Abstract
Extraction of large pancreatic and common bile duct (CBD) calculi has always challenged the therapeutic endoscopist. Extracorporeal shockwave lithotripsy (ESWL) is an excellent tool for patients with large pancreatic and CBD calculi that are not amenable to routine endotherapy. Pancreatic calculi in the head and body are targeted by ESWL, with an aim to fragment them to < 3 mm diameter so that they can be extracted by subsequent endoscopic retrograde cholangiopancreatography (ERCP). In our experience, complete clearance of the pancreatic duct was achieved in 76% and partial clearance in 17% of 1006 patients. Short-term pain relief with reduction in the number of analgesics ingested was seen in 84% of these patients. For large CBD calculi, a nasobiliary tube is placed to help target the calculi, as well as bathe the calculi in saline - a simple maneuver which helps to facilitate fragmentation. The aim is to fragment calculi to < 5 mm size and clear the same during ERCP. Complete clearance of the CBD was achieved in 84.4% of and partial clearance in 12.3% of 283 patients. More than 90% of the patients with pancreatic and biliary calculi needed three or fewer sessions of ESWL with 5000 shocks being delivered at each session. The use of epidural anesthesia helped in reducing patient movement. This, together with the better focus achieved with newer third-generation lithotripters, prevents collateral tissue damage and minimizes the complications. Complications in our experience with nearly 1300 patients were minimal, and no extension of hospital stay was required. Similar rates of clearance of pancreatic and biliary calculi with minimal adverse effects have been reported from the centers where ESWL is performed regularly. In view of its high efficiency, non-invasive nature and low complication rates, ESWL can be offered as the first-line therapy for selected patients with large pancreatic and CBD calculi.
Keywords: Pancreatic calculi, Extracorporeal shockwave lithotripsy, Common bile duct calculi
INTRODUCTION
Extracorporeal shock wave lithotripsy (ESWL) was first introduced in the 1980s for the fragmentation of renal and ureteric calculi[1]. Its application was quickly extended to include large biliary and pancreatic calculi. Over the past three decades, it has been utilized at many centers worldwide for fragmentation of biliary and pancreatic calculi that are not amenable to routine endotherapy[2-16]. In this review, we briefly highlight the principles of ESWL as well as its place in therapy of biliary and pancreatic calculi.
PRINCIPLES OF ESWL
ESWL is based on the principle of shock wave energy. Whenever energy is abruptly released in an enclosed space, shock waves are generated. The passage of these shock waves through substances of different acoustic impedance generates compressive stress on the boundary surface. This stress eventually overcomes the tensile strength of the object (in the present case, biliary and pancreatic calculi) and the anterior surface of the calculi crumbles as a result. The shock waves cross to the posterior surface of the calculi and some of them are reflected back and cause further fragmentation[17] (Figure 1). Modern lithotripsy machines consist of the following basic components.
Figure 1.
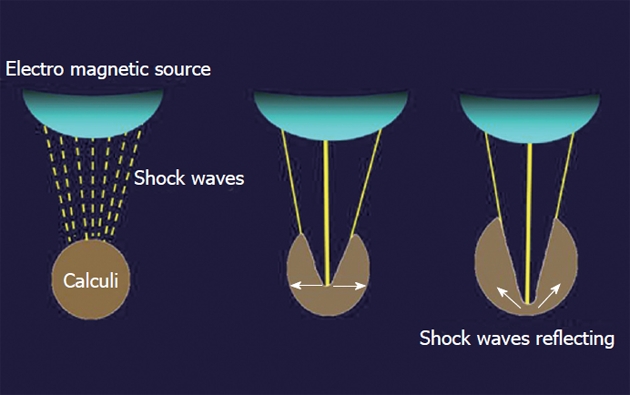
Principle of extracorporeal shockwave lithotripsy. Shockwaves from the source are targeted on the calculi and these induce fragmentation.
Shock wave generator
The earlier generation lithotripter utilized electrohydraulic energy or piezoelectric crystals for shock wave generation. The newer third-generation lithotripter utilizes the principle of electromagnetic shock wave generation from an electromagnetic coil. These shock waves are focused on a target (calculi) using an acoustic lens or cylindrical reflector.
Focusing system
Shock waves are focused to the focal point or target in the body. This focal path is conical in shape and all the waves are concentrated at the apex of the cone, which is called the focal point. During ESWL, the focal point targets the calculi. Targeted focusing reduces collateral tissue damage and minimizes the complications.
Localization
Localization of the calculi is basically done by fluoroscopy or ultrasound. All the newer lithotripters are equipped with both these facilities.
Coupling device
The generated shockwaves are transmitted via a coupling device, to the skin surface and then through the body tissue to the calculi. The earlier lithotripters used a “water bath” for this purpose. The newer machines use a small water-filled cushion covered with a silicone membrane to transmit the shock waves to the patient’s skin.
