Abstract
Polycystic ovary syndrome (PCOS) is recognized as the most common endocrinopathy in reproductive-aged women. The symptoms of PCOS vary with age, race, weight, and medications, adding to the challenges of accurate diagnosis. Adolescent patients pose particular diagnostic problems because characteristics of normal puberty often overlap with signs and symptoms of PCOS. This article reviews the diagnosis of PCOS in adolescents.
Key words: Polycystic ovary syndrome, Endocrinopathy, Menstrual irregularity, Hyperandrogenism, Hyperinsulinemia
In 1935, Stein and Leventhal published a case series of seven women with amenorrhea, hirsutism, and bilateral polycystic ovaries, a condition that later came to be known as polycystic ovary syndrome (PCOS).1 PCOS is now recognized as the most common endocrinopathy in reproductive-aged women (affecting 5%–7%), with key features of menstrual irregularity, elevated androgens, and polycystic-appearing ovaries. Since its original description in 1935, however, the definition of PCOS has undergone several revisions (Table 1).
Table 1.
PCOS Definitions 1990–2009
| PCOS Definition | Clinical Hyperandrogenism (Ferriman-Gallwey Score ≥ 8) or Biochemical Hyperandrogenism (Elevated Total/Free Testosterone) | Oligomenorrhea (Less Than 6-9 Menses per Year) or Oligo-Ovulation | Polycystic Ovaries on Ultrasound (≥ 12 Antral Follicles in One Ovary or Ovarian Volume ≥ 10 cm3) |
| NICHD (1990)2 | Yes | Yes | No |
| Rotterdam (2003)3 | Yes | Yes | Yes |
| 2 of 3 criteria | |||
| AE-PCOS Society (2009)4 | Yes | Yes | Yes |
| 1 of 2 criteria |
AE-PCOS, androgen excess and polycystic ovary syndrome; NICHD, Eunice Kennedy Shriver National Institute of Child Health and Human Development; PCOS, polycystic ovary syndrome.
At the National Institutes of Health (NIH) consensus conference held in 1990, PCOS was defined as chronic anovulation with clinical and/or biochemical hyperandrogenism, with exclusion of other mimicking etiologies, such as thyroid or adrenal dysfunction.2 In 2003, the Rotterdam European Society for Human Reproduction/American Society of Reproductive Medicine (ESHRE/ASRM)-sponsored PCOS consensus workshop group proposed that the diagnosis include two of the following three criteria: oligo- and/or anovulation, clinical and/or biochemical hyperandrogenism, and polycystic ovaries on ultrasound; other etiologies must be excluded.3 By adding the polycystic ovaries criterion, the Rotterdam definition extended the diagnosis of PCOS to women with oligo-ovulation and polycystic ovaries (nonhyperandrogenic), as well as to women with hyperandrogenism and polycystic ovaries (ovulatory), both of whom would not have met the narrower NIH criteria for PCOS. Some have argued that the expanded Rotterdam criteria can result in an overdiagnosis or misdiagnosis of PCOS; more importantly, these different phenotypes may not have similar risks of long-term metabolic morbidities.
Most recently, in 2009, the Androgen Excess and PCOS (AE-PCOS) Society published a task force report emphasizing that PCOS is primarily a hyperandrogenic disorder and proposed revising the definition to hyperandrogenism (hirsutism and/or hyperandrogenemia) and ovarian dysfunction (oligo-anovulation and/or polycystic ovaries), thereby encompassing the Rotterdam ultrasound criteria but requiring hyperandrogenism for the diagnosis (Table 1).4 None of the above groups has proposed different criteria for diagnosis of PCOS in the adolescent population.
The symptoms of PCOS vary with age, race, weight, and medications, adding to the challenges of accurate diagnosis. In adolescent patients, the criteria described above pose particular diagnostic problems because characteristics of normal puberty often overlap with signs and symptoms of PCOS. Therefore, different diagnostic criteria for adolescent PCOS have been proposed by some authors. Sultan and Paris5 recommended that the adolescent girl meet four of the five following criteria: oligo- or amenorrhea > 2 years after menarche, clinical hyperandrogenism, biochemical hyperandrogenism, insulin resistance or hyperinsulinemia, and polycystic ovaries on ultrasound. Carmina and colleagues6 suggested applying the Rotterdam criteria, but limiting definitive diagnosis to the adolescent patient who met all three criteria. These authors suggest that adolescents who exhibit only two of the three criteria may well be diagnosed with PCOS as adults and therefore their symptoms should be followed and reevaluated. These proposed adolescent criteria are stricter than their adult counterparts, may limit inappropriate early diagnosis, but are currently not endorsed by expert panels or societies in the field.
