Abstract
Objective
To compare responses to a sexual behavioral survey of spouses in cohabiting heterosexual relationships in Kigali, Rwanda.
Design
Cross-sectional survey.
Methods
Husbands and wives in 779 cohabiting couples were interviewed separately with parallel questionnaires. Participants were recruited from a three-year old cohort of 1458 antenatal clinic attendees enrolled in a prospective study in 1988. Analyses compared responses at the gender- and couple-level for agreement and disagreement.
Results
Couples were in disagreement more than agreement. Women reported occasionally refusing sex, suggesting condom use, and believing married men were unfaithful. Men reported being in a faithful relationship, greater condom use, and being understanding when wives refused sex. Agreement included relationship characteristics, safety of condoms, and whether condoms had ever been used in the relationship. Disagreement included the preferred timing of next pregnancy, desire for more children, and whether a birth control method was currently used and type of method.
Conclusions
Rwandan husbands and wives differed in sexual behavior and reproductive-related topics. Couple-level reporting provides the most reliable measure for relationship aspects as couples’ agreement cannot be assumed among cohabiting partnerships. Furthermore, HIV prevention programs for couples should incorporate communication skills to encourage couple agreement of HIV-related issues.
Keywords: HIV, couples, counseling and testing, agreement and disagreement, sexual behavior, condom use, and pregnancy
Introduction
In Africa, cohabiting couples are the largest risk group for human immunodeficiency virus (HIV) infection1–4 and are experiencing most new HIV infections.5–7 Among married women, the risk of infection is largely related to partner- and couple-level factors.1,8–12 Yet, studies typically focus upon individual risk factors and determinants of condom use rather than assessing both partners’ sexual behavior and other measures of HIV factors.10,13–17 Furthermore, the impact of gender and cultural roles and the male partner’s influence upon a woman’s ability to reduce her risk for HIV infection have not been incorporated in HIV prevention programs.18–20
Investigating partner agreement and communication, or lack thereof, is vital to understanding partner-level determinants of HIV risk and prevention, such as condom use, sexual behaviors, partner’s desire for additional children, and awareness of current contraception use.7,17 Fertility desires influence HIV risk behaviors and understanding fertility intentions within couples is critical to the prevention of vertical and heterosexual transmission.21 The desire to conceive by people living with HIV is similar to that of the general population21–25 with one study finding that 20% of HIV-positive individuals did not agree with their partner regarding wanting to have additional children.24
Among the limited number of couple-level studies, results assessing partner agreement have ranged from fair to substantial agreement26–28 to low agreement and inaccurate perceptions of the partner and his/her risk behaviors.14,28–31 Individual-level reporting does not always provide reliable measures of couples’ behaviors whereas couple-level data allow for the examination of interdependent behaviors28,32 that are either driving the HIV epidemic or protecting couples from it.
Communication between partners has been identified as an important indicator for predicting condom use for the prevention of HIV among heterosexual couples.2,10,18,33–41 Yet, couple communication has received little research and promotion10,18,42–44 as partnership dynamics are commonly conceptualized and analyzed at the individual-level.17 Understanding couple communication and its influence upon couple agreement is crucial to investigating and understanding HIV risk reduction and determinants for infection at the couple-level. We present here a comparison of responses by Rwandan men and women in stable heterosexual partnerships to assess agreement in regards to characteristics of relationships, sexual behavior, condom use, and reproductive issues.
Methods
Study sample
In 1988, a stratified random sampling of 1458 women aged 18–35 years was recruited from among 3702 antenatal and pediatric clinic visitors screened for HIV at the Central Hospitalier in Kigali, Rwanda and enrolled in a prospective observational study.45 Details of the sampling and enrollment procedures and HIV risk factors have been previously described elsewhere.1,46,47 After obtaining written informed consent, a medical history was obtained and physical examination performed. All women were provided voluntary HIV counseling and testing (VCT) and followed every six months. At their request, HIV testing was also offered to their spouses.45 This established cohort of women was used for recruitment of their steady male partners. Men were eligible for enrollment if their female partner was approaching her 36-month visit in the study and she had reported only one steady sexual partner at her 24-month appointment. A systematic effort was made to recruit the primary partner of all the women. In 1991, eligible men who were interested in participation were enrolled into the study resulting in a study population of 779 heterosexual couples who participated in individual-level VCT and completed the behavioral assessment. Thirty three percent of the enrolled men had previously participated in individual-level VCT when women were initially enrolled in 1988. Joint counseling was not standard procedure neither in 1988 nor in enrollment in this study in 1991, though for ethical reasons, systematic efforts were made to ensure that HIV discordant couples were brought in for joint counseling and encouraged to mutually disclose their results. For the behavioral assessment, men and women received individual parallel structured interviews at separate research buildings by gender-matched Rwandan counselors in the national language of Kinyarwanda.
Measures
Along with collecting demographic information (age, income, level of education, etc.), the behavioral questionnaire investigated each partner’s responses regarding sexual behavior within the couple, sexual beliefs, and reproductive-related items. All questions were phrased specifically to reference the relationship between the respondent and their partner enrolled in the study. As dichotomous variables allow for the greatest accuracy when conducting a conditional probability analysis, variables were collapsed into two-levels when possible while maintaining an accurate representation of the data based upon response distributions.*
Research protocols were approved by the Institutional Review Boards of the University of California at San Francisco and the Rwandan Ministry of Health.