ESWL FOR PANCREATIC CALCULI
Chronic calcific pancreatitis (CCP) is a disease of varied etiology that is associated with the development of pancreatic ductal calculi, which result in upstream hypertension, increased parenchymal pressure, and ischemia. Pain is the dominant feature of both alcoholic and non-alcoholic CCP. Decompression of the duct by clearing the stones leads to relief of pain in many patients. Small pancreatic duct (PD) stones can be extracted by the routine technique of endoscopic pancreatic sphincterotomy and basketing. Stones > 5 mm in diameter are often impacted in the main pancreatic duct and require fragmentation to facilitate their expulsion[15]. ESWL has been successfully used at many centers for fragmentation of large PD calculi followed by spontaneous or endoscopic clearance with resultant relief in pain[7-15].
Indications and contraindications
ESWL is indicated in all patients of CCP with large PD calculi (> 5 mm) that are not amenable to routine endotherapy - where pain is the predominant symptom. The aim is to break the calculi to fragments of ≤ 3 mm, so that they can be removed by subsequent endoscopic retrograde cholangiopancreatography (ERCP). Calculi in the head and body are targeted during ESWL.
ESWL is not indicated in patients with extensive calculi in the head, body and tail of the pancreas, or in patients with isolated calculi in the tail area because of increased chance of collateral damage to the spleen are high. Patients with multiple stricture, head mass, pancreatic ascites or pseudocysts are not treated by ESWL. Cholangitis or coagulopathy due to biliary stricture are treated before subjecting the patient to ESWL.
Procedure protocol
The protocol followed for ESWL of pancreatic calculi at our institute is depicted in Figure 2.
Figure 2.
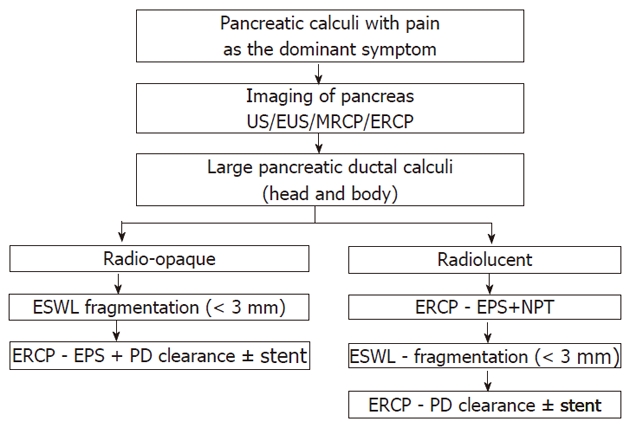
Protocol followed at Asian Institute of Gastroenterology, for extracorporeal shockwave lithotripsy of large pancreatic duct calculi[7]. EPS: Endoscopic pancreatic sphincterotomy; US: Ultrasound; EUS: Endoscopic ultrasound; MRCP: Magnetic resonance cholangiopancreatography; ERCP: Endoscopic retrograde cholangiopancreatography; PD: Pancreatic duct; ESWL: Extracorporeal shock wave lithotripsy; NPT: Naso-pancreatic tube.
A third-generation electromagnetic lithotripter (Delta Compact; Dornier Med Tech, Weissling, Germany.) (Figure 3) is used to deliver a maximum of 5000 shocks are delivered per session. Repeat sessions are carried out on successive days until the stone fragments are < 3 mm in diameter. An intensity of 5-6 (15 000-16 000 kV) on a scale of 1-6 with a frequency of 90 shocks per minute is used for fragmentation[7,8].
Figure 3.
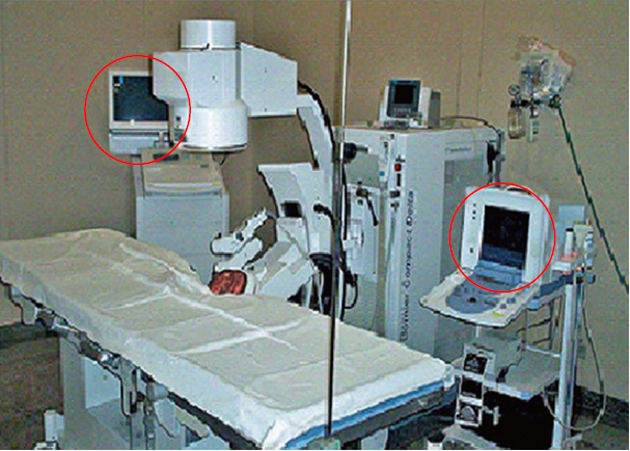
Third-generation lithotripter with fluoroscopic and ultrasound imaging facility.