Hormonal Changes in Normal Puberty and the Pathophysiology of PCOS
Puberty is initiated with the maturation of the hypothalamic-pituitaryovarian axis and secretion of gonadotrophin-releasing hormone (GnRH), whose activity is suppressed during childhood. Varying GnRH pulse frequencies trigger the pituitary to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which stimulate ovarian theca and granulosa cells, respectively. Theca cells produce androstenedione, which nearby granulosa cells aromatize into estradiol. The resulting estrogenic changes during puberty include breast development, bone growth, and fat deposition. During this period the adrenal gland also releases increasing amounts of androgens, such as dehydroepiandrosterone (DHEA) and DHEA sulfate (DHEAS), which are responsible for the development of pubic and axillary hair, as well as acne. The subsequent increase in ovarian androgens also facilitates the development of sexual hair growth.
Although the exact etiology of PCOS is unclear, androgen excess is proposed to be a core defect. Increased androgen levels, primarily produced by the ovaries (with a smaller contribution from the adrenals and peripheral adipose tissue) interfere with hypothalamic sensitivity to negative feedback from the ovary, thereby increasing GnRH pulse frequency.7 This persistently rapid pulse frequency favors increased LH secretion,8 which in turn stimulates the ovarian theca cells to produce more androgens. The relative decrease in FSH secretion leads to less aromatization of androgens to estradiol and impaired follicular development, resulting in the prolonged periods of oligomenorrhea that are characteristic of PCOS.
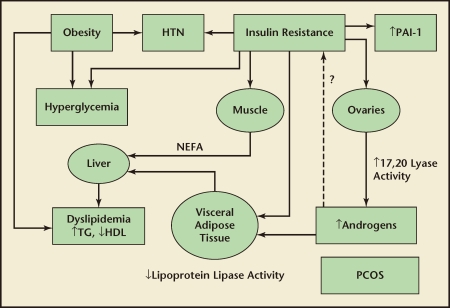
Like the central features of PCOS, certain metabolic changes that are associated with PCOS are also physiologic during puberty. Hyperinsulinemia is common in healthy adolescents; insulin sensitivity decreases by about 50% and there is a compensatory rise in insulin secretion, which later returns to prepubertal levels in adulthood.9,10 However, both insulin resistance and hyperinsulinemia are more severe in adolescents with PCOS compared with the general adolescent population.11 Insulin stimulates ovarian theca cell synthesis of androgens12 and inhibits hepatic production of sex hormone-binding globulin.13 Together, these effects result in increased circulating free androgen levels, thus perpetuating the underlying pathophysiology of PCOS. In addition, insulin resistance promotes release of nonesterified fatty acids from the liver and adipose tissue due to decreased lipoprotein lipase activity, which contributes to the dyslipidemia that is associated with PCOS (Figure 1).
Figure 1.
Pathophysiology of metabolic risks in polycystic ovary syndrome (PCOS). HDL, high-density lipoprotein; HTN, hypertension; NEFA, nonesterified fatty acids; PAI-1, plasminogen activator inhibitor 1; TG, triglycerides.
Diagnosis of PCOS in the Adolescent
Currently, adolescents are diagnosed with PCOS by the same criteria described previously for adults (Table 1). The workup includes both laboratory and ultrasound testing (Table 2).
Table 2.
Testing in Adolescents Presenting with PCOS-Like Symptoms
| TSH |
| Prolactin |
| Total and free testosterone |
| DHEAS |
| 17-OH progesterone |
| Ultrasound of ovaries (not essential if other 2 criteria are met) |
| FSH, LH, estradiol (in amenorrheic adolescents) |
| Once PCOS has been confirmed |
| Fasting and 2-hour GTT |
| Lipid panel |
| Fasting insulin |
DHEAS, dehydroepiandrosterone sulfate; FSH, follicle-stimulating hormone; GTT, glucose tolerance test; PCOS, polycystic ovary syndrome; LH, luteinizing hormone; TSH, thyroid-stimulating hormone.
