Abstract
The generation of recombinant enhanced green fluorescent protein (EGFP)--expressing viruses has significantly improved the study of their life cycle and opened up the possibility for the rapid screening of antiviral drugs. Here we report rescue of a recombinant Marburg virus (MARV) expressing EGFP from an additional transcription unit (ATU). The ATU was inserted between the second and third genes, encoding VP35 and VP40, respectively. Live-cell imaging was used to follow virus spread in real time. EGFP expression was detected at 32 hours postinfection (hpi), and infection of neighboring cells was monitored at 55 hpi. Compared to the parental virus, production of progeny rMARV-EGFP was reduced 4-fold and lower protein levels of VP40, but not nucleoprotein, were observed, indicating a decrease in downstream protein expression due to the insertion of an ATU. Interestingly, EGFP concentrated in viral inclusions in infected cells. This was reproduced by transient expression of both EGFP and other fluorescent proteins along with filovirus nucleocapsid proteins, and may suggest that a general increase in protein synthesis occurs at viral inclusion sites. In conclusion, the EGFP-expressing MARV will be a useful tool not only to monitor virus spread and screen for antiviral compounds, but also to investigate the biology of inclusion body formation.
Marburg virus (MARV) and the closely related Ebola virus (EBOV) belong to the filovirus family and cause a severe hemorrhagic fever in humans, with mortality rates up to 90%. Currently, there is no approved vaccine or antiviral treatment.
Filoviruses have a nonsegmented negative-sense RNA genome encoding 7 structural proteins. Four of these proteins constitute the nucleocapsid complex, containing the nucleoprotein (NP), the viral polymerase L, the polymerase cofactor VP35, and the viral protein VP30 in close association with the viral genome (for review, see [1]). Cytoplasmic inclusions, which are thought to represent active sites of viral replication, are present as large aggregates in filovirus-infected cells. These inclusions are formed by all 4 nucleocapsid proteins, with NP being the driving force for aggregation due to self-assembly of NP [2, 3]. NP interacts with VP35, VP30, and L, either directly or via a linker protein, thereby redirecting the nucleocapsid proteins into cytoplasmic aggregates [4–8].
Rescue systems to recover infectious virus from full-length complementary DNA (cDNA) clones have been established for both MARV and EBOV [9–13]. These techniques were used to generate recombinant forms of EBOV, derived from isolates of the Zaire ebolavirus (ZEBOV) species, containing the enhanced green fluorescent protein (EGFP) gene within an additional transcription unit (ATU), which provide a sensitive and quantitative readout for antiviral drug screening assays and virus spread studies [14–21]. EGFP was efficiently expressed over 10 passages, confirming the stability of the EBOV constructs [15].
In this study, we rescued a recombinant MARV from a clone containing an ATU encoding EGFP. This clone allows for the visualization of MARV spread in infected cells and was used to assess the localization of EGFP and nucleocapsid proteins in infected cells.
MATERIALS AND METHODS
Cell Lines and Viruses
Vero E6 (African green monkey kidney), HT-1080 (human fibrosarcoma), and U2OS (human osteosarcoma) were maintained in Dulbecco’s modified Eagle’s medium supplemented with penicillin (50 units/mL), streptomycin (50 mg/mL), and 10% fetal calf serum (FCS). MARV strain Musoke and recombinant Marburg viruses were propagated in Vero E6 cells as described previously [9]. All work with infectious MARV was performed under biosafety level 4 conditions at the Institute of Virology, Philipps University of Marburg, Marburg, Germany.
Generation of an Infectious MARV Clone Expressing EGFP
The MARV strain Musoke cDNA clone pMARV(+) described in [9] was used as a template to insert an ATU encoding EGFP between the second and third genes. The intergenic region between VP35 and VP40 genes spanning 5 nucleotides (CTATG) was mutated by in vitro mutagenesis, generating an AvrII restriction site (CCTAGG; inserted or substituted nucleotides underlined). The AvrII restriction site was then used to insert the ATU consisting of the EGFP open reading frame (ORF) flanked by authentic MARV transcription start and stop signals [22]. Virus rescue was performed as previously described [10].
Stable integration of the ATU in the viral genome was verified by reverse transcription–polymerase chain reaction (RT-PCR). Vero E6 cells were infected with rMARV-EGFP and total RNA was isolated from cells and supernatants at 6 days postinfection (dpi) using TRIZOL reagent (Invitrogen). The isolated RNA was subjected to RT-PCR (OneStep RT-PCR, Qiagen) using primers flanking a 362–base pair (bp) PCR fragment of the EGFP gene.
Transfections
HT-1080 cells, grown on glass coverslips, were transfected using FuGeneHD (Roche), and U2OS cells were transfected using TransIT-LT1 (Mirus) according to the suppliers’ protocols. Unless otherwise stated, cells were transfected with 50 ng expression plasmid for EGFP, or red fluorescent proteins TagRFP, DsRed, or mCherry in the absence of or along with plasmids encoding NP (500 ng) and VP35 (500 ng).
