Abstract
Cystic dystrophy of the duodenal wall is a rare form of the disease which was described in 1970 by French authors who reported the presence of focal pancreatic disease localized in an area comprising the C-loop of the duodenum and the head of the pancreas. German authors have defined this area as a “groove”. We report our recent experience on cystic dystrophy of the paraduodenal space and systematically review the data in the literature regarding the alterations of this space. A MEDLINE search of papers published between 1966 and 2010 was carried out and 59 papers were considered for the present study; there were 19 cohort studies and 40 case reports. The majority of patients having groove pancreatitis were middle aged. Mean age was significantly higher in patients having groove carcinoma. The diagnosis of cystic dystrophy of the duodenal wall can now be assessed by multidetector computer tomography, magnetic resonance imaging and endoscopic ultrasonography. These latter two techniques may also add more information on the involvement of the remaining pancreatic gland not involved by the duodenal malformation and they may help in differentiating “groove pancreatitis” from “groove adenocarcinoma”. In conclusion, chronic pancreatitis involving the entire pancreatic gland was present in half of the patients with cystic dystrophy of the duodenal wall and, in the majority of them, the pancreatitis had calcifications.
Keywords: Pancreatitis, Cystic dystrophy of duodenal wall, Therapy, Outcome
INTRODUCTION
Cystic dystrophy of the duodenal wall is a rare form of the disease which was described for the first time in 1970 by Potet and Duclert[1]. Potet and Duclert and other French authors[2,3] described the presence of focal pancreatic disease localized in an area comprising the C-loop of the duodenum and the head of the pancreas (Figure 1A). In 1991, Becker and Mischke[4] defined this area as a “groove” and pointed out that it serves as a bed for the large vessels, lymph nodes, common bile duct (CBD) and main pancreatic duct. These authors also reported that pancreatitis can be found in this area and they suggested the term “groove pancreatitis” which was well received. They also classified groove pancreatitis as “pure groove pancreatitis” (Figure 1B), segmental pancreatitis of the head and chronic pancreatitis with groove involvement (Figure 1C). In addition, in recent years, Adsay and Zamboni[5] proposed the term “paraduodenal pancreatitis” in patients classified as having “cystic dystrophy of the heterotopic pancreas” or “paraduodenal wall cyst” or “groove pancreatitis”; they also recognized two types of pancreatitis: one characterized by cystic changes and the other characterized by solid lesions. These authors pointed out that the latter type of pancreatitis is difficult to distinguish from an adenocarcinoma originating in this area. Finally, the presence of cystic dystrophy of the duodeno-pancreatic space together with chronic pancreatitis of the remaining pancreas is not always true because there is also the possibility of disease limited to the CBD[6]. Thus, in this review, we report our recent experience on cystic dystrophy of the space from the C-loop of the duodenum and the pancreas by reporting three cases observed in the last year, and also systematically review and discuss the data in the literature on the alteration of the groove space.
Figure 1.

Classification of the various types of groove pancreatitis. A: Typical finding of groove pancreatitis (purple area); B: Segmental head pancreatitis: the scar tissue (dark blue) expands towards the duodenum; C: Pancreatitis of the head: the scar tissue (dark blue) expands to the duodenal area, determining duodenal stenosis and displacement of the common bile duct.
OUR EXPERIENCE ON THREE RECENT OBSERVED CASES OF CYSTIC DYSTROPHY OF THE DUODENAL WALL
We report our experience on three recently observed cases of cystic dystrophy of duodenal wall. Patients were one female and two males aged 49-65 years having persistent abdominal pain and weight loss. One male patient was a drinker and the diagnosis in all 3 patients was confirmed at laparotomy. The pathological examination in two cases confirmed cystic dystrophy of duodenal wall associated with chronic pancreatitis in one case and autoimmune pancreatitis and pancreatic carcinoma in the remaining one.
Case 1
A 65-year-old female was admitted to our department in April 2009 for persistent abdominal discomfort and progressive weight loss (about 5 kg in two months). Before this admission, she had had a one-year history of recurrent epigastric pain; an ultrasonographic (US) examination showed gallstones and the patient had been cholecystectomized in another hospital. After surgery, she continued to have recurrent and frequent episodes of epigastric pain; US showed a dilation of the CBD and, two months after surgery, she underwent an endoscopic sphincterotomy. One month after this procedure, epigastric pain reappeared and, due to the presence of scleral jaundice (total bilirubin 3.2 mg/dL), the patient underwent another endoscopic retrograde cholangiopancreatography (ERCP). The papilla of Vater was substenotic and another sphincterotomy was carried out without any clinical improvement. On admission to our department, physical examination was unremarkable as was a routine blood examination; her body temperature was 37.2 °C, her arterial pressure was 110/60 mmHg and her cardiac rate was 73 bpm. Contrast-enhanced multidetector computer tomography (MDCT) was carried out. This examination showed the presence of multiple hypodense lesions in the liver (Figure 2); a US fine needle biopsy of one of these lesions was carried out and the pathological specimen was compatible with an abscess; the liver tissue was also cultured and the patient was treated with a specific antibiotic. At computer tomography (CT) examination, there was the presence of biliary sludge and a dilation of the left intrahepatic biliary tree. There was also the presence of duodenal bulging (Figure 3A) while the pancreatic gland was normal (Figure 3B). An endoscopic US (EUS) was finally carried out. It confirmed the presence of duodenal bulging (Figure 4A) and showed CBD sludge; in addition, cysts in the duodenal wall were seen (Figure 4B) and a diagnosis of cystic dystrophy of duodenal wall was made. The patient refused surgery, and conservative treatment with ursodeoxycholic acid was carried out. Twenty months after discharge, the patient was free of abdominal discomfort and regained her lost weight.
Figure 2.

Case No. 1 computer tomography liver evaluation. Liver multiple hypodense lesions compatible with abscesses.
Figure 3.
Case No. 1 computer tomography duodenal and pancreatic gland evaluation. A: Presence of duodenal bulging; B: Normal appearance of the pancreatic gland.
Figure 4.

Case No. 1 computer tomography duodenal and pancreatic gland evaluation. A: Presence of duodenal bulging; B: Presence of cysts in the duodenal wall.
Case 2
A 49-year-old male patient with a history of chronic alcoholic consumption (about 40 g of pure alcohol intake per day) was admitted to our Department in May 2010 with persistent epigastric pain of seven months duration associated with nausea and biliary vomiting; there was also weight loss of 13 kg. The following biochemical tests were carried out: Hb 11.9 g/dL, MCV 85.8; amylase 156 U/L (upper reference value 100), CA 19-9: 52 U/mL (upper reference value 37). The patient underwent an upper gastrointestinal endoscopy which was normal. Ultrasonographic examination did not show alterations of the abdominal parenchyma. MDCT showed an enlarged pancreatic head and the presence of multiple cysts between the enlarged pancreatic head and the duodenum (Figure 5A); the remaining pancreas was normal as was demonstrated by magnetic resonance imaging (MRI) (Figure 5B). The patient was operated on and a pancreatic head resection was performed. The pathology of the resected specimen showed cystic dystrophy of the duodenal wall with hypertrophy of the Brunner glands and the presence of an ectopic pancreas (Figure 6A), showing chronic pancreatitis (Figure 6B). Seven months after surgery, the patient was symptom free and in good general health.
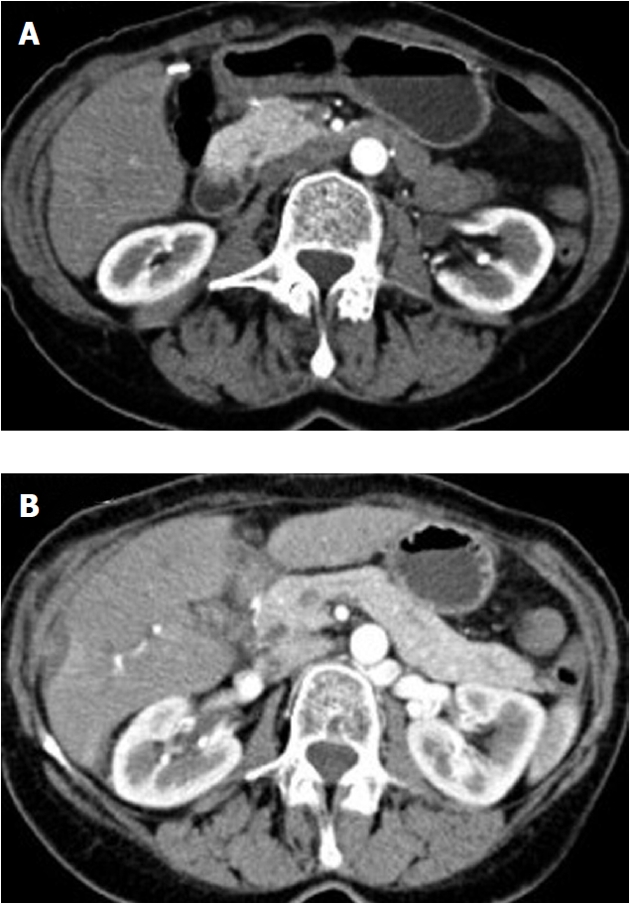
Figure 5.

Case No. 2 computer tomography duodenal and pancreatic gland evaluation. A: Enlarged pancreatic head and the presence of multiple cysts between the enlarged pancreatic head and the duodenum (multidetector computer tomography); B: The remaining pancreas was normal as demonstrated by the magnetic resonance imaging.
Figure 6.

Case No. 2 pancreatic and duodenal surgical specimens. A: Resected specimen showing cystic dystrophy of the duodenal wall with hypertrophy of the Brunner glands and the presence of an ectopic pancreas (arrows); B: Chronic pancreatitis in the remaining pancreas together with cystic dystrophy of the duodenal wall.
Case 3
A 56-year-old male affected by Crohn’s disease was seen in August 2010 with persistent epigastric pain of one month duration associated with jaundice, weight loss, nausea and intermittent vomiting. The patient was not an alcohol drinker. The following biochemical tests were carried out: total bilirubin, 25.4 mg/dL, AST, 63 U/L (upper normal limit 38), ALT, 66 U/L (upper normal limit 40), alkaline phosphatases, 1105 U/L (normal value 98-280), amylase, 108 U/L (upper normal limit 100), lipase, 293 U/L (upper normal limit 60), CA, 19-9 2345 U/mL (upper reference value 37). The patient underwent US which showed a dilated CBD and a mass of 2.5 cm in the head of the pancreas. The MDCT showed the pancreatic head focally enlarged with a 2.5 cm heterogeneous area extending to and involving the wall of the posterior bulbar duodenum. The main pancreatic duct was uniformly dilated in caliber and appearance with no changes in the pancreatic body or tail. The patient underwent a pancreaticoduodenectomy and surgical pathology showed the presence of cystic dystrophy of the duodenal wall (Figure 7A) with aspects of chronic pancreatitis in the heterotopic pancreas (Figure 7A), aspects of autoimmune pancreatitis (Figure 7B) and, finally, groove adenocarcinoma extending to the pancreatic head (Figure 7C). At present, the patient is still alive and is in adjuvant chemotherapy with gemcitabine.
Figure 7.

Case No. 3 pancreatic and duodenal pathological specimens. A: Cystic dystrophy of the duodenal wall with aspects of chronic pancreatitis in the heterotopic pancreas; B: Aspects of autoimmune pancreatitis (arrow); C: Groove adenocarcinoma extending to the pancreatic head (arrow).