Irregular Menses
Menstrual irregularity is a common feature of PCOS, occurring in more than 75% of the adult PCOS population,14 and is often the earliest clinical manifestation in the adolescent.15 It is defined as menses that occur at intervals of greater than 6 to 8 weeks in the absence of thyroid, adrenal, or other pituitary dysfunction. This menstrual pattern can be difficult to distinguish from anovulation associated with puberty because the hypothalamicpituitary- ovarian axis matures progressively over a period of several years after menarche. Although many adolescents establish regular cycles by 2 years postmenarche, irregularity may continue beyond that time period, often without cause for clinical concern.16 In a longitudinal study of 112 adolescents, 65% had established a pattern of > 10 menses per year after 1 year postmenarche and > 90% had > 10 menses per year at the end of 3 years postmenarche.17 The age of onset of menstruation also determines the age at which ovulatory cycles are established; in girls who begin menstruation at age < 12, 12 to 13, and > 13 years, 50% of cycles are ovulatory by 1, 3, and 4.5 years, respectively.18 Van Hooff and colleagues19 observed a cohort of adolescents from the general population and reported that oligomenorrhea at age 15 was the best predictor of oligomenorrhea 3 years later, with 51% of these oligomenorrheic girls remaining so at follow-up. On the other hand, only 2% of adolescents with regular menstrual cycles and 12% of those with slightly irregular menstrual cycles (average cycle length between 22 and 41 days), went on to develop oligomenorrhea subsequently. Although irregular menstrual cycles cannot be the sole criterion for PCOS, they comprise an important symptom that should be followed in the adolescent. When oligomenorrhea is persistent or presents in conjunction with symptoms of androgen excess, further evaluation for PCOS is recommended (Table 2).
Androgen Excess
Androgen excess plays an important role in the pathophysiology of PCOS and has been hypothesized to be the final common pathway for the development of the signs and symptoms of this disorder. The majority (> 80%) of adults with PCOS have hyperandrogenemia.14 In the adolescent, clinical evidence of androgen excess, such as severe acne or hirsutism, may prompt evaluation for PCOS. But although acne may be the presenting symptom of underlying hyperandrogenism,20 it is too commonplace in the adolescent population to be used alone as a criterion for clinical hyperandrogenism. Over 90% of 18-year-old women have some form of acne, and 23% have acne requiring pharmacotherapy, the prevalence of which declines in adulthood.21 The presence of severe acne in the adolescent population has been shown to correlate with DHEAS levels and to a lesser extent with total and free testosterone levels.22 Hirsutism may be a more reliable marker of hyperandrogenism in adolescents, and occurs in approximately 60% of adult women with PCOS.14 Hirsutism is often less prominent during the adolescent period compared with adulthood as hair growth becomes thick and coarse with increasing duration of androgen exposure.23 To quantify hirsutism, the modified Ferriman-Gallwey scoring system should be used, although there are no separate diagnostic cutoffs in adolescents (Table 2). There is little information on the prevalence of androgenic alopecia in adults, and even less in the adolescent population.
Given the low reliability of these clinical symptoms of hyperandrogenism, increased serum androgen levels provide the best measure of androgen excess in the adolescent. Although there is a physiologic increase in androgen levels during normal puberty, biochemical hyperandrogenemia remains a defining feature of PCOS. Elevated free testosterone is the most frequent abnormal biochemical finding, although total testosterone and DHEAS may also be elevated.24 Currently, there are no androgen ranges specific to the adolescent population that may be used to establish the diagnosis of PCOS. As in adults, using a sensitive testosterone assay is important. The AE-PCOS Society recommends using mass spectrometry for the measurement of total testosterone.4
Polycystic Ovaries
Ovarian morphology was introduced as one of the Rotterdam diagnostic criteria for PCOS (Table 2) and has received criticism for broadening the definition of PCOS. Indeed, PCOS and control populations share a significant overlap in ovarian morphology, and a large proportion (estimates range from 10%–48%) of adolescents who do not have PCOS may have polycystic-appearing ovaries.25–27 Nevertheless, polycystic ovaries per se have been linked to both menstrual irregularity and hyperandrogenism.28 Van Hooff and colleagues29 observed polycystic ovaries in 9% of adolescent girls with regular menstrual cycles, in 28% with irregular cycles (average cycle length between 22 and 41 days), and in 45% with oligomenorrhea and found a similar association with higher androgen levels.
