INTRODUCTION
Short-bowel syndrome (SBS) is a relatively common disease of insufficient small-bowel absorptive capacity with an estimated 5-year mortality rate of 37.5%, mostly because of sepsis and liver failure associated with central venous access and parenteral nutrition (1,2). Manifestations of SBS include growth retardation, malnutrition, diarrhea and frequent infection. Sources of infection include central venous access and bacterial overgrowth within chronically dilated bowel. One complication of bacterial overgrowth is d-lactic acidosis, a syndrome of neurological disturbances and acidemia first described in 1979 (3). Patients present with recurrent, often escalating episodes of neurological derangement associated with acidosis, widened anion gap and elevated levels of plasma d-lactic acid. d-Lactic acid, the product of anaerobic carbohydrate metabolism by resident intestinal bacteria, is believed to cause acidosis because it is metabolized much more slowly than l-lactic acid and therefore accumulates if produced in abundance. In the case of SBS, decreased absorption of enteral carbohydrates and bacterial overgrowth are thought to lead to increased bacterial production of lactic acid. The responsible bacteria may colonize the remnant small or large intestine as a result of stasis and dysmotility within chronically dilated bowel or administration of probiotic medications such as the gram-positive anaerobic rod Lactobacillus acidophilus (4,5). Traditional treatment of this disease consists of altering the intestinal flora with antibiotics and minimizing the metabolic substrate by using a low-carbohydrate diet (6). Unfortunately, these therapies are not always successful, and refractory cases are a difficult management problem in this chronically ill patient population.
Serial transverse enteroplasty (STEP), which involves sequential linear stapling of the dilated bowel from opposite directions to create a new “zig-zag” lengthened and tapered intestinal channel, has gained acceptance in the treatment of patients with SBS since its introduction in 2003 (7–12). In addition, a recent animal study has shown that the STEP procedure reduces bacterial overgrowth in SBS (13). A potential advantage of the STEP operation compared with conventional tapering is its ability to narrow dilated bowel while preserving small-bowel mucosal mass. Thus, the STEP procedure could be a useful therapy for treatment of SBS patients with refractory d-lactic acidosis.
We describe here the case of a patient with SBS who had been relatively well until she developed recurrent episodes of d-lactic acidosis. After failure of medical management, she was successfully treated with the STEP procedure to provide tapering of a massively dilated segment of duodenum that was felt to be a reservoir for d-lactic acid producing bacterial flora.
CASE REPORT
An 18-year-old woman was referred to our multidisciplinary SBS program for recurrent d-lactic acidosis. The patient was diagnosed with malrotation at age 7 and underwent a Ladd procedure at that time. At age 10 years, she developed intestinal volvulus requiring extensive bowel resection. Two years before referral, she acutely developed gait instability, irritability, fatigue and slurred speech. She was diagnosed with d-lactic acidosis, with a peak d-lactic acid level of 1.08 mmol/L (normal, 0.0–0.25 mmol/L), and successfully treated in the hospital. After discharge, prophylaxis against recurrence consisted of multiple oral antibiotic regimens, including metronidazole, gentamicin, tetracycline, sulfamethoxazole/trimethoprim, neomycin, amoxicillin/clavulanate and nitazoxanide. She was also maintained on low-carbohydrate tube feeding with Nutrivent, minimal oral carbohydrate intake, scheduled GoLytely bowel lavages and a specially formulated probiotic with no d-lactate–producing bacteria. She had been receiving a high-protein high-acetate formulation of parenteral nutrition, amounting to approximately 33% of her energy intake, in an attempt to improve her acid-base balance. Despite these therapies managed by 2 tertiary care pediatric facilities, she continued to have worsening episodes of neurological derangement associated with d-lactic acidosis. At the time of presentation to our institution, she had undergone 6 hospital admissions in the preceding 6 months, including an admission for ataxia resulting in a fall and head trauma that ultimately forced the patient to drop out of her first year of college.