Immunofluorescence Analysis of Infected Cells
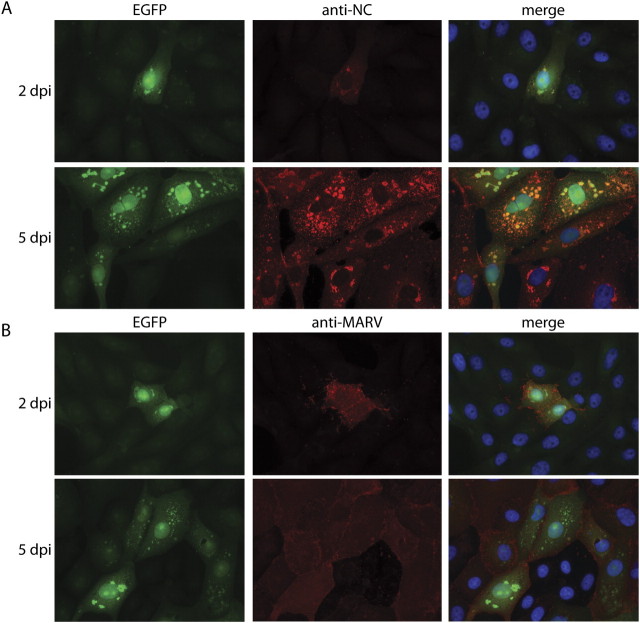
105 Vero E6 cells per well of a 6-well plate were infected with rMARV-EGFP at a multiplicity of infection (MOI) of 0.05. At 2 and 5 dpi, cells were fixed in 4% (w/v) paraformaldehyde for at least 24 hours and permeabilized with a mixture of acetone and methanol (1:1, v/v) for 5 minutes at −20°C. As primary antibodies, a rabbit antiserum directed against the nucleocapsid complex of MARV (anti-NC antiserum) or a goat anti-MARV antiserum were used. Antibody binding was visualized by using Alexa Fluor 568-conjugated and Alexa Fluor 594-labeled secondary antibodies (Invitrogen). In addition, the cells were stained with 100 ng/mL 4′-6-diamidino-2-phenylindole (DAPI) for 10 minutes.
Virus titration was performed by counting foci of infected cells. Vero E6 cells were infected with recombinant MARV at an MOI of 0.05. Supernatants were collected at 2 and 6 dpi, purified by low-speed centrifugation, and 500 μL of the supernatants was used for infection of 105 Vero E6 cells per well of a 6-well plate. Cells were fixed and permeabilized at 2 dpi as described above. Staining of infected cells was performed using the anti-NC antiserum. Foci of infected cells were counted by UV fluorescence microscopy.
Immunofluorescence Analysis of Transfected Cells
HT-1080 or U2OS cells were transfected as described above and subjected to immunofluorescence analysis at 1 day post transfection (dpt). Cells were fixed with 4% (w/v) paraformaldehyde and permeabilized with 0.1% (v/v) Triton X100. A MARV anti-NC rabbit antiserum was used to detect MARV proteins. For the detection of ZEBOV and Reston ebolavirus (REBOV) proteins, a goat anti-ZEBOV serum that cross-reacts with REBOV NP was used. Alexa Fluor 594–conjugated antibodies were used for visualization. The cell nuclei were stained with DAPI.
Western Blot Analysis
Vero E6 cells seeded in 6-well plates were infected with recombinant MARV at an MOI of 0.05. At 2 and 5 dpi, cells were scraped into 200 μL radioimmunoprecipitation assay (RIPA) buffer (20 mM Tris–HCl, pH 7.5; 150 mM NaCl; 10 mM EDTA; 0.1% (w/v) SDS; 1% (v/v) Triton X100; 1% (v/v) deoxycholate; 10 mM iodacetamide) and subjected to Western blot analysis using mouse monoclonal antibodies directed against EGFP (B-2; Santa Cruz Biotechnology), MARV NP, MARV VP40, or β-actin (Abcam). As a secondary antibody, an IRDye800-conjugated antibody was used (Rockland). Protein bands were quantified using an Odyssey imaging system (LI-COR) and standardized to β-actin.
Live-Cell Imaging
Vero E6 cells were infected with rMARV-EGFP at an MOI of 0.05 in a μ-Dish35mm (Ibidi). At 1 hpi, the inoculum was replaced by GIBCO Leibovitz’s L-15 Medium (Invitrogen) containing 20% (v/v) FCS. The cell monolayer was analyzed with a DM16000B Leica inverted fluorescence microscope. EGFP fluorescence and phase contrast images were captured every hour for a period of 9 days. Images were taken with a 20× objective. A Zeiss Axiovert 200 M inverted microscope was used for live-cell imaging of the transfected cells. Fluorescence and phase contrast images were taken with a 40× objective.
RESULTS
Rescue of Recombinant Marburg Virus Expressing EGFP
An additional ATU encoding EGFP was inserted into a full-length antigenomic cDNA plasmid pMARV(+) of MARV strain Musoke [9, 23] between the second and third genes, encoding VP35 and VP40, respectively (Figure 1A).
Figure 1.
