Abstract
Objective
Retrospective analysis to compare the effect and complication of epidural patient-controlled analgesia (epidural PCA) with intravenous patient-controlled analgesia (IV PCA) for the treatment of the post-operative pain after posterior lumbar instrumented fusion.
Methods
Sixty patients who underwent posterior lumbar instrumented fusion for degenerative lumbar disease at our institution from September 2007 to January 2008 were enrolled in this study. Out of sixty patients, thirty patients received IV PCA group and thirty patients received epidural PCA group. The pain scale was measured by the visual analogue scale (VAS) score.
Results
There were no significant difference between IV PCA group and epidural PCA group on the PCA related complications (p=0.7168). Ten patients in IV PCA group and six patients in epidural PCA group showed PCA related complications. Also, there were no significant differences in reduction of VAS score between two groups on postoperative 2 hours (p=0.9618) and 6 hours (p=0.0744). However, postoperative 12 hours, 24 hours and 48 hours showed the significant differences as mean of reduction of VAS score (p=0.0069, 0.0165, 0.0058 respectively).
Conclusion
The epidural PCA is more effective method to control the post-operative pain than IV PCA after 12 hours of spinal fusion operation. However, during the first twelve hours after operation, there were no differences between IV PCA and epidural PCA.
Keywords: Patient-controlled analgesia, Postoperative pain, Spinal fusion
INTRODUCTION
Traditional posterior lumbar interbody fusion and posterior transpedicular screw fixation is associated with high degree of postoperative pain. Most patients require parenteral administration of analgesics especially during 2 days after operations or more. High degree of postoperative pain precludes them from early mobilization, which is known to lengthen hospital stay and might result in various complications7,11).
Patient-controlled analgesia (PCA) has long been used for pain control after spinal operations3,5,6,13,14,20). And, there were various methods to administrate the analgesics such as epidural or intravenous route. Excellent pain control and a decrease in the total amount of narcotic used and therefore less respiratory depression and sedation are the benefits of the epidural PCA although there were serious side effects including pruiritus, nausea, urine retention and neurologic abnormality12,18). this property should facilitate mobilization and improve patient outcome and satisfaction5). This retrospective comparative study was designed to compare the efficacy and complication of epidural PCA with intravenous (IV) PCA in patients who underwent posterior lumbar instrumented fusion at our institute.
MATERIALS AND METHODS
Indication and evaluation
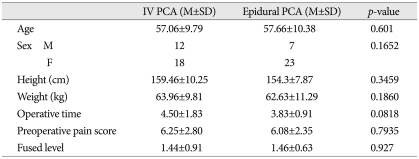
We included consecutive 60 patients who underwent one or two level posterior lumbar instrumented fusion for degenerative disc disease, spondylolisthesis, or spinal instability between Sep 2007 and Jan 2008. IV PCA group included 30 patients, 12 male and 18 female and epidural PCA group included 30 patients, 7 male and 23 female. Average age of epidural PCA was 57.66±10.38 and IV PCA was 57.06±9.79 (Table 1).
Table 1.
Demographics of patients
IV : intravenous PCA : patient-controlled analgesia
Pain was assessed using a printed copy of both verbal numerical analogue scale and faced pain scale by researcher and members of this research (nurses) and recorded for time periods of 2, 6, 12, 48 hours after surgery unless PCA was removed before 48 hours (Fig. 1).
Fig. 1.
VAS score. Pain was assessed using the VAS ranging from "0" (no pain) to "10" (worst imaginable pain). VAS : visual analogue scale.
All symptoms such as nausea, vomiting, headache, dizziness, chest discomfort, urine retention and neurologic deficit were recorded as adverse effects. Among patients who were not removed the PCA until 48 hours after surgery, the number of additional analgesics injected were counted.
All data were compared statistically using chi-square test and Student's t-test for homogeneity between two groups, Fisher's exact test for adverse effect and Student's t-test for pain scale (SAS 9.1) and significance was defined as p<0.05.
Technique and protocol
Using continuous and bolus infusion kit (continuous and bolus ambix anaplus), the PCA medication were dosed in the following manners : flow rate was 2mL/hr and additional doses of 0.5 mL/5 min with 20-minute lockout are given by patient-controlled demand.
1) IV PCA medications : total mixture of Ketoracin® (ketorolac tromethamine, Roche, Korea) 120 mg, Fentanyl citrate (Hana Pharm CO LTD, Korea) 1,000 µg and Zofran® (Ondanstron dehydrate, GlaxoSmithKline) 16 mg with saline (100 mL).
2) Epidural PCA medications : total mixture of Morphine 5 mg and 0.75% Ropivacaine 20 cc with saline (100 mL).
Epidural catheter was inserted into the epidural space 5 cm above laminectomy level under direct visualization and was passed retrograde through the needle in the paraspinal muscles after removal of the stylet by the surgeon before wound closure.