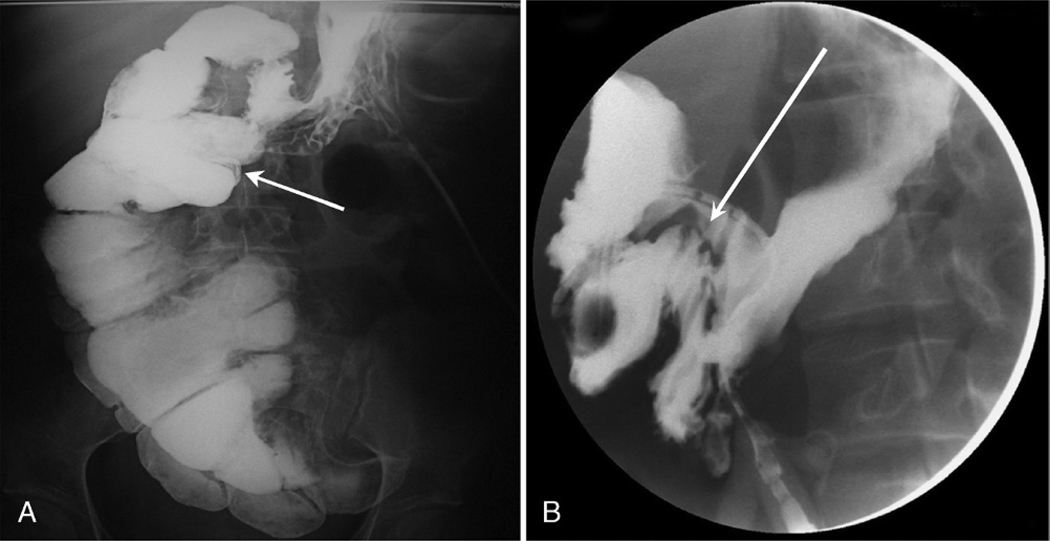
At referral, an upper gastrointestinal radiographic series demonstrated a largely dilated duodenum with a slow small bowel transit time of 5 hours and no evidence of mechanical obstruction (Fig. 1A). Barium enema confirmed the absence of distal mechanical obstruction. Quantitative aerobic cultures of duodenal aspirates from endoscopy at the referring institution grew Escherichia coli, Klebsiella pneumoniae and Proteus mirabilis.
FIG. 1.
Preoperative and postoperative upper gastrointestinal series. A, Preoperative image demonstrating dilated duodenum (arrow). B, Postoperative image demonstrating resolution of duodenal dilation and characteristic “zig-zag” pattern of post-STEP bowel (arrow).
It seemed the dilated bowel, which contained colonic flora, was responsible for bacterial overgrowth of d-lactate–producing bacteria. Given the failure of maximal medical management at 2 other tertiary care facilities, the patient was counseled on the potential use of the STEP procedure to limit the degree of stasis and bacterial overgrowth by tapering the dilated duodenum without removing mucosal mass and surface area. In contrast to the usual indication for STEP of bowel lengthening for SBS, the goal in this case was to taper the dilated duodenum to eliminate the focus of d-lactate–producing bacteria.
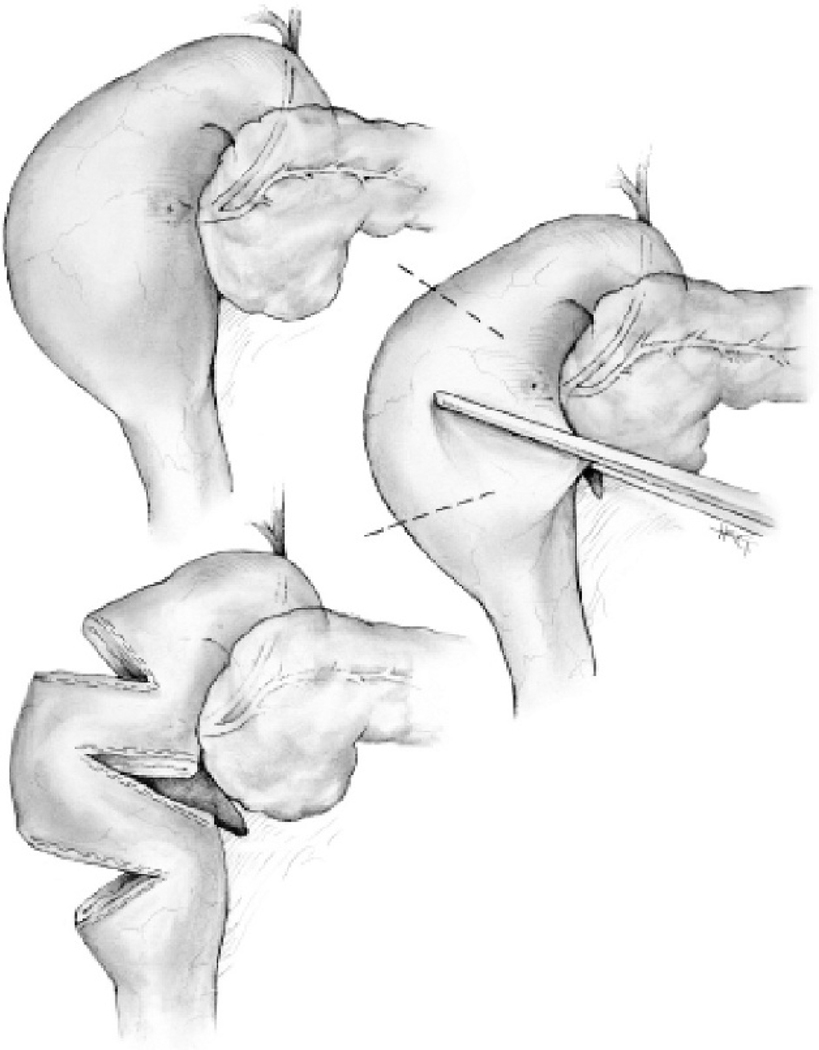
After consent, the patient underwent laparotomy with extensive lysis of adhesions and full mobilization of the intestine. Measurement of the antimesenteric border demonstrated only 32 cm of residual small bowel from pylorus to enterocolic anastomosis. The only dilated portion was the proximal duodenum, measuring 8 cm in diameter. The STEP procedure was performed on this segment using 3 firings of the gastrointestinal anastomosis stapler as previously described (7,12), although the stapler applications were performed from the anterior and posterior aspects (“antimesenteric” and “mesenteric”) of the duodenum to avoid injury to the pancreas and biliary structures (Fig. 2). The patient subsequently did well and was discharged home on postoperative day 11 tolerating a regular diet. An upper gastrointestinal series on postoperative day 7 revealed a normal caliber small bowel with a small-bowel transit time of 2.5 hours, indicating improved motility and less stasis (Fig. 1B).
FIG. 2.
Stepwise artist’s rendition of the method used in this patient for performing the STEP procedure on the duodenum. Note the window created between the pancreas and duodenum for placement of the “mesenteric” staple line and the subsequent tapered and lengthened segment.
After 11 months of follow-up, the patient has required only one admission for d-lactic acidosis, which occurred 8 months postoperatively. This episode was initiated by a course of antibiotics prescribed for pharyngitis. She has subsequently been managed as an outpatient with intermittent courses of metronidazole and medical management. Her quality of life is drastically improved, and she has been able to successfully return to college where she is a “straight-A” student. She has maintained her weight and is currently receiving 75% of her calories enterally.