A few centers have advocated ESWL alone without any subsequent endotherapy for large PD calculi, stating that good fragmentation is followed by spontaneous expulsion of the fragments[18,19]. At our center, ERCP, pancreatic sphincterotomy and pancreatic ductal clearance is always performed after ESWL because of the dense nature of the calculi present in patients with idiopathic chronic pancreatitis[7]. Pancreatic sphincterotomy prior to ESWL is technically challenging because these dense calculi tend to obstruct the pancreatic duct completely and prevent deep cannulation. In our study, the majority of ESWL procedures were carried out under epidural anesthesia (EA)[20]. However, general anesthesia or total intravenous analgesia has also been used for this procedure.
Efficacy and pain relief
Over 95% of our patients require three sessions or fewer of ESWL for adequate fragmentation. In 76% of patients, the PD cleared completely, in 17% partially, and there was clearance failure in the remaining 7%[7] (Table 1 and Figures 4 and 5). Similar results for clearance of the PD, ranging from 37% to 100% have been reported earlier[9]. Comparative efficacy of ESWL for pancreatic calculi is shown in Table 2. Short-term pain relief was seen in 84% of our patients. This experience is also similar to others who have reported short-term pain in 82%-94% of the patients[9,10,21-23]. The results of a large meta-analysis have indicated that ESWL has a significant impact on improvement of pain. The mechanism of pain relief is due to decompression of the main PD following clearance of the obstruction[9]. Pain relief was reflected by decreased use of analgesics and of number of hospitalizations during the follow-up period[7,14] (Table 3). Failure of pain relief, despite adequate clearance could be because of multiple mechanisms of pain in patients of chronic pancreatitis. These include pancreatic inflammation, ischemia, and associated lesions such as duodenal and biliary strictures. Surgery is often considered as the gold standard in the management of chronic pancreatitis. However, even after duodenum-preserving resection of the head of the pancreas, which is considered to be the best surgical approach for chronic pancreatitis, almost 25% of patients experience recurrence of pain[21]. In addition, there is considerable procedure-related morbidity and mortality. ESWL followed by PD clearance on ERCP is therefore increasingly used in the management of CCP, with results that are comparable to surgery[10-12,19].
Table 1.
Details of extracorporeal shockwave lithotripsy in 1006 patients treated at Asian Institute of Gastroenterology
| No. of sessions | n (%) | Shock waves (n) | |
| Mean | Range | ||
| 1 | 292 (29) | 4450 | (4250-4900) |
| 2 | 370 (37) | 9270 | (8800-9940) |
| 3 | 300 (30) | 13 250 | (11 800-14 700) |
| 4 | 32 (3) | 18 900 | (18 100-19 400) |
| ≥ 5 | 12 (1) | 23 550 | (22 100-27 750) |
| Clearance | |||
| Complete cleared | 762 (76) | ||
| Partially cleared | 173 (17) | ||
| Failed clearance | 71 (7) | ||
Figure 4.
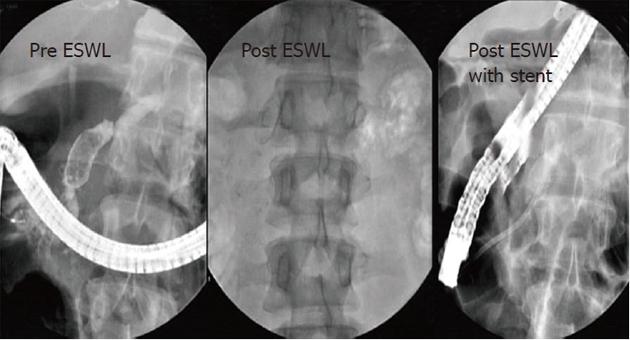
Large pancreatic calculi in head and genu, cleared by extracorporeal shockwave lithotripsy followed by pancreatic stenting. ESWL: Extracorporeal shockwave lithotripsy.
Figure 5.
Large pancreatic calculi in head. Post extracorporeal shockwave lithotripsy (ESWL) reduction in diameter of main pancreatic duct.
Table 2.
Efficacy of extracorporeal shockwave lithotripsy for pancreatic calculi
Table 3.
Pain relief and analgesic use, pre- and post-extracorporeal shockwave lithotripsy[7]
| Post-ESWL | Pre-ESWL | ||||
| (n = 846) | (n = 711) | ||||
| Pain relief VAS (Scale 0-10) | 0 | 326 | P < 0.001 | ||
| 6/10 | 212 | 1/10 | 161 | ||
| 7/10 | 320 | 2/10 | 96 | ||
| 8/10 | 204 | 3/10 | 85 | ||
| 9/10 | 110 | 4/10 | 43 | ||
| Analgesic use Doses/mo | 0 | - | 0 | 326 | P < 0.001 |
| 1-5 | 48 | 1-5 | 258 | ||
| 6-10 | 190 | 6-10 | 127 | ||
| 11-15 | 385 | ||||
| > 15 | 223 | ||||
VAS: Visual analog score; ESWL: Extracorporeal shockwave lithotripsy.