CLINICAL CONSIDERATIONS AND AIMS
The present report involving three cases of cystic dystrophy of the duodenal wall represents one of the few case series published concerning this rare entity. All of our patients presented with symptoms consistent with chronic pancreatitis; however, pancreatic diseases were found in two and these two patients improved dramatically after surgical head pancreatic resection while one is symptom free after medical treatment. It is important to diagnose the pathological involvement of the proximal duodenum in order to detect the presence of malignancy and to evaluate the prognosis of these subjects. In order to better establish the features of this rare entity we also undertook a systematic review of the literature.
LITERATURE SEARCH AND DATA EXTRACTION
A search was carried out on December 18, 2010 using the MEDLINE/PubMed database (United States National Library of Medicine National Institutes of Health) in order to select the data existing in the literature under the headings of pancreatitis and groove pancreatitis. The terms used were “groove pancreatitis” or “duodenal cystic dystrophy” (explanatory variables) and “pancreatic diseases” (outcome variable). The search was limited to human studies written in English. We identified additional studies by means of a hand search of the bibliographies from the primary studies, review articles and key journals. A total of 70 citations were found in MEDLINE/PubMed[4-73]. Four investigators (Pezzilli R, Morselli-Labate AM, Fabbri D, and Imbrogno A) independently screened all articles for those meeting the broad inclusion criteria. Of the 70 papers, 4 were excluded because they contained data regarding diseases other than those searched for[8,15,48,71]. Of the remaining 66 papers, 10 were excluded because they were review articles not containing data useful for the analyses[4,5,24,41,42,45,56,58,60,68] and one because it was a comment on an article[19] without new data/cases; therefore, 55 papers with available data remained. Of these 55 papers, 4 were also excluded for the following reasons: 1 because it was a duplicated publication[55] and 3 because it was not possible to extract useful data[49,57,73]. Eight papers were added to these 51 papers because they were extracted from the references[74-81]. Thus, 59 papers were considered for the present study; there were 19 cohort studies[6,7,10-13,16,18,23,30,36,37,39,40,46,47,52,63,81] and 40 case reports[9,14,17,20-22,25-29,31-35,38,43,44,50,51,53,54,59,61,62,64-67,69,70,72,74-80].
For each study, the following information was recorded: gender, mean age for the cohort studies or age of the subjects studied in the case reports, interval time from the appearance of the symptoms to diagnosis, alcoholism, the presence of clinical variables (such as abdominal pain, weight loss and jaundice, hyperamylasemia, CBD stenosis, duodenal stenosis), the need for surgery and the type of surgery, the possible presence of chronic pancreatitis in the pancreas together with cystic dystrophy as well as the presence of pseudocysts, the possible presence of pancreatic neoplasms, the time of follow-up and death.
Data are presented as absolute numbers and relative frequencies, mean ± SD, medians, ranges, and interquartile ranges (IQR); follow-up data are also presented as crude survival.
EVALUATION OF THE SELECTED STUDIES
Due to the low frequency of diseases, such as groove pancreatitis and groove carcinomas, there is a limited number of cohort studies (No. 19) and a large number of case reports (No. 40). All the cohort studies were retrospective and patients were enrolled from 1959[11] to 2008[6]. Thus, the changes in diagnostic techniques with the appearance of MRI and EUS in clinical practice render the studies not comparable as to what is the best technique for diagnosing groove diseases. Furthermore, the mean follow-ups vary greatly and the longest follow-up is about 8 years which is that reported by Casetti et al[63]. As shown in Tables 1, 2, 3, 4, 5, 6, 7 and 8, we found no substantial differences between the data reported in the cohort studies and those we calculated when grouping the series of case reports by gender, age at diagnosis, alcoholism, presence of pain, weight loss, jaundice, hyperamylasemia, CBD stenosis, duodenal stenosis and the need for surgery. The presence of chronic pancreatitis and deaths were more frequently reported in the cohort studies than in the case reports while associated adenocarcinoma and pseudocysts were more frequently reported in the case reports than in the cohort studies.
Table 1.
Epidemiological and clinical characteristics of patients in the 18 retrospective studies involving patients with a benign cystic duodenal wall
| Author[Ref.] yr | Time interval of | n (%) | Age (yr) | Alcohol drinkers | ||
| patient enrollment | Total | Males | Females | Mean (range) | n (%) | |
| Stolte et al[7] 1982 | NR | 30 | 30 (100) | - | 41.3 (NR) | 22 (73.3) |
| Yamaguchi et al[10] 1992 | 1983-1989 | 8 | 8 (100) | - | 58.0 (33-70) | 4 (50.0) |
| Fléjou et al[11] 1993 | 1959-1991 | 10 | 10 (100) | - | 41.0 (31-56) | 2 (20.0) |
| Itoh et al[12] 1994 | NR | 4 | 3 (75.0) | 1 (25.0) | 43.0 (37-53) | NR |
| Fékété et al[13] 1996 | 1989-1993 | 6 | 6 (100) | - | 40.0 (35-46) | 4 (66.7) |
| Procacci et al[16] 1997 | 1992-1996 | 10 | 10 (100) | - | 41.0 (32-59) | 9 (90.0) |
| Irie et al[18] 1998 | 1995-1996 | 5 | 5 (100) | - | 41.0 (33-46) | 2 (40.0) |
| Vullierme et al[23] 2000 | 1988-1998 | 20 | 18 (90.0) | 2 (10.0) | 44.0 (36-56) | NR |
| Aoun et al[81] 2005 | NR | 4 | 2 (50.0) | 2 (50.0) | 69.0 (66-71) | NR |
| Pessaux et al[36] 2006 | 1990-2004 | 12 | 11 (91.7) | 1 (8.3) | 42.4 (34-54) | 9 (75.0) |
| Jouannaud et al[37] 2006 | 1990-2002 | 23 | 20 (87.0) | 3 (13.0) | 45.0 (30-66) | 23 (100) |
| Tison et al[39] 2007 | 1983-2001 | 9 | 8 (88.9) | 1 (11.1) | 48.0 (37-63) | 8 (88.9) |
| Rebours et al[40] 2007 | 1995-2004 | 105 | 96 (91.4) | 9 (8.6) | 46.0 (24-75) | 86 (81.9) |
| Rahman et al[46] 2007 | 2000-2005 | 11 | 10 (90.9) | 1 (9.1) | 48.0 (35-61) | 10 (90.9) |
| Castell-Monsalve et al[47] 2008 | NR | 5 | 4 (80.0) | 1 (20.0) | 47.0 (40-53) | 4 (80.0) |
| Jovanovic et al[52] 2008 | 1996-2006 | 13 | 10 (76.9) | 3 (23.1) | 41.5 (17-60) | 6 (6.2) |
| Casetti et al[63] 2009 | 1990-2006 | 58 | 54 (93.1) | 4 (6.9) | 44.7 (IQR 36.8-51.8) | 57 (98.3) |
| Ishigami et al[6] 2010 | 2001-2008 | 15 | 14 (93.3) | 1 (6.7) | 48.0 (31-64) | NR |
| Overall | - | 348 | 319 (91.70) | 29 (8.30) | - | 246/305 (80.70) |
IQR: Interquartile range; NR: Not reported.
Table 2.
Epidemiological and clinical characteristics of patients in the 18 retrospective studies involving patients with a benign cystic duodenal wall (continues from Table 1) n (%)
| Author[Ref.] yr | Time interval from the symptoms to the diagnosis | Abdominal pain | Weight loss | Jaundice | Hyperamylasemia | |
| Mean (range) | No. of cases | Type | ||||
| Stolte et al[7] 1982 | NR | NR | NR | 30 (100) | NR | NR |
| Yamaguchi et al[10] 1992 | NR | 3 (37.5) | NR | 0 | 2 (25.0) | NR |
| Fléjou et al[11] 1993 | NR | 7 (70.0) | Persistent | 9 (90.0) | 4 (40.0) | NR |
| Itoh et al[12] 1994 | NR | 3 (75.0) | NR | NR | NR | 3 (75.0) |
| Fékété et al[13] 1996 | NR | 6 (100) | Recurrent | 6 (100) | 0 | 6 (100) |
| Procacci et al[16] 1997 | 4.5 yr (1-9) | 10 (100) | Recurrent | 4 (40.0) | 1 (10.0) | NR |
| Irie et al[18] 1998 | NR | 4 (80.0) | NR | 0 | 0 | NR |
| Vullierme et al[23] 2000 | 41.5 d (1-140) | NR | NR | NR | NR | NR |
| Aoun et al[81] 2005 | NR | 3 (75.0) | NR | 0 | 1 (25.0) | NR |
| Pessaux et al[36] 2006 | NR | 9 (75.0) | Persistent in 4 (44.4) | 12 (100) | 2 (16.7) | NR |
| Jouannaud et al[37] 2006 | NR | 22 (95.7) | NR | 16 (69.6) | 0 | NR |
| Tison et al[39] 2007 | NR | 9 (100) | NR | 9 (100) | 2 (22.2) | NR |
| Rebours et al[40] 2007 | 1 yr (0-24) | 91 (86.7) | Continuous in 35 (38.4); occasional in 56 (61.5) | 73 (69.6) | 13 (12.4) | NR |
| Rahman et al[46] 2007 | NR | 11 (100) | Recurrent in 8 (72.7) | 10 (90.9) | 0 | 2 (18.2) |
| Castell-Monsalve et al[47] 2008 | NR | 5 (100) | Persistent | NR | NR | 5 (100) |
| Jovanovic et al[52] 2008 | 7.5 mo (0.5-36) | 12 (92.3) | NR | 4 (30.8) | 4 (30.8) | NR |
| Casetti et al[63] 2009 | NR | 46 (79.3) | Persistent | NR | 3 (5.2) | NR |
| Ishigami et al[6] 2010 | NR | NR | NR | NR | NR | NR |
| Overall | - | 241/283 | - | 173/246 | 32/274 | 16/26 |
| (85.20) | (70.30) | (11.70) | (61.50) | |||
NR: Not reported.
Table 3.
