Abstract
Most research on birth weight and adult health status has reported adult measures at a single time point. This study examined the relationship of self-reported birth weight to longitudinal changes in adult body composition in 587 women of the Michigan Bone Health and Metabolism Study, followed from 1992 to 2007 and aged 24–50 years at baseline. Linear mixed models were used to estimate the association between three birth weight categories and women’s 15-year changes in adult weight, height, BMI, waist and hip circumference, waist-to-hip ratio, and fat, lean, and skeletal muscle mass. Body composition measures increased in all women over the 15-year study period. At their adult baseline, high birth weight women weighed 13% more and had waist circumference and lean mass measures that were 5.51 cm and 3.91 kg larger, respectively, than normal birth weight women. No differences were observed in adult body composition between low and normal birth weight women and rates of change in the adult measures did not vary across the birth weight groups. Women heavier at birth continued to be heavier through adulthood, corroborating previous reports based on single measures of adult body composition. Research to address whether higher adult body composition in high birth weight women increases the longitudinal risk for obesity-related chronic diseases is needed.
The developmental origins of health and disease theory posits that early life experiences may be associated with adult chronic disease development, including obesity (1–6). Birth weight is a frequently used marker for the early life experience. Earlier studies focused on low birth weight associations (1,7), but recent investigations have expanded to include high birth weight (5,8). However, most studies examined health outcomes at a single time point in adulthood and studies with longitudinally collected adult outcomes, such as weight trajectories, are rare.
We examined the relationship of birth weight in relation to 15-year changes in body composition in a population-based sample of middle-class adult white women. It was hypothesized that adult body composition trajectories would differ among low and high birth weight groups of women compared to women in the normal birth weight group.
Methods and Procedures
The study population was from the Michigan Bone Health and Metabolism Study (MBHMS), a prospective cohort study investigating changes in women’s health prior to and through the menopause (9). Recruitment and enrollment occurred in 1988 and 1992 and, upon completion, comprised 664 women who were aged 24–50 years in 1992. Since 1992, participants have been evaluated annually for 15 years, excluding two time intervals of 13–18-months duration associated with funding lapses. These analyses incorporated data from the 587 (88.4%) MBHMS women for whom birth weight data were available and who were singletons at birth.
At the 1988 enrollment, women self-reported their birth weight. In 2008, active MBHMS participants were contacted to participate in a supplemental telephone-based interview to further characterize their birth history, including birth weights. These interviews gathered additional birth-related characteristics, including mother’s age and smoking behavior at participant’s birth, participant’s birth order, and whether participant was from a singleton birth. Among the 561 participants active in 2008, 82% completed the supplemental birth history interview.
Self-reported birth weight, in grams (g), was categorized based on clinical cut-points: low (<2,500 g); normal (2,500–4,000 g); and high, (>4,000 g). Since there was little variation in the birth weight data collected in 2008 compared to 1988, birth weight reported in 2008 was used only when the 1988 data were missing (n = 74).
Body composition measures (weight, height, waist and hip circumferences, and fat, lean, and skeletal muscle mass) were collected annually. A calibrated stadiometer and balance-beam scales were used to measure height and weight, respectively. BMI was calculated by dividing the weight, in kilograms, by the square of the height, in meters. Using non-stretching tape, waist circumference was measured during expiration at the narrowest section of the torso and hip circumference was evaluated at the widest section of the hip. Waist-to-hip ratio was calculated by dividing waist by hip circumference. Fat, lean, and skeletal muscle mass were collected using measures from bioelectrical impedance (10,11).
Non-normally distributed outcomes were log transformed to satisfy model assumptions and, as appropriate, were back transformed to their original scale to ease interpretation. Linear mixed modeling with repeated measures was used to compare the 15-year adult body composition trajectories of the normal birth weight group to the low and high birth weight groups. Birth weight by time interactions were tested to determine whether the rates of change in the adult body composition measures varied by birth weight category. Models were adjusted for participant’s baseline age. Analyses were completed using SAS v 9.2 (SAS Institute, Cary, NC) and statistical significance was defined as α < 0.05.
Results
In this population of adult women born between the years 1942 and 1967, self-reported birth weight was normally distributed with a mean of 3,289 g and range of 1,531–5,897 g. Most (81.9%) women were in the normal birth weight group (mean = 3,291 g); 9.2% of women were in the low birth weight category (mean = 2,208 g) while 8.9% of women were in the high birth weight group (mean = 4,399 g).