Limitations of ESWL in CCP
Long-term follow-up is necessary to evaluate the role of ESWL in PD clearance of patients with CCP. Data on this issue are conflicting. Although no benefit on glandular function and pain has been reported by some workers[16,24], others have shown a definite improvement in exocrine and endocrine functions[23]. We feel that more long-term follow-up studies are required to define the role of ESWL in pain and exocrine or endocrine dysfunction, as well as the possibility of carcinoma development, which are all potential sequelae of CCP. This is especially true in tropical regions and in patients with idiopathic chronic pancreatitis in whom the disease begins at a young age.
Although the numbers are small, failure of complete fragmentation has been reported at most centers. It would be ideal to identify this set of patients, so that they can be subjected to surgery directly. Yet another limitation is the failure to prevent recurrence following ESWL, which has been reported in 22%-35% of patients[22,24].
In conclusion, ESWL is a good technique for extraction of large PD calculi in patients with CCP and offers good pain relief. It is conceivable that ESWL done at a young age, followed by intensive medical therapy could alter the course of the patients with CCP, besides obviating the need for surgery[8].
ESWL FOR LARGE COMMON BILE DUCT STONES
Conventional therapy for common bile duct (CBD) stones involves endoscopic sphincterotomy and extraction by balloon catheter or Dormia basket. Between 80% and 90% of CBD stones can be extracted using these techniques[4,5,25]. The rest are categorized as difficult CBD stones and include large stones (> 15 mm diameter), impacted stones in patients with narrow distal CBD and/or difficult anatomy. Large stones can either be fragmented or the CBD passage dilated to facilitate extraction. Fragmentation of large CBD stones can be carried out by mechanical lithotripsy, electro hydraulic lithotripsy (EHL)[26], intraductal laser lithotripsy (ILL)[27], spy scope and holmium laser[28], and ESWL. The narrow distal CBD can be subjected to balloon dilatation to facilitate extraction of large calculi[29-31]. Sauerbruch and colleagues first demonstrated the efficacy in achieving CBD stone disintegration successfully and with minimal side effects[8].
Indications and contraindications
ESWL is indicated all patients with large CBD calculi that are not extractable by routine techniques of sphincterotomy followed by basket or balloon trawl. It is especially useful for patients with post-cholecystectomy retained stones, isolated or primary CBD stones, and in those who refuse or are unfit for surgery.
Acute cholangitis and coagulopathy are relative contraindications and ESWL can be performed once these conditions are treated.
Procedure protocol
The majority of CBD calculi are radiolucent. An initial ERCP is performed and a nasobiliary tube (NBT) is placed in the CBD. This is used to opacify the calculi for targeting and fragmentation. It is also used to bathe the stones in saline - a simple technique that aids fragmentation. ESWL is carried out at an intensity of 4 (in a scale of 1-6) corresponding to 11 000-16 000 kV) at a rate of 90 shocks/min. A maximum of 5000 shocks are given per session. The aim is to break the calculi into fragments < 5 mm in diameter for extraction by subsequent ERCP. Stenting is done if clearance is partial or an associated stricture is present. The protocol followed at our institute is shown in Figure 6.
Figure 6.
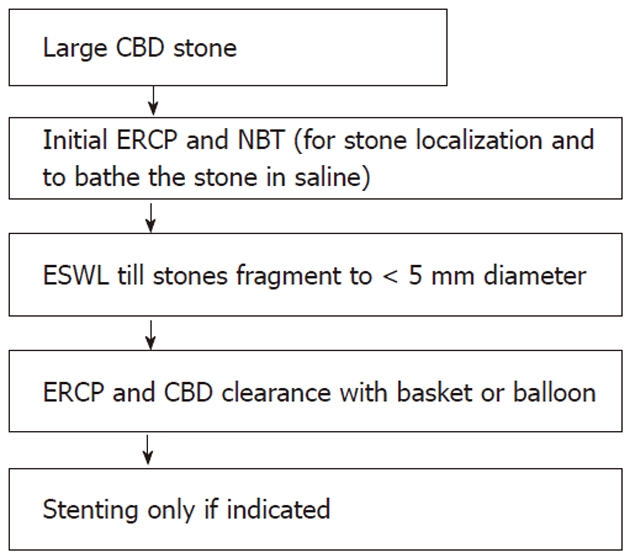
Protocol for extracorporeal shockwave lithotripsy of large common bile duct calculi. CBD: Common bile duct; ERCP: Endoscopic retrograde cholangiopancreatography; NBT: Nasobiliary tube; ESWL: Extracorporeal shockwave lithotripsy.