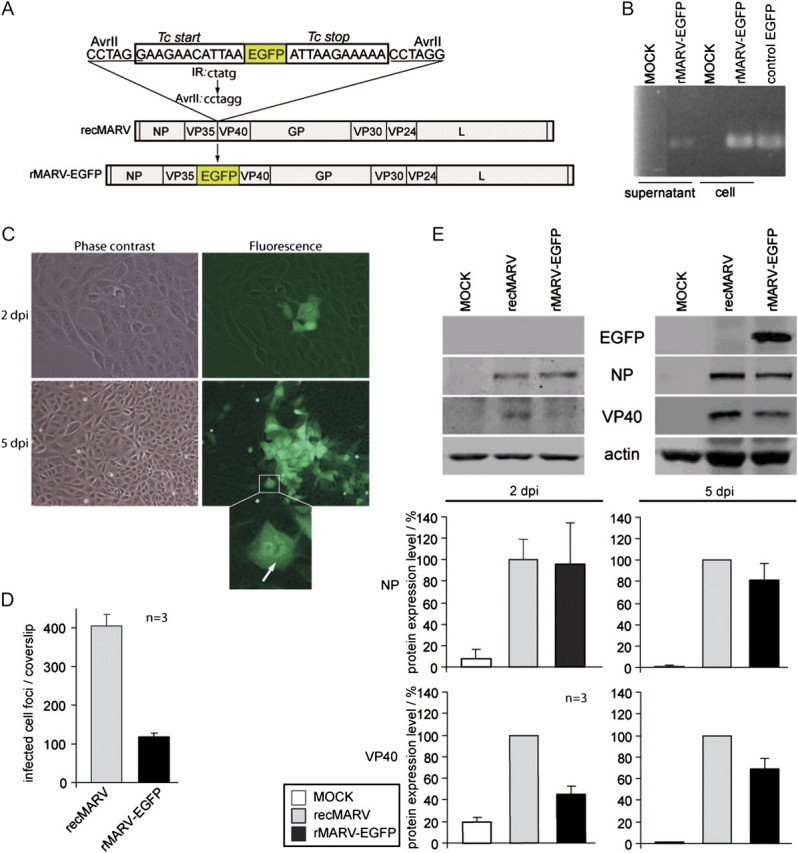
Characterization of recombinant MARV containing an ATU encoding EGFP. A, Scheme of rMARV-EGFP genome. The EGFP coding sequence is flanked by conserved MARV transcription start and stop signals. The EGFP ORF was inserted between the VP35 and VP40 gene via a newly created AvrII restriction site within the intergenic region (IR). The intergenic region spanning 5 nucleotides (CTATG) was altered to CCTAGG. B, Detection of recombinant genomes in supernatants and cell lysates of rMARV-EGFP-infected Vero E6 cells by RT-PCR. RT-PCR was conducted using primers binding in the EGFP ORF. Cellular RNA from Vero E6 cells transiently expressing EGFP was used as a positive control. C, Fluorescence microscopy of rMARV-EGFP-infected cells. Living cells were analyzed by phase contrast and fluorescence microscopy. Images were collected at 2 and 5 dpi. Bottom panel shows rMARV-EGFP-infected cell at higher magnification. Inclusions are indicated by an arrow. D, Comparison of progeny production of recombinant wild-type MARV (recMARV) and rMARV-EGFP. Vero E6 were seeded on glass coverslips and infected with recMARV or rMARV-EGFP. At 2 dpi, cells were subjected to immunofluorescence analysis using a MARV-specific antibody, and foci of infected cells were counted. The experiment was performed in triplicate and the bars represent mean values, including standard deviations. E, Quantitative Western blot analysis of virus protein and EGFP levels in Vero E6 cells infected with recombinant wild-type recMARV or rMARV-EGFP. Assays were performed in triplicate and standard deviations are shown.
Successful rescue of the MARV containing the EGFP gene (rMARV-EGFP) was confirmed by RT-PCR, detection of EGFP expression in infected cells, Western blot analysis, and immunofluorescence analysis. Stable integration of the EGFP gene in the viral genome was verified by amplification of a 362-bp PCR fragment of the EGFP gene using template RNA isolated from rMARV-EGFP-infected cells (Figure 1B) and by sequencing.
Expression of EGFP in living Vero E6 cells infected with rMARV-EGFP was analyzed by phase contrast and fluorescence microscopy. Foci formation of green fluorescent cells was initiated at 1–2 dpi without inducing visible cytopathic effects (CPE). The initial signs of CPE were observed at 5 dpi, when EGFP was detected in clusters of infected cells (Figure 1C). These data show that rMARV-EGFP productively infects susceptible cells and can be used as a sensitive marker to visualize virus spread over time.
To assess the replication efficiency of rMARV-EGFP compared with recombinant wild-type virus (recMARV; described in [9]), supernatant fluids of Vero E6 cells infected with either virus were collected at 6 dpi and used for infection of Vero E6 cells. At 2 dpi, cells were subjected to immunofluorescence analysis using an antiserum directed against MARV nucleocapsid proteins (anti-NC antiserum). Foci of infected cells were counted by fluorescence microscopy (Figure 1D). Progeny virus production of rMARV-EGFP was reduced approximately 4-fold compared with wild-type virus.
To further address this, we compared the protein expression of both viruses. Vero E6 cells were infected as described above, harvested at 2 and 5 dpi, and lysates were analyzed by quantitative Western blot analysis using antibodies directed against EGFP, MARV NP, MARV VP40, and actin. While viral proteins could be readily detected at 2 dpi, EGFP accumulated to detectable levels only at 5 dpi, which might be due to differences in the sensitivity of the used antibodies (Figure 1E). NP levels were similar at all time points, whereas VP40 levels were reduced in rMARV-EGFP-infected cells at 2 dpi and to a lesser extent at 5 dpi. Since the EGFP gene is located downstream of NP and upstream of VP40 gene (Figure 1A), the reduced VP40 expression in rMARV-EGFP indicates that the presence of the ATU causes a decrease in downstream protein expression, thereby explaining the slightly growth-restricted phenotype of rMARV-EGFP.
Cell-to-Cell Spread of MARV-EGFP Observed by Live-Cell Imaging
Next we examined the spread of rMARV-EGFP in cell culture by live-cell imaging. Vero E6 cells were infected with rMARV-EGFP and the cell monolayer was analyzed by collecting EGFP fluorescence and phase contrast photomicrographs. Photomicrographs of 25 different positions were captured every hour from 1 hpi for a period of 9 days (Supplementary Video; online only). Single infected cells expressing EGFP were observed at 26 hpi. In most of the infectious centers, EGFP expression in neighboring cells was detected 20–30 hours later with a mean value of 24.6 hours, which correlates with the MARV Musoke replication cycle of approximately 21 hours [24]. However, in some infectious centers, EGFP expression in surrounding cells was observed as late as 48 hpi. Intriguingly, even late in infection, EGFP fluorescence was not homogenously distributed throughout the monolayer but restricted to individual foci, suggesting that virus spread occurred by direct cell-to-cell contact rather than by release of viral particles. Typically, individual infected cells were observed early in infection, and later on, the infection spread to cells in close proximity to the primarily infected cell (Figure 1C and Supplementary Video). In addition, virus spread was promoted by viral replication in actively dividing cells (Figure 2A and Supplementary Video).