RESULTS
Patient profile and homogeneity
There were a total of 60 patients. Thirty patients were in IV PCA group and 30 patients were in epidural PCA group. There were no statistically significant differences in regards to patients' demographic data, number of fused level and operative time between two groups (Student's t-test, chi-square test) (Table 1).
Pain score results
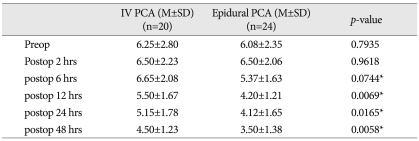
There was no significant difference about preoperative pain score between two groups. Average preoperative pain score of IV PCA group was 6.25±2.80, and epidural PCA was 6.08±2.35 (p=0.7935). There was also no significant difference between two groups about postoperative pain score at 2 hours and 6 hours (p=0.9618, p=0.0744 respectively). However, epidural PCA group showed significant lower pain score than IV PCA group at 12 hours, 24 hours and 48 hours postoperatively (all p<0.05) (Table 2).
Table 2.
Postoperative pain scores
*p<0.05. preop : preoperatively, postop : postoperatively, hrs : hours, IV : intravenous PCA : patient-controlled analgesia
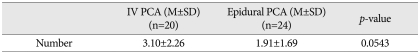
We also reviewed, based on medical records, for the number of injection of additional analgesics (intravenous ketoracin 30 mg/ample) in patients who did not remove PCA until 48 hours. Although there was no significant difference between two groups, epidural PCA group (aver 3.10±2.26) required less additional analgesics than IV PCA group (aver 1.91±1.69) (p=0.0543) (Table 3).
Table 3.
Number of additional analgesic injections
IV : intravenous, PCA : patient-controlled analgesia
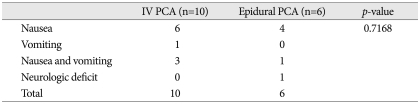
Adverse effect
There was no significant difference in regard to adverse effect between two groups.
PCA had to be removed in 10 patients of IV PCA group versus 6 patients of epidural PCA group. Of 10 patients of IV PCA group, 6 patients complained nausea, 1 patient had vomiting, and 3 patients had both symptoms. Among 6 patients of epidural PCA group, 4 patients complained nausea, 1 patient had both nausea and vomiting, and 1 patient had both leg hypoesthesia. These symptoms and neurologic deficit were improved after removal of PCA (Table 4).
Table 4.
Adverse effects
IV : intravenous, PCA : patient-controlled analgesia
DISCUSSION
In posterior lumbar instrumented fusion, appropriate postoperative pain management is essential for early ambulation, reduced hospital stay, avoidance of additional analgesics, and consequently for improvement of patient outcome. PCA via ether intravenous or epidural route has been considered standard management after major orthopedic or spinal surgery2,8,9) and there have been many comparative studiess on the effectiveness and complication of epidural PCA with intravenous PCA10,15,17,19). Postoperative pain score (visual analog scale) were significantly lower in the epidural PCA group when compared with that in the IV PCA group16,20). Epidural PCA group showed superior result in pain control on post-operation day 1 and 2 than on the day of operation20).
Other studies have reported that the capacity of excellent pain control in Epidural PCA were probably due to the higher concentration of ropivacaine, the higher infusion rate and the use of an epidural opioid lately14,16). But, the total amount of opioid used in epidural PCA was less than IV PCA group14).
In present study, epidural PCA group showed superior postoperative pain control after 6 hours of operation to IV PCA group (p=0.0744 respectively at 6 hours, all p<0.05 at 12 hours, 24 hours and 48 hours postoperatively). Also, in patients who was not removed PCA until 48 hours, epidural PCA group required less additional analgesics than IV PCA group although it was not statistically significant (p=0.0543).
In addition, although we did not investigate in this study, shorter hospital stay and earlier full diet were other positive effects of the epidural PCA20). Van Boerum et al., reported that the patient in the epidural PCA group could start a full diet earlier and were discharged earlier in one and half days on average than the IV PCA group10,15,17,19). Also, patients in the epidural PCA group started ambulation earlier than in the IV PCA group16,20). Moreover, patients in the PCEA group were significantly more satisfied with pain therapy16).
Common side effects associated with epidural administration of local anesthetics or opioids, such as nausea and vomiting or pruritus were not evaluated systematically by all authors14,16,20). Pruritus was described with an incidence between 7% and 43%, nausea and vomiting with an incidence between 14% and 86%16). Because of the amount of opioid used in PCA is small, the nausea and vomititng can be reduced1,10,15,17,19). Nausea and vomiting are the most common and distress side effect of IV PCA, although the pain control medication is morphine or fentanyl14,16,20). Because of small amount of morphine used in epidural PCA, some patients have nausea symptom but patients with vomiting are usually tolerable8,10,15,17,19).