Statistical methods
Gender and couple-level reporting were the primary outcomes for this study. Item responses were presented as raw percentages (women, men, positive couple agreement, negative couple agreement, and total couple agreement) with missing data excluded. Couple agreement was assessed for each item using four methods: (1) total percent agreement, (2) kappa statistic, (3) kappa p-value, and (4) conditional probability. Each is discussed briefly below. Total percent agreements were derived from the total number of couples in which men and women shared the same response. The kappa statistic is a widely used measure of reliability that corrects for chance agreement and is appropriate for use when the outcome is dichotomous.48,49 When response options were greater than two and dichotomies were not able to be created, kappa statistics were computed for each category compared with all other responses combined. Landis and Koch’s nomenclature of kappa values was followed: 0.0 to 0.39 indicates low agreement; 0.40 to 0.74 indicates fair, and 0.75 and greater denotes excellent agreement.50 The kappa statistics can convey incomplete and possibly misleading information when the binary variables have very disparate marginal probabilities or asymmetric data, and can be overly conservative when derived from behaviors that occur at either high or low base-rates.51–53 Conditional probability assesses the probability of one partner’s response given the other partner’s response.48,53 The direction of the agreement is determined by the positive and negative probability results. Positive conditional probability (CP+) is the likelihood that both members of the couple will report that an event or behavior occurred.26 Negative conditional probability (CP−) is the likelihood that the couple agrees that an event or behavior did not occur. When both conditional probabilities are high, agreement is high.
Theoretically, a statistically significant p-value (p < 0.05) paired with a fair or excellent kappa statistic (≥0.40) demonstrates agreement. Likewise, an insignificant p-value paired with a low kappa theoretically denotes little to no agreement. The other two paired possibilities (significant p-value/low kappa and insignificant p-value/high kappa) result in undeterminable agreement outcomes requiring additional examination of the conditional probabilities and raw percentages. Therefore, to derive the most accurate and complete perspective of the data, it is important to consider all four statistical assessments as complementary information for each item.
When response options were not able to be dichotomized, “Agree+ %” continues to represent the percent of couples who were in positive agreement while “Agree− %” represents the percent of couples that negatively agreed to all other options (rather than just negatively agreed upon the specific response). This approach should also be noted when interpreting “Total % Couple Agree” for nondichotomized items.
Data were analyzed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) and Excel 2003 (Microsoft Corp., Redmond, WA, USA).
Results
Sample demographic characteristics
The mean age of women was 32 years (SD, 4.4) and mean age of sexual debut was 19 years (SD, 2.9) (Table 1). The majority of women had at least five years of schooling (63%), two lifetime sexual partners (SD, 6.0), no individual income during the past year (78%), and were Catholic (67%). The mean age of men was 39 years (SD, 7.6) and mean age of sexual debut was 20 years (SD, 4.0). Men also typically had at least five years of schooling (70%), a mean of 11 lifetime sexual partners (SD, 24.0), and were Catholic (66%). Only 1% of men had no individual income during the past year. Regardless of religious preference, 62% of women and 66% of men participated in religious services at least once a week. The mean duration of relationships was 11 years with an average of four children.
Table 1.
Selected individual-level demographic characteristics of sample (N = 779 couples)
| Women % or Mean | Women n or (SD) | Men % or Mean | Men n or (SD) | |
|---|---|---|---|---|
| Age | 32 | (4.4) | 39 | (7.6) |
| Age at sexual debut | 19 | (2.9) | 20 | (4.0) |
| Years of school | ||||
| No schooling | 20% | 150 | 12% | 94 |
| 1–4 years | 16% | 123 | 18% | 137 |
| 5–7 years | 44% | 332 | 42% | 325 |
| 8–14 years | 18% | 139 | 25% | 196 |
| More than 14 years | 1% | 10 | 3% | 23 |
| Number of lifetime partners | 2 | (6.0) | 11 | (24.0) |
| Number of prior cohabiting relationships | 0.2 | (0.4) | 0.3 | (0.5) |
| Had no income in past year | 78% | 605 | 1% | 7 |
| Years in Kigali | 17 | (10) | 22 | (12.5) |
| Number of people known who have died from AIDS | 5 | (9.9) | 8 | (5.0) |
| Religion preference | ||||
| Catholic | 67% | 519 | 66% | 514 |
| Other Christian | 22% | 167 | 20% | 155 |
| Muslim | 11% | 82 | 12% | 93 |
| None | 1% | 5 | 1% | 11 |
| Religious service participation at least once a week | 62% | 483 | 66% | 515 |
| Years in union | 11 | (4.8) | 11 | (4.9) |
| Number of children with partner | 4 | (2.1) | 4 | (2.1) |
Notes: Percentages may not total 100 due to rounding.
As this paper addresses the methodological approach of couples-level analysis as an addition to gender-level reporting to provide a more comprehensive investigation of relationship dynamics, the following subsection results (demographics, sexual behavior and beliefs, and reproductive desires and pregnancy-related issues) will highlight key areas of couples’ agreement or disagreement as well as identify critical areas at the gender-level that are relevant to HIV prevention. Therefore, each result section identifies key topics of couple agreement (if any were present) followed by important findings at the gender-level.
Demographics and sexual behavior within the couple
As expected, couple agreement was high regarding type of marriage (civil vs common law: 92% couple agreement) and type of relationship (monogamous vs polygamous: 96% couple agreement) (Table 2). High agreement was also found in regards to not being in an abstinent relationship (100%; not shown). Women were more likely than men to report having ever used a condom in their relationship (45% vs 36%) resulting in 31% of couples in positive agreement and 50% of couples agreeing upon nonuse. While this represents high agreement according to our criteria, it also indicates that 14% of women and 5% of men reported having used condoms with their spouse while the spouse denied condom use. Among couples who reported never having used condoms, couples were in agreement that the husband had never suggested use (90%) but differed in opinion as to whether the wife had ever suggested use. Forty-six percent of women reported that they had suggested condom use in the relationship although only 17% of men reported similarly with only 10% of couples in positive agreement. When asked if condoms had been used in the last month, 27% of women and 29% of men agreed positively. Surprisingly, both partners reported condom use in 19% of couples and in a roughly equal number (8% of women and 10% of men) only one partner reported condom use and the other denied it.