Epidemiological and clinical characteristics of patients in the 18 retrospective studies involving patients with a benign cystic duodenal wall (continues from Table 2) n (%)
| Author[Ref.] yr | Imaging | Duodenal findings | CBD stenosis | Duodenal stenosis |
| Stolte et al[7] 1982 | NR | Brunner hyperplasia in 25 | 15 (50.0) | NR |
| Yamaguchi et al[10] 1992 | US, CT, ERCP, PTC | Edema and nodular appearance; Brunner hyperplasia | 4 (50.0) | 5 (62.5) |
| Fléjou et al[11] 1993 | ERCP, EUS | Edema and congestion of the mucosa | 0 | 7 (70.0) |
| Itoh et al[12] 1994 | CT | NR | NR | NR |
| Fékété et al[13] 1996 | CT, ERCP, EUS | Edema and congestion of the mucosa | 0 | 5 (83.3) |
| Procacci et al[16] 1997 | CT, ERCP, EUS | Inflammation in 8 | 2 (20.0) | 2 (20.0) |
| Irie et al[18] 1998 | MRI | Brunner hyperplasia in 3 | 2 (40.0) | 3 (60.0) |
| Vullierme et al[23] 2000 | CT | NR | 3 (15.0) | 20 (100) |
| Aoun et al[81] 2005 | US, CT, ERCP, EUS | NR | 4 (100) | NR |
| Pessaux et al[36] 2006 | US, EUS, CT, ERCP, MRI | NR | NR | NR |
| Jouannaud et al[37] 2006 | EUS, CT | Inflammation in 3 | NR | 8 (34.8) |
| Tison et al[39] 2007 | US, CT, MRI, angiography | Non specific inflammation in 9 | 5 (55.6) | 9 (100) |
| Rebours et al[40] 2007 | CT, EUS | Brunner hyperplasia in 61 | 26 (24.8) | 50 (47.6) |
| Rahman et al[46] 2007 | CT, MRI, EUS | Brunner hyperplasia | 0 | 5 (45.5) |
| Castell-Monsalve et al[47] 2008 | MRI, EUS | Duodenal stenosis in 3 | 3 (60.0) | 3 (60.0) |
| Jovanovic et al[52] 2008 | US, CT, MRI, EUS | NR | 6 (46.2) | NR |
| Casetti et al[63] 2009 | US, CT, MRI, EUS | NR | 3 (5.2) | NR |
| Ishigami et al[6] 2010 | CT, MRI | NR | 9 (60.0) | NR |
| Overall | - | - | 82/309 | 117/212 |
| (26.50) | (55.20) |
CBD: Common bile duct; NR: Not reported; US: Transabdominal ultrasonography; CT: Computer tomography; MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasonography; ERCP: Endoscopic retrograde cholangiopancreatography; PTC: Percutaneous transhepatic cholangiography.
Table 4.
Epidemiological and clinical characteristics of patients in the 18 retrospective studies involving patients with a benign cystic duodenal wall (continues from Table 3) n (%)
| Author[Ref.] yr | Surgery | Associated chronic pancreatitis | Associated neoplasms | Pseudocyst | Follow-up | |||
| No. of cases | Type | Mean (range) | Death | Lost | ||||
| Stolte et al[7] 1982 | 30 (100) | PD | 4 (13.3) (all with calcification) | No | 5 (16.7) | NR | NR | NR |
| Yamaguchi et al[10] 1992 | 8 (100) | PD | NR | No | No | 2 yr | 1 (12.5) | NR |
| Fléjou et al[11] 1993 | 10 (100) | WP in 8; | 0 | No | No | 1-5 yr | 1 (10.0) | 4 (40.0) |
| derivative in 2 | ||||||||
| Itoh et al[12] 1994 | 3 (75.0) | PD | NR | No | No | No | NR | NR |
| Fékété et al[13] 1996 | 6 (100) | PD in 5; | NR | No | No | 32 mo (18-64) | No | NR |
| antrectomy in 1 | ||||||||
| Procacci et al[16] 1997 | 10 (100) | PD | 7 (70.0) (calcifications in 5) | No | 5 (head) (50.0) | NR | NR | NR |
| Irie et al[18] 1998 | 3 (60.0) | PD | 2 (40.0) (all with calcifications) | No | No | NR | NR | NR |
| Vullierme et al[23] 2000 | 20 (100) | PD | 9 (45.0)(calcifications in 5) | No | No | NR | NR | NR |
| Aoun et al[81] 2005 | 4 (100) | PD | NR | NR | NR | NR | NR | NR |
| Pessaux et al[36] 2006 | 12 (100) | PD | 8 (66.7) (calcification in 2) | No | No | 64 mo (6-158) | 1 (8.3) | 1 (8.3) |
| Jouannaud et al[37] 2006 | 14 (60.9) | PD in 11; | 17 (73.9) (calcification in 10) | No | No | 47 mo | 1 (4.3) | NR |
| derivative in 3 | ||||||||
| Tison et al[39] 2007 | 9 (100) | PD | 5 (55.6) | No | No | 72 mo | 4 (44.4) | NR |
| Rebours et al[40] 2007 | 29 (27.6) | PD in 17; digestive and biliary by pass in 12 | 97 (92.4) (calcification in 96) | No | No | 15 mo (0-243) | NR | NR |
| Rahman et al[46] 2007 | 11 (100) | PD | 0 | No | No | NR | NR | NR |
| Castell-Monsalve et al[47] 2008 | 4 (80.0) | WP in 3; | 3 (60.0) | No | No | NR (13-36 mo) | No | NR |
| 1 laparotomy | ||||||||
| Jovanovic et al[52] 2008 | 13 (100) | PD | 6 (46.2) | No | No | NR | NR | NR |
| Casetti et al[63] 2009 | 58 (100) | PD | NR | Neuroendocrine in 1 | No | 93.6 mo | NR | NR |
| (IQR 59.7-129.7) | ||||||||
| Ishigami et al[6] 2010 | 6 (40.0) | PD in 3, derivative surgery in 3 | NR | NR | NR | NR | NR | NR |
| Overall | 250/348 | - | 158/253 | 1/329 | 10/329 | - | 8/73 | 5/22 |
| (71.8) | (62.5) | (0.3%) | (3.0) | (11.0) | (22.7) | |||
IQR: Interquartile range; NR: Not reported; PD: Pancreaticoduodenectomy; WP: Whipple procedure.
Table 5.
Epidemiological and clinical characteristics of patients in the 38 case report papers involving 46 subjects with a benign cystic duodenal wall (a paper may report more than one patient), the three cases reported in the present paper are also shown
| Author[Ref.] yr | Gender | Age (yr) | Alcohol drinker |
| Bill et al[74] 1982 | Male | 64 | Yes |
| Holstege et al[75] 1985 | Male | 44 | Yes |
| Tio et al[9] 1991 | Male | 48 | NR |
| Tio et al[9] 1991 | Male | 53 | NR |
| Flaherty et al[75] 1992 | Female | 20 mo | No |
| Izbicki et al[77] 1994 | Male | 25 | NR |
| Fujita et al[14] 1997 | Male | 42 | Yes |
| Shudo et al[17] 1998 | Male | 66 | Yes |
| Wu et al[78] 1998 | Male | 39 | NR |
| Babál et al[79] 1998 | Female | 70 | NR |
| Rubay et al[21] 1999 | Male | 46 | Yes |
| Balachandar et al[22] 1999 | Male | 18 | NR |
| Mohl et al[25] 2001 | Male | 44 | Yes |
| Mohl et al[25] 2001 | Male | 42 | Yes |
| Munthali Lovemore et al[26] 2001 | Male | 24 | No |
| Indinnimeo et al [27] 2001 | Male | 46 | Yes |
| Shudo et al[28] 2002 | Male | 53 | Yes |
| Glaser et al[29] 2002 | Male | 51 | Yes |
| Hwang et al[31] 2003 | Male | 46 | Yes |
| Jovanovic et al[32] 2004 | Male | 38 | No |
| McFaul et al[80] 2004 | Male | 29 | Yes |
| McFaul et al[80] 2004 | Male | 62 | Yes |
| Isayama et al[33] 2005 | Male | 56 | Yes |
| Chatelain et al[34] 2005 | Male | 47 | Yes |
| Chatelain et al[34] 2005 | Female | 44 | Yes |
| Balzan et al[35] 2005 | Male | 47 | NR |
| Sanada et al[43] 2007 | Male | 81 | No |
| Balakrishnan et al[44] 2007 | Male | 40 | Yes |
| de Tejada et al[50] 2008 | Male | 47 | Yes |
| Stefanescu et al[51] 2008 | Male | 15 | No |
| Varma et al[53] 2008 | Female | 23 | NR |
| Galloro et al[54] 2008 | Male | 44 | Yes |
| Thomas et al[59] 2009 | Male | 43 | NR |
| Levenick et al[61] 2009 | Female | 35 | Yes |
| Levenick et al[61] 2009 | Male | 47 | Yes |
| Levenick et al[61] 2009 | Female | 36 | Yes |
| Levenick et al[61] 2009 | Female | 54 | NR |
| Yoshida et al[62] 2009 | Male | 63 | Yes |
| Meesiri[64] 2009 | Male | 44 | Yes |
| Funamizu et al[65] 2009 | Female | 54 | NR |
| Viñolo Ubiña et al[66] 2010 | Male | 40 | Yes |
| Tezuka et al[67] 2010 | Male | 55 | Yes |
| Lee et al[69] 2010 | Male | 75 | NR |
| Egorov et al[70] 2010 | Male | 32 | Yes |
| Egorov et al[70] 2010 | Male | 43 | NR |
| German et al[72] 2010 | Male | 34 | Yes |
| Pezzilli2011 Present paper | Female | 65 | No |
| Pezzilli 2011 Present paper | Male | 49 | Yes |
| Pezzilli 2011 Present paper | Male | 56 | No |
| Overall | Males: 40 (81.6%) | 45.3 ± 15.2 | 29/36 |
| Females: 9 (18.4%) | (80.50%) |
NR: Not reported.
Table 6.