Other side effects associated with epidural PCA include, respiratory depression and motor deficit and infection18). Mild respiratory depression occurred rarely in patients with epidural PCA, which was unresponsive to naloxone, but needed no ventilator support, and the resolved uneventfully16,18,20). In this study, none of patients suffered from respiratory depression.
Although spine surgery causes severe postoperative pain, epidural PCA is not commonly used16). The main reason is that it might cause some complications such as motor block16,18,20). The motor block can make difficulty in early detection of surgical related neurologic deficit16,18,20). In our study, one patient in epidural PCA group had temporary hypoesthesia of bilateral lower extremities, we assumed that the cause of hypoesthesia might be associated with local analgesics (ropivacane), not epidural procedure, surgery or opioid because it showed bilaterally involved whole dermatome of the lower extremities10). Thus, we thought this problem could be resolved by controlling the amount of medication and as soon as we removed the epidural PCA, the symptom had disappeared10,14,18). A small number of patients showed significant postoperative ileus. But it was recovered shortly (1 or 2 days) and no adverse sequelae16).
IV PCA has been more commonly accepted postoperative pain control method for several reason2). First, IV PCA needs no additional surgical procedure2,5,18). Second, because fentanyl, the main pain killer of IV PCA, usually does not cause neurologic deficit, it is possible to detect surgical procedure related neurologic deficit immediately after operation2,5,10,16).
However, nausea and vomiting are the most common and distress side effect of fentanyl in IV PCA4,5,14,18,20). In our study, PCA had to be removed in 10 patients of IV PCA group. The most common cause to discontinue PCA infusion in IV PCA group was intolerable nausea and vomiting.
The two limitations of this study are as follows. The first, the main medications of two PCA were different, we used morphine in epidural PCA and fentanyl in IV PCA. Fentanyl is the most common medication which used in IV PCA2,4,5,14,16). Because morphine is usually associated with nausea and vomiting symptom (incidence being 10%), morphine is commonly used rather than fentanyl in IV PCA2,4,5,14,18). Secondly, we investigated only pain relief for patient' outcome in two PCA groups. The future prospective randomized controlled study should be done for patient's functional outcome, hospital stay, time to ambulation and time to start full diet beyond pain control.
CONCLUSION
Epidural PCA group showed significant lower pain score than IV PCA group after 6 hours postoperatively (p<0.05). There was no statistically significant difference in adverse effect of PCA between two groups. The number of additional analgesics injection in epidural PCA group was lower than IV PCA group (p=0.0543). Prospective randomized controlled study should be needed for pain control, functional outcome, duration of hospital stay, time to ambulation, and time to start full diet.
References
- 1.Bonhomme V, Doll A, Dewandre PY, Brichant JF, Ghassempour K, Hans P. Epidural administration of low-dose morphine combined with clonidine for postoperative analgesia after lumbar disc surgery. J Neurosurg Anesthesiol. 2002;14:1–6. doi: 10.1097/00008506-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Bost P, Commun F, Albuisson E, Guichard C, Mom T, Eschalier A, et al. [Postoperative pain assessment in head and neck cancer surgery : benefit of patient controlled analgesia (PCA)] Ann Otolaryngol Chir Cervicofac. 1999;116:154–161. [PubMed] [Google Scholar]
- 3.Cata JP, Noguera EM, Parke E, Ebrahim Z, Kurz A, Kalfas I, et al. Patient-controlled epidural analgesia (PCEA) for postoperative pain control after lumbar spine surgery. J Neurosurg Anesthesiol. 2008;20:256–260. doi: 10.1097/ANA.0b013e31817ffe90. [DOI] [PubMed] [Google Scholar]
- 4.Choi YS, Shim JK, Yoon do H, Jeon DH, Lee JY, Kwak YL. Effect of ramosetron on patient-controlled analgesia related nausea and vomiting after spine surgery in highly susceptible patients : comparison with ondansetron. Spine (Phila Pa 1976) 2008;33:E602–E606. doi: 10.1097/BRS.0b013e31817c6bde. [DOI] [PubMed] [Google Scholar]
- 5.Cohen BE, Hartman MB, Wade JT, Miller JS, Gilbert R, Chapman TM. Postoperative pain control after lumbar spine fusion. Patient-controlled analgesia versus continuous epidural analgesia. Spine (Phila Pa 1976) 1997;22:1892–1896. doi: 10.1097/00007632-199708150-00016. discussion 1896-1897. [DOI] [PubMed] [Google Scholar]