Diagnosis of polycystic ovaries poses additional difficulties in the adolescent population. First, ovarian appearance and volume may vary during adolescence; it has been reported that ovaries can develop a polycystic morphology over time, and enlarged ovaries with a polycystic appearance can subsequently become normal in size.30 Second, transabdominal ultrasound is preferred to the transvaginal approach in adolescent girls, but this approach may be technically limited in overweight and obese individuals. These challenges to ultrasound evaluation make this diagnostic criterion much less useful in the adolescent. Recent studies have suggested magnetic resonance imaging (MRI) as a potentially more accurate modality to evaluate the ovaries,31 but currently transabdominal ultrasound remains the primary imaging tool in this population.
Metabolic Risk in Adolescent PCOS
Once the diagnosis of PCOS has been established in an adolescent girl, she should be screened for metabolic abnormalities. Although not part of the definition of PCOS, metabolic dysfunction constitutes an important risk associated with PCOS, and it can manifest at an early age. Acanthosis nigricans (pigmentation of the skin creases on the nape of the neck and underarms) and truncal obesity are clinical surrogates for insulin resistance. One-third of adolescents with PCOS meet criteria for metabolic syndrome- a constellation of risk factors including obesity, dyslipidemia, hypertension, and glucose intolerance-compared with approximately 5% of adolescents from the general population.32,33 Different criteria have been published for the diagnosis of metabolic syndrome in adolescents (Table 3). Coviello and colleagues32 reported an association between PCOS and metabolic syndrome independent of body mass index (BMI); obese adolescents with PCOS had a greater prevalence of metabolic syndrome than obese adolescents without PCOS. As with adults, adolescents of European descent have lower prevalence rates for metabolic syndrome- 9% in Italy and 11% in Turkey compared with no cases of metabolic syndrome among controls in the latter study.34,35 The increased prevalence of metabolic syndrome at such a young age underscores the importance of regular screening of this population to decrease the future risk of diabetes and coronary artery disease.
Table 3.
Pediatric ATP III Diagnostic Criteria for Metabolic Syndrome in Adolescents (3 of 5 criteria)
| Blood glucose > 100 mg/dL |
| HDL-C < 40 mg/dL |
| Triglycerides ≥ 110 mg/dL |
| Waist circumference ≥ 90th percentile for age and sex |
| Blood pressure ≥ 90th percentile for age and sex |
ATP III, Adult Treatment Panel III; HDL-C, high-density lipoprotein cholesterol.
Abdominal obesity is common in PCOS and is associated with greater metabolic dysfunction in adolescents with PCOS.36 Obesity also modulates the development and course of PCOS and a high BMI predicts persistent oligomenorrhea.19 Although obesity may be a better predictor of metabolic dysfunction than PCOS status,37,38 androgen excess may also increase the risk for metabolic syndrome independent of obesity.32,34 Within a cohort of adolescents diagnosed with PCOS, hyperandrogenic subgroups exhibited the highest degree of insulin resistance and inflammation.33 Lipid abnormalities have also been reported in adolescents with PCOS; triglycerides and low-density lipoprotein cholesterol levels were higher in hyperandrogenic phenotypes, as compared with other PCOS subgroups.34 The risks of impaired glucose tolerance and type 2 diabetes are also increased in adolescents with PCOS.39,40 Although these studies are small and the overall risk low, they emphasize the need to screen this population at regular intervals. The AE-PCOS Society currently recommends all women with PCOS, including adolescents, be screened using the 2-hour glucose tolerance test and a complete lipid profile (Table 2).41
Conclusions
Although the diagnosis of PCOS in adolescent girls can be difficult given its strong association with metabolic syndrome, a complete evaluation is indicated. Hyperandrogenemia is often the most reliable finding in this age group, and it may be prudent to define adolescent PCOS according to the AE-PCOS Society criteria. The current epidemic of childhood obesity may increase the severity of symptoms of PCOS and underscores the importance of its early and accurate diagnosis. In patients with welldefined hyperandrogenemia, a metabolic workup should be performed. Additionally, given the evidence for PCOS as a complex genetic disorder with familial clustering, it is important to ascertain the family history for both PCOS and metabolic disease. In the adolescent where the diagnosis is not clear, it is preferable to follow the symptoms and repeat the evaluation in 6 to 12 months.
