Abstract
Objective
The aim of this study was to analyze the treatment outcome of patients with vein of Galen aneurysmal malformations (VGM).
Methods
Clinical and angiographic data of six consecutive patients with VGM were retrospectively reviewed. VGMs were angiographically classified by Yasargil's method. Treatment outcomes were evaluated.
Results
Mean age at initial treatment was 4.4±5.7 months. Angiographic types of VGMs were type II in two patients and type III in four. Three patients had cardiac symptoms and the others were asymptomatic. Two patients were treated with transvenous embolization, three with transarterial embolization, and one was managed conservatively. Two patients died due to venous hypertension few days after transvenous approach. Of three patients who were transarterially embolized, one was completely occluded with Onyx and two were incompletely occluded. During the follow-up period (range, one to six years) two of three patients treated with transarterial approach were asymptomatic and the other showed mild symptoms. One patient who was managed conservatively showed normal performance.
Conclusion
Transarterial embolization of VGMs may be better than transvenous approach in terms of the treatment outcome and complication. Further studies are needed because of the rarity of the disease and rapid advancement of endovascular techniques.
Keywords: Endovascular treatment, Transvenous embolization, Transarterial embolization, Vein of Galen aneurysmal malformation
INTRODUCTION
Vein of Galen aneurysmal malformation (VGM) is a rare congenital abnormality with a prevalence of less than 1/25,000 deliveries8). It is characterized by a midline intracranial vascular fistula with aneurysmal dilatation of the vein of Galen. During the normal development, the large median prosencephalic vein of Markowski gradually involutes and eventually persists as the great cerebral vein of Galen11). Thus, VGM is assumed to be a persistent structure of the embryonic median prosencephalic vein of Markowski.
Majority of the VGM present in the early childhood, and the most striking presentation is congestive cardiac failure in the newborn period8). In the past, this was usually associated with rapid progression to multisystem organ failure and death, despite vigorous treatment and supportive medical care3). With the advent of endovascular techniques, treatment outcome of VGM has much improved3,4,8). Embolization of feeding arteries or draining veins can considerably reduce the shunt flow. The authors were to present their experience of treatment for VGM, mainly in terms of endovascular embolization.
MATERIALS AND METHODS
Overall, six patients were diagnosed and treated in our institute between January 1998 and December 2010. We retrospectively reviewed medical record and imaging data of them. VGMs were angiographically classified according to the Yasargil's method (type I, small pure cisternal fistula between VGM and pericallosal arteries or posterior cerebral arteries; type II, multiple fistulous communications between the vein of Galen and the thalamoperforating vessels; type III, high flow mixed type I and II)13). VGMs were treated with observation and endovascular embolization via the transvenous and transarterial approaches, using various detachable coils [Guglielmi detachable coils (Boston Scientific, Fremont, CA, USA), MicroPlex (MicroVention, AlisoViejo, CA, USA), Trufill-DCS (Cordis, Miami Lakes, FL, USA), Axium (ev3, Irvine, CA, USA)], fibered pushable coils (Tornado, Cook, Bloomington, IL, USA), 25-33% N-butyl 2-cyanoacrylate glue (NBCA, B Braun, Melsungen, Germany), and ethylene vinyl alcohol copolymer dissolved in dimethyl sulfoxide (Onyx®, ev3, Irvine, CA, USA). Transvenous approach was performed via the femoral and internal jugular veins to VGMs. Transarterial approach was done via the femoral artery toward the various arterial feeders such as anterior and posterior choroidal (AChA and PChA) and pericallosal arteries (PA). Clinical outcome was graded according to Jones' 5-point scale (score of 0 : death; score of 1 : severe neurological impairment; score of 2 : moderate neurological impairment; score of 3 : mild neurological impairment; score of 4 : normal)5).
RESULTS
Clinical and angiographic data were summarized in Table 1. All patients were boys under two years old with mean age of 4.4±5.7 months (range, 0.2 to 15 months) at the time of the initial treatment. Two patients (patient 1 and 2) were delivered by cesarean section in normal full term, three (patient 3 to 5) were by vaginal delivery in normal full-term, and one (patient 6) were by vaginal delivery on gestational age of 35 weeks. Clinical presentation included asymptomatic cardiomegaly, cardiac anomalies such as arterial septal defect (ASD), patent ductus arteriosus (PDA), and patent foramen ovale (PFO), congestive heart failure, increased head circumference (HC), and hydrocephalus. Three asymptomatic patients were detected on brain untrasonography, and they accompanied PDA, PFO, cardiomegaly, and increased HC. The other symptomatic patients presented with cardiac symptoms and signs such as murmur, tachycardia, tachypnea, ASD, and pulmonary hypertension. Angiographic types of VGMs were type II in two patients and type III in four.