Epidemiological and clinical characteristics of patients in the 38 case report papers involving 46 subjects with a benign cystic duodenal wall (a paper may report more than one patient), the three cases reported in the present paper are also shown (continues from Table 5)
| Author[Ref.] yr | Time interval from the onset of symptoms to diagnosis | Abdominal pain | Weight loss | Jaundice | Hyperamylasemia |
| Bill et al[74] 1982 | NR | Yes (Persistent) | Yes | No | No |
| Holstege et al[75] 1985 | 6 mo | Yes (Persistent) | Yes | No | Yes |
| Tio et al[9] 1991 | NR | Yes (NR) | No | No | NR |
| Tio et al[9] 1991 | NR | Yes (NR) | No | Yes | NR |
| Flaherty et al[75] 1992 | NR | Yes (NR) | No | No | NR |
| Izbicki et al[77] 1994 | NR | Yes (Recurrent) | No | No | No |
| Fujita et al[14] 1997 | NR | Yes (Recurrent) | Yes | No | No |
| Shudo et al[17] 1998 | NR | Yes (Persistent) | No | No | Yes |
| Wu et al[78] 1998 | 10 yr | Yes (Recurrent) | Yes | No | NR |
| Babál et al[79] 1998 | NR | No | No | No | NR |
| Rubay et al[21] 1999 | 7 yr | Yes (Recurrent) | Yes | No | Yes |
| Balachandar et al[22] 1999 | NR | No | No | Yes | No |
| Mohl et al[25] 2001 | 1 yr | Yes (Recurrent) | Yes | No | NR |
| Mohl et al[25] 2001 | 1 yr | Yes (Persistent) | Yes | No | NR |
| Munthali Lovemore et al[26] 2001 | NR | Yes (Persistent) | NR | Yes | Yes |
| Indinnimeo et al[27] 2001 | 10 yr | Yes (Recurrent) | No | No | Yes |
| Shudo et al[28] 2002 | NR | Yes (Persistent) | No | No | Yes |
| Glaser et al[29] 2002 | NR | Yes (Persistent) | Yes | No | No |
| Hwang et al[31] 2003 | NR | Yes (Persistent) | Yes | No | Yes |
| Jovanovic et al[32] 2004 | NR | Yes (Persistent) | Yes | No | Yes |
| McFaul et al[80] 2004 | 13 mo | Yes (Recurrent) | Yes | No | NR |
| McFaul et al[80] 2004 | 2 yr | Yes (Recurrent) | Yes | Yes | NR |
| Isayama et al[33] 2005 | 2 yr | Yes (Persistent) | Yes | No | No |
| Chatelain et al[34] 2005 | 1 yr | Yes (Recurrent) | Yes | No | No |
| Chatelain et al[34] 2005 | NR | Yes (Persistent) | Yes | No | No |
| Balzan et al[35] 2005 | 2 yr | Yes (Persistent) | No | No | Yes |
| Sanada et al[43] 2007 | NR | Yes (Persistent) | No | No | Yes |
| Balakrishnan et al[44] 2007 | NR | Yes (Persistent) | Yes | No | Yes |
| de Tejada et al[50] 2008 | 2 mo | Yes (Persistent) | Yes | No | NR |
| Stefanescu et al[51] 2008 | 5 mo | Yes (Persistent) | Yes | No | NR |
| Varma et al[53] 2008 | 3 mo | Yes (Persistent) | Yes | No | NR |
| Galloro et al[54] 2008 | NR | Yes (Recurrent) | Yes | No | Yes |
| Thomas et al[59] 2009 | NR | Yes (NR) | Yes | No | NR |
| Levenick et al[61] 2009 | NR | Yes (Recurrent) | NR | No | NR |
| Levenick et al[61] 2009 | NR | Yes (Recurrent) | Yes | No | NR |
| Levenick et al[61] 2009 | NR | Yes (Recurrent) | Yes | No | NR |
| Levenick et al[61] 2009 | NR | No | Yes | No | NR |
| Yoshida et al[62] 2009 | NR | Yes (Persistent) | No | No | Yes |
| Meesiri[64] 2009 | NR | Yes (Recurrent) | No | No | Yes |
| Funamizu et al[65] 2009 | NR | Yes (Persistent) | No | Yes | Yes |
| Viñolo Ubiña et al[66] 2010 | 3 mo | Yes (Persistent) | No | No | Yes |
| Tezuka et al[67] 2010 | NR | Yes (NR) | No | No | Yes |
| Lee et al[69] 2010 | NR | Yes (Recurrent) | No | No | Yes |
| Egorov et al[70] 2010 | 2 mo | Yes (Persistent) | Yes | No | Yes |
| Egorov et al[70] 2010 | 1 yr | Yes (Persistent) | Yes | Yes | No |
| German et al[72] 2010 | NR | Yes (Recurrent) | Yes | No | Yes |
| Pezzilli 2011 Present paper | 1 yr | Yes (Recurrent) | Yes | Yes | No |
| Pezzilli 2011 Present paper | 7 mo | Yes (Persistent) | Yes | No | Yes |
| Pezzilli 2011 Present paper | 1 mo | Yes (Persistent) | Yes | Yes | Yes |
| Overall | 2.1 ± 3.1 yr | 46/49 | 30/47 | 8/49 | 22/33 |
| (93.90%) | (63.80%) | (16.30%) | (66.70%) |
CBD: Common bile duct; NR: not reported.
Table 7.
Epidemiological and clinical characteristics of patients in the 38 case report papers involving 46 subjects with a benign cystic duodenal wall (a paper may report more than one patient), the three cases reported in the present paper are also shown (continues from Table 6)
| Author[Ref.] yr | Imaging | Duodenal findings | CBD stenosis | Duodenal stenosis |
| Bill et al[74] 1982 | US, ERCP, angiography | NR | Yes | No |
| Holstege et al[75] 1985 | US, CT, ERCP | Severe erosive gastritis + bulging of the duodenum | No | Yes |
| Tio et al[9] 1991 | ERCP, EUS, US | Polypoid lesion | Yes | Yes |
| Tio et al[9] 1991 | ERCP, EUS, US | NR | No | Yes |
| Flaherty et al[75] 1992 | US | No | No | No |
| Izbicki et al[77] 1994 | US, angiography, ERCP | NR | Yes | Yes |
| Fujita et al[14] 1997 | US, CT, ERCP | Inflammation | No | Yes |
| Shudo et al[17] 1998 | CT, US, ERCP, EUS, celiac angiography | Edema duodenal wall, Brunner hyperplasia | No | Yes |
| Wu et al[78] 1998 | CT | NR | No | No |
| Babál et al[79] 1998 | NR | NR | No | No |
| Rubay et al[21] 1999 | CT, ERCP, MRI, EUS | No alterations | NR | Yes |
| Balachandar et al[22] 1999 | CT, ERCP | No duodenal alteration | Yes | No |
| Mohl et al[25] 2001 | CT | Stenosis | No | Yes |
| Mohl et al[25] 2001 | US, CT, ERCP | Normal duodenal mucosa | No | No |
| Munthali Lovemore et al[26] 2001 | US, CT, ERCP | NR | Yes | No |
| Indinnimeo et al[27] 2001 | CT, MRI, EUS | No alterations | No | No |
| Shudo et al[28] 2002 | CT, US, ERCP, EUS, celiac angiography | Irregular polypoid bulging; inflammation of the mucosa | NR | Yes |
| Glaser et al[29] 2002 | US | Severe deformation + inflammatory changes | No | Yes |
| Hwang et al[31] 2003 | US, CT, MRI | Duodenal inflammation, duodenal stenosis | NR | Yes |
| Jovanovic et al[32] 2004 | US, CT, EUS, MRI | Stenosis | No | Yes |
| McFaul et al[80] 2004 | US, CT, MRI | Brunner hyperplasia | Yes | Yes |
| McFaul et al[80] 2004 | US, PET-CT | Brunner hyperplasia | No | No |
| Isayama et al[33] 2005 | CT, EUS, MRCP, ERCP | NR | No | Yes |
| Chatelain et al[34] 2005 | EUS, CT | Duodenal stenosis, inflammation | No | Yes |
| Chatelain et al[34] 2005 | EUS, CT | Duodenal stenosis | No | Yes |
| Balzan et al[35] 2005 | US, MRI, CT | NR | NR | NR |
| Sanada et al[43] 2007 | CT, ERCP | Edema duodenal wall, Brunner hyperplasia | Yes | No |
| Balakrishnan et al[44] 2007 | CT, ERCP, EUS | Edematous, shiny, reddish raise mucosa with polypoid appearance; Brunner hyperplasia | No | No |
| de Tejada et al[50] 2008 | MRI, EUS | Bulging, Brunner hyperplasia | No | No |
| Stefanescu et al[51] 2008 | CT, EUS | NR | No | Yes |
| Varma et al[53] 2008 | US, CT | Brunner hyperplasia | No | No |
| Galloro et al[54] 2008 | US, CT, EUS | Duodenal stenosis | No | Yes |
| Thomas et al[59] 2009 | US, CT, EUS, octreotide scan | Brunner hyperplasia | No | Yes |
| Levenick et al[61] 2009 | EUS, MRCP | Duodenal stenosis | No | Yes |
| Levenick et al[61] 2009 | CT, EUS | Duodenal inflammation, duodenal stenosis | NR | Yes |
| Levenick et al[61] 2009 | CT, EUS | Edema with acute and chronic inflammation | No | Yes |
| Levenick et al[61] 2009 | CT, EUS, ERCP | NR | Yes | No |
| Yoshida et al[62] 2009 | CT, MRCP | Normal mucosa | No | Yes |
| Meesiri[64] 2009 | US, CT, MRI | Edema and hemorrhagic mucosa with inflammation | NR | No |
| Funamizu et al[65] 2009 | ERCP, CT, angiography | NR | Yes | No |
| Viñolo Ubiñaet al[66] 2010 | CT | Stenosis | NR | Yes |
| Tezuka et al[67] 2010 | CT, ERCP | Edema duodenal wall | No | Yes |
| Lee et al[69] 2010 | CT, MRCP | Active ulcer | Yes | No |
| Egorov et al[70] 2010 | US, CT, EUS | Deformation, infiltration and ulcer; Inflammation | No | Yes |
| Egorov et al[70] 2010 | US, CT, MRI, EUS | NR | Yes | Yes |
| German et al[72] 2010 | US, CT, MRI | Edema duodenal wall; Brunner hyperplasia | Yes | Yes |
| Pezzilli 2011 Present paper | US, CT, EUS, ERCP | No | Yes | No |
| Pezzilli 2011 Present paper | US, CT, MRI | Hypertrophy of the Brunner glands | No | No |
| Pezzilli 2011 Present paper | US, CT | No | Yes | No |
| Overall | - | - | 14/42 | 28/48 |
| (33.30%) | (58.30%) |
CBD: Common bile duct; NR: Not reported; US: Transabdominal ultrasonography; CT: Computer tomography; MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasonography; ERCP: Endoscopic retrograde cholangiopancreatography; MRCP: Magnetic resonance cholangiopancreatography; PET-CT: Positron emission tomography with associated computer tomography.
Table 8.
Epidemiological and clinical characteristics of patients in the 38 case report papers involving 46 subjects with a benign cystic duodenal wall (a paper may report more than one patient), The three cases reported in the present paper are also shown (continues from Table 7)
| Author[Ref.] yr | Surgery | Type of surgery | Endoscopic treatment | Associated chronic pancreatitis | Associated neoplasms | Pseudocyst | Follow-up | Death |
| Bill et al[74] 1982 | Yes | PD | No | NR | No | No | No | NR |
| Holstege et al[75] 1985 | Yes | WP | No | No | No | No | No | NR |
| Tio et al[9] 1991 | No | No | No | No | No | 7 yr | No | |
| Tio et al[9] 1991 | Yes | Derivative surgery | No | No | No | No | 6 mo | NR |
| Flaherty et al[75] 1992 | Yes | PD | No | No | No | No | 9 mo | No |
| Izbicki et al[77] 1994 | Yes | PD | No | No | No | No | 6 yr | No |
| Fujita et al[14] 1997 | Yes | PD | No | No | No | No | 3 yr | No |
| Shudo et al[17] 1998 | Yes | PD | No | No | No | No | NR | NR |
| Wu et al[78] 1998 | Yes | WP | No | No | No | No | 9 mo | No |
| Babál et al[79] 1998 | No | No | No | No | No | NR | During hospitalization | |
| Rubay et al[21] 1999 | Yes | PD | No | No | No | No | 2 mo | No |
| Balachandar et al[22] 1999 | Yes | Derivative | No | Yes | No | No | NR | NR |
| Mohl et al[25] 2001 | Yes | PD | No | No | No | No | No | NR |
| Mohl et al[25] 2001 | Yes | PD | No | No | No | No | 4 wk after surgery | No |
| Munthali Lovemore et al[26] 2001 | Yes | Derivative CBD | No | No | No | No | No | NR |
| Indinnimeo et al[27] 2001 | Yes | PD | No | No | No | No | 2 yr | No |
| Shudo et al[28] 2002 | Yes | PD | No | No | No | No | NR | NR |
| Glaser et al[29] 2002 | No | No | No | No | No | No | NR | |
| Hwang et al[31] 2003 | No | No | No | No | No | NR | NR | |
| Jovanovic et al[32] 2004 | Yes | PD | No | No | No | No | No | NR |
| McFaul et al[80] 2004 | Yes | PD | No | Yes | No | No | 2 yr | No |
| McFaul et al[80] 2004 | Yes | WP | No | Yes | No | No | NR | No |
| Isayama et al[33] 2005 | No | Yes | No | No | No | 12 mo | No | |
| Chatelain et al[34] 2005 | Yes | PD | No | No | No | No | 6 mo | No |
| Chatelain et al[34] 2005 | Yes | PD | No | No | No | No | 12 mo | No |
| Balzan et al[35] 2005 | Yes | PD | No | Yes | No | Yes (head) | No | NR |
| Sanada et al[43] 2007 | Yes | PD | No | No | No | Yes (head) | No | NR |
| Balakrishnan et al[44] 2007 | Yes | Laparotomy | No | Yes | No | No | NR | NR |
| de Tejada et al[50] 2008 | Yes | WP | No | No | No | No | 3 mo | No |
| Stefanescu et al[51] 2008 | Yes | Derivative | No | No | No | No | 8 mo | No |
| Varma et al[53] 2008 | Yes | WP | No | No | No | No | 9 mo | No |
| Galloro et al[54] 2008 | Yes | WP | No | Yes | Cystadenoma | Yes | 14 mo | No |
| (with calcifications) | ||||||||
| Thomas et al[59] 2009 | Yes | PD | No | No | No | No | NR | NR |
| Levenick et al[61] 2009 | Yes | PD | No | No | No | No | 3 yr | No |
| Levenick et al[61] 2009 | Yes | PD | No | Yes | No | No | NR | NR |
| Levenick et al[61] 2009 | Yes | PD | No | No | No | No | NR | NR |
| Levenick et al[61] 2009 | Yes | PD | No | No | No | No | NR | NR |
| Yoshida et al[62] 2009 | Yes | PD | No | No | No | No | Yes (time NR) | No |
| Meesiri[64] 2009 | No | No | No | No | No | Yes (time NR) | No | |
| Funamizu et al[65] 2009 | Yes | PD | No | No | Yes | No | 15 mo | No |
| Viñolo Ubiña et al[66] 2010 | Yes | PD | No | No | No | No | NR | No |
| Tezuka et al[67] 2010 | Yes | PD | No | No | No | No | NR | No |
| Lee et al[69] 2010 | No | No | No | No | No | NR | NR | |
| Egorov et al[70] 2010 | Yes | Pancreas-preserving duodenal resection | No | No | No | No | 6 mo | No |
| Egorov et al[70] 2010 | Yes | Pancreas-preserving duodenal resection | No | No | No | No | 5 mo | No |
| German et al[72] 2010 | Yes | PD | No | No | No | No | 2 mo | NR |
| Pezzilli 2011 Present paper | No | Yes | No | No | No | 20 mo | No | |
| Pezzilli 2011 Present paper | Yes | PD | No | No | No | No | 7 mo | No |
| Pezzilli 2011 Present paper | Yes | PD | No | Autoimmune pancreatitis | Yes | No | 4 mo | No |
| Overall | 41/49 | - | 2/49 | 8/48 | 3/49 | 3/49 | 17.9 ± 20.6 mo | 1/28 |
| (83.70%) | (4.10%) | (16.70%) | (6.10%) | (6.10%) | (3.60%) |
CBD: Common bile duct; NR: Not reported; PD: Pancreaticoduodenectomy; WP: Whipple procedure.