Figure 2.
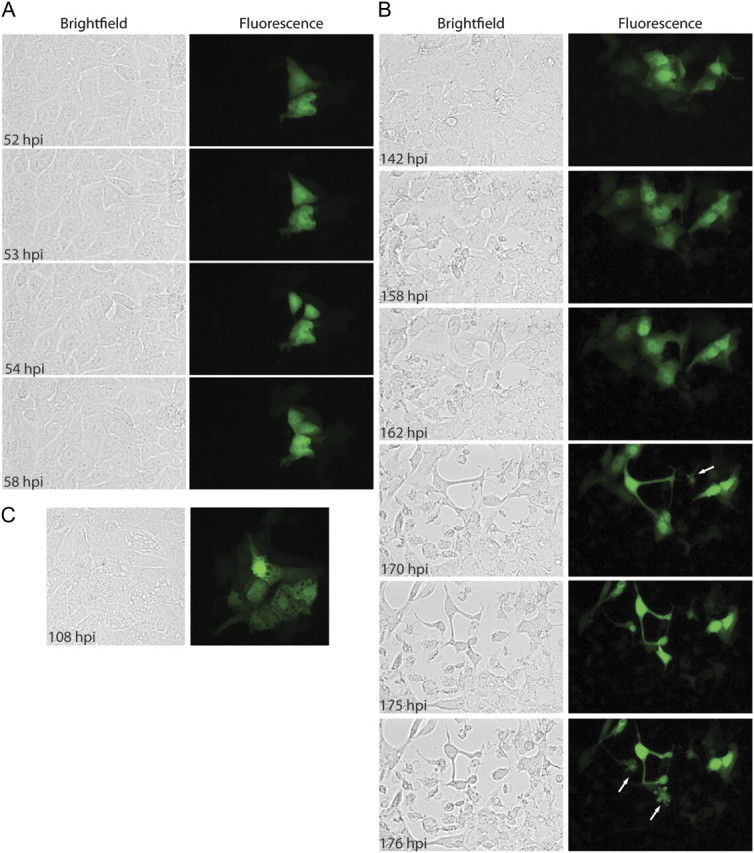
Time-lapse fluorescent microscopy of rMARV-EGFP spread. Vero E6 cells were infected with rMARV-EGFP at an MOI of 0.05, and EGFP fluorescence and phase contrast images were captured every hour for a period of 9 days. A, Cell division of infected cells. B and C, Cytopathic effects at late stages of infection. Blebbing cells are indicated by arrows. Time points postinfection when images were taken are indicated.
After the first signs of CPE appeared at 5 dpi, the cell monolayer began to disintegrate at 6–7 dpi, followed by cell rounding and blebbing of EGFP-expressing cells, which correlates with impending cell death (Figure 2B, arrows). Some, but not all, fluorescent cells formed large intracytoplasmic vacuoles resembling vacuolated degenerating cells as described for nonapoptotic forms of cell death [25] (Figure 2C).
Higher magnification of infected cells revealed that EGFP was homogenously distributed in the nucleus and in the cytoplasm, but unexpectedly was also observed in intracytoplasmic aggregates (Figure 1C, bottom panel). Since MARV infection leads to the formation of inclusions in infected cells, we examined whether the EGFP aggregates were localized with nucleocapsid-derived inclusions. Therefore, at 2 and 5 dpi, rMARV-EGFP-infected cells were examined by indirect immunofluorescence using anti-NC antiserum recognizing the nucleocapsid proteins. EGFP autofluorescence was assessed in parallel. Cytoplasmic EGFP aggregates colocalized with MARV-induced inclusions (Figure 3A). Interestingly, immunofluorescence analysis revealed infected cells that were stained with the virus-specific antiserum but lacked detectable EGFP expression at 5 dpi, indicating that immunodetection using virus-specific antibodies is more sensitive than EGFP detection. To exclude the possibility of “cross-talk” or nonspecific binding of antibodies, rMARV-EGFP-infected cells were stained with a goat anti-MARV antiserum that predominantly recognizes the MARV surface protein GP. Surface staining of infected cells was observed with the GP-specific antibody (Figure 3B, middle panels, red staining). However, green fluorescent inclusions were also visible (Figure 3B, left panels).
Figure 3.
Fluorescence microscopy analysis of EGFP and immunohistochemically labeled viral proteins in rMARV-EGFP-infected cells. Vero E6 cells were infected with rMARV-EGFP and subjected to immunofluorescence analysis at 2 and 5 dpi. Antibodies were directed against (A) intracellular viral proteins or (B) viral surface proteins. Antibody staining is indicated by red color; EGFP autofluorescence, green; and DAPI staining of the nuclei, blue.
EGFP Accumulates in Nucleocapsid Protein-Derived Inclusion Bodies
To further investigate the nature of the EGFP-positive viral inclusions, EGFP was expressed in the absence or presence of MARV nucleocapsid proteins NP and VP35, and cells were monitored by live-cell imaging. We used U2OS cells for the transfection experiments because these cells are large and flat, resulting in high-quality images. U2OS cells were transfected with 500 ng or 50 ng EGFP expression plasmids along with plasmids encoding MARV NP and VP35 genes. When 50 ng of EGFP plasmid was used for transfection, EGFP accumulated in the nucleus but was also observed in the cytoplasm of transfected cells, where it was concentrated in inclusion-like aggregates surrounded by homogenously distributed protein (Figure 4A). We also observed cells in which EGFP was not concentrated in intracytoplasmic inclusions. However, since it was not possible to verify the expression of the nucleocapsid proteins in the live-cell imaging studies, it is not clear whether these cells expressed NP and VP35. When 500 ng of EGFP plasmid was used for transfection, it was difficult to distinguish between concentrated EGFP and nonspecifically distributed EGFP due to the high intensity of overexpressed EGFP. Inclusions were only observed in few cells with lower EGFP expression (Figure 4A). EGFP inclusions were not detected in cells expressing EGFP in the absence of NP and VP35 (Figure 4A, bottom panels).