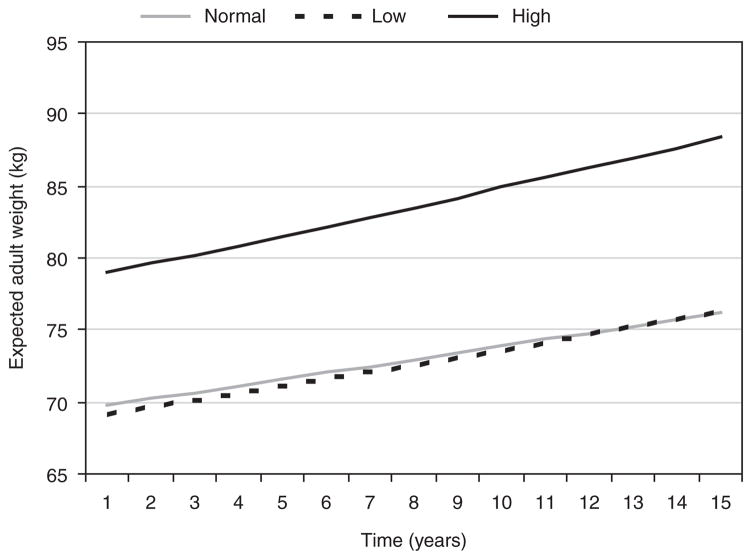
The 15-year trajectories observed from fitted linear mixed models indicated that all women experienced an increase in their body composition measures during adulthood. However, women in the high birth weight group had significantly higher levels of adult weight, height, BMI, waist and hip circumference, and fat, lean, and skeletal muscle mass across the 15-year study period compared to women in the normal birth weight group, before and after adjusting for age. Figure 1 illustrates the 15-year expected adult weight trajectories by birth weight group. The trajectories were similar for all other body composition measures, except waist-to-hip ratio.
Figure 1.
Fifteen-year expected adult weight trajectories by birth weight group in Michigan Bone Health and Metabolism Study women. Normal, low, and high birth weight was defined as 2,500–4,000 g, <2,500 g, and >4,000 g, respectively. Fifteen-year trajectories were adjusted for participant’s age at baseline and were similar in all other body composition measures, except waist-to-hip ratio.
At the study baseline, women in the high birth weight group were, on average, 13% (P < 0.01) heavier and had BMI and fat mass levels that were, on average, 11% (P < 0.01) and 20% (P < 0.01) higher, respectively, than women in the normal birth weight group (Table 1). Similarly, waist circumference and lean mass were an average of 5.51 cm (P < 0.01) and 3.91 kg (P < 0.01) larger, respectively, in high relative to normal birth weight women at baseline.
Table 1.
Fifteen-year longitudinal relationship of birth weight with adult body composition in MBHMS women
| Body composition | Low birth weight (<2,500 g)a |
High birth weight (>4,000 g)a |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Main effectb |
Slopeb |
Main effectb |
Slopeb |
|||||||||
| β | s.e. | P | β | s.e. | P | β | s.e. | P | β | s.e. | P | |
| Log weight (kg) | −0.03 | 0.03 | 0.37 | 0.001 | 0.001 | 0.41 | 0.13 | 0.03 | <0.01 | 0.001 | 0.001 | 0.26 |
| Height (cm) | −1.15 | 0.82 | 0.16 | −0.001 | 0.010 | 0.96 | 1.83 | 0.82 | 0.03 | 0.0003 | 0.010 | 0.97 |
| Log BMI (kg/m2) | −0.01 | 0.03 | 0.73 | 0.001 | 0.001 | 0.42 | 0.10 | 0.03 | <0.01 | 0.001 | 0.001 | 0.27 |
| Waist circumference (cm) | −0.45 | 1.92 | 0.81 | 0.091 | 0.104 | 0.38 | 5.51 | 1.92 | <0.01 | 0.182 | 0.100 | 0.07 |
| Log hip circumference (cm) | −0.005 | 0.02 | 0.77 | 0.0004 | 0.001 | 0.67 | 0.06 | 0.02 | <0.01 | 0.001 | 0.001 | 0.15 |
| Waist-to-hip ratio | −0.003 | 0.01 | 0.75 | 0.001 | 0.001 | 0.34 | 0.01 | 0.01 | 0.49 | 0.0001 | 0.001 | 0.89 |
| Log fat mass (kg) | −0.04 | 0.06 | 0.46 | 0.002 | 0.003 | 0.54 | 0.19 | 0.06 | <0.01 | 0.002 | 0.003 | 0.44 |
| Lean mass (kg) | −0.97 | 0.96 | 0.31 | 0.035 | 0.040 | 0.38 | 3.91 | 0.96 | <0.01 | 0.065 | 0.039 | 0.09 |
| Skeletal muscle mass (kg) | −0.29 | 0.37 | 0.43 | 0.010 | 0.015 | 0.52 | 1.52 | 0.37 | <0.01 | 0.023 | 0.015 | 0.11 |
Adjusted for participant’s age at baseline.