EPIDEMIOLOGY
We have no epidemiological data regarding the prevalence and incidence of cystic dystrophy of the duodenal wall in the general population. The data regarding this anomaly mainly describes patients with associated chronic pancreatitis. A recent Italian survey which reviewed the data on chronic pancreatitis in Italy in mixed medical/surgical cases from 2000 to 2005[57] reported that the frequency of groove pancreatitis was 6.2% (55 out of 893 patients) with a higher frequency in males (7.6%, 50/660) than in females (2.1%, 5/233). In a surgical setting, groove pancreatitis ranges from 2.7% to 24.5%[4,7,10,63]; in these cases, the frequency in males is also higher than that in females. We have no epidemiological data regarding groove carcinomas or biliary involvement without pancreatitis or pancreatic adenocarcinoma. In all these studies, the patients having groove pancreatitis were middle aged (about 45 years of age), having a wide range from 20 mo[76] to 75 years of age[40]. Only two of the patients described were children (a 20-mo-old girl and a 15-year-old boy)[51,76]. Mean age was significantly higher in patients having groove carcinoma than in those having groove pancreatitis, namely 70 years of age (range 57 to 80 years)[51].
CLINICAL AND BIOCHEMICAL FEATURES
As shown in Tables 1-8, the main symptoms of cystic dystrophy of the duodenal wall were epigastric pain, weight loss and jaundice. These symptoms were similar in those patients having associated chronic groove pancreatitis and in those patients having groove carcinoma. All these symptoms can be present, further complicating the differential diagnosis with ampullary and periampullary cancers. Pain may be persistent or recurrent, and nausea and vomiting are usually present as accompanying symptoms. The majority of these patients are heavy alcohol drinkers (275/341, 80.6%), and this may explain the fact that most of the patients with groove pancreatitis are males. In addition, in the 18 patients with groove adenocarcinoma, the majority of cases were males (11/18, 61.1%) (Tables 9, 10, 11 and 12).
Table 9.
Epidemiological and clinical characteristics of patients in the two retrospective studies and two case report papers involving two subjects with groove adenocarcinoma
| Author[Ref.] yr | Type of study | Time interval of patient enrollment | No. of patients | Age (yr) | Alcohol drinkers | ||
| Total | Males | Females | Mean (range) | ||||
| Suehara et al[20] 1998 | Case report | 1995 | 1 | 1 | - | 61 | Yes |
| Gabata et al[30] 2003 | Retrospective | 1998-2001 | 9 | 4 (44.4%) | 5 (55.6%) | 72 (56-87) | NR |
| Tan et al[38] 2006 | Case report | NR | 1 | - | 1 | 69 | NR |
| Ishigami et al[6] 2010 | Retrospective | 2001-2008 | 7 | 6 (85.7%) | 1 (14.3%) | 70 (57-80) | NR |
NR: Not reported.
Table 10.
Epidemiological and clinical characteristics of patients in the two retrospective studies and two case report papers involving two subjects with groove adenocarcinoma (continues from Table 9)
| Author[Ref.] yr | Abdominal pain | Weight loss | Jaundice | Hyperamylasemia |
| Suehara et al[20] 1998 | Yes (Persistent) | No | Yes | Yes |
| Gabata et al[30] 2003 | NR | NR | NR | NR |
| Tan et al[38] 2006 | Yes (Persistent) | Yes | Yes | Yes |
| Ishigami et al[6] 2010 | NR | NR | NR | NR |
NR: Not reported.
Table 11.
Epidemiological and clinical characteristics of patients in the two retrospective studies and two case report papers involving two subjects with groove adenocarcinoma (continues from Table 10)
| Author[Ref.] yr | Imaging | Duodenal findings | CBD stenosis | Duodenal stenosis |
| Suehara et al[20] 1998 | US, EUS, CT, MRI, angiography | NR | Yes | No |
| Gabata et al[30] 2003 | CT, RMI, ERCP, angiography | Edema with erosions | 9 (100%) | 9 (100%) |
| Tan et al[38] 2006 | US, MRI, ERCP | NR | Yes | No |
| Ishigami et al[6] 2010 | CT, MRI | NR | 7 (100%) | NR |
CBD: Common bile duct; NR: Not reported; US: Transabdominal ultrasonography; CT: Computer tomography; MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasonography; ERCP: Endoscopic retrograde cholangiopancreatography.
Table 12.
Epidemiological and clinical characteristics of patients in the two retrospective studies and two case report papers involving two subjects with groove adenocarcinoma (continues from Table 11)
| Author[Ref.] yr | Surgery | Associated chronic pancreatitis | Pseudocyst | Follow-up | |
| No. of cases | Type | ||||
| Suehara et al[20] 1998 | Yes | PD | No | No | NR |
| Gabata et al[30] 2003 | 9 (100%) | PD in 7; derivative in 2 | No | No | NR |
| Tan et al[38] 2006 | Yes | By-pass surgery | No | No | NR |
| Ishigami et al[6] 2010 | 6 (85.7%) | PD in 5; derivative in 1 | No | NR | NR |
NR: Not reported; PD: Pancreaticoduodenectomy.
Regarding the laboratory examinations, serum amylase activity was usually abnormally high in these patients (38/59, 64.4%) (Tables 1-8), but the magnitude of this elevation varied greatly. An increase in bilirubin may have also been present, along with an increase in alkaline phosphatases in patients with jaundice. Finally, it has also been reported in the literature that tumor markers, such as serum CA 19-9, are usually within the normal limits[10,58].
ASSOCIATED DISEASES
The majority of patients with cystic dystrophy of the duodenal wall have been reported to have chronic groove pancreatitis or groove carcinoma. However, the lesions in the remaining pancreatic gland not affected by groove pancreatitis have not been fully evaluated. As shown in Tables 1-12, in patients with groove pancreatitis as well as in those with groove carcinoma, the pancreatic gland above the groove lesion is generally not affected by chronic pancreatitis. Chronic pancreatitis of the entire pancreas was reported in 166 of the 302 (55.1%) patients and there were pancreatic calcifications in 125 of these 166 patients (75.3%) (Tables 1-8). The presence of pancreatic pseudocysts was usually rare (13 out of 378, 3.4%) (Tables 1-8), and, in most cases, they were localized in the head of the pancreas (7/13, 53.8%). In addition, some authors have reported that groove pancreatitis is associated with the occasional findings of neuroendocrine tumors[63] or pancreatic cystadenoma[54].
IMAGING ASSESSMENT
As shown in Tables 3, 7, 8 and 11, the imaging diagnosis of dystrophy of the duodenal wall is rarely assessed using a single radiological modality. Even if US is the first line imaging modality in these patients, it is rarely diagnostic. ERCP, which was frequently used in the past, is feasible and in typical cases it demonstrates smooth tubular stenosis at the distal part of the CBD without abnormality of the main pancreatic duct or, occasionally, with only slight irregularities[44,65]. ERCP may also demonstrate irregularity, tapering obstruction or dilatation of the Santorini duct and its branches, sometimes with intraductal stones or protein plugs[44]. At present, ERCP is used mainly for endoscopic therapy[33]; in fact, successful treatment for groove pancreatitis by endoscopic drainage via the minor papilla was carried out in only one patient[33].
For many years, CT has been an excellent imaging modality for diagnosing chronic pancreatitis or adenocarcinoma associated with cystic dystrophy of the duodenal wall[6,16]. In the pure form of groove pancreatitis, it may be visualized as a poorly enhancing hypodense lesion between the pancreatic head and the duodenum, near the minor papilla, reflecting the pathological characteristics of the mass. The delayed enhancement is mainly due to delayed blood circulation caused by fibrous tissue proliferation and artery constriction[12]. In addition, CT may reveal the presence of duodenal stenosis with wall thickening and cystic lesions in the duodenal wall or in the groove area. The cysts may be tiny even if multilocular cystic lesions may be observed. The main pancreatic duct may be mildly dilated above the lesion while, in the pure form, paraduodenal pancreatitis can be expected. In groove pancreatitis and in groove carcinoma, the CBD may be stenosed in its distal part and a dilation of the extra- and intra-hepatic biliary system can be observed[6,16].