Efficacy
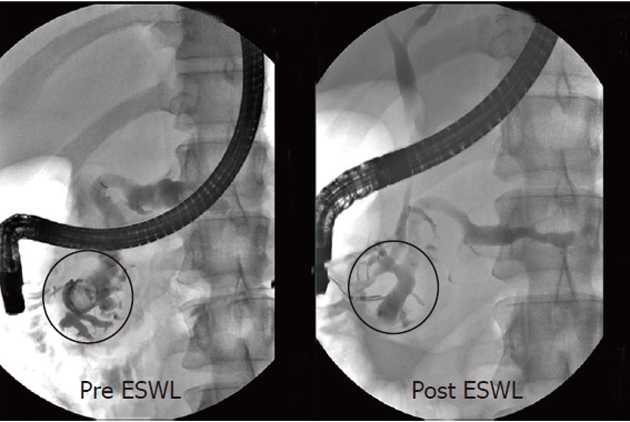
In our experience, complete clearance was achieved in 84.4%, partial in 12.3%, and failure in 3.1% of patients[3] (Figure 7). ESWL was useful in clearing intrahepatic calculi also. Similar successful clearance has been reported at other centers (Table 4). Over 75% of our patients needed ≤ 3 less sessions of ESWL. Clearance of the CBD in patients with post-cholecystectomy calculi or primary CBD calculi by ESWL and subsequent ERCP obviates the need for surgery[3]. ESWL was successful in patients in whom mechanical lithotripsy or surgical extraction of CBD stones was unsuccessful[5]. Non-operative options for removing large CBD calculi include laser lithotripsy, EHL or ESWL. The success rates are similar at between 80% and 95%[6]. No significant differences in CBD clearance was seen in comparison of ESWL with EHL[25]. Laparoscopic CBD exploration (LCBDE) is a well-established technique for management of large CBD stones. Despite several studies supporting LCBDE, current surgical practice suggests an overwhelming preference for preoperative ERCP[33]. Potential explanations for this preference include the challenging nature of LCBDE, lack of necessary equipment, lack of formal training in LCBDE, and increased operative time[34,35].
Figure 7.
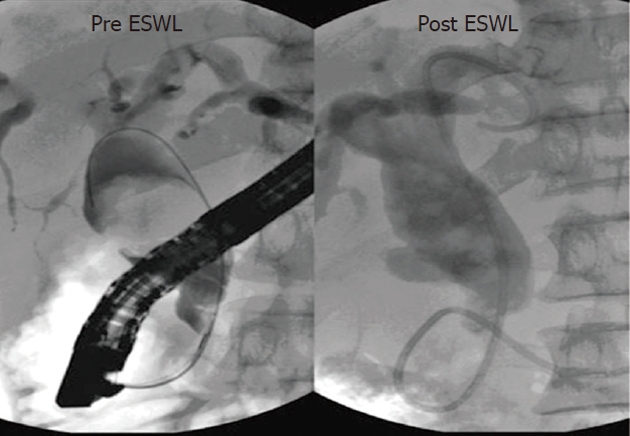
Large common bile duct calculi with narrow distal common bile duct. Good fragmentation achieved with extracorporeal shockwave lithotripsy (ESWL).
Table 4.
Efficacy of extracorporeal shockwave lithotripsy for large common bile duct calculi
Factors that influence fragmentation of CBD stones
Factors that promote better fragmentation and patient compliance have been analyzed at our center[3]: (1) Use of EA. EA provides good sensory block and reduces patient movement[20]. This helps with better targeting and reduces the total number of shocks. The same catheter can be used for three sessions of ESWL, which is often adequate to fragment calculi in the majority of patients; (2) Frequency of shocks at 90/min. At a higher frequency, the ongoing shock waves and those reflected from the surface of the calculus tend to cancel each other out[17]; (3) The presence of fluid around the calculi aids better fragmentation. Saline irrigation via the NBT is carried out during ESWL; and (4) Radiolucent calculi fragment easier compared to radio-opaque ones.
At our center, patients with large CBD calculi undergo ESWL, under EA, at a shock wave frequency of 90/min, with saline irrigation via an NBT. Limitations include failure to prevent recurrence, which is reported around 14% at 1 year following ESWL[36]. The other limitation is failure to identify the calculi that are not amenable to fragmentation, prior to ESWL.
COMPARISON WITH COMPETING STRATEGIES
Mechanical lithotripsy, ILL, EHL and Spy Glass are the other modalities of stone fragmentation for large CBD calculi. Neuhaus et al[27] have reported better clearance with ILL as compared with ESWL, whereas Adamek and colleagues have found no difference between these modalities[25]. The availability of instrumentation and expertise at a center often determines the choice of the procedure adopted at that center. Very few studies have compared different strategies for fragmentation of large CBD stones.