Figure 4.
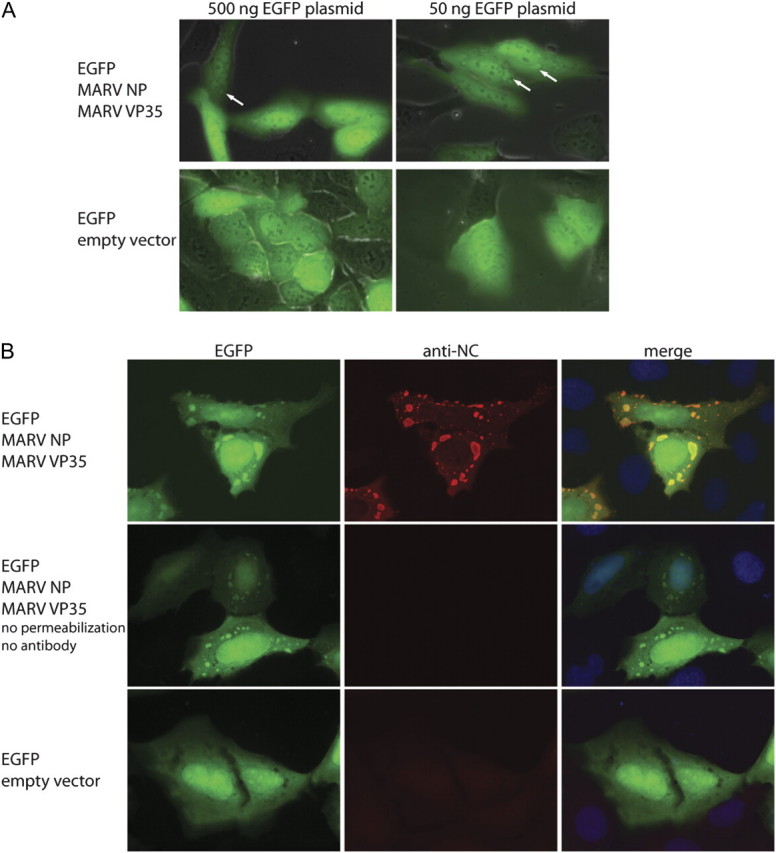
Accumulation of EGFP in MARV inclusions formed by NP and VP35. U2OS cells were transfected with an EGFP expression construct alone or along with plasmids encoding MARV NP and MARV VP35, as indicated. A, Live-cell imaging of transfected cells. EGFP autofluorescence is shown in green. Intracytoplasmic EGFP aggregates are indicated by arrows. B, Cells were stained using an antiserum directed against MARV nucleocapsid proteins (anti-NC; red) and DAPI (blue).
Next, the distribution of EGFP in transfected cells was analyzed by indirect immunofluorescence. Since concentrated EGFP could not be differentiated from the homogenous nonspecific distribution when 500 ng EGFP plasmid was used for transfection, U2OS cells were transfected with 50 ng EGFP plasmid along with plasmids for NP and VP35 stained with anti-NC antiserum. As shown in the upper panels of Figure 4B, EGFP was distributed in a punctate pattern and colocalized with intracytoplasmic nucleocapsid inclusions. Interestingly, the amount of intracytoplasmic homogenously distributed EGFP was reduced compared with the live-cell imaging data, which might be due to fixation and/or permeabilization effects or due to the fact that EGFP is constantly being formed in the live cells, leading to limited bleaching. To exclude the possibility of antibody cross-reactivity, antibody staining was omitted. Fluorescence analysis revealed that EGFP was distributed in large cytoplasmic aggregates (Figure 4B, middle panels). In contrast, EGFP was homogenously distributed when expressed in the absence of NP and VP35 (Figure 4B, bottom panels). The transfection experiments were repeated using HT-1080 cells with a similar outcome (data not shown).
To analyze whether the association with filovirus inclusions is restricted to EGFP or can also be observed with other fluorescent proteins, we expressed MARV NP and VP35 proteins along with various fluorescent proteins from a range of different taxa and exhibiting different physicochemical features. We selected TagRFP and DsRed as genealogically different proteins, which share about 20% amino acid sequence identity with EGFP [26, 27]. In addition, the monomeric mCherry derivative of the tetrameric DsRed was included [28]. Intriguingly, each of the fluorescent proteins colocalized with nucleocapsid-derived inclusions, when coexpressed with NP and VP35 (Figure 5A). Similar to EGFP, fluorescent inclusions were also observed when antibody staining was omitted (Figure 5A, right panels). As a control, the examined fluorescent proteins were expressed in the absence of NP and VP35, and were found to be homogeneously distributed in the cells (data not shown).
Figure 5.
Accumulation of coexpressed fluorescent proteins (FPs) in nucleocapsid protein-induced inclusions. A, Fluorescence microscopy analysis of HT-1080 cells expressing TagRFP (red), DsRed (orange), or mCherry (pink), along with MARV NP and VP35. Cells were either stained with anti-NC antiserum (green) and DAPI (blue) or DAPI alone (right panels). B, Fluorescence microscopy analysis of HT-1080 cells coexpressing EGFP along with ZEBOV (upper panel) or REBOV (lower panel) NP and VP35 proteins. Cells were stained with DAPI (blue) and an antibody detecting the nucleocapsid proteins of both virus species (red).