The same CT findings can also be observed when utilizing MRI which may reveal a mass between the head of the pancreas and the duodenum associated with duodenal wall thickening. The mass visualized in the groove and/or in the adjacent head of the gland is hypointense to the pancreatic parenchyma. Delayed enhancement may also be seen in the thickened duodenal wall. These imaging features reflect the fibrous involvement of the lesions of groove pancreatitis. Cysts, which may be present in the groove area and the duodenal wall, have high signal intensity. An important diagnostic aspect of MRI, which cannot be evaluated by CT, is the fact that MRI can be followed by magnetic resonance cholangiopancreatography (MRCP); this additional evaluation provides images similar to those of ERCP without the morbidity of this latter technique. In addition, MRCP may visualize those lesions which are not seen in ERCP in the case of serrated duodenal stenosis[18]. The diagnostic value of MRI is superior to CT in evaluating biliary ducts in paraduodenal pancreatitis as well as in groove carcinomas. The stricture, or narrowing of the CBD, may be better approached by using MRCP rather than CT and/or ERCP. The dilation of the space comprising the main pancreatic duct, the CBD and the duodenum is another sign which can be observed in patients with groove pancreatitis or groove carcinoma when using MRCP[47].
In the last few years, EUS has emerged as a useful technique for diagnosing pancreatic diseases because of the accurate evaluation of the biliopancreatic structures through the gastro-duodenal lumen without interference of the abdominal wall or other organs[82]. EUS can easily demonstrate the hypoechoic area between the duodenal wall and the pancreatic parenchyma, narrowing of the duodenal lumen and stenosis of the CBD and/or pancreatic duct in both groove pancreatitis and groove carcinomas[50]. Furthermore, the diagnosis can be confirmed by EUS-guided fine-needle aspiration of the mass visualized.
PATHOLOGY
Macroscopically, groove pancreatitis is associated with an absent or narrow Santorini duct or the presence of pancreas divisum[17], and the difficult outflow of pancreatic fluid may be hypothesized for lesions of the groove similar to those of chronic pancreatitis[17]. The duodenal wall contains dilated ducts, in the majority of cases with thickened secretions, pseudocystic changes as well as adjacent stromal reactions, foreign-body type giant cell reaction engulfing mucoprotein material and myofibroblastic proliferation. Brunner gland hyperplasia is usually present as is dense myoid stromal proliferation, with intervening rounded lobules of pancreatic acinar tissue. Fibrosis into the adjacent pancreas and soft tissue occurs, especially in the groove area which involves the CBD[5].
In groove carcinoma, the macroscopic pathology is similar to that of groove pancreatitis while the pancreatic tissue has the same histology as that of pancreatic adenocarcinoma[6,20,30,38].
TREATMENT
Conservative treatment is the main option in the acute phase of the disease, including analgesia and parenteral nutrition. In some patients, enteral nutrition is not always possible due to the presence of duodenal stenosis[17]. The main therapeutic option for these patients is a surgical approach in benign as well as in malignant diseases of the groove, as shown in Tables 1-12. The most frequent surgical approach is a pylorus-preserving pancreaticoduodenectomy or a Whipple procedure; in a limited number of patients, a gastrointestinal by-pass, with or without biliary by-pass, has been carried out. More recently, a new approach has been reported by Egorov et al[70]; these authors have described a new surgical approach carried out on two patients who were successfully treated by two modifications of a pancreas-preserving duodenal resection with reimplantation of the bile and pancreatic ducts into the neoduodenum (Figure 8). The authors have claimed that these two cases are a good example of a pancreas-preserving approach to duodenal dystrophy treatment and that the technique may be an alternative to the Whipple procedure in cases of mild changes of the orthotopic gland.
Figure 8.
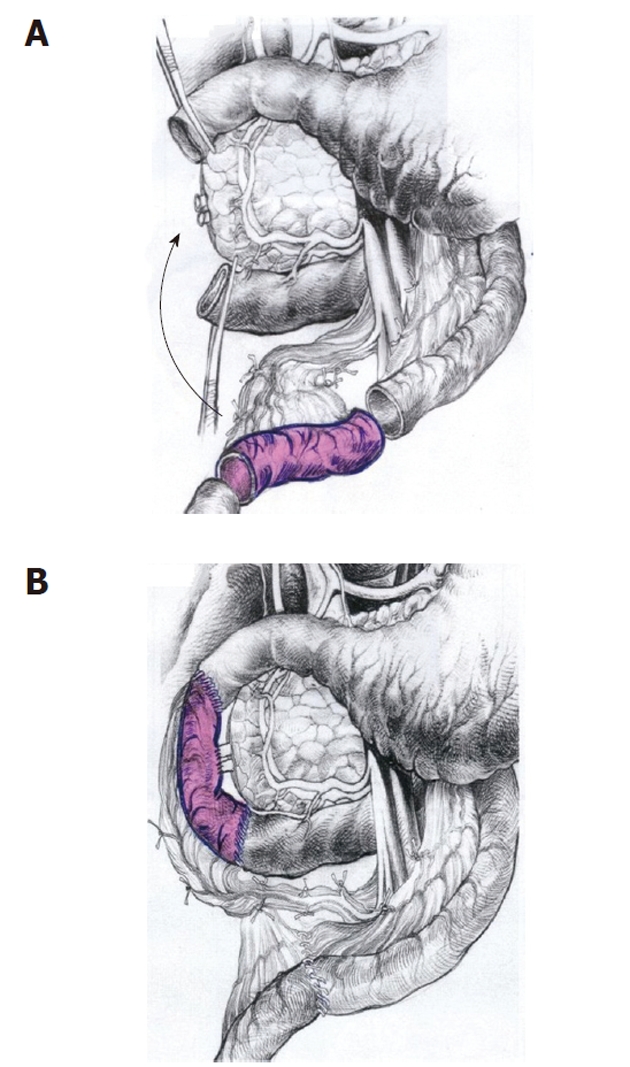
New surgical option for patients having cystic dystrophy of duodenal wall. A: Scheme of the pancreas-preserving resection of the second portion of the duodenum. The second part of the duodenum, including the main papilla, is removed and the segment of the proximal jejunum supplied by the artery and vein is cut out and prepared for transposition between the 1st and 3rd portions of the duodenum; B: The shifted segment is interposed between the 1st and the 3rd parts of the duodenum. Jejuno-jejuno- and duodeno-jejuno-anastomoses are performed. The bile and the pancreatic ducts were implanted in the neodudenum 4 cm below the proximal duodeno-jejuno-anastomosis (from Egorov et al[70] with the kind permission of the authors).
Only in a few cases was a medical approach carried out (see Case 1 of our three patients), mainly because the patients refused surgery, and also in one patient in whom successful treatment for groove pancreatitis was carried out by endoscopic drainage via the minor papilla[33].
THE FATE OF PATIENTS
The first important question arising from the studies analyzed is the extreme length of time necessary from the onset of the symptoms to reach a diagnosis in patients with groove pancreatitis: it varies from a few days to ten years (Tables 1-8). In one of the larger studies in this field, such as that of Rebours et al[40], the mean time from the appearance of the symptoms and the diagnosis is 1 year with a range of 0 to 24 mo. This long time period is similar to that previously reported in chronic pancreatitis[83]. In patients with groove adenocarcinoma, we have no information on time to diagnosis. The perioperative mortality rate seems to be negligible, the only death being reported by Babál et al[79]. In the only study reporting this information (Tables 1-8), the mortality rate was 8.9% (9/101) in the follow-up period in patients with benign disease. However, this information should be taken with caution because, as previously stated, the follow-up period is not quite as long in the majority of studies.
CONCLUSION
The diagnosis of cystic dystrophy of the duodenal wall can be easily assessed by MDCT, MRI and EUS. These latter two techniques may also add more information on the involvement of the part of the pancreatic gland not involved in the duodenal malformation.
Chronic pancreatitis involving the entire pancreatic gland is present in half the patients with cystic dystrophy of the duodenal wall, and the pancreatitis has calcifications in the majority of them. We have no information about exocrine function in these patients and this topic requires additional study. In subjects without pancreatitis, the patients with cystic dystrophy of the duodenal wall are usually in satisfactory general condition after surgical treatment and they regain weight after surgery.
The fact that only two children have been reported to have cystic dystrophy of the duodenal wall confirms the hypothesis that pancreatic and biliary diseases develop over a long period of time.
ACKNOWLEDGMENTS
The authors wish to thank Mr. Paolo Bassi of the Surgical Department, Dr. Maurizio Zani and Dr. Maurizio Iorio of the University of Bologna Clinical Library at Sant’Orsola-Malpighi Hospital for their technical assistance.
