean trajectory as estimated in a linear mixed effects model.
Fig. 3.
Dashed lines represent individual trajectories, and the solid line represents mean trajectory as estimated in a linear mixed effects model.
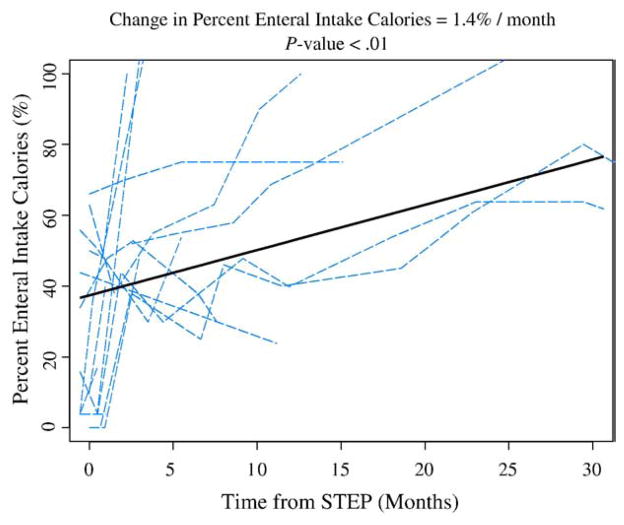
Patients also had improved enteral tolerance of 1.4% per month (P < .0001). Fig. 4 shows the trend of improvement in enteral tolerance up to 48 months postoperatively. Six patients (38%) were transitioned off PN, with a median time of 248 days. These 6 patients have remained off PN. Long-term outcomes (Table 3) included catheter-related bacteremias (n = 5), gastrointestinal bleeding (n = 3), and small bowel obstruction (n = 1). Two patients ultimately underwent transplantation (1 multivisceral, 1 liver small bowel) for complications of progressive liver disease. There were no deaths.
Fig. 4.
Dashed lines represent individual trajectories, and the solid line represents mean trajectory as estimated in a linear mixed effects model.
Table 3.
| Clinical Outcomes (n = 16) | n (%) |
|---|---|
| Transitioned off PN | 6 (38%) |
| Catheter-related bacteremia | 5 (31%) |
| Redilation | 5 (31%) |
| Gastrointestinal bleeding | 2 (13%) |
| Transplant | 2 (13%) |
| Small bowel obstruction | 1 (7%) |
| Death | 0 (0%) |
3. Discussion
The STEP procedure has become an increasingly used technique in the surgical management of intestinal failure since its first description 5 years ago. This is in large part because of the technical ease and the broader applicability of the procedure compared to other methods of AIRS. There are already several reports from various centers demonstrating excellent short and intermediate-term results, including efficacy in lengthening and tapering intestine, improving enteral tolerance, and improving overall nutritional status [8–12]. There are, however, limited reports, on long-term nutritional outcomes after AIRS in general [13–15], and only short-term reports exist after the STEP procedure [9,11]. This current report demonstrates that patients can sustain improved enteral tolerance and significant catch-up growth at 4 years from time of the STEP procedure. z Scores for weight (Fig. 1), height (Fig. 2), and weight-for-height (Fig. 3), all had significant annual increases of 0.36, 0.24, and 0.48 units, respectively. This improved growth is in the setting of a decreased need for PN.
Overall, enteral tolerance improved 1.4% per month (Fig. 1). Six of our patients transitioned off PN. One patient, who had the STEP for bacterial overgrowth, did not require PN before the surgery, and she remained on full enteral feeds postoperatively, with resolution of bacterial overgrowth. All 6 patients who weaned completely from PN have remained off PN.
These results are the longest follow-up to date on patients undergoing the STEP procedure. Although our Center for Advanced Intestinal Rehabilitation receives referrals and manages patients who have undergone the STEP at other institutions, this study was limited to those patients who underwent the procedure at our own institution. Our patients are evaluated and managed by a single multidisciplinary team involving surgeons, gastroenterologists, nurses, nurse practitioners, nutritionists, pharmacists, and social workers [16].
The most common indication for surgery in our cohort was the failure to advance on enteral nutrition. Before the decision is made to undergo the STEP procedure, patients are maximized with medical and nutritional therapy, including motility agents, changes in enteral formulas, and jejunal feedings. If these maneuvers fail to improve enteral tolerance, and an upper gastrointestinal series demonstrates sufficiently dilated bowel, the STEP procedure is given strong consideration. We did not deem patients with a pathologic diagnosis of cirrhosis, clinical signs of portal hypertension, or coagulopathy as strong candidates for the STEP procedure. In these cases, medical therapy was maximized in conjunction with evaluation for transplantation.
The STEP procedure can significantly increase bowel length. In our patients, the mean increase was 91%, which is consistent with other reported mean increases of 52% to 94% [10–12]. Although the increase of bowel length may facilitate intestinal rehabilitation, tapering of dilated bowel may also be of benefit. Three patients had the STEP procedure for complications of bacterial overgrowth. In these instances, the technique was used more for its tapering effect with preservation of existing mucosal surface area.
Long-term outcomes have included recurrent catheter-related bacteremias, gastrointestinal bleeding, and one case of small bowel obstruction requiring surgery. Catheter-related bacteremias continue to be associated with significant morbidity in patients with short bowel syndrome, affecting 5 (31%) of our patients. Our 3 patients with gastrointestinal bleeding were managed conservatively and did not require surgery. The patient with the small bowel obstruction presented a year after the STEP procedure and required surgical intervention. Interestingly, her obstruction was caused by a stricture in a prior Bianchi segment (performed at another institution), and none of her STEP bowel was involved.
Two patients (13%) ultimately underwent transplantation (1 liver small bowel, 1 multivisceral) at 1 month and 12 months post-STEP. There were no deaths among our patients, and this compares favorably to other reported mortality rates of 8% to 21% [11,12] after AIRS.