Next, we addressed the question of the observed relocalization of EGFP in virus-derived inclusions was specific for MARV or could also be observed with other filovirus species. Therefore, EGFP was coexpressed with either REBOV or ZEBOV NP and VP35 proteins. Cells were subjected to immunofluorescence analysis at 1 dpi using an anti-ZEBOV antiserum that cross-reacts with REBOV NP. Figure 5B shows that EGFP colocalized with both ZEBOV and REBOV inclusions, demonstrating that EGFP accumulation in inclusion bodies is not restricted to MARV. These data demonstrate that the accumulation of coexpressed proteins in inclusion bodies is neither restricted to MARV nor EGFP, but occurs irrespective of filoviral species or fluorescent proteins used in the assay.
DISCUSSION
Here we report the generation of a recombinant MARV expressing EGFP from an ATU inserted between the VP35 and VP40 genes. We chose this position for the insertion of the ATU to avoid altering the balance between NP (first gene product) and VP35 (second gene product), since previous results with a MARV minigenome system suggested that the ratio of NP to VP35 is critical for efficient replication and transcription [5]. EGFP has been expressed from the closely related ZEBOV from different positions in the genome, and insertion of the ATU between the NP and VP35 genes did not lead to significant growth defects in cell culture. However, the virus was attenuated in a STAT-1 knockout mouse model [14, 15]. Similar effects were observed with a ZEBOV variant containing the ATU between the VP30 and VP24 genes (fifth and sixth genes). This virus showed no or mild growth defects in cell culture depending on the cell line used for propagation, was moderately attenuated in the mouse model, and was severely attenuated in a nonhuman primate model [15]. A recombinant ZEBOV in which the ATU was added between the VP35 and VP40 genes (second and third genes) could be rescued and propagated in cell culture [16]. Taken together, these data show that ZEBOV tolerates the addition of a foreign gene at different positions, although the insertion of extra nonviral genetic material may lead to reduced virulence in animal models.
Although replication of the recombinant MARV expressing EGFP was reduced 4-fold in cell culture, it was successfully used to monitor viral spread in living cells. Our data suggest that virus spread in the infectious centers occurred predominantly through cell-to-cell-contact. Release of viral particles in MARV-infected cells takes place at filamentous protrusions, the filopodia [29]. Since filopodia act as sensory cellular organelles to explore the extracellular environment, including neighboring cells [30], it has been suggested that MARV particles may bud into adjacent cells via filopodia-mediated cell-to-cell contact [29]. Besides cell-to-cell-contact, virus replication in actively dividing cells seems to be an important mechanism of MARV spread in cell culture. Cell division was not inhibited by MARV infection, indicating that MARV does not interfere with cell cycle progression. The collected data clearly illustrate the strength of live-cell imaging.
Toward the end of the observation period of 9 days, cell rounding, blebbing, then detachment of infected cells was observed. Some of the infected cells formed large intracytoplasmic vacuoles. While blebbing is associated with both apoptotic and necrotic cell death [31], vacuolization of dying cells has been described for nonapoptotic cell death, such as necrosis or autophagy [25], suggesting that MARV-infected cells might not undergo apoptosis late in infection. Although the induction of apoptosis in the context of filovirus infection has been observed in bystander cells, there are conflicted data on the induction of apoptosis in infected cells [32–36].
Surprisingly, we found that EGFP accumulates in filoviral inclusions. A similar observation was reported for some members of the nucleorhabdoviruses, where green fluorescent protein colocalized with viral nucleocapsid protein in loci within and around the nuclei [37]. In contrast, EGFP was found to be homogenously distributed in the nuclei and cytoplasm of cells infected with EGFP-expressing measles virus, which also produces intracytoplasmic inclusions [38, 39]. The intracellular distribution of EGFP was examined by live-cell imaging and immunofluorescence analysis using infected and transfected cells. In both infected and transfected cells, the fluorescence intensity of homogenously distributed EGFP surrounding the intracytoplasmic EGFP aggregates was higher in living cells, making it difficult to distinguish between EGFP aggregates and nonspecific-distributed EGFP. Moreover, when large amounts of EGFP plasmid were used for transfection (500 ng), the punctate pattern of EGFP was not observed in cells coexpressing MARV NP and VP35, suggesting that the EGFP aggregates were masked when overall EGFP expression was high, illustrating the importance of making observations in cells that do not express too much of a protein. In fixed and permeabilized cells, punctate EGFP was clearly visible in both infected cells and transfected cells coexpressing NP and VP35, indicating that the intensity of EGFP autofluorescence was reduced by the treatment of the cells.
Intriguingly, EGFP did not only colocalize with MARV inclusions but also with ZEBOV and REBOV inclusions formed by NP and VP35. In addition, fluorescent proteins other than EGFP also accumulated in MARV inclusions. These data indicate that the accumulation of ectopic proteins in filoviral inclusions is most likely not mediated by direct protein–protein interaction, and future studies are planned to elucidate the underlying mechanisms. For now, the observed colocalization of ectopic fluorescent proteins with filovirus inclusions may be useful to investigate nucleocapsid maturation and transport in infected cells without tagging viral proteins.
In conclusion, this study describes the generation and characterization of an EGFP-containing MARV, which will be a useful tool for imaging-based antiviral drug screening assays. High-throughput screening assays based on the expression of EGFP are currently the preferred approaches for testing potential therapeutic compounds against EBOV infection [19], and the availability of an EGFP-expressing MARV facilitates the development of similar assays for MARV. Furthermore, we demonstrated that rMARV-EGFP can be used to study important steps of the viral replication cycle in living cells, including virus spread and infection-related morphological changes. Since EGFP and other fluorescent proteins colocalize with the viral inclusions, the putative sites of viral replication, rMARV-EGFP could also be used to study the temporal and spatial regulatory steps involved in the formation of these virus-derived intracytoplasmic structures. Future studies are planned to use rodent-adapted recombinant Marburg viruses expressing EGFP or luciferase as valuable tools for the development of whole-animal imaging assays and pathogenesis studies.