COMPLICATIONS OF ESWL
A number of rare and serious complications have been reported following ESWL[37-40]. These occur infrequently and appear to be limited in number. The complications include perirenal hematoma, biliary obstruction, bowel perforation, splenic rupture, lung trauma, and necrotizing pancreatitis. In our experience, as well as in most of the other centers with high patient volume, complications are minimal and mild, and are managed conservatively without extension of hospital stay[3,7,25,27]. Pain at the site of shock wave delivery, skin ecchymosis, abdominal pain, occasional fever, and hemobilia were observed in some of our patients. No blood transfusion or intervention was required in any of these cases. There is no increased incidence of pancreatitis following ESWL and ERCP. Accurate targeting achieved by the third-generation lithotripter, as well as reduced patient movements with EA, are responsible for reducing collateral tissue damage and minimizing complications[3,7].
AREAS OF FUTURE RESEARCH
Although fragmentation of pancreatic and biliary calculi by ESWL is satisfactory, there is ample scope for future research to improve results and minimize complications. The long-term results of ESWL in CCP, especially in young patients, are yet to be determined. Data on post-ESWL long-term follow-up are conflicting, with no benefit being shown in some studies[16], whereas others have revealed good long-term results[23]. Can intervention at an early age change the course of CCP and help avoid surgery and long-term sequelae[7]? A long term prospective study in this regard would give us a clearer insight. Another focus of research would be to identify the small percentage of pancreatic and biliary calculi that do not respond to ESWL, so that they can be subjected to alternate modes of endoscopic therapy or surgery. An improvement in the focusing and intensity of shock waves would minimize the failure rate as well as help target pancreatic calculi in the tail region while avoiding splenic complications[38,39]. Recurrence of pancreatic and biliary calculi after initial successful clearance is known to occur[22,36]. Identification of this subset of patients and prevention of such recurrences using pharmacological agents would be ideal.
CONCLUSION
ESWL is an excellent therapeutic modality for large pancreatic and CBD calculi. The high efficacy, non-invasive nature of the procedure, along with the low complication rate make it a procedure of choice and can be offered as first-line therapy for selected patients with large pancreatic and CBD calculi.
Footnotes
Peer reviewer: Pete Muscarella, MD, Division of Gastrointestinal Surgery, The Ohio State University, N711 Doan Hall, 410 W. 10th Ave, Columbus, OH 43210, United States
S- Editor Tian L L- Editor Kerr C E- Editor Li JY
References
- 1.Chaussy C, Schmiedt E, Jocham D, Brendel W, Forssmann B, Walther V. First clinical experience with extracorporeally induced destruction of kidney stones by shock waves. J Urol. 1982;127:417–420. doi: 10.1016/s0022-5347(17)53841-0. [DOI] [PubMed] [Google Scholar]
- 2.Sauerbruch T, Stern M. Fragmentation of bile duct stones by extracorporeal shock waves. A new approach to biliary calculi after failure of routine endoscopic measures. Gastroenterology. 1989;96:146–152. doi: 10.1016/0016-5085(89)90775-0. [DOI] [PubMed] [Google Scholar]
- 3.Tandan M, Reddy DN, Santosh D, Reddy V, Koppuju V, Lakhtakia S, Gupta R, Ramchandani M, Rao GV. Extracorporeal shock wave lithotripsy of large difficult common bile duct stones: efficacy and analysis of factors that favor stone fragmentation. J Gastroenterol Hepatol. 2009;24:1370–1374. doi: 10.1111/j.1440-1746.2009.05919.x. [DOI] [PubMed] [Google Scholar]
- 4.Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol. 2001;32:106–118. doi: 10.1097/00004836-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Ellis RD, Jenkins AP, Thompson RP, Ede RJ. Clearance of refractory bile duct stones with extracorporeal shockwave lithotripsy. Gut. 2000;47:728–731. doi: 10.1136/gut.47.5.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hochberger J, Tex S, Maiss J, Hahn EG. Management of difficult common bile duct stones. Gastrointest Endosc Clin N Am. 2003;13:623–634. doi: 10.1016/s1052-5157(03)00102-8. [DOI] [PubMed] [Google Scholar]