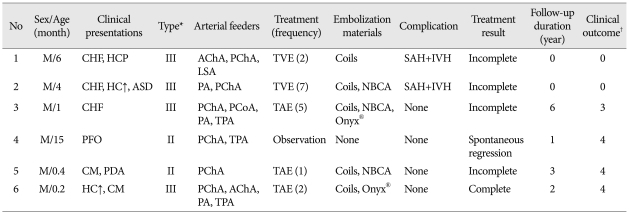
Table 1.
Clinical data and treatment outcomes in patients with vein of Galen malformation
*Yasargil's classification of vein of Galen malformation13), †Clinical outcome was scored according to an article5). CHF : congestive heart failure, HCP : hydrocephalus, AChA : anterior choroidal artery, PChA : posterior choroidal artery, LSA : lenticulostriate artery, TVE : transvenous embolization, SAH : subarachnoid hemorrhage, IVH : intraventricular hemorrhage, HC : head circumference, ASD : astrial septal defect, PA : pericallosal artery, NBCA : N-butyl 2-cyanoacrylate glue, PCoA : posterior communicating artery, TPA : thalamoperforating artery, TAE : transarterial embolization, PFO : patent foramen ovale, CM : cardiomegaly, PDA : patent ductus arteriosus
Five of six patients were treated with endovascular embolization via transvenous or transarterial approaches. One who was not treated (patient 4) was due to no symptoms and evidence of spontaneous regression on follow-up angiography. Two patients (patient 1 and 2) were incompletely treated by transvenous embolization with coils. However, they all died in a few hours after the procedures, with signal change at the deep basal brain parenchyma and subarachnoid and intraventricular hemorrhage on computed tomography. Three patients were embolized with transarterial approach. Patient 3 was embolized first two times through the PChA and PA with coil alone, subsequent two times through the PChA and posterior communicating artery with coil and 25% NBCA, and the last through the PChA and thalamoperforating artery (TPA) with coil, 33% NBCA, and Onyx. Patient 5 underwent one incomplete embolization through the PChA with coil and 33% NBCA, and patient 6 complete embolization through the PChA with coils and Onyx. All the patients treated with transarterial embolization have been followed-up with good clinical outcome scales of 3 and 4.
Illustrative cases
Patient 1
A six-month child presented with cold sweating and feeding difficulty. Brain ultrasonography and magnetic resonance imaging revealed a VGM. Subsequent cerebral angiography showed that the lesion had multiple direct fistulae from lenticulostriate artery, AChA, and PChA to the vein of Galen. VGM was embolized twice with multiple coils via transvenous approach. First embolization was performed without any complication. However, patient died after the second embolization due to subarachnoid and intraventricular hemorrhages (Fig. 1).
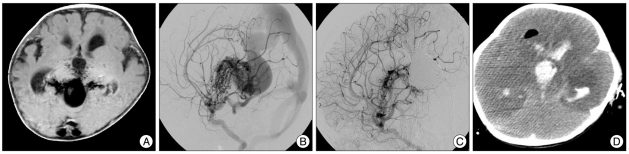
Fig. 1.
A : Brain MR axial imaging. Dilated vein of Galen is observed. B and C : Cerebral angiography. The lesion has multiple direct fistulae from lenticulostriate artery, pericallosal artery, and posterior cerebral artery to the vein of Galen (B). The lesion was embolized with multiple coils via 2 times of transvenous approach (C). D : Brain CT. Diffuse brain swelling and intracranial hemorrhage are observed. MR : magnetic resonance, CT : computed tomography.
Patient 6
A two-week child was born by vaginal delivery on gestational age of 35 weeks with 2.9 kg. There were no perinatal problems, and VGM was coincidentally found on screening brain ultrasonography shortly after birth. His HC was 95 percentile and cardiomegaly was identified on echocardiography. It was supplied by PChA, AChA, PA, and TPA. Transarterial embolization via PChA was incompletely performed at two weeks of age with coils with no complication. The second transarterial embolization via PChA achieved complete occlusion of the lesion at one year of age with Onyx with no complication (Fig. 2). Thereafter, he has been followed-up without any problems.