Supplementary Data
Supplementary video available at The Journal of Infectious Diseases online.
Funding
This work was supported by the Manchot Foundation (to K. M. S. and J. O.); by funds from the German Research Foundation (SFB 535); by National Institutes of Health (NIH; grants AI082954 and AI057159; New England Regional Center of Excellence–Kasper, subaward 149047-0743); and by start-up funds from Boston University.
Supplementary Material
Acknowledgments
The authors are grateful to O. Dolnik, Philipps University of Marburg, Germany, for rescue of rMARV-EGFP, J. Connor, Boston University, Boston, MA, for his help with carrying out live-cell imaging, and W. P. Duprex, Boston University, for critical review of the manuscript. We also thank N. Kedersha and P. Anderson, Brigham And Women’s Hospital, Harvard Medical School, Boston, MA. for providing the U2OS cells, V. von Messling, University of Quebec, Quebec, Canada, for the mCherry plasmid, and S. Becker, Philipps University of Marburg, for kindly providing anti-MARV antiserum, anti-EBOV antiserum, and anti-MARV VP40 monoclonal antibody.
References
- 1.Mühlberger E. Filovirus replication and transcription. Future Virol. 2007;2:205–15. doi: 10.2217/17460794.2.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolesnikova L, Mühlberger E, Ryabchikova E, Becker S. Ultrastructural organization of recombinant Marburg virus nucleoprotein: comparison with Marburg virus inclusions. J Virol. 2000;74:3899–904. doi: 10.1128/jvi.74.8.3899-3904.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mavrakis M, Kolesnikova L, Schoehn G, Becker S, Ruigrok RW. Morphology of Marburg virus NP-RNA. Virology. 2002;296:300–7. doi: 10.1006/viro.2002.1433. [DOI] [PubMed] [Google Scholar]
- 4.Becker S, Rinne C, Hofsäss U, Klenk H-D, Mühlberger E. Interactions of Marburg virus nucleocapsid proteins. Virology. 1998;249:406–17. doi: 10.1006/viro.1998.9328. [DOI] [PubMed] [Google Scholar]
- 5.Mühlberger E, Lötfering B, Klenk H-D, Becker S. Three of the four nucleocapsid proteins of Marburg virus, NP, VP35, and L, are sufficient to mediate replication and transcription of Marburg virus-specific monocistronic minigenomes. J Virol. 1998;72:8756–64. doi: 10.1128/jvi.72.11.8756-8764.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Möller P, Pariente N, Klenk HD, Becker S. Homo-oligomerization of Marburgvirus VP35 is essential for its function in replication and transcription. J Virol. 2005;79:14876–86. doi: 10.1128/JVI.79.23.14876-14886.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiCarlo A, Moller P, Lander A, Kolesnikova L, Becker S. Nucleocapsid formation and RNA synthesis of Marburg virus is dependent on two coiled coil motifs in the nucleoprotein. Virol J. 2007;4:105. doi: 10.1186/1743-422X-4-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartlieb B, Muziol T, Weissenhorn W, Becker S. Crystal structure of the C-terminal domain of Ebola virus VP30 reveals a role in transcription and nucleocapsid association. Proc Natl Acad Sci USA. 2007;104:624–9. doi: 10.1073/pnas.0606730104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Enterlein S, Volchkov V, Weik M, et al. Rescue of recombinant Marburg virus from cDNA is dependent on nucleocapsid protein VP30. J Virol. 2006;80:1038–43. doi: 10.1128/JVI.80.2.1038-1043.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krähling V, Dolnik O, Kolesnikova L, et al. Establishment of fruit bat cells (Rousettus aegyptiacus) as a model system for the investigation of filoviral infection. PLoS Negl Trop Dis. 2010;4:e802. doi: 10.1371/journal.pntd.0000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volchkov VE, Volchkova VA, Mühlberger E, et al. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science. 2001;291:1965–9. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- 12.Neumann G, Feldmann H, Watanabe S, Lukashevich I, Kawaoka Y. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J Virol. 2002;76:406–10. doi: 10.1128/JVI.76.1.406-410.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Theriault S, Groseth A, Neumann G, Kawaoka Y, Feldmann H. Rescue of Ebola virus from cDNA using heterologous support proteins. Virus Res. 2004;106:43–50. doi: 10.1016/j.virusres.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Towner JS, Paragas J, Dover JE, et al. Generation of eGFP expressing recombinant Zaire ebolavirus for analysis of early pathogenesis events and high-throughput antiviral drug screening. Virology. 2005;332:20–7. doi: 10.1016/j.virol.2004.10.048. [DOI] [PubMed] [Google Scholar]
- 15.Ebihara H, Theriault S, Neumann G, et al. In vitro and in vivo characterization of recombinant Ebola viruses expressing enhanced green fluorescent protein. J Infect Dis. 2007;196(Suppl 2):S313–22. doi: 10.1086/520590. [DOI] [PubMed] [Google Scholar]