Table 2.
Gender-level reporting and couple agreement of partnership demographics, sexual behavior within the couple, and sexual beliefs (N = 779 couples)
| Women % | Men % | Couple agree+ % | Couple agree− % | Total % couple agree (CP+, CP−) | Kappa | n | |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Civil marriage (vs common law) | 57 | 58 | 53 | 39 | 92 (93, 91) | 0.84*** | 778 |
| Monogamous (vs polygamous) | 92 | 94 | 91 | 5 | 96 (96, 87) | 0.69*** | 778 |
| Sexual behavior within the couple | |||||||
| Condoms ever used with partner | 45 | 36 | 31 | 50 | 81 (76, 84) | 0.61*** | 779 |
| Condoms used in the last month with partner | 27 | 29 | 19 | 63 | 82 (68, 88) | 0.55*** | 774 |
| Of couples who never used condoms, husband ever suggested usea | 3 | 7 | 0 | 90 | 90 (0.0, 95) | −0.05 | 386 |
| Of couples who never used condoms, wife ever suggested usea | 46 | 17 | 10 | 47 | 57 (31,68) | 0.07 | 386 |
| Husband is sole initiator of sex | 81 | 86 | 72 | 5 | 77 (86, 28) | 0.15*** | 773 |
| Wife refuses sex at times | 57 | 37 | 25 | 30 | 55 (52, 57) | 0.12** | 774 |
| When wife refuses sex, husband understands | 26 | 68 | 19 | 25 | 44 (41, 48) | 0.06 | 190 |
| When wife refuses, husband insists on sex | 35 | 34 | 14 | 45 | 59 (41, 69) | 0.09 | 190 |
| Sexual beliefs | |||||||
| Faithful relationship | 69 | 96 | 67 | 3 | 70 (82, 15) | 0.09*** | 769 |
| Husband has fewer sexual partners due to the presence of HIV in the communitya | |||||||
| Yes | 13 | 68 | 10 | 29 | 39 (25, 49) | 0.05* | 629 |
| No | 7 | 20 | 1 | 74 | 75 (5, 86) | −0.06 | |
| Not applicable | 80 | 12 | 10 | 18 | 28 (23, 33) | 0.02 | |
| Husband uses condoms with other partnersa | |||||||
| Yes | 5 | 4 | 0 | 94 | 94 (6, 97) | 0.04 | 519 |
| No | 9 | 4 | 1 | 88 | 89 (9, 94) | 0.04 | |
| Not applicable | 86 | 93 | 82 | 1 | 83 (90, 10) | 0.03 | |
| Most married men are not faithful | 51 | 20 | 11 | 39 | 50 (30, 61) | 0.02 | 764 |
| Most married women are not faithful | 12 | 17 | 3 | 74 | 77 (19, 87) | 0.07 | 759 |
| Male condoms are dangerous for women | 1 | 18 | 0 | 81 | 81 (4, 89) | 0.03 | 697 |
| Male condoms are dangerous for men | 1 | 11 | 0 | 88 | 88 (4, 93) | 0.03 | 726 |
| The exchange of fluids during sex is important for the health of the man | 89 | 82 | 74 | 3 | 77 (86, 21) | 0.08 | 448 |
| The exchange of fluids during sex is important for the health of the woman | 58 | 84 | 50 | 8 | 58 (70, 28) | 0.06 | 670 |
| The exchange of fluids during sex is important for the health of the fetus | 57 | 70 | 42 | 14 | 56 (65, 38) | 0.06 | 654 |
P-value key:
< 0.05;
< 0.01;
< 0.0001.
CP+ = positive conditional probability index; CP− = negative conditional probability index.
Kappa key: low = 0.0 to 0.39; fair = 0.40 to 0.74; excellent = 0.75 and greater.
Includes partner perceptions: results are of the partner’s perception of the spouse’s behavior versus the spouse’s self-report.
Women reported refusing sex more often than men reported refusal from their wives (57% vs 37%) resulting in more than half of the couples (65%) in disagreement. This suggests that some indications of refusal may have been subtle and not perceived as such by the husband or that men would not acknowledge this in an interview.
When women’s refusal of sex was reported by both partners, two additional questions were asked, both resulting in low agreement: Was the husband understanding when his wife refused sex? And did he insist upon sex despite the refusal? Husbands were more likely to report being understanding when the wife refused sex (68% vs 26% of wives) with only 19% of couples agreeing that the husband understood while 25% of couples agreed that the husband was not understanding. Although 34%–35% of men and women reported that the husband insisted on sex after the refusal, only 14% of couples were in agreement on this point, again suggesting that either couples do not communicate well about having sex or that there is reluctance to disclose such sensitive information.
Sexual beliefs related to partnership and HIV prevention
Men and women’s perceptions of sexual behavior in and outside of the relationship differed greatly. Whereas 96% of men reported being in a faithful relationship, only 69% of women reported similarly resulting also in poor agreement between spouses (Table 2). When asked if the husband’s sexual behavior had changed due to the presence of HIV in the community, couples were largely in disagreement. Men were more likely to respond positively (68%) whereas women were more likely to report ‘not applicable’ (80%) perhaps suggesting that women were unsure of their husband’s behavior.
The majority of couples (74%) disagreed with the statement ‘most married women are not faithful’ although men and women were not in agreement regarding the faithfulness of married men. Women were more likely than men to report that most married men were not faithful, with 11% of couples in agreement that married men were not faithful and 39% agreeing that they were faithful.