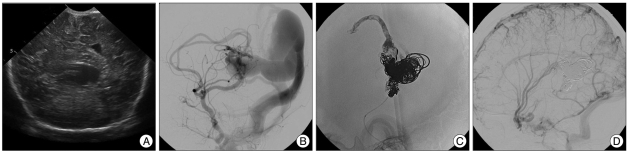
Fig. 2.
A : Brain sonography. Dilated vein of Galen is observed. B : Cerebral angiography. Vein of Galen is supplied by posterior cerebral artery and pericallosal artery. C : Transarterial embolization with coil and Onyx. First transarterial embolization with coil via posterior cerebral artery at 2 weeks of age and second embolization with Onyx via pericallosal artery at 1 year of age were performed, respectively. D : Follow-up angiography. There is no evidence of remaining shunt.
DISCUSSION
VGMs consist of high-flow arteriovenous fistulas and can lead to congestive heart failure and hydrocephalus. They are rare, and usually associated with high mortality and morbidity, particularly in neonates (up to 100%)3,10). There have been a lot of efforts to understand the angioarchitecture and pathophysiology, and to perform effective treatment. As the endovascular techniques have developed, understanding of the VGM has greatly advanced during the past two decades. Analyzing the vascular anatomy of VGM and correlating it with embryologic development of the cerebral vasculature, Raybaud et al.11) concluded that the malformation develops between the sixth and eleventh week of gestation, after development of the circle of Willis. It is thought to result from the development of an arteriovenous connection between primitive choroidal vessels and the median prosencephalic vein of Markowski.
Clinical presentations and angioarchitectures are known to have a tight correlation with age at presentation3,6). Symptomatic neonates typically present with severe cardiac failure, and high flow shunt of Yasargil type I is dominant. Infants usually present with increase in head circumference, hydrocephalus, or seizure. Older children tend to present with milder symptoms such as headache. In the present study, age did not have such a close relationship with the clinical presentations. Two (patient 1 and 2) of three patients with congestive heart failure (CHF) were older than one month of age, and one (patient 3) of three neonates presented with CHF. It was because the age at admission did not exactly correspond to the one at clinical presentations. Diagnosis of VGM in patient 2 was delayed because initial symptoms had been thought to result from ASD alone. Patient 5 and 6 were incidentally diagnosed with routine check-ups of brain ultrasonography.
Endovascular intervention is known to be treatment of choice for VGM. There are two kinds of techniques : transvenous and transarterial embolization. Transvenous approach is performed, either with femoral or jugular vein, or through direct puncture of the torcula3,4,12). The venous approach to the VGMs is technically less demanding and can be performed in situation where a superselective arterial embolization is not feasible. However, the drawback of transvenous approach is that rapid closure of the venous drainage can cause the development of "normal perfusion breakthrough syndrome", with severe complications, including malignant brain swelling and intracranial hemorrhages3). In addition, recent studies reported that normal deep veins could be connected to the venous component of a VGMs2,3,11). This particular anatomy can be a major pitfall of transvenous embolization because it may potentially result in detrimental complications such as venous infarct and hemorrhage. Therefore, majority of VGMs have been treated with transarterial embolization6) except just a few cases1,7). Casasco et al.1) achieved excellent results with transvenous approach and believed that transvenous approach was better than transarterial embolization or surgery. They could escape from the disastrous complications in the manner that embolization stopped when intra-VGM pressure increased more than 50% of the initial pressure. In the present study, patients who were treated with transvenous approach died all due to the deep brain swelling and intracranial hemorrhage. The reasons of selecting a transvenous approach were that they had complex angioarchitectures of Yasargil type III. Thereafter, transarterial approach with or without combined transvenous approach was the treatment of choice for the treatment of VGMs in our institute.
On the other hand, transarterial embolization is performed through the perforators. Some fine perforators are sometimes impossible to approach, and embolic material within a larger fistula can fly away from the fistula point and occlude the draining veins, which can cause venous hypertension. As Onyx has been used, transarterial embolization became more feasible and safer. It is a bio-compatible liquid polymer that precipitates and solidifies upon contact with blood, thus forming a soft, spongy embolus. So, it can be molded and extended through the fine channels distant from the injection point for a longer time rather than the previous glues. In this series, transarterial embolization showed satisfactory clinical outcome even after incomplete treatment. Furthermore, procedures with Onyx were safe and effective that one case could achieve complete occlusion. As the clinical experience of Onyx increases, better treatment results are expected.