- 7.Tandan M, Reddy DN, Santosh D, Vinod K, Ramchandani M, Rajesh G, Rama K, Lakhtakia S, Banerjee R, Pratap N, et al. Extracorporeal shock wave lithotripsy and endotherapy for pancreatic calculi-a large single center experience. Indian J Gastroenterol. 2010;29:143–148. doi: 10.1007/s12664-010-0035-y. [DOI] [PubMed] [Google Scholar]
- 8.Ong WC, Tandan M, Reddy V, Rao GV, Reddy N. Multiple main pancreatic duct stones in tropical pancreatitis: safe clearance with extracorporeal shockwave lithotripsy. J Gastroenterol Hepatol. 2006;21:1514–1518. doi: 10.1111/j.1440-1746.2006.04224.x. [DOI] [PubMed] [Google Scholar]
- 9.Guda NM, Partington S, Freeman ML. Extracorporeal shock wave lithotripsy in the management of chronic calcific pancreatitis: a meta-analysis. JOP. 2005;6:6–12. [PubMed] [Google Scholar]
- 10.Delhaye M, Vandermeeren A, Baize M, Cremer M. Extracorporeal shock-wave lithotripsy of pancreatic calculi. Gastroenterology. 1992;102:610–620. doi: 10.1016/0016-5085(92)90110-k. [DOI] [PubMed] [Google Scholar]
- 11.Dumonceau JM, Devière J, Le Moine O, Delhaye M, Vandermeeren A, Baize M, Van Gansbeke D, Cremer M. Endoscopic pancreatic drainage in chronic pancreatitis associated with ductal stones: long-term results. Gastrointest Endosc. 1996;43:547–555. doi: 10.1016/s0016-5107(96)70189-x. [DOI] [PubMed] [Google Scholar]
- 12.Costamagna G, Gabbrielli A, Mutignani M, Perri V, Pandolfi M, Boscaini M, Crucitti F. Extracorporeal shock wave lithotripsy of pancreatic stones in chronic pancreatitis: immediate and medium-term results. Gastrointest Endosc. 1997;46:231–236. doi: 10.1016/s0016-5107(97)70092-0. [DOI] [PubMed] [Google Scholar]
- 13.Neuhaus H. Fragmentation of pancreatic stones by extracorporeal shock wave lithotripsy. Endoscopy. 1991;23:161–165. doi: 10.1055/s-2007-1010647. [DOI] [PubMed] [Google Scholar]
- 14.Kozarek RA, Brandabur JJ, Ball TJ, Gluck M, Patterson DJ, Attia F, France R, Traverso LW, Koslowski P, Gibbons RP. Clinical outcomes in patients who undergo extracorporeal shock wave lithotripsy for chronic calcific pancreatitis. Gastrointest Endosc. 2002;56:496–500. doi: 10.1067/mge.2002.128105. [DOI] [PubMed] [Google Scholar]
- 15.Lehman GA. Role of ERCP and other endoscopic modalities in chronic pancreatitis. Gastrointest Endosc. 2002;56:S237–S240. doi: 10.1067/mge.2002.129008. [DOI] [PubMed] [Google Scholar]
- 16.Adamek HE, Jakobs R, Buttmann A, Adamek MU, Schneider AR, Riemann JF. Long term follow up of patients with chronic pancreatitis and pancreatic stones treated with extracorporeal shock wave lithotripsy. Gut. 1999;45:402–405. doi: 10.1136/gut.45.3.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grasso M, Spaliviero M. Extracorporeal shockwave emedicine lithotripsy. Available from: http: //www.emedicine.com/topic3024.html.
- 18.Dumonceau JM, Costamagna G, Tringali A, Vahedi K, Delhaye M, Hittelet A, Spera G, Giostra E, Mutignani M, De Maertelaer V, et al. Treatment for painful calcified chronic pancreatitis: extracorporeal shock wave lithotripsy versus endoscopic treatment: a randomised controlled trial. Gut. 2007;56:545–552. doi: 10.1136/gut.2006.096883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ohara H, Hoshino M, Hayakawa T, Kamiya Y, Miyaji M, Takeuchi T, Okayama Y, Gotoh K. Single application extracorporeal shock wave lithotripsy is the first choice for patients with pancreatic duct stones. Am J Gastroenterol. 1996;91:1388–1394. [PubMed] [Google Scholar]
- 20.Darisetty S, Tandan M, Reddy DN, Kotla R, Gupta R, Ramchandani M, Lakhtakia S, Rao GV, Banerjee R. Epidural anesthesia is effective for extracorporeal shock wave lithotripsy of pancreatic and biliary calculi. World J Gastrointest Surg. 2010;2:165–168. doi: 10.4240/wjgs.v2.i5.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farnbacher MJ, Schoen C, Rabenstein T, Benninger J, Hahn EG, Schneider HT. Pancreatic duct stones in chronic pancreatitis: criteria for treatment intensity and success. Gastrointest Endosc. 2002;56:501–506. doi: 10.1067/mge.2002.128162. [DOI] [PubMed] [Google Scholar]