Among respondents who believed that male condoms were dangerous to one’s health, men were much more likely than women to think that condoms were dangerous for men (11% vs 1%) and women (18% vs 1%). Overall, the majority of couples were in agreement that male condoms were not dangerous for women (81%) or men (88%). Intra-couple agreement was low regarding the perceived health benefits of the exchange of fluids during sex for the man, woman, and fetus. Three-quarters of couples (74%) believed that exchange of fluids during sex was important for the health of the man (men: 82%; women: 89%). Women were less likely than men to hold this belief for the health of the woman (58% vs 84%) and fetus (57% vs 70%).
Reproductive desires and pregnancy-related issues
In general, questions pertaining to pregnancy resulted in low agreement (Table 3). Less than half of the couples (46%) were in agreement regarding the preferred timing of the last pregnancy of which 7% had not desired the pregnancy at that time (women: 25%; men: 15%) and only 39% of couples felt that the timing was appropriate (men: 74%; women: 48%).
Table 3.
Gender-level reporting, couple agreement, and partner perceptions regarding pregnancy-related issues and reproductive desires (N = 779 couples)
| Women % | Men % | Couple agree+ % | Couple agree− % | Total % couple agree (CP+, CP−) | Kappa | n | |
|---|---|---|---|---|---|---|---|
| The preferred timing for the last pregnancy would have been ... | 776 | ||||||
| At that time | 48 | 74 | 39 | 17 | 56 (63, 43) | 0.13 *** | |
| Later | 10 | 9 | 0 | 83 | 83 (9, 91) | 0.01 | |
| Earlier | 18 | <1 | 0 | 81 | 81 (0, 90) | −0.01 | |
| Not at all | 25 | 15 | 7 | 67 | 74 (33, 83) | 0.18 *** | |
| Contraceptive used at last pregnancy | 6 | 35 | 3 | 61 | 64 (14, 77) | 0.03 | 770 |
| Husband happy about last pregnancya | 78 | 89 | 73 | 6 | 79 (87, 34) | 0.23 *** | 648 |
| Wife happy about last pregnancya | 87 | 88 | 80 | 5 | 85 (91, 38) | 0.29 *** | 606 |
| Desire for more children | 768 | ||||||
| 0 children | 65 | 62 | 49 | 22 | 71 (78, 61) | 0.30 *** | |
| 1 child | 17 | 21 | 6 | ||||
| 2 children | 16 | 14 | 6 | ||||
| More than 2 children | 2 | 3 | 0 | ||||
| Wife’s desire for more childrena | 703 | ||||||
| 0 children | 67 | 62 | 52 | 23 | 75 (80, 64) | 0.44 *** | |
| 1 child | 17 | 23 | 8 | ||||
| 2 children | 14 | 12 | 5 | ||||
| More than 2 children | 2 | 3 | 0 | ||||
| Husband’s desire for more childrena | 657 | ||||||
| 0 children | 63 | 64 | 52 | 25 | 77 (82, 68) | 0.49 *** | |
| 1 child | 21 | 17 | 7 | ||||
| 2 children | 14 | 15 | 7 | ||||
| More than 2 children | 3 | 3 | 1 | ||||
| Preferred timing for next pregnancy | 739 | ||||||
| Already pregnant | 11 | 9 | 6 | 86 | 92 (61, 96) | 0.56 *** | |
| As soon as possible | 6 | 5 | 2 | 91 | 93 (30, 96) | 0.26 *** | |
| Next year | 2 | 6 | 1 | 93 | 94 (14, 97) | 0.11 ** | |
| In two years | 3 | 4 | 1 | 94 | 95 (20, 97) | 0.18 *** | |
| In more than two years | 19 | 18 | 9 | 72 | 81 (47, 88) | 0.35 *** | |
| No more pregnancies | 60 | 58 | 46 | 27 | 73 (77, 67) | 0.44 *** | |
| Using method to delay pregnancy | 65 | 85 | 60 | 10 | 70 (80, 39) | 0 23 *** | 663 |
| If method is used, what method | 395 | ||||||
| Practicing abstinence | 15 | 30 | 10 | 64 | 74 (43, 83) | 0.28 *** | |
| Using pills | 17 | 12 | 10 | 81 | 91 (66, 94) | 0.61 *** | |
| Using condoms | 33 | 34 | 26 | 58 | 84 (76, 88) | 0.64 *** | |
| Using injections | 16 | 11 | 8 | 80 | 88 (57, 93) | 0.50 *** | |
P-value key:
< 0.05;
< 0.01;
< 0.0001.
CP+ = positive conditional probability index; CP− = negative conditional probability index.
Kappa key: low = 0.0 to 0.39; fair = 0.40 to 0.74; excellent = 0.75 and greater.
Includes partner perceptions: results are of the partner's perception of the spouse’s behavior versus the spouse's self-report.
Contraceptive use at last pregnancy also showed couples’ discrepancy. Men (35%) were more likely than women (6%) to report the use of contraception resulting in only 3% of couples in positive agreement. It may be that withdrawal or the rhythm method, which are commonly used in Africa to prevent pregnancy, are viewed as “contraceptives” by men more than by women. Alternatively, men may believe that women are taking precautions of some kind when in fact they are not. Although knowledge of contraception use at last pregnancy was strikingly low, couples were in fairly good agreement regarding whether their partner and they were happy about the last pregnancy. Seventy-three percent of couples believed that the husband was happy with the last pregnancy and 80% of couples believed that the wife was happy.
Couples were also asked about their desire for future children and the preferred timing of their next pregnancy. Nearly half of couples (49%) were in agreement that they did not desire future children, with 29% of couples having one partner desiring more children and the other not. Two questions investigated partner perceptions for the desire for more children. Overall, positive agreement was found regarding the perceived number of additional children that the wife and husband desired. Seventy-five percent of couples agreed upon the wife’s desire to have no more children (agree: yes, 52%; agree: no, 23%) and 77% of couples agreed upon the husband’s desire for no more children (agree: yes, 52%; agree: no, 25%).