DISCUSSION
This case highlights many of the management difficulties seen with refractory d-lactic acidosis. The natural history is one of progressive, worsening episodes with increasing frequency unless medical therapy with a low-carbohydrate diet and a scheduled antibiotic regimen are successful (3,5). This sustained decline can have a major impact upon the daily lives of these chronically ill patients, and definitive therapy must be sought.
The successful treatment of this patient with STEP is encouraging. Serial transverse enteroplasty has many advantages over previously existing methods of tapering the dilated short bowel. Compared with the Bianchi (14), and Kimura and Soper (15) techniques, the STEP procedure is technically less difficult, has a decreased risk of intraperitoneal contamination because the bowel is never opened and has a decreased risk of intestinal ischemia because it preserves the natural vascular anatomy of the bowel (7). Compared with standard tapering enteroplasty, the STEP procedure allows tapering without excision of the antimesenteric portion of the bowel, a distinct advantage in patients whose SBS mandates preservation of small-bowel mucosa. Application of the STEP procedure to the duodenum, as in this case, may also be used for lengthening procedures. Specific attention to the anatomy and location of the ampulla of Vater must be practiced by the surgeon in this setting, however, to avoid potentially morbid complications associated with injury to the pancreaticobiliary system.
The STEP procedure has been successful in patients with SBS by tapering and lengthening their dilated short bowel to help wean them from parenteral nutrition. The treatment of bacterial overgrowth and refractory d-lactic acidosis, as in our patient, represents another indication for this procedure. This patient has had an excellent short-term outcome with the ability to reestablish the relatively normal life she was leading before developing refractory d-lactic acidosis. Her long-term outcome and the long-term success of the STEP procedure in treating this disease process remains to be seen.
The mechanisms by which the STEP procedure may function to decrease or even eliminate d-lactic acidosis in SBS patients include decreased bacterial load, decreased stasis and increased absorption. All of these potential mechanisms serve to decrease d-lactic acid production by decreasing the amount of bacteria, the amount of carbohydrate substrate or both. Work by our group on an animal model of SBS has established that the STEP procedure improves intestinal carbohydrate absorptive capacity and suggests that it eliminates bacterial overgrowth (13). Ongoing work will help to better define other potential mechanisms.