Footnotes
Peer reviewer: José Julián calvo Andrés, Department of Physiolgy and Pharmacology, University of Salamanca, Edificio Departamentl, Plaza de los Doctores de la Reina, Campus Miguel de Unamuno. 37007 Salamanca, Spain
S- Editor Tian L L- Editor O’Neill M E- Editor Zhang DN
References
- 1.Potet F, Duclert N. [Cystic dystrophy on aberrant pancreas of the duodenal wall] Arch Fr Mal App Dig. 1970;59:223–238. [PubMed] [Google Scholar]
- 2.Leger L, Lemaigre G, Lenriot JP. [Cysts on heterotopic pancreas of the duodenal wall] Nouv Presse Med. 1974;3:2309–2314. [PubMed] [Google Scholar]
- 3.Vankemmel M, Paris JC, Houcke M, Laurent JC, Burzynski A. [Paraduodenal cysts near Vater’s ampulla and chronic pancreatitis] Med Chir Dig. 1975;4:181–185. [PubMed] [Google Scholar]
- 4.Becker V, Mischke U. Groove pancreatitis. Int J Pancreatol. 1991;10:173–182. doi: 10.1007/BF02924155. [DOI] [PubMed] [Google Scholar]
- 5.Adsay NV, Zamboni G. Paraduodenal pancreatitis: a clinico-pathologically distinct entity unifying “cystic dystrophy of heterotopic pancreas”, “para-duodenal wall cyst”, and “groove pancreatitis”. Semin Diagn Pathol. 2004;21:247–254. doi: 10.1053/j.semdp.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Ishigami K, Tajima T, Nishie A, Kakihara D, Fujita N, Asayama Y, Ushijima Y, Irie H, Nakamura M, Takahata S, et al. Differential diagnosis of groove pancreatic carcinomas vs. groove pancreatitis: usefulness of the portal venous phase. Eur J Radiol. 2010;74:e95–e100. doi: 10.1016/j.ejrad.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 7.Stolte M, Weiss W, Volkholz H, Rösch W. A special form of segmental pancreatitis: “groove pancreatitis”. Hepatogastroenterology. 1982;29:198–208. [PubMed] [Google Scholar]
- 8.Lai EC, Tompkins RK. Heterotopic pancreas. Review of a 26 year experience. Am J Surg. 1986;151:697–700. doi: 10.1016/0002-9610(86)90045-0. [DOI] [PubMed] [Google Scholar]
- 9.Tio TL, Luiken GJ, Tytgat GN. Endosonography of groove pancreatitis. Endoscopy. 1991;23:291–293. doi: 10.1055/s-2007-1010691. [DOI] [PubMed] [Google Scholar]
- 10.Yamaguchi K, Tanaka M. Groove pancreatitis masquerading as pancreatic carcinoma. Am J Surg. 1992;163:312–316; discussion 317-318. doi: 10.1016/0002-9610(92)90009-g. [DOI] [PubMed] [Google Scholar]
- 11.Fléjou JF, Potet F, Molas G, Bernades P, Amouyal P, Fékété F. Cystic dystrophy of the gastric and duodenal wall developing in heterotopic pancreas: an unrecognised entity. Gut. 1993;34:343–347. doi: 10.1136/gut.34.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Itoh S, Yamakawa K, Shimamoto K, Endo T, Ishigaki T. CT findings in groove pancreatitis: correlation with histopathological findings. J Comput Assist Tomogr. 1994;18:911–915. doi: 10.1097/00004728-199411000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Fékété F, Noun R, Sauvanet A, Fléjou JF, Bernades P, Belghiti J. Pseudotumor developing in heterotopic pancreas. World J Surg. 1996;20:295–298. doi: 10.1007/s002689900047. [DOI] [PubMed] [Google Scholar]
- 14.Fujita N, Shirai Y, Tsukada K, Kurosaki I, Iiai T, Hatakeyama K. Groove pancreatitis with recurrent duodenal obstruction. Report of a case successfully treated with pylorus-preserving pancreaticoduodenectomy. Int J Pancreatol. 1997;21:185–188. [PubMed] [Google Scholar]
- 15.Behrens R, Lang T, Muschweck H, Richter T, Hofbeck M. Percutaneous endoscopic gastrostomy in children and adolescents. J Pediatr Gastroenterol Nutr. 1997;25:487–491. doi: 10.1097/00005176-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Procacci C, Graziani R, Zamboni G, Cavallini G, Pederzoli P, Guarise A, Bogina G, Biasiutti C, Carbognin G, Bergamo-Andreis IA, et al. Cystic dystrophy of the duodenal wall: radiologic findings. Radiology. 1997;205:741–747. doi: 10.1148/radiology.205.3.9393530. [DOI] [PubMed] [Google Scholar]
- 17.Shudo R, Obara T, Tanno S, Fujii T, Nishino N, Sagawa M, Ura H, Kohgo Y. Segmental groove pancreatitis accompanied by protein plugs in Santorini’s duct. J Gastroenterol. 1998;33:289–294. doi: 10.1007/s005350050086. [DOI] [PubMed] [Google Scholar]
- 18.Irie H, Honda H, Kuroiwa T, Hanada K, Yoshimitsu K, Tajima T, Jimi M, Yamaguchi K, Masuda K. MRI of groove pancreatitis. J Comput Assist Tomogr. 1998;22:651–655. doi: 10.1097/00004728-199807000-00027. [DOI] [PubMed] [Google Scholar]
- 19.Arrivé L, Saint-Maurice JP. CT features of cystic dystrophy of the duodenal wall. Radiology. 1998;208:830–831. doi: 10.1148/radiology.208.3.830-b. [DOI] [PubMed] [Google Scholar]
- 20.Suehara N, Mizumoto K, Kusumoto M, Niiyama H, Ogawa T, Yamaguchi K, Yokohata K, Tanaka M. Telomerase activity detected in pancreatic juice 19 months before a tumor is detected in a patient with pancreatic cancer. Am J Gastroenterol. 1998;93:1967–1971. doi: 10.1111/j.1572-0241.1998.00557.x. [DOI] [PubMed] [Google Scholar]
- 21.Rubay R, Bonnet D, Gohy P, Laka A, Deltour D. Cystic dystrophy in heterotopic pancreas of the duodenal wall: medical and surgical treatment. Acta Chir Belg. 1999;99:87–91. [PubMed] [Google Scholar]
- 22.Balachandar TG, Surendran R, Kannan D, Darwin P, Jeswanth S. Groove pancreatitis. Trop Gastroenterol. 1999;20:78–79. [PubMed] [Google Scholar]
- 23.Vullierme MP, Vilgrain V, Fléjou JF, Zins M, O’Toole D, Ruszniewski P, Belghiti J, Menu Y. Cystic dystrophy of the duodenal wall in the heterotopic pancreas: radiopathological correlations. J Comput Assist Tomogr. 2000;24:635–643. doi: 10.1097/00004728-200007000-00023. [DOI] [PubMed] [Google Scholar]
- 24.Ito K, Koike S, Matsunaga N. MR imaging of pancreatic diseases. Eur J Radiol. 2001;38:78–93. doi: 10.1016/s0720-048x(01)00293-5. [DOI] [PubMed] [Google Scholar]
- 25.Mohl W, Hero-Gross R, Feifel G, Kramann B, Püschel W, Menges M, Zeitz M. Groove pancreatitis: an important differential diagnosis to malignant stenosis of the duodenum. Dig Dis Sci. 2001;46:1034–1038. doi: 10.1023/a:1010710011767. [DOI] [PubMed] [Google Scholar]
- 26.Munthali Lovemore CE, Hsu JT, Chiu CT, Chen HM, Chen MF. Groove pancreatitis: case report and literature review. Chang Gung Med J. 2001;24:512–516. [PubMed] [Google Scholar]
- 27.Indinnimeo M, Cicchini C, Stazi A, Ghini C, Laghi A, Memeo L, Iannaccone R, Teneriello FL, Mingazzini PL. Duodenal pancreatic heterotopy diagnosed by magnetic resonance cholangiopancreatography: report of a case. Surg Today. 2001;31:928–931. doi: 10.1007/s005950170038. [DOI] [PubMed] [Google Scholar]
- 28.Shudo R, Yazaki Y, Sakurai S, Uenishi H, Yamada H, Sugawara K, Okamura M, Yamaguchi K, Terayama H, Yamamoto Y. Groove pancreatitis: report of a case and review of the clinical and radiologic features of groove pancreatitis reported in Japan. Intern Med. 2002;41:537–542. doi: 10.2169/internalmedicine.41.537. [DOI] [PubMed] [Google Scholar]
- 29.Glaser M, Roskar Z, Skalicky M, Krajnc I. Cystic dystrophy of the duodenal wall in a heterotopic pancreas. Wien Klin Wochenschr. 2002;114:1013–1016. [PubMed] [Google Scholar]
- 30.Gabata T, Kadoya M, Terayama N, Sanada J, Kobayashi S, Matsui O. Groove pancreatic carcinomas: radiological and pathological findings. Eur Radiol. 2003;13:1679–1684. doi: 10.1007/s00330-002-1743-1. [DOI] [PubMed] [Google Scholar]
- 31.Hwang JY, Park KS, Cho KB, Hwang JS, Ahn SH, Park SK, Kwon JH. Segmental groove pancreatitis: report of one case. Korean J Intern Med. 2003;18:234–237. doi: 10.3904/kjim.2003.18.4.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jovanovic I, Knezevic S, Micev M, Krstic M. EUS mini probes in diagnosis of cystic dystrophy of duodenal wall in heterotopic pancreas: a case report. World J Gastroenterol. 2004;10:2609–2612. doi: 10.3748/wjg.v10.i17.2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Isayama H, Kawabe T, Komatsu Y, Sasahira N, Toda N, Tada M, Nakai Y, Yamamoto N, Hirano K, Tsujino T, et al. Successful treatment for groove pancreatitis by endoscopic drainage via the minor papilla. Gastrointest Endosc. 2005;61:175–178. doi: 10.1016/s0016-5107(04)02460-5. [DOI] [PubMed] [Google Scholar]
- 34.Chatelain D, Vibert E, Yzet T, Geslin G, Bartoli E, Manaouil D, Delcenserie R, Brevet M, Dupas JL, Regimbeau JM. Groove pancreatitis and pancreatic heterotopia in the minor duodenal papilla. Pancreas. 2005;30:e92–e95. doi: 10.1097/01.mpa.0000161885.79373.1d. [DOI] [PubMed] [Google Scholar]
- 35.Balzan S, Kianmanesh R, Farges O, Sauvanet A, O’toole D, Levy P, Ruszniewski P, Ogata S, Belghiti J. Right intrahepatic pseudocyst following acute pancreatitis: an unusual location after acute pancreatitis. J Hepatobiliary Pancreat Surg. 2005;12:135–137. doi: 10.1007/s00534-004-0929-0. [DOI] [PubMed] [Google Scholar]
- 36.Pessaux P, Lada P, Etienne S, Tuech JJ, Lermite E, Brehant O, Triau S, Arnaud JP. Duodenopancreatectomy for cystic dystrophy in heterotopic pancreas of the duodenal wall. Gastroenterol Clin Biol. 2006;30:24–28. doi: 10.1016/s0399-8320(06)73073-1. [DOI] [PubMed] [Google Scholar]
- 37.Jouannaud V, Coutarel P, Tossou H, Butel J, Vitte RL, Skinazi F, Blazquez M, Hagège H, Bories C, Rocher P, et al. Cystic dystrophy of the duodenal wall associated with chronic alcoholic pancreatitis. Clinical features, diagnostic procedures and therapeutic management in a retrospective multicenter series of 23 patients. Gastroenterol Clin Biol. 2006;30:580–586. doi: 10.1016/s0399-8320(06)73231-6. [DOI] [PubMed] [Google Scholar]
- 38.Tan CH, Chow PK, Thng CH, Chung AY, Wong WK. Pancreatic adenocarcinoma that mimics groove pancreatitis: case report of a diagnostic dilemma. Dig Dis Sci. 2006;51:1294–1296. doi: 10.1007/s10620-006-8052-5. [DOI] [PubMed] [Google Scholar]
- 39.Tison C, Regenet N, Meurette G, Mirallié E, Cassagnau E, Frampas E, Le Borgne J. Cystic dystrophy of the duodenal wall developing in heterotopic pancreas: report of 9 cases. Pancreas. 2007;34:152–156. doi: 10.1097/01.mpa.0000246669.61246.08. [DOI] [PubMed] [Google Scholar]
- 40.Rebours V, Lévy P, Vullierme MP, Couvelard A, O’Toole D, Aubert A, Palazzo L, Sauvanet A, Hammel P, Maire F, et al. Clinical and morphological features of duodenal cystic dystrophy in heterotopic pancreas. Am J Gastroenterol. 2007;102:871–879. doi: 10.1111/j.1572-0241.2007.01091.x. [DOI] [PubMed] [Google Scholar]