Of the 663 couples who agreed that they were either currently delaying or avoiding pregnancy, 70% of couples were in agreement as to whether they were doing so by use of a method (yes: 60%; no: 10%). Among couples trying to delay or avoid pregnancy and using a method, only half of the couples (54%) were in agreement as to the method being used. Men were more likely to report the use of condoms (34%) or abstinence (30%) whereas women reported the use of condoms (33%), birth control pills (17%), hormonal injections (16%), and abstinence (15%).
Discussion
This study confirms that married Rwandan men and women differ in their reporting of sexual behaviors, condom use, reproductive desires, and pregnancy-related issues. Furthermore, it confirms that the methodological approach of couples-level data collection and analysis (versus individual-level only) is vital to understanding relationship dynamics necessary for the prevention of HIV within couples. Though agreement within couples was high regarding key characteristics of the partnership (type of marriage and relationship), agreement was generally low regarding condom use in the couple, sexual behavior outside the couple, and fertility-related issues. These are all critical to understanding HIV prevention for the largest HIV risk group in Africa. Without confident understanding of couple-level agreement on such relationship and sexual behavior issues, risk reduction programs that target either the individual or the couple may be misguided and unsuccessful in changing the behavior necessary for the prevention of HIV transmission. To untangle the partnership dynamics of individual- and couple-related factors impacting the sexual dyad’s risk for HIV, investigating couples’ agreement regarding HIV-related risk and prevention factors is crucial7,18,32 and primary to risk reduction and condom use.
Due to the methodological approach taken in this paper, we would like to address the limitations of our study first to provide a clear context in which this study was undertaken. First, we recognize that our findings represent sexual behaviors and perceptions during the early years of the HIV epidemic. Secondly, recall and reporting biases, such as social desirability, may have impacted individual’s responses that in analysis have been identified as lack of agreement. Thirdly, the questionnaire was not designed to evaluate couples’ agreement resulting in some questions not being able to be dichotomized for the assessment of kappa and conditional probability. Fourthly, this was a convenience sample based upon the recruitment of husbands of women enrolled in a longitudinal HIV research project. Couples in which the husband chose not to participate in the study may have differed from participating couples, thus affecting external validity. Finally, we recognize that the women’s participation in an HIV observational study for 36-months and prior VCT, along with one third of the men who had previously undergone VCT, may have resulted in responses different from the general population of Kigali.
Unlike previous studies,31,53–55 this study did not find that individual-level responses were reliable measures for sexual behavior, partner perceptions, and the desire for children that impact decision-making within the partnership. Lack of couples’ agreement on such issues of condom use, refusal of sex, faithfulness, and the desire for children each have direct impact upon HIV prevention. Although we recognize that recall bias and/or social desirability may be contributing to the lack of agreement of past condom behavior, this would not be a likely explanation for the discrepancies in both ‘ever use’ and ‘ever use in the last month’ as these are straightforward questions about a behavior that is unlikely to be misclassified when response options are yes/no in an environment where condom use is negligible. We suggest that these differences more likely represent gender differences in the reporting of sexual behavior56 and therefore is of primary concern. Furthermore, it remains the forefront of HIV prevention for this at-risk population and calls for greater investigation and development of biological and survey tools to more accurately assess condom use.33,40
As pregnancy cannot occur without unprotected sex, low couple agreement regarding the desire of children directly impacts one’s ability to remain HIV-negative through the use of consistent and correct condom use. Among couples in disagreement regarding the desire for children or the desired timing of pregnancy, consistent condom use may be jeopardized.
The lack of agreement surrounding the issues of refusal of sex by the wife was also striking as husbands and wives’ perceptions of their partner’s intentions were unclear, eliciting concerns of gender and power dynamics and communication within in the relationship. With a majority of women reporting that their husbands were not understanding when refusal occurred and more than a quarter of women reporting that relations were still insisted upon, many women lacked control of their sexual environment as well as their ability to avoid HIV transmission.
We also found that men’s fidelity was questioned by women although their husbands’ responses did not support these perceptions. Unfortunately the survey did not explore women’s reasons for such beliefs of infidelity. It is possible that these discrepancies exist due to lack of communication between partners, differing opinions, social desirability to not admit to outside relations, or even a potential protective strategy for women to assume infidelity if unsure of their partner’s behavior. Regardless, concerns of infidelity coupled with low condom use within married partnerships significantly jeopardize the HIV negative partner’s efforts to remain healthy.
The benefits of couples-level analysis are numerous. Along with providing insight about agreement and disagreement, couples-level analysis provides for the examination of individual- level responses and allows for the comparison of results at both levels. As presented in the tables, looking exclusively at gender-level responses created a dissimilar view than that presented at the couple-level. Our findings aid in the development of HIV behavioral research in four important ways: (1) provides a rare opportunity to examine couple-level behavioral issues at the onset of the HIV epidemic in Rwanda providing the baseline data for a 20-year comparison study in a largely understudied population and methodology; (2) highlights the need for further research on partner communication and its impact upon couples’ agreement relevant to the development of HIV prevention methods to address the decision-making needs of couples; (3) identifies the critical topic areas of condom use and faithfulness to be targeted for improved couples’ communication for risk reduction; and (4) confirms that the collection of couples’ data for analysis is vital to understanding and preventing the spread of HIV within couples.
To obtain the greatest reliability of data, couple-level data as a complementary source to individual-level reporting should be adopted as the gold standard, particularly among populations and cultures in which gender and power dynamics are known to impact communication and decision- making. Without the pilot-testing of couple- versus individual-level reporting within populations and sub-groups, individual-level data should not be assumed to adequately reflect the social and behavioral complexities of partnerships and partner’s perceptions. Understanding couple agreement is the first step to understanding a couple’s communication patterns that ultimately determine condom use, fidelity, and reproductive decision-making. Subsequently, the adoption of couple-level research by the scientific community will aid in the development of couple-level interventions that specifically target communication and decision-making crucial to protecting couples from HIV transmission.