MBMHS, Michigan Bone Health and Metabolism Study.
Women in the low and high birth weight groups were examined relative to women in the normal birth weight group.
The main effect describes the mean difference in the adult body composition measure at baseline relative to the normal birth weight group. The slope is the interaction of birth weight and time and describes the rate of change on the adult body composition measure relative to the normal birth weight group.
Over the 15-year study period, there were no significant differences in adult body composition trajectories between low and normal birth weight women (Figure 1). Marginally significant differences in the rates of change of waist circumference and lean mass were observed when comparing women in the high to the normal birth weight group (Table 1).
Discussion
This population-based study compared middle-class, white women, grouped using clinically defined cut-points for birth weight, for differences in their body composition trajectories as middle-aged adults. Women who were heavier at birth continued to be heavier into adulthood. Mixed modeling identified that rates of change in adult body composition measures did not differ across the birth weight groups. Thus, although high birth weight women had higher adult body composition measures, their rates of body composition change over time were similar to those of normal birth weight women.
This is one of the few studies to examine the relationship between birth weight and annually collected measures of adult body composition over a 15-year time period. The finding that high birth weight women had a greater propensity for higher adult body composition levels corroborates studies that consistently described a positive association between birth weight and weight, BMI, and lean mass later in life. The addition of longitudinal data provided greater insight about the trajectories in adult body composition in women that have not been previously described. Notably, these results suggest that the relative position of body composition trajectories is maintained during young adulthood.
While we found an association with high birth weight and adult fat mass, no relationship was observed with waist-to-hip ratio, suggesting that the higher levels of adipose tissue in the high birth weight group women were not more likely to be centrally distributed. The relationship between birth weight and adult fat mass and waist-to-hip ratio, a marker for central adiposity, has been inconsistently observed. Prior studies reported a positive association between birth weight and fat mass (2,12), while others describe either no association (5,8) or an inverse one (3).
Rapid and excessive postnatal growth in low birth weight infants, particularly within developed countries, has been implicated as a mechanism for increased fat mass in adulthood (6). We reported no statistically significant differences in adult central adiposity and fat mass between low and normal birth weight women, possibly due to healthy weight gain in low birth weight infants after birth, although this hypothesis could not be tested in our study.
Previous research with the capacity to assess birth weight and longitudinal changes in adult body composition is limited. In a 9-year study of Dutch adults followed over four time points, increasing birth weight in females was associated with decreasing subcutaneous fat mass, truncal fat, and waist circumference; however, the highest birth weight tertile remained within the clinically accepted range of normal birth weight (5).
This study examined a population-based sample of white women, born between 1942 and 1967. Although birth weight and adult body composition may be influenced by age and cohort effects, we found no evidence of these effects in our data. Further, most of the MBHMS participants were born and continue to reside in Tecumseh, MI, supporting the lack of evidence of a cohort effect.
The homogeneity of the study population, which permitted minimal concern for selected confounding factors, such as race, socioeconomic status, and social environment, was a study strength. Further, since BMI measures do not differentiate the relative contribution of lean and fat mass (4,6), this study collected lean, skeletal muscle, and fat mass and fat distribution data.
A study limitation was the self-report of birth weight. However, several studies have described the validity of self-reported birth data (13,14). A recent study reported good level of agreement and sensitivity in self-reported birth weight when compared to medical records (13). Self-reported low birth weight may be less sensitive to measurement error than normal or high birth weight (13), so our observation of no association may also arise from the attenuation of effects from measurement error.