- 16.Martinez MJ, Biedenkopf N, Volchkova V, et al. Role of Ebola virus VP30 in transcription reinitiation. J Virol. 2008;82:12569–73. doi: 10.1128/JVI.01395-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prins KC, Delpeut S, Leung DW, et al. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J Virol. 2010;84:3004–15. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michelow IC, Dong M, Mungall BA, et al. A novel L-ficolin/mannose-binding lectin chimeric molecule with enhanced activity against Ebola virus. J Biol Chem. 2010;285:24729–39. doi: 10.1074/jbc.M110.106260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panchal RG, Kota KP, Spurgers KB, et al. Development of high-content imaging assays for lethal viral pathogens. J Biomol Screen. 2010;15:755–65. doi: 10.1177/1087057110374357. [DOI] [PubMed] [Google Scholar]
- 20.Radoshitzky SR, Dong L, Chi X, et al. Infectious Lassa virus, but not filoviruses, is restricted by BST-2/tetherin. J Virol. 2010;84:10569–80. doi: 10.1128/JVI.00103-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. Cellular entry of Ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog. 2010;6e1001110 doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mühlberger E, Trommer S, Funke C, Volchkov V, Klenk H-D, Becker S. Termini of all mRNA species of Marburg virus: sequence and secondary structure. Virology. 1996;223:376–80. doi: 10.1006/viro.1996.0490. [DOI] [PubMed] [Google Scholar]
- 23.Enterlein S, Schmidt KM, Schümann M, et al. The Marburg virus 3′ noncoding region structurally and functionally differs from that of Ebola virus. J Virol. 2009;83:4508–19. doi: 10.1128/JVI.02429-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mühlberger E. Genome organization, replication, and transcription of filoviruses. In: Feldmann H, Klenk H-D, editors. Ebola and Marburg viruses: molecular and cellular biology. Wymondham, UK: Horizon Scientific Press; 2004. pp. 1–12. [Google Scholar]
- 25.Overmeyer JH, Kaul A, Johnson EE, Maltese WA. Active ras triggers death in glioblastoma cells through hyperstimulation of macropinocytosis. Mol Cancer Res. 2008;6:965–77. doi: 10.1158/1541-7786.MCR-07-2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Merzlyak EM, Goedhart J, Shcherbo D, et al. Bright monomeric red fluorescent protein with an extended fluorescence lifetime. Nat Methods. 2004;4:555–7. doi: 10.1038/nmeth1062. [DOI] [PubMed] [Google Scholar]
- 27.Chudakov DM, Matz MV, Lukyanov S, Lukyanov KA. Fluorescent proteins and their applications in imaging living cells and tissues. Physiol Rev. 2010;90:1103–63. doi: 10.1152/physrev.00038.2009. [DOI] [PubMed] [Google Scholar]
- 28.Shaner NC, Campbell RE, Steinbach PA, Giepmans BN, Palmer AE, Tsien RY. Improved monomeric red, orange and yellow fluorescent proteins derived from Discosoma sp. red fluorescent protein. Nat Biotechnol. 2004;22:1567–72. doi: 10.1038/nbt1037. [DOI] [PubMed] [Google Scholar]
- 29.Kolesnikova L, Bohil AB, Cheney RE, Becker S. Budding of Marburgvirus is associated with filopodia. Cell Microbiol. 2007;9:939–51. doi: 10.1111/j.1462-5822.2006.00842.x. [DOI] [PubMed] [Google Scholar]
- 30.Mellor H. The role of formins in filopodia formation. Biochim Biophys Acta. 2010;1803:191–200. doi: 10.1016/j.bbamcr.2008.12.018. [DOI] [PubMed] [Google Scholar]
- 31.Barros LF, Kanaseki T, Sabirov R, et al. Apoptotic and necrotic blebs in epithelial cells display similar neck diameters but different kinase dependency. Cell Death Differ. 2003;10:687–97. doi: 10.1038/sj.cdd.4401236. [DOI] [PubMed] [Google Scholar]
- 32.Baize S, Leroy EM, Georges-Courbot MC, et al. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients [see comments] Nat Med. 1999;5:423–6. doi: 10.1038/7422. [DOI] [PubMed] [Google Scholar]
- 33.Bradfute SB, Braun DR, Shamblin JD, et al. Lymphocyte death in a mouse model of Ebola virus infection. J Infect Dis. 2007;196(Suppl 2):S296–304. doi: 10.1086/520602. [DOI] [PubMed] [Google Scholar]
- 34.Bradfute SB, Swanson PE, Smith MA, et al. Mechanisms and consequences of ebolavirus-induced lymphocyte apoptosis. J Immunol. 2010;184:327–35. doi: 10.4049/jimmunol.0901231. [DOI] [PubMed] [Google Scholar]
- 35.Geisbert TW, Hensley LE, Gibb TR, Steele KE, Jaax NK, Jahrling PB. Apoptosis induced in vitro and in vivo during infection by Ebola and Marburg viruses. Lab Invest. 2000;80:171–86. doi: 10.1038/labinvest.3780021. [DOI] [PubMed] [Google Scholar]
- 36.Gupta M, Spiropoulou C, Rollin PE. Ebola virus infection of human PBMCs causes massive death of macrophages, CD4 and CD8 T cell sub-populations in vitro. Virology. 2007;364:45–54. doi: 10.1016/j.virol.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 37.Goodin M, Yelton S, Ghosh D, Mathews S, Lesnaw J. Live-cell imaging of rhabdovirus-induced morphological changes in plant nuclear membranes. Mol Plant Microbe Interact. 2005;18:703–9. doi: 10.1094/MPMI-18-0703. [DOI] [PubMed] [Google Scholar]
- 38.Duprex WP, McQuaid S, Hangartner L, Billeter MA, Rima BK. Observation of measles virus cell-to-cell spread in astrocytoma cells by using a green fluorescent protein-expressing recombinant virus. J Virol. 1999;73:9568–75. doi: 10.1128/jvi.73.11.9568-9575.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duprex WP, McQuaid S, Roscic-Mrkic B, Cattaneo R, McCallister C, Rima BK. In vitro and in vivo infection of neural cells by a recombinant measles virus expressing enhanced green fluorescent protein. J Virol. 2000;74:7972–9. doi: 10.1128/jvi.74.17.7972-7979.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.