- 41.Klöppel G. Chronic pancreatitis, pseudotumors and other tumor-like lesions. Mod Pathol. 2007;20 Suppl 1:S113–S131. doi: 10.1038/modpathol.3800690. [DOI] [PubMed] [Google Scholar]
- 42.Blasbalg R, Baroni RH, Costa DN, Machado MC. MRI features of groove pancreatitis. AJR Am J Roentgenol. 2007;189:73–80. doi: 10.2214/AJR.06.1244. [DOI] [PubMed] [Google Scholar]
- 43.Sanada Y, Yoshida K, Itoh H, Kunita S, Jinushi K, Matsuura H. Groove pancreatitis associated with true pancreatic cyst. J Hepatobiliary Pancreat Surg. 2007;14:401–409. doi: 10.1007/s00534-006-1180-7. [DOI] [PubMed] [Google Scholar]
- 44.Balakrishnan V, Chatni S, Radhakrishnan L, Narayanan VA, Nair P. Groove pancreatitis: a case report and review of literature. JOP. 2007;8:592–597. [PubMed] [Google Scholar]
- 45.Siddiqi AJ, Miller F. Chronic pancreatitis: ultrasound, computed tomography, and magnetic resonance imaging features. Semin Ultrasound CT MR. 2007;28:384–394. doi: 10.1053/j.sult.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 46.Rahman SH, Verbeke CS, Gomez D, McMahon MJ, Menon KV. Pancreatico-duodenectomy for complicated groove pancreatitis. HPB (Oxford) 2007;9:229–234. doi: 10.1080/13651820701216430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Castell-Monsalve FJ, Sousa-Martin JM, Carranza-Carranza A. Groove pancreatitis: MRI and pathologic findings. Abdom Imaging. 2008;33:342–348. doi: 10.1007/s00261-007-9245-x. [DOI] [PubMed] [Google Scholar]
- 48.Lopez-Pelaez MS, Hoyos FB, Isidro MG, Unzurrunzaga EA, Lopez Ede V, Collazo YQ. Cystic dystrophy of heterotopic pancreas in stomach: radiologic and pathologic correlation. Abdom Imaging. 2008;33:391–394. doi: 10.1007/s00261-007-9275-4. [DOI] [PubMed] [Google Scholar]
- 49.Lenhart DK, Balthazar EJ. MDCT of acute mild (nonnecrotizing) pancreatitis: abdominal complications and fate of fluid collections. AJR Am J Roentgenol. 2008;190:643–649. doi: 10.2214/AJR.07.2761. [DOI] [PubMed] [Google Scholar]
- 50.de Tejada AH, Chennat J, Miller F, Stricker T, Matthews J, Waxman I. Endoscopic and EUS features of groove pancreatitis masquerading as a pancreatic neoplasm. Gastrointest Endosc. 2008;68:796–798. doi: 10.1016/j.gie.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 51.Stefanescu C, Vullierme MP, Couvelard A, Bretagnol F, Amouyal P, Maire F, Rebours V, Hammel P, Ruszniewski P, Lévy P. Cystic dystrophy in gastric heterotopic pancreas complicated by intracystic hemorrhage and fistulisation in the stomach - a pediatric case. Gastroenterol Clin Biol. 2008;32:645–648. doi: 10.1016/j.gcb.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 52.Jovanovic I, Alempijevic T, Lukic S, Knezevic S, Popovic D, Dugalic V, Micev M, Krstic M. Cystic dystrophy in heterotopic pancreas of the duodenal wall. Dig Surg. 2008;25:262–268. doi: 10.1159/000148133. [DOI] [PubMed] [Google Scholar]
- 53.Varma V, Gandhi V, Bheerappa N, Sastry RA. Groove pancreatitis mimicking pancreatic malignancy. Indian J Gastroenterol. 2008;27:86. [PubMed] [Google Scholar]
- 54.Galloro G, Napolitano V, Magno L, Diamantis G, Nardone G, Bruno M, Mollica C, Persico G. Diagnosis and therapeutic management of cystic dystrophy of the duodenal wall in heterotopic pancreas. A case report and revision of the literature. JOP. 2008;9:725–732. [PubMed] [Google Scholar]
- 55.Galloro G, Napolitano V, Magno L, Diamantis G, Pastore A, Mosella F, Donisi M, Ruggiero S, Pascariello A, Bruno M, et al. Pancreaticoduodenectomy as the primary therapeutic choice in cystic dystrophy of the duodenal wall in heterotopic pancreas. Chir Ital. 2008;60:835–841. [PubMed] [Google Scholar]
- 56.Kwak SW, Kim S, Lee JW, Lee NK, Kim CW, Yi MS, Kim GH, Kang DH. Evaluation of unusual causes of pancreatitis: role of cross-sectional imaging. Eur J Radiol. 2009;71:296–312. doi: 10.1016/j.ejrad.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 57.Frulloni L, Gabbrielli A, Pezzilli R, Zerbi A, Cavestro GM, Marotta F, Falconi M, Gaia E, Uomo G, Maringhini A, et al. Chronic pancreatitis: report from a multicenter Italian survey (PanCroInfAISP) on 893 patients. Dig Liver Dis. 2009;41:311–317. doi: 10.1016/j.dld.2008.07.316. [DOI] [PubMed] [Google Scholar]
- 58.Triantopoulou C, Dervenis C, Giannakou N, Papailiou J, Prassopoulos P. Groove pancreatitis: a diagnostic challenge. Eur Radiol. 2009;19:1736–1743. doi: 10.1007/s00330-009-1332-7. [DOI] [PubMed] [Google Scholar]
- 59.Thomas H, Marriott P, Portmann B, Heaton N, Rela M. Cystic dystrophy in heterotopic pancreas: a rare indication for pancreaticoduodenectomy. Hepatobiliary Pancreat Dis Int. 2009;8:215–217. [PubMed] [Google Scholar]
- 60.Shanbhogue AK, Fasih N, Surabhi VR, Doherty GP, Shanbhogue DK, Sethi SK. A clinical and radiologic review of uncommon types and causes of pancreatitis. Radiographics. 2009;29:1003–1026. doi: 10.1148/rg.294085748. [DOI] [PubMed] [Google Scholar]
- 61.Levenick JM, Gordon SR, Sutton JE, Suriawinata A, Gardner TB. A comprehensive, case-based review of groove pancreatitis. Pancreas. 2009;38:e169–e175. doi: 10.1097/MPA.0b013e3181ac73f1. [DOI] [PubMed] [Google Scholar]
- 62.Yoshida N, Nakayama H, Hemmi A, Suzuki T, Takayama T. Duodenal stenosis caused by cystic dystrophy in heterotopic pancreas: report of a case. Surg Today. 2009;39:803–806. doi: 10.1007/s00595-009-3939-3. [DOI] [PubMed] [Google Scholar]
- 63.Casetti L, Bassi C, Salvia R, Butturini G, Graziani R, Falconi M, Frulloni L, Crippa S, Zamboni G, Pederzoli P. “Paraduodenal” pancreatitis: results of surgery on 58 consecutives patients from a single institution. World J Surg. 2009;33:2664–2669. doi: 10.1007/s00268-009-0238-5. [DOI] [PubMed] [Google Scholar]
- 64.Meesiri S. Groove pancreatitis: report of one case in Thailand. J Med Assoc Thai. 2009;92:1554–1559. [PubMed] [Google Scholar]
- 65.Funamizu N, Aramaki M, Matsumoto T, Inomata M, Shibata K, Himeno Y, Yada K, Hirano S, Sasaki A, Kawano K, et al. Groove pancreatic carcinoma. Hepatogastroenterology. 2009;56:1742–1744. [PubMed] [Google Scholar]
- 66.Viñolo Ubiña C, Morales Ruiz J, Heredia Carrasco C, Ruiz-Cabello Jiménez M, Villegas Herrera MT, Garrote Lara D. Groove pancreatitis with duodenal stenosis. Rev Esp Enferm Dig. 2010;102:59–60. doi: 10.4321/s1130-01082010000100012. [DOI] [PubMed] [Google Scholar]
- 67.Tezuka K, Makino T, Hirai I, Kimura W. Groove pancreatitis. Dig Surg. 2010;27:149–152. doi: 10.1159/000289099. [DOI] [PubMed] [Google Scholar]
- 68.Sunnapwar A, Prasad SR, Menias CO, Shanbhogue AK, Katre R, Raut A. Nonalcoholic, nonbiliary pancreatitis: cross-sectional imaging spectrum. AJR Am J Roentgenol. 2010;195:67–75. doi: 10.2214/AJR.09.4048. [DOI] [PubMed] [Google Scholar]
- 69.Lee TH, Park SH, Lee CK, Chung IK, Kim SJ. Ectopic opening of the common bile duct accompanied by groove pancreatitis: diagnosis with magnetic resonance cholangiopancreatography. Gastrointest Endosc. 2010;71:1301–1302. doi: 10.1016/j.gie.2009.12.052. [DOI] [PubMed] [Google Scholar]
- 70.Egorov VI, Butkevich AC, Sazhin AV, Yashina NI, Bogdanov SN. Pancreas-preserving duodenal resections with bile and pancreatic duct replantation for duodenal dystrophy. Two case reports. JOP. 2010;11:446–452. [PubMed] [Google Scholar]
- 71.Lee TH, Park SH, Lee CK, Lee SH, Chung IK, Kim SJ, Kim SW. Ampulla of Vater metastasis from recurrent uterine cervix carcinoma presenting as groove pancreatitis. Gastrointest Endosc. 2011;73:362–363. doi: 10.1016/j.gie.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 72.German V, Ekmektzoglou KA, Kyriakos N, Patouras P, Kikilas A. Pancreatitis of the gastroduodenal groove: a case report. Case Report Med. 2010;2010:329587. doi: 10.1155/2010/329587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rana SS, Bhasin DK, Chandail VS, Gupta R, Nada R, Kang M, Nagi B, Singh R, Singh K. Endoscopic balloon dilatation without fluoroscopy for treating gastric outlet obstruction because of benign etiologies. Surg Endosc. 2011;25:1579–1584. doi: 10.1007/s00464-010-1442-y. [DOI] [PubMed] [Google Scholar]
- 74.Bill K, Belber JP, Carson JW. Adenomyoma (pancreatic heterotopia) of the duodenum producing common bile duct obstruction. Gastrointest Endosc. 1982;28:182–184. doi: 10.1016/s0016-5107(82)73049-4. [DOI] [PubMed] [Google Scholar]
- 75.Holstege A, Barner S, Brambs HJ, Wenz W, Gerok W, Farthmann EH. Relapsing pancreatitis associated with duodenal wall cysts. Diagnostic approach and treatment. Gastroenterology. 1985;88:814–819. doi: 10.1016/0016-5085(85)90157-x. [DOI] [PubMed] [Google Scholar]
- 76.Flaherty MJ, Benjamin DR. Multicystic pancreatic hamartoma: a distinctive lesion with immunohistochemical and ultrastructural study. Hum Pathol. 1992;23:1309–1312. doi: 10.1016/0046-8177(92)90301-i. [DOI] [PubMed] [Google Scholar]
- 77.Izbicki JR, Knoefel WT, Müller-Höcker J, Mandelkow HK. Pancreatic hamartoma: a benign tumor of the pancreas. Am J Gastroenterol. 1994;89:1261–1262. [PubMed] [Google Scholar]
- 78.Wu SS, Vargas HI, French SW. Pancreatic hamartoma with Langerhans cell histiocytosis in a draining lymph node. Histopathology. 1998;33:485–487. doi: 10.1046/j.1365-2559.1998.0491c.x. [DOI] [PubMed] [Google Scholar]
- 79.Babál P, Zaviacic M, Danihel L. Evidence that adenomyoma of the duodenum is ectopic pancreas. Histopathology. 1998;33:487–488. doi: 10.1046/j.1365-2559.1998.0491d.x. [DOI] [PubMed] [Google Scholar]
- 80.McFaul CD, Vitone LJ, Campbell F, Azadeh B, Hughes ML, Garvey CJ, Ghaneh P, Neoptolemos JP. Pancreatic hamartoma. Pancreatology. 2004;4:533–537; discussion 537-538. doi: 10.1159/000080528. [DOI] [PubMed] [Google Scholar]
- 81.Aoun N, Zafatayeff S, Smayra T, Haddad-Zebouni S, Tohmé C, Ghossain M. Adenomyoma of the ampullary region: imaging findings in four patients. Abdom Imaging. 2005;30:86–89. doi: 10.1007/s00261-004-0224-1. [DOI] [PubMed] [Google Scholar]
- 82.Petrone MC, Arcidiacono PG, Testoni PA. Endoscopic ultrasonography for evaluating patients with recurrent pancreatitis. World J Gastroenterol. 2008;14:1016–1022. doi: 10.3748/wjg.14.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pezzilli R, Morselli Labate AM, Ceciliato R, Frulloni L, Cavestro GM, Comparato G, Ferri B, Corinaldesi R, Gullo L. Quality of life in patients with chronic pancreatitis. Dig Liver Dis. 2005;37:181–189. doi: 10.1016/j.dld.2004.10.007. [DOI] [PubMed] [Google Scholar]