Main Points.
Adolescents are diagnosed with polycystic ovary syndrome (PCOS) using the same criteria for adults.
Menstrual irregularity is a common feature of PCOS and is often the earliest clinical manifestation in the adolescent. However, this menstrual pattern can be difficult to distinguish from anovulation associated with puberty because the hypothalamic-pituitaryovarian axis matures progressively over a period of several years after menarche.
Clinical evidence of androgen excess, such as severe acne or hirsutism, may prompt evaluation for PCOS. Given the low reliability of these clinical symptoms of hyperandrogenism, increased serum androgen levels provide the best measure of androgen excess in the adolescent.
Diagnosis of polycystic ovaries poses additional difficulties in the adolescent population. Ovarian appearance and volume may vary during adolescence and transabdominal ultrasound is preferred to the transvaginal approach in adolescent girls; however, this approach may be technically limited in overweight and obese individuals. These challenges to ultrasound evaluation make this diagnostic criterion much less useful in the adolescent.
The current epidemic of childhood obesity may increase the severity of symptoms of PCOS and underscores the importance of its early and accurate diagnosis. In patients with well-defined hyperandrogenemia, a metabolic workup should be performed. Additionally, given the evidence for PCOS as a complex genetic disorder with familial clustering, it is important to ascertain the family history for both PCOS and metabolic disease.
References
- 1.Stein IF, Leventhal ML. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol. 1935;29:181–191. [Google Scholar]
- 2.Zawadski JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In: Dunaif A, Givens JR, Haseltine FP, Merriam GR, editors. Polycystic Ovary Syndrome. Boston: Blackwell Scientific Publications; 1992. pp. 377–384. [Google Scholar]
- 3.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group, authors. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Azziz R, Carmina E, Dewailly D, et al. Task Force on the Phenotype of the Polycystic Ovary Syndrome of The Androgen Excess and PCOS Society. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91:456–488. doi: 10.1016/j.fertnstert.2008.06.035. [DOI] [PubMed] [Google Scholar]
- 5.Sultan C, Paris F. Clinical expression of polycystic ovary syndrome in adolescent girls. Fertil Steril. 2006;86(suppl 1):S6. doi: 10.1016/j.fertnstert.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 6.Carmina E, Oberfield SE, Lobo RA. The diagnosis of polycystic ovary syndrome in adolescents. Am J Obstet Gynecol. 2010;203:201.e1–201.e5. doi: 10.1016/j.ajog.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Waldstreicher J, Santoro NF, Hall JE, et al. Hyperfunction of the hypothalamic-pituitary axis in women with polycystic ovarian disease: indirect evidence for partial gonadotroph desensitization. J Clin Endocrinol Metab. 1988;66:165–172. doi: 10.1210/jcem-66-1-165. [DOI] [PubMed] [Google Scholar]
- 8.Venturoli S, Porcu E, Fabbri R, et al. Longitudinal evaluation of the different gonadotropin pulsatile patterns in anovulatory cycles of young girls. J Clin Endocrinol Metab. 1992;74:836–841. doi: 10.1210/jcem.74.4.1548348. [DOI] [PubMed] [Google Scholar]
- 9.Caprio S, Plewe G, Diamond MP, et al. Increased insulin secretion in puberty: a compensatory response to reductions in insulin sensitivity. J Pediatr. 1989;114:963–967. doi: 10.1016/s0022-3476(89)80438-x. [DOI] [PubMed] [Google Scholar]
- 10.Hannon TS, Janosky J, Arslanian SA. Longitudinal study of physiologic insulin resistance and metabolic changes of puberty. Pediatr Res. 2006;60:759–763. doi: 10.1203/01.pdr.0000246097.73031.27. [DOI] [PubMed] [Google Scholar]