- 6.Fisher CG, Belanger L, Gofton EG, Umedaly HS, Noonan VK, Abramson C, et al. Prospective randomized clinical trial comparing patient-controlled intravenous analgesia with patient-controlled epidural analgesia after lumbar spinal fusion. Spine (Phila Pa 1976) 2003;28:739–743. [PubMed] [Google Scholar]
- 7.Fountas KN, Kapsalaki EZ, Johnston KW, Smisson HF, 3rd, Vogel RL, Robinson JS., Jr Postoperative lumbar microdiscectomy pain. Minimalization by irrigation and cooling. Spine (Phila Pa 1976) 1999;24:1958–1960. doi: 10.1097/00007632-199909150-00016. [DOI] [PubMed] [Google Scholar]
- 8.Garstka J, Mikolajczak G. [Patient-controlled analgesia (PCA) in postop pain management in scoliosis surgery] Chir Narzadow Ruchu Ortop Pol. 1998;63:281–286. [PubMed] [Google Scholar]
- 9.Hecker BR, Albert L. Patient-controlled analgesia : a randomized, prospective comparison between two commercially available PCA pumps and conventional analgesic therapy for postoperative pain. Pain. 1988;35:115–120. doi: 10.1016/0304-3959(88)90283-7. [DOI] [PubMed] [Google Scholar]
- 10.Jayr C, Beaussier M, Gustafsson U, Leteurnier Y, Nathan N, Plaud B, et al. Continuous epidural infusion of ropivacaine for postoperative analgesia after major abdominal surgery : comparative study with i.v. PCA morphine. Br J Anaesth. 1998;81:887–892. doi: 10.1093/bja/81.6.887. [DOI] [PubMed] [Google Scholar]
- 11.Jo DJ, Jun JK, Kim KT, Kim SM. Lumbar interbody fusion outcomes in degenerative lumbar disease : comparison of results between patients over and under 65 years of age. J Korean Neurosurg Soc. 2010;48:412–418. doi: 10.3340/jkns.2010.48.5.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lebovits AH, Zenetos P, O'Neill DK, Cox D, Dubois MY, Jansen LA, et al. Satisfaction with epidural and intravenous patient-controlled analgesia. Pain Med. 2001;2:280–286. doi: 10.1046/j.1526-4637.2001.01051.x. [DOI] [PubMed] [Google Scholar]
- 13.Matsui H, Kanamori M, Terahata N, Miaki K, Makiyama N, Satone T, et al. Significance of patient-controlled analgesia in combination with continuous epidural block for patients who underwent posterior lumbar surgery. Eur Spine J. 1998;7:120–124. doi: 10.1007/s005860050041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reuben SS, Connelly NR, Lurie S, Klatt M, Gibson CS. Dose-response of ketorolac as an adjunct to patient-controlled analgesia morphine in patients after spinal fusion surgery. Anesth Analg. 1998;87:98–102. doi: 10.1097/00000539-199807000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Rockemann MG, Seeling W, Goertz AW, Konietzko I, Steffen P, Georgieff M. [Effectiveness, side effects and costs of postoperative pain therapy : intravenous and epidural patient-controlled analgesia (PCA)] Anasthesiol Intensivmed Notfallmed Schmerzther. 1997;32:414–419. doi: 10.1055/s-2007-995082. [DOI] [PubMed] [Google Scholar]
- 16.Schenk MR, Putzier M, Kügler B, Tohtz S, Voigt K, Schink T, et al. Postoperative analgesia after major spine surgery : patient-controlled epidural analgesia versus patient-controlled intravenous analgesia. Anesth Analg. 2006;103:1311–1317. doi: 10.1213/01.ane/0000247966.49492.72. [DOI] [PubMed] [Google Scholar]
- 17.Singelyn FJ, Gouverneur JM. Postoperative analgesia after total hip arthroplasty : i.v. PCA with morphine, patient-controlled epidural analgesia, or continuous "3-in-1" block? : a prospective evaluation by our acute pain service in more than 1,300 patients. J Clin Anesth. 1999;11:550–554. doi: 10.1016/s0952-8180(99)00092-6. [DOI] [PubMed] [Google Scholar]
- 18.Teng YH, Hu JS, Tsai SK, Liew C, Lui PW. Efficacy and adverse effects of patient-controlled epidural or intravenous analgesia after major surgery. Chang Gung Med J. 2004;27:877–886. [PubMed] [Google Scholar]
- 19.Toussaint S, Maidl J, Schwagmeier R, Striebel HW. Patient-controlled intranasal analgesia : effective alternative to intravenous PCA for postoperative pain relief. Can J Anaesth. 2000;47:299–302. doi: 10.1007/BF03020941. [DOI] [PubMed] [Google Scholar]
- 20.Van Boerum DH, Smith JT, Curtin MJ. A comparison of the effects of patient-controlled analgesia with intravenous opioids versus epidural analgesia on recovery after surgery for idiopathic scoliosis. Spine (Phila Pa 1976) 2000;25:2355–2357. doi: 10.1097/00007632-200009150-00014. [DOI] [PubMed] [Google Scholar]