Nine of our patients have had long-term follow-up (ie, >6 months) with upper gastrointestinal series. Of these 9 patients, 5 were noted to have redilation of their intestine. It is not clear if this occurrence is part of the intestinal rehabilitation process or reflects the natural history of the underlying disease process. Despite the evidence of redilation in our patients, only one has undergone a repeat STEP at our center. For this patient, however, the initial STEP procedure was performed at a different institution.
4. Conclusions
Because the STEP procedure is a novel technique, there are limited reports of its long-term nutritional and clinical outcomes. To date, the longest reported follow-up of patients after STEP is less than 2 years [10–12]. In long-term follow-up of our patients of up to 5 years, we have had a relatively low rate of complications, including no deaths. We believe that with proper patient selection and ongoing intensive intestinal rehabilitation management, patients undergoing the STEP procedure can have improved enteral tolerance, decreased PN dependence, and can sustain significant catch-up growth, as measured by z scores for weight, height, and weight-for-length. Of our patients, 38% have achieved complete enteral autonomy, and none have required reinstitution of PN. Continued close follow-up of these patients will be required to ensure adequate ongoing nutrition and growth as well as to detect and assess the clinical significance of recurrent bowel dilation.
Footnotes
Presented at the 40th Annual CAPS Meeting, August 21–24, 2008, Toronto, Ontario, Canada.
References
- 1.Kim HB, Fauza D, Garza J, et al. Serial transverse enteroplasty (STEP): a novel bowel lengthening procedure. J Pediatr Surg. 2003;38:425–9. doi: 10.1053/jpsu.2003.50073. [DOI] [PubMed] [Google Scholar]
- 2.Bianchi A. Intestinal loop lengthening - A technique for increasing small intestinal length. J Pediatr Surg. 1980;15:145–51. doi: 10.1016/s0022-3468(80)80005-4. [DOI] [PubMed] [Google Scholar]
- 3.Piper H, Modi BP, Kim HB, et al. The second STEP: the feasibility of repeat serial transverse enteroplasty. J Pediatr Surg. 2006;41:1951–6. doi: 10.1016/j.jpedsurg.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 4.Ehrlich PF, Mychaliska GB, Teitelbaum DH. The 2 STEP: an approach to repeating a serial transverse enteroplasty. J Pediatr Surg. 2007;42:819–22. doi: 10.1016/j.jpedsurg.2006.12.056. [DOI] [PubMed] [Google Scholar]
- 5.Andres AM, Thompson J, Grant W, et al. Repeat surgical bowel lengthening with the STEP procedure. Transplantation. 2008;85:1294–9. doi: 10.1097/TP.0b013e31817268ca. [DOI] [PubMed] [Google Scholar]
- 6.Wales PW, Dutta S. Serial transverse enteroplasty as primary therapy for neonates with proximal jejunal atresia. J Pediatr Surg. 2005;40:E31–4. doi: 10.1016/j.jpedsurg.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Modi BP, Langer M, Duggan C, et al. Serial transverse enteroplasty for management of refractory D-lactic acidosis in short-bowel syndrome. J Pediatr Gastroenterol Nutr. 2006;43:395–7. doi: 10.1097/01.mpg.0000228116.52229.7b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Javid PJ, Kim HB, Duggan CP, et al. Serial transverse enteroplasty is associated with successful short-term outcomes in infants with short bowel syndrome. J Pediatr Surg. 2005;40:1019–23. doi: 10.1016/j.jpedsurg.2005.03.020. discussion 23-24. [DOI] [PubMed] [Google Scholar]
- 9.Duggan C, Piper H, Javid PJ, et al. Growth and nutritional status in infants with short-bowel syndrome after the serial transverse enteroplasty procedure. Clin Gastroenterol Hepatol. 2006;4:1237–41. doi: 10.1016/j.cgh.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Modi BP, Javid PJ, Jaksic T, et al. First report of the international serial transverse enteroplasty data registry: indications, efficacy, and complications. J Am Coll Surg. 2007;204:365–71. doi: 10.1016/j.jamcollsurg.2006.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sudan D, Thompson J, Botha J, et al. Comparison of intestinal lengthening procedures for patients with short bowel syndrome. Ann Surg. 2007;246:593–601. doi: 10.1097/SLA.0b013e318155aa0c. [discussion -4] [DOI] [PubMed] [Google Scholar]
- 12.Wales PW, de Silva N, Langer JC, et al. Intermediate outcomes after serial transverse enteroplasty in children with short bowel syndrome. J Pediatr Surg. 2007;42:1804–10. doi: 10.1016/j.jpedsurg.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 13.Walker SR, Nucci A, Yaworski JA, et al. The Bianchi procedure: a 20-year single institution experience. J Pediatr Surg. 2006;41:113–9. doi: 10.1016/j.jpedsurg.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 14.Georgeson K, Halpin D, Figueroa R, et al. Sequential intestinal lengthening procedures for refractory short bowel syndrome. J Pediatr Surg. 1994;29:316–20. doi: 10.1016/0022-3468(94)90339-5. [DOI] [PubMed] [Google Scholar]
- 15.Figueroa-Colon R, Harris PR, Birdsong E, et al. Impact of intestinal lengthening on the nutritional outcome for children with short bowel syndrome. J Pediatr Surg. 1996;31:912–6. doi: 10.1016/s0022-3468(96)90409-1. [DOI] [PubMed] [Google Scholar]
- 16.Modi BP, Langer M, Ching YA, et al. Improved survival in a multidisciplinary short bowel syndrome program. J Pediatr Surg. 2008;43:20–4. doi: 10.1016/j.jpedsurg.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]