- 11.Lewy VD, Danadian K, Witchel SF, Arslanian S. Early metabolic abnormalities in adolescent girls with polycystic ovarian syndrome. J Pediatr. 2001;138:38–44. doi: 10.1067/mpd.2001.109603. [DOI] [PubMed] [Google Scholar]
- 12.Nestler JE, Jakubowicz DJ, de Vargas AF, et al. Insulin stimulates testosterone biosynthesis by human thecal cells from women with polycystic ovary syndrome by activating its own receptor and using inositolglycan mediators as the signal transduction system. J Clin Endocrinol Metab. 1998;83:2001–2005. doi: 10.1210/jcem.83.6.4886. [DOI] [PubMed] [Google Scholar]
- 13.Nestler JE, Powers LP, Matt DW, et al. A direct effect of hyperinsulinemia on serum sex hormonebinding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991;72:83–89. doi: 10.1210/jcem-72-1-83. [DOI] [PubMed] [Google Scholar]
- 14.Azziz R, Carmina E, Dewailly D, et al. Androgen Excess Society. Position statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. 2006;91:4237–4245. doi: 10.1210/jc.2006-0178. [DOI] [PubMed] [Google Scholar]
- 15.Avvad CK, Holeuwerger R, Silva VC, et al. Menstrual irregularity in the first postmenarchal years: an early clinical sign of polycystic ovary syndrome in adolescence. Gynecol Endocrinol. 2001;15:170–177. [PubMed] [Google Scholar]
- 16.Gardner J. Adolescent menstrual characteristics as predictors of gynaecological health. Ann Hum Biol. 1983;10:31–40. doi: 10.1080/03014468300006161. [DOI] [PubMed] [Google Scholar]
- 17.Legro RS, Lin HM, Demers LM, Lloyd T. Rapid maturation of the reproductive axis during perimenarche independent of body composition. J Clin Endocrinol Metab. 2000;85:1021–1025. doi: 10.1210/jcem.85.3.6423. [DOI] [PubMed] [Google Scholar]
- 18.Apter D, Vihko R. Early menarche, a risk factor for breast cancer, indicates early onset of ovulatory cycles. J Clin Endocrinol Metab. 1983;57:82–86. doi: 10.1210/jcem-57-1-82. [DOI] [PubMed] [Google Scholar]
- 19.van Hooff, Voorhorst FJ, Kaptein MB, et al. Predictive value of menstrual cycle pattern, body mass index, hormone levels and polycystic ovaries at age 15 years for oligo-amenorrhoea at age 18 years. Hum Reprod. 2004;19:383–392. doi: 10.1093/humrep/deh079. [DOI] [PubMed] [Google Scholar]
- 20.Slayden SM, Moran C, Sams WM Jr, et al. Hyperandrogenemia in patients presenting with acne. Fertil Steril. 2001;75:889–892. doi: 10.1016/s0015-0282(01)01701-0. [DOI] [PubMed] [Google Scholar]
- 21.Cunliffe WJ, Gould DJ. Prevalence of facial acne vulgaris in late adolescence and in adults. Br Med J. 1979;1:1109–1110. doi: 10.1136/bmj.1.6171.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lucky AW, Biro FM, Simbartl LA, et al. Predictors of severity of acne vulgaris in young adolescent girls: results of a five-year longitudinal study. J Pediatr. 1997;130:30–39. doi: 10.1016/s0022-3476(97)70307-x. [DOI] [PubMed] [Google Scholar]
- 23.Pfeifer SM, Kives S. Polycystic ovary syndrome in the adolescent. Obstet Gynecol Clin North Am. 2009;36:129–152. doi: 10.1016/j.ogc.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Chang WY, Knochenhauer ES, Bartolucci AA, Azziz R. Phenotypic spectrum of polycystic ovary syndrome: clinical and biochemical characterization of the three major clinical subgroups. Fertil Steril. 2005;83:1717–1723. doi: 10.1016/j.fertnstert.2005.01.096. [DOI] [PubMed] [Google Scholar]
- 25.Bridges NA, Cooke A, Healy MJ, et al. Standards for ovarian volume in childhood and puberty. Fertil Steril. 1993;60:456–460. [PubMed] [Google Scholar]
- 26.Mortensen M, Rosenfield RL, Littlejohn E. Functional significance of polycystic-size ovaries in healthy adolescents. J Clin Endocrinol Metab. 2006;91:3786–3790. doi: 10.1210/jc.2006-0835. [DOI] [PubMed] [Google Scholar]
- 27.Blank SK, Helm KD, McCartney CR, Marshall JC. Polycystic ovary syndrome in adolescence. Ann N Y Acad Sci. 2008;1135:76–84. doi: 10.1196/annals.1429.005. [DOI] [PubMed] [Google Scholar]