This study has a critical limitation. Case number is too small to draw an analytic conclusion but an individual description. Although VGM itself is extremely rare, the true incidence may be higher because VGMs are known to consist of 30% of all pediatric vascular anomalies9). Some factors may contribute the rarity of the disease, such as low birth rate, unreported treatment at the other institutes, preterm detection and abortion, and undetected cases. In spite of the rarity, the intention of this report was to share the experience of disastrous situations with treatment strategies for VGMs.
CONCLUSION
VGMs are rare, but serious diseases with high morbidity and mortality. As the endovascular procedures are introduced, treatment of VGMs is successfully performed. In this series, transarterial embolization showed better outcome than transvenous approach. However, small number of case and ongoing advancement in endovascular techniques require more experiences and research.
References
- 1.Casasco A, Lylyk P, Hodes JE, Kohan G, Aymard A, Merland JJ. Percutaneous transvenous catheterization and embolization of vein of galen aneurysms. Neurosurgery. 1991;28:260–266. doi: 10.1097/00006123-199102000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Gailloud P, O'riordan DP, Burger I, Lehmann CU. Confirmation of communication between deep venous drainage and the vein of galen after treatment of a vein of Galen aneurysmal malformation in an infant presenting with severe pulmonary hypertension. AJNR Am J Neuroradiol. 2006;27:317–320. [PMC free article] [PubMed] [Google Scholar]
- 3.Gailloud P, O'Riordan DP, Burger I, Levrier O, Jallo G, Tamargo RJ, et al. Diagnosis and management of vein of galen aneurysmal malformations. J Perinatol. 2005;25:542–551. doi: 10.1038/sj.jp.7211349. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Monaco R, De Victor D, Mann C, Hannedouche A, Terbrugge K, Lasjaunias P. Congestive cardiac manifestations from cerebrocranial arteriovenous shunts. Endovascular management in 30 children. Childs Nerv Syst. 1991;7:48–52. doi: 10.1007/BF00263834. [DOI] [PubMed] [Google Scholar]
- 5.Jones BV, Ball WS, Tomsick TA, Millard J, Crone KR. Vein of Galen aneurysmal malformation : diagnosis and treatment of 13 children with extended clinical follow-up. AJNR Am J Neuroradiol. 2002;23:1717–1724. [PMC free article] [PubMed] [Google Scholar]
- 6.Khullar D, Andeejani AM, Bulsara KR. Evolution of treatment options for vein of Galen malformations. J Neurosurg Pediatr. 2010;6:444–451. doi: 10.3171/2010.8.PEDS10231. [DOI] [PubMed] [Google Scholar]
- 7.Lasjaunias PL, Chng SM, Sachet M, Alvarez H, Rodesch G, Garcia-Monaco R. The management of vein of Galen aneurismal malformations. Neurosurgery. 2006;59:S184–S194. doi: 10.1227/01.NEU.0000237445.39514.16. discussion S3-S13. [DOI] [PubMed] [Google Scholar]
- 8.Lasjaunias P, Hui F, Zerah M, Garcia-Monaco R, Malherbe V, Rodesch G, et al. Cerebral arteriovenous malformations in children. Management of 179 consecutive cases and review of the literature. Childs Nerv Syst. 1995;11:66–79. doi: 10.1007/BF00303807. discussion 79. [DOI] [PubMed] [Google Scholar]
- 9.Long DM, Seljeskog EL, Chou SN, French LA. Giant arteriovenous malformations of infancy and childhood. J Neurosurg. 1974;40:304–312. doi: 10.3171/jns.1974.40.3.0304. [DOI] [PubMed] [Google Scholar]
- 10.Park SH, Hwang SK, Kim YS, Kim SL. Vein of Galen malformation in a neonate : case report. J Korean Neurosurg Soc. 2003;34:51–53. [Google Scholar]
- 11.Raybaud CA, Strother CM, Hald JK. Aneurysms of the vein of Galen : embryonic considerations and anatomical features relating to the pathogenesis of the malformation. Neuroradiology. 1989;31:109–128. doi: 10.1007/BF00698838. [DOI] [PubMed] [Google Scholar]
- 12.Yamashita Y, Abe T, Ohara N, Maruoka T, Toyoda O, Inoue O, et al. Successful treatment of neonatal aneurysmal dilatation of the vein of Galen : the role of prenatal diagnosis and trans-arterial embolization. Neuroradiology. 1992;34:457–459. doi: 10.1007/BF00596519. [DOI] [PubMed] [Google Scholar]
- 13.Yasargil MG. Microneurosurgery IIIB. New York: Thieme Medical Publishers; 1988. pp. 323–357. [Google Scholar]