Currently, individual-level research and interventions continue to be the norm in HIV research. Few HIV interventions have been delivered at the couple-level even though couples’ interventions have been found to be more effective than interventions targeted at individuals.2,14,15,41 HIV/sexually transmitted infection (STI) behavior change models have been criticized for being individualistic in their conceptualization and fail to account for broader cultural factors and the gendered nature of sexual behaviors and risk reduction.18,32,57 Likewise, prevention models and interventions have largely been directed towards women even though condom use is male controlled.15,18,36,58
Conclusions
As the sexually active couple is the most appropriate unit of study for HIV prevention in Africa,14 the focus upon couples’ sexual behavior and agreement is a much-needed and appropriate return to the socio-cultural context of heterosexual infections in sub-Saharan Africa.10 The lack of couple-level social and behavioral research related to HIV infection is a call for greater examination of the values, beliefs, and practices related to gender and sexual roles of the partnership as well as their impact upon HIV risk behaviors and behavior change strategies.13,26 With the evolution of and increased demand for couple-level research as a complementary tool to individual-level reporting, couple-level interventions will benefit from an improved understanding of how individual members of a relationship behave as a dyad. Couple-level research and interventions must target couples’ agreement and communication for decision-making in order to facilitate effective, culturally appropriate, and sustainable risk reduction plans in this at-risk, but largely overlooked, population for HIV infection.
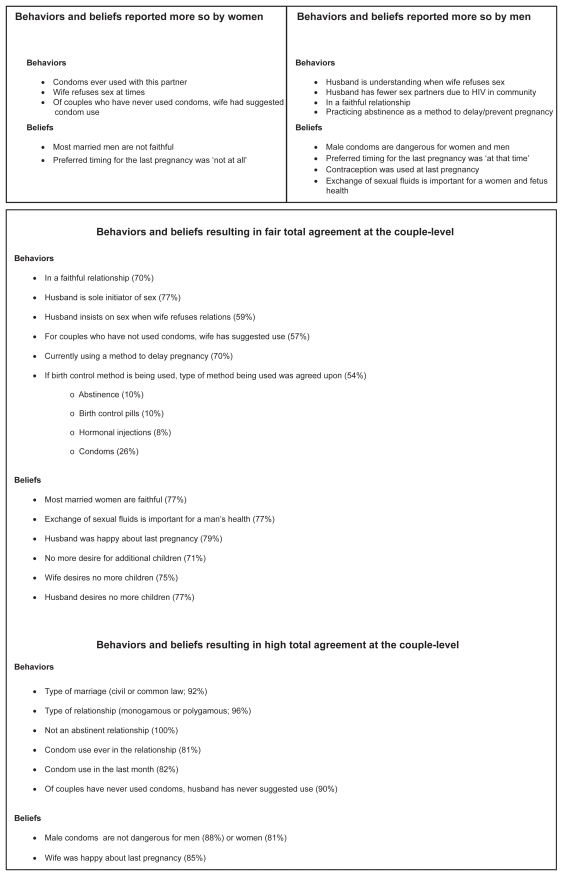
Figure 1.
Responses predominately reported by either women or men and sexual behaviors and beliefs resulting in fair and high agreement at the couple-level.
Acknowledgments
This study received financial support from the National Institutes of Allergy and Infection Disease (AI 23980 and 40951), the National Institutes of Mental Health (MH 42459, 082634, and 66767), the Fogarty AIDS International Training and Research Program (FIC TW001042), the International AIDS Vaccine Initiative (IAVI), the National Institutes of Child Health and Human Development (HD 40125), and the Social and Behavioral Core of the Emory Center for AIDS Research (AI050409).
Footnotes
Individuals were asked their frequency of religious service participation. Response options included at least once a week, once or twice a month, a few times a year, rarely, and never. Responses were collapsed into whether they participated in religious services at least once a week. When asked what one’s income was in the past year, respondents reported a number that was collapsed into whether or not they had an income. Regarding sexual refusal by the wife and if the husband insisted upon sexual relations after the refusal, response options included never, sometimes, and often which were collapsed into “never” and “at times (sometimes/often)”. When asked if the husband was understanding when the wife refused sex, response options included “he understands”, “it depends”, “he gets mad”, “he does not understand but he accepts”, and “he goes to other partners”. Responses were collapsed into “he understands” and “he does not understand”. Lastly, when asked about the number of future children desired, respondents reported a number that was then collapsed into four categories: zero, one, two, and more than two children. Eight questions allowed for the comparison of an individual’s response to their partner’s perceptions of their response. For example, individuals were asked whether they had ever suggested condom use and whether their partner had ever suggested it. Each wife’s reporting of suggesting condom use was compared with her husband’s perception of whether she had suggested use and vice versa.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Allen S, Lindan C, Serufilira A, Van de Perre P, Rundle A, Nsengumuremyi F. Human immunodeficiency virus infection in urban Rwanda: Demographic and behavioral correlates in a representative sample of childbearing women. JAMA. 1991;266(12):1657–1663. [PubMed] [Google Scholar]
- 2.Allen S, Tice J, Van de Perre P, et al. Effect of serotesting with counselling on condom use and seroconversion among HIV discordant couples in Africa. British Medical Journal. 1992;304(6842):1605–1609. doi: 10.1136/bmj.304.6842.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hugonnet S, Mosha F, Todd J, et al. Incidence of HIV infection in stable sexual partnerships: a retrospective cohort study of 1802 couples in Mwanza Region, Tanzania. J Acquir Immune Defic Syndr. 2002;30(1):73–80. doi: 10.1097/00042560-200205010-00010. [DOI] [PubMed] [Google Scholar]