In conclusion, these findings indicate that high birth weight was related to subsequently measured higher levels of adult body composition. However, birth weight group assignment was not associated with slopes representing 15-year changes in body composition measures. Our observation that high birth weight was not related with centrally distributed fat mass, despite a positive association with total fat mass, suggests the value in examining whether high birth weight women have a decreased risk for developing chronic diseases in which central adiposity is a prominent risk factor.
Acknowledgments
This work was supported by the National Institutes for Health (grants AR051384, AR040888, and AR-20557 to MF.R.S). The authors thank Mary Crutchfield, Cora Alcock, Angela Crippen, and Megan McFarland for their assistance with the 2008 collection of the birth history data.
Footnotes
Disclosure
The authors declared no conflict of interest.
References
- 1.Barker DJ. In utero programming of chronic disease. Clin Sci. 1998;95:115–128. [PubMed] [Google Scholar]
- 2.Barker M, Robinson S, Osmond C, Barker DJ. Birth weight and body fat distribution in adolescent girls. Arch Dis Child. 1997;77:381–383. doi: 10.1136/adc.77.5.381. [DOI] [PubMed] [Google Scholar]
- 3.Loos RJ, Beunen G, Fagard R, Derom C, Vlietinck R. Birth weight and body composition in young women: a prospective twin study. Am J Clin Nutr. 2002;75:676–682. doi: 10.1093/ajcn/75.4.676. [DOI] [PubMed] [Google Scholar]
- 4.Sayer AA, Cooper C. Fetal programming of body composition and musculoskeletal development. Early Hum Dev. 2005;81:735–744. doi: 10.1016/j.earlhumdev.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Te Velde SJ, Twisk JW, Van Mechelen W, Kemper HC. Birth weight, adult body composition, and subcutaneous fat distribution. Obes Res. 2003;11:202–208. doi: 10.1038/oby.2003.32. [DOI] [PubMed] [Google Scholar]
- 6.Wells JC, Chomtho S, Fewtrell MS. Programming of body composition by early growth and nutrition. Proc Nutr Soc. 2007;66:423–434. doi: 10.1017/S0029665107005691. [DOI] [PubMed] [Google Scholar]
- 7.Eriksson JG, Forsén T, Tuomilehto J, Osmond C, Barker DJ. Early growth and coronary heart disease in later life: longitudinal study. BMJ. 2001;322:949–953. doi: 10.1136/bmj.322.7292.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singhal A, Wells J, Cole TJ, Fewtrell M, Lucas A. Programming of lean body mass: a link between birth weight, obesity, and cardiovascular disease? Am J Clin Nutr. 2003;77:726–730. doi: 10.1093/ajcn/77.3.726. [DOI] [PubMed] [Google Scholar]
- 9.Sowers MF, Zheng H, McConnell D, et al. Testosterone, sex hormone-binding globulin and free androgen index among adult women: chronological and ovarian aging. Hum Reprod. 2009;24:2276–2285. doi: 10.1093/humrep/dep209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boulier A, Fricker J, Thomasset AL, Apfelbaum M. Fat-free mass estimation by the two-electrode impedance method. Am J Clin Nutr. 1990;52:581–585. doi: 10.1093/ajcn/52.4.581. [DOI] [PubMed] [Google Scholar]
- 11.Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol. 2000;89:465–471. doi: 10.1152/jappl.2000.89.2.465. [DOI] [PubMed] [Google Scholar]
- 12.Sachdev HS, Fall CH, Osmond C, et al. Anthropometric indicators of body composition in young adults: relation to size at birth and serial measurements of body mass index in childhood in the New Delhi birth cohort. Am J Clin Nutr. 2005;82:456–466. doi: 10.1093/ajcn.82.2.456. [DOI] [PubMed] [Google Scholar]
- 13.Tehranifar P, Liao Y, Flom JD, Terry MB. Validity of self-reported birth weight by adult women: sociodemographic influences and implications for life-course studies. Am J Epidemiol. 2009;170:910–917. doi: 10.1093/aje/kwp205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Troy LM, Michels KB, Hunter DJ, et al. Self-reported birthweight and history of having been breastfed among younger women: an assessment of validity. Int J Epidemiol. 1996;25:122–127. doi: 10.1093/ije/25.1.122. [DOI] [PubMed] [Google Scholar]