This report represents the first successful surgical treatment of d-lactic acidosis refractory to medical therapy and a potential new indication for STEP. d-Lactic acidosis is most often controlled with appropriate medical management. If, as in this case, maximal medical therapy is not able to prevent symptomatic recurrence of disease, surgical intervention using the STEP procedure should be considered as a potential therapy in SBS patients with refractory d-lactic acidosis.
REFERENCES
- 1.Wales PW, de Silva N, Kim J, et al. Neonatal short bowel syndrome: population-based estimates of incidence and mortality rates. J Pediatr Surg. 2004;39:690–695. doi: 10.1016/j.jpedsurg.2004.01.036. [DOI] [PubMed] [Google Scholar]
- 2.Wales PW, de Silva N, Kim JH, et al. Neonatal short bowel syndrome: a cohort study. J Pediatr Surg. 2005;40:755–762. doi: 10.1016/j.jpedsurg.2005.01.037. [DOI] [PubMed] [Google Scholar]
- 3.Oh MS, Phelps KR, Traube M, et al. d-lactic acidosis in a man with the short bowel syndrome. N Engl J Med. 1979;301:249–252. doi: 10.1056/NEJM197908023010505. [DOI] [PubMed] [Google Scholar]
- 4.Bongaerts GP, Tolboom JJ, Naber AH, et al. Role of bacteria in the pathogenesis of short bowel syndrome-associated d-lactic acidemia. Microb Pathog. 1997;22:285–293. doi: 10.1006/mpat.1996.0122. [DOI] [PubMed] [Google Scholar]
- 5.Uribarri J, Oh MS, Carroll HJ. d-lactic acidosis. A review of clinical presentation, biochemical features, and pathophysiologic mechanisms. Medicine (Baltimore) 1998;77:73–82. doi: 10.1097/00005792-199803000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Mayne AJ, Handy DJ, Preece MA, et al. Dietary management of d-lactic acidosis in short bowel syndrome. Arch Dis Child. 1990;65:229–231. doi: 10.1136/adc.65.2.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HB, Fauza D, Garza J, et al. Serial transverse enteroplasty (STEP): a novel bowel lengthening procedure. J Pediatr Surg. 2003;38:425–429. doi: 10.1053/jpsu.2003.50073. [DOI] [PubMed] [Google Scholar]
- 8.Sudan D, DiBaise J, Torres C, et al. A multidisciplinary approach to the treatment of intestinal failure. J Gastrointest Surg. 2005;9:165–177. doi: 10.1016/j.gassur.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Javid PJ, Kim HB, Duggan CP, et al. Serial transverse enteroplasty is associated with successful short-term outcomes in infants with short bowel syndrome. J Pediatr Surg. 2005;40:1019–1024. doi: 10.1016/j.jpedsurg.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 10.Wales PW, Dutta S. Serial transverse enteroplasty as primary therapy for neonates with proximal jejunal atresia. J Pediatr Surg. 2005;40:E31–E34. doi: 10.1016/j.jpedsurg.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Ismail A, Alkadhi A, Alnagaar O, et al. Serial transverse enteroplasty in intestinal atresia management. J Pediatr Surg. 2005;40:E5–E6. doi: 10.1016/j.jpedsurg.2004.10.059. [DOI] [PubMed] [Google Scholar]
- 12.Kim HB, Lee PW, Garza J, et al. Serial transverse enteroplasty for short bowel syndrome: a case report. J Pediatr Surg. 2003;38:881–885. doi: 10.1016/s0022-3468(03)00115-5. [DOI] [PubMed] [Google Scholar]
- 13.Chang RW, Javid PJ, Oh JT, et al. Serial transverse enteroplasty enhances intestinal function in a model of short bowel syndrome. Ann Surg. 2006;243:223–228. doi: 10.1097/01.sla.0000197704.76166.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bianchi A. Intestinal lengthening: an experimental and clinical review. J R Soc Med. 1984;77 suppl 3:35–41. [PMC free article] [PubMed] [Google Scholar]
- 15.Kimura K, Soper RT. A new bowel elongation technique for the short-bowel syndrome using the isolated bowel segment Iowa models. J Pediatr Surg. 1993;28:792–794. doi: 10.1016/0022-3468(93)90328-i. [DOI] [PubMed] [Google Scholar]