- 4.Dunkle KL, Stephenson R, Karita E, et al. New heterosexually transmitted HIV infections in married or cohabiting couples in urban Zambia and Rwanda: an analysis of survey and clinical data. Lancet. 2008;371(9631):2183–2191. doi: 10.1016/S0140-6736(08)60953-8. [DOI] [PubMed] [Google Scholar]
- 5.Allen S, Karita E, N’gandu N, Tichacek A. The evolution of voluntary testing and counseling as an HIV prevention strategy. In: al Ge, editor. HIV in Developing Countries: Biomedical and behavioral approaches. New York: Plenum Press; 1999. [Google Scholar]
- 6.McKenna SL, Muyinda GK, Roth D, et al. Rapid HIV testing and counseling for voluntary testing centers in Africa. AIDS. 1997;11(Suppl 1):S103–S110. [PubMed] [Google Scholar]
- 7.Guthrie BL, de Bruyn G, Farquhar C. HIV-1-discordant couples in sub-Saharan Africa: explanations and implications for high rates of discordancy. Curr HIV Res. 2007;5(4):416–429. doi: 10.2174/157016207781023992. [DOI] [PubMed] [Google Scholar]
- 8.Bassett MT, McFarland WC, Ray S, et al. Risk factors for HIV infection at enrollment in an urban male factory cohort in Harare, Zimbabwe. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;13(3):287–293. doi: 10.1097/00042560-199611010-00012. [DOI] [PubMed] [Google Scholar]
- 9.Glynn JR, Carael M, Auvert B, et al. Why do young women have a much higher prevalence of HIV than young men? A study in Kisumu, Kenya and Ndola, Zambia. AIDS. 2001;15(Suppl 4):S51–S60. doi: 10.1097/00002030-200108004-00006. [DOI] [PubMed] [Google Scholar]
- 10.Painter TM. Voluntary counseling and testing for couples: a high-leverage intervention for HIV/AIDS prevention in sub-Saharan Africa. Soc Sci Med. 2001;53(11):1397–1411. doi: 10.1016/s0277-9536(00)00427-5. [DOI] [PubMed] [Google Scholar]
- 11.Kohler HP, Behrman JR, Watkins SC. Social networks and HIV/AIDs risk perceptions. Demography. 2007;44(1):1–33. doi: 10.1353/dem.2007.0006. [DOI] [PubMed] [Google Scholar]
- 12.Stephenson R, Barker J, Cramer R, et al. The demographic profile of sero-discordant couples enrolled in clinical research in Rwanda and Zambia. AIDS Care. 2008;20(3):395–405. doi: 10.1080/09540120701593497. [DOI] [PubMed] [Google Scholar]
- 13.Amaro H, Raj A. On the margin: Power and women’s HIV risk reduction strategies. Sex Roles. 2000;42(7–8):723–749. [Google Scholar]
- 14.Becker S. Couples and reproductive health: a review of couple studies. Stud Fam Plann. 1996;27(6):291–306. [PubMed] [Google Scholar]
- 15.Harvey SM, Beckman LJ, Doty M. Couple dynamics in sexual and reproductive decision-making among Mexican immigrants. In: Miller LJSW, editor. Advances in Population: Psychosocial perspectives. London: J Kingsley; 1999. pp. 251–279. [Google Scholar]
- 16.Colebunders R, Ndumbe P. Priorities for HIV testing in developing countries? Lancet. 1993;342(8871):601–602. doi: 10.1016/0140-6736(93)91417-k. [DOI] [PubMed] [Google Scholar]
- 17.Gorbach PM, Holmes KK. Transmission of STIs/HIV at the partnership level: beyond individual-level analyses. J Urban Health. 2003;80(4 Suppl 3):iii15–25. doi: 10.1093/jurban/jtg079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amaro H. Love, sex, and power: Considering women’s realities in HIV prevention. Am Psychol. 1995;50(6):437–447. doi: 10.1037//0003-066x.50.6.437. [DOI] [PubMed] [Google Scholar]
- 19.Strebel A, Crawford M, Shefer T, et al. Social constructions of gender roles, gender-based violence and HIV/AIDS in two communities of the Western Cape, South Africa. SAHARA J. 2006;3(3):516–528. doi: 10.1080/17290376.2006.9724879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaufman MR, Shefer T, Crawford M, Simbayi LC, Kalichman SC. Gender attitudes, sexual power, HIV risk: a model for understanding HIV risk behavior of South African men. AIDS Care. 2008;20(4):434–441. doi: 10.1080/09540120701867057. [DOI] [PubMed] [Google Scholar]
- 21.Thornton AC, Romanelli F, Collins JD. Reproduction decision making for couples affected by HIV: a review of the literature. Top HIV Med. 2004;12(2):61–67. [PubMed] [Google Scholar]
- 22.Chen JL, Philips KA, Kanouse DE, Collins RL, Miu A. Fertility desires and intentions of HIV-positive men and women. Fam Plann Perspect. 2001;33(4):144–152. [PubMed] [Google Scholar]
- 23.Nakayiwa S, Abang B, Packel L, et al. Desire for children and pregnancy risk behavior among HIV-infected men and women in Uganda. AIDS Behav. 2006;10(4 Suppl):S95–S104. doi: 10.1007/s10461-006-9126-2. [DOI] [PubMed] [Google Scholar]
- 24.Panozzo L, Battegay M, Friedl A, Vernazza PL, Swiss Cohort S. High risk behaviour and fertility desires among heterosexual HIV-positive patients with a serodiscordant partner – two challenging issues. Swiss Med Wkly 22. 2003;133(7–8):124–127. doi: 10.4414/smw.2003.10124. [DOI] [PubMed] [Google Scholar]