- 22.Delhaye M, Arvanitakis M, Bali M, Matos C, Devière J. Endoscopic therapy for chronic pancreatitis. Scand J Surg. 2005;94:143–153. doi: 10.1177/145749690509400211. [DOI] [PubMed] [Google Scholar]
- 23.Inui K, Tazuma S, Yamaguchi T, Ohara H, Tsuji T, Miyagawa H, Igarashi Y, Nakamura Y, Atomi Y. Treatment of pancreatic stones with extracorporeal shock wave lithotripsy: results of a multicenter survey. Pancreas. 2005;30:26–30. [PubMed] [Google Scholar]
- 24.Schneider HT, May A, Benninger J, Rabenstein T, Hahn EG, Katalinic A, Ell C. Piezoelectric shock wave lithotripsy of pancreatic duct stones. Am J Gastroenterol. 1994;89:2042–2048. [PubMed] [Google Scholar]
- 25.Adamek HE, Maier M, Jakobs R, Wessbecher FR, Neuhauser T, Riemann JF. Management of retained bile duct stones: a prospective open trial comparing extracorporeal and intracorporeal lithotripsy. Gastrointest Endosc. 1996;44:40–47. doi: 10.1016/s0016-5107(96)70227-4. [DOI] [PubMed] [Google Scholar]
- 26.Binmoeller KF, Brückner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy. 1993;25:201–206. doi: 10.1055/s-2007-1010293. [DOI] [PubMed] [Google Scholar]
- 27.Neuhaus H, Zillinger C, Born P, Ott R, Allescher H, Rösch T, Classen M. Randomized study of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for difficult bile duct stones. Gastrointest Endosc. 1998;47:327–334. doi: 10.1016/s0016-5107(98)70214-7. [DOI] [PubMed] [Google Scholar]
- 28.Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video) Gastrointest Endosc. 2007;65:832–841. doi: 10.1016/j.gie.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 29.Attasaranya S, Sherman S. Balloon dilation of the papilla after sphincterotomy: rescue therapy for difficult bile duct stones. Endoscopy. 2007;39:1023–1025. doi: 10.1055/s-2007-966922. [DOI] [PubMed] [Google Scholar]
- 30.Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH, et al. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720–726; quiz 768, 771. doi: 10.1016/j.gie.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 31.Lee JH. Is combination biliary sphincterotomy and balloon dilation a better option than either alone in endoscopic removal of large bile-duct stones? Gastrointest Endosc. 2007;66:727–729. doi: 10.1016/j.gie.2007.03.1060. [DOI] [PubMed] [Google Scholar]
- 32.MA Kocdor, S Bora, C Terzi, I Ozman, E Tankut. Extracorporeal shock wave lithotripsy for retained common bile duct stones. Minim. Invasive Ther. Allied Technol. 2000;9:371–374. [Google Scholar]
- 33.Livingston EH, Rege RV. Technical complications are rising as common duct exploration is becoming rare. J Am Coll Surg. 2005;201:426–433. doi: 10.1016/j.jamcollsurg.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 34.Tichansky DS, Taddeucci RJ, Harper J, Madan AK. Minimally invasive surgery fellows would perform a wider variety of cases in their “ideal” fellowship. Surg Endosc. 2008;22:650–654. doi: 10.1007/s00464-007-9430-6. [DOI] [PubMed] [Google Scholar]
- 35.Singh VK, Khashab MA, Okolo PI, Kalloo AN. ERCP or laparoscopic exploration for the treatment of suspected choledocholithiasis? Arch Surg. 2010;145:796; author reply 796. doi: 10.1001/archsurg.2010.128. [DOI] [PubMed] [Google Scholar]
- 36.Kratzer W, Mason RA, Grammer S, Preclik G, Beckh K, Adler G. Difficult bile duct stone recurrence after endoscopy and extracorporeal shockwave lithotripsy. Hepatogastroenterology. 1998;45:910–916. [PubMed] [Google Scholar]
- 37.Hirata N, Kushida Y, Ohguri T, Wakasugi S, Kojima T, Fujita R. Hepatic subcapsular hematoma after extracorporeal shock wave lithotripsy (ESWL) for pancreatic stones. J Gastroenterol. 1999;34:713–716. doi: 10.1007/s005350050325. [DOI] [PubMed] [Google Scholar]
- 38.Leifsson BG, Borgström A, Ahlgren G. Splenic rupture following ESWL for a pancreatic duct calculus. Dig Surg. 2001;18:229–230. doi: 10.1159/000050139. [DOI] [PubMed] [Google Scholar]
- 39.Plaisier PW, den Hoed PT. Splenic abscess after lithotripsy of pancreatic duct stones. Dig Surg. 2001;18:231–232. doi: 10.1159/000050140. [DOI] [PubMed] [Google Scholar]
- 40.Karakayali F, Sevmiş S, Ayvaz I, Tekin I, Boyvat F, Moray G. Acute necrotizing pancreatitis as a rare complication of extracorporeal shock wave lithotripsy. Int J Urol. 2006;13:613–615. doi: 10.1111/j.1442-2042.2006.01366.x. [DOI] [PubMed] [Google Scholar]