- 28.Fernandes AR, de Sá Rosa e Silva, Romão GS, et al. Insulin resistance in adolescents with menstrual irregularities. J Pediatr Adolesc Gynecol. 2005;18:269–274. doi: 10.1016/j.jpag.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 29.van Hooff, Voorhorst FJ, Kaptein MB, et al. Polycystic ovaries in adolescents and the relationship with menstrual cycle patterns, luteinizing hormone, androgens, and insulin. Fertil Steril. 2000;74:49–58. doi: 10.1016/s0015-0282(00)00584-7. [DOI] [PubMed] [Google Scholar]
- 30.Venturoli S, Porcu E, Fabbri R, et al. Longitudinal change of sonographic ovarian aspects and endocrine parameters in irregular cycles of adolescence. Pediatr Res. 1995;38:974–980. doi: 10.1203/00006450-199512000-00024. [DOI] [PubMed] [Google Scholar]
- 31.Yoo RY, Sirlin CB, Gottschalk M, Chang RJ. Ovarian imaging by magnetic resonance in obese adolescent girls with polycystic ovary syndrome: a pilot study. Fertil Steril. 2005;84:985–995. doi: 10.1016/j.fertnstert.2005.04.039. [DOI] [PubMed] [Google Scholar]
- 32.Coviello AD, Legro RS, Dunaif A. Adolescent girls with polycystic ovary syndrome have an increased risk of the metabolic syndrome associated with increasing androgen levels independent of obesity and insulin resistance. J Clin Endocrinol Metab. 2006;91:492–497. doi: 10.1210/jc.2005-1666. [DOI] [PubMed] [Google Scholar]
- 33.Alemzadeh R, Kichler J, Calhoun M. Spectrum of metabolic dysfunction in relationship with hyperandrogenemia in obese adolescent girls with polycystic ovary syndrome. Eur J Endocrinol. 2010;162:1093–1099. doi: 10.1530/EJE-10-0205. [DOI] [PubMed] [Google Scholar]
- 34.Fruzzetti F, Perini D, Lazzarini V, et al. Adolescent girls with polycystic ovary syndrome showing different phenotypes have a different metabolic profile associated with increasing androgen levels. Fertil Steril. 2009;92:626–634. doi: 10.1016/j.fertnstert.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 35.Vural B, Caliskan E, Turkoz E, et al. Evaluation of metabolic syndrome frequency and premature carotid atherosclerosis in young women with polycystic ovary syndrome. Hum Reprod. 2005;20:2409–2413. doi: 10.1093/humrep/dei100. [DOI] [PubMed] [Google Scholar]
- 36.Bruni V, Dei M, Nannini S, et al. Polycystic ovary syndrome in adolescence. Ann N Y Acad Sci. 2010;1205:175–184. doi: 10.1111/j.1749-6632.2010.05648.x. [DOI] [PubMed] [Google Scholar]
- 37.Rossi B, Sukalich S, Droz J, et al. Prevalence of metabolic syndrome and related characteristics in obese adolescents with and without polycystic ovary syndrome. J Clin Endocrinol Metab. 2008;93:4780–4786. doi: 10.1210/jc.2008-1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fulghesu A, Magnini R, Portoghese E, et al. Obesity-related lipid profile and altered insulin incretion in adolescents with polycystic ovary syndrome. J Adolesc Health. 2010;46:474–481. doi: 10.1016/j.jadohealth.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 39.Sawathiparnich P, Weerakulwattana L, Santiprabhob J, Likitmaskul S. Obese adolescent girls with polycystic ovary syndrome (PCOS) have more severe insulin resistance measured by HOMA-IR score than obese girls without PCOS. J Med Assoc Thai. 2005;88(suppl 8):S33–S37. [PubMed] [Google Scholar]
- 40.Leibel NI, Baumann EE, Kocherginsky M, Rosenfield RL. Relationship of adolescent polycystic ovary syndrome to parental metabolic syndrome. J Clin Endocrinol Metab. 2006;91:1275–1283. doi: 10.1210/jc.2005-1707. [DOI] [PubMed] [Google Scholar]
- 41.Salley KE, Wickham EP, Cheang KI, et al. Glucose intolerance in polycystic ovary syndrome-a position statement of the Androgen Excess Society. J Clin Endocrinol Metab. 2007;92:4546–4556. doi: 10.1210/jc.2007-1549. [DOI] [PubMed] [Google Scholar]