- 25.Wesley Y. Desire for children among black women with and without HIV infection. J Nurs Scholarsh. 2003;35(1):37–43. doi: 10.1111/j.1547-5069.2003.00037.x. [DOI] [PubMed] [Google Scholar]
- 26.Harvey SM, Bird ST, Henderson JT, Beckman LJ, Huszti HC. He said, she said: concordance between sexual partners. Sex Transm Dis. 2004;31(3):185–191. doi: 10.1097/01.olq.0000114943.03419.c4. [DOI] [PubMed] [Google Scholar]
- 27.Witte SS, El-Bassel N, Gilbert L, Wu E, Chang M. Predictors of discordant reports of sexual and HIV/sexually transmitted infection risk behaviors among heterosexual couples. Sex Transm Dis. 2007;34(5):302–308. doi: 10.1097/01.olq.0000240288.90846.6a. [DOI] [PubMed] [Google Scholar]
- 28.De Walque D. Sero-discordant couples in five African countries: Implications for prevention strategies. Popul Dev Rev. 2007;33(3):501–523. [Google Scholar]
- 29.Ellen JM, Vittinghoff E, Bolan G, Boyer CB, Padian NS. Individuals’ perceptions about their sex partners’ risk behaviors. J Sex Res. 1998;35(4):328–332. [Google Scholar]
- 30.Niccolai LM, Farley TA, Ayoub MA, Magnus M, Kissinger PJ. HIV-infected persons’ knowledge of their sexual partners’ HIV status. AIDS Educ Prev. 2002;14(3):183–189. doi: 10.1521/aeap.14.3.183.23893. [DOI] [PubMed] [Google Scholar]
- 31.Seal DW. Interpartner concordance of self-reported sexual behavior among college dating couples. J Sex Res. 1997;34(1):39–55. [Google Scholar]
- 32.Harvey SM. New kinds of data, new options for HIV prevention among women: a public health challenge. Health Educ Behav. 2000;27(5):566–569. doi: 10.1177/109019810002700503. discussion 570–561. [DOI] [PubMed] [Google Scholar]
- 33.Allen S, Meinzen-Derr J, Kautzman M, et al. Sexual behavior of HIV discordant couples after HIV counseling and testing. AIDS. 2003;17(5):733–740. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- 34.Sweat M, Gregorich S, Sangiwa G, et al. Cost-effectiveness of voluntary HIV-1 counselling and testing in reducing sexual transmission of HIV-1 in Kenya and Tanzania. Lancet. 2000;356(9224):113–121. doi: 10.1016/S0140-6736(00)02447-8. [DOI] [PubMed] [Google Scholar]
- 35.Bentley ME, Spratt K, Shepherd ME, et al. HIV testing and counseling among men attending sexually transmitted disease clinics in Pune, India: changes in condom use and sexual behavior over time. AIDS. 1998;12(14):1869–1877. doi: 10.1097/00002030-199814000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Edwards S. Husband’s involvement boosts contraceptive use among Ethiopian couples. Int Fam Plan Perspect. 1994;20(1):39–40. [Google Scholar]
- 37.Higgins DL, Galavotti C, O’Reilly KR, et al. Evidence for the effects of HIV antibody counseling and testing on risk behaviors. JAMA. 1991;266(17):2419–2429. [PubMed] [Google Scholar]
- 38.Klein H, Elifson KW, Sterk CE. Partner communication and HIV risk behaviors among “at risk” women. Sozial- und Praventivmedizin. 2004;49(6):363–374. doi: 10.1007/s00038-004-3044-8. [DOI] [PubMed] [Google Scholar]
- 39.Helleringer S, Kohler HP. Social networks, perceptions of risk, and changing attitudes towards HIV/AIDS: new evidence from a longitudinal study using fixed-effects analysis. Popul Stud (Camb) 2005;59(3):265–282. doi: 10.1080/00324720500212230. [DOI] [PubMed] [Google Scholar]
- 40.Pequegnat W, Stover E. Behavioral prevention is today’s AIDS vaccine! AIDS. 2000;14(Suppl 2):S1–S7. [PubMed] [Google Scholar]
- 41.Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: a randomised trial. The Voluntary HIV-1 Counseling and Testing Efficacy Study Group. Lancet. 2000;356(9224):103–112. [PubMed] [Google Scholar]
- 42.Smith KP, Watkins SC. Perceptions of risk and strategies for prevention: responses to HIV/AIDS in rural Malawi. Soc Sci Med. 2005;60(3):649–660. doi: 10.1016/j.socscimed.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 43.Chomba E, Allen S, Kanweka W, et al. Evolution of couples’ voluntary counseling and testing for HIV in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008 Jan 1;47(1) doi: 10.1097/QAI.0b013e31815b2d67. [DOI] [PubMed] [Google Scholar]
- 44.Allen S, Karita E, Chomba E, et al. Promotion of couples’ voluntary counselling and testing for HIV through influential networks in two African capital cities. BMC Public Health. 2007;7:349. doi: 10.1186/1471-2458-7-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allen S, Serufilira A, Bogaerts J, et al. Confidential HIV testing and condom promotion in Africa. Impact on HIV and gonorrhea rates. JAMA. 1992;268(23):3338–3343. [PubMed] [Google Scholar]
- 46.Allen S, Van de Perre P, Serufilira A, et al. Human immunodeficiency virus and malaria in a representative sample of childbearing women in Kigali, Rwanda. J Infect Dis. 1991;164(1):67–71. doi: 10.1093/infdis/164.1.67. [DOI] [PubMed] [Google Scholar]
- 47.Roth DL, Stewart KE, Clay OJ, van Der Straten A, Karita E, Allen S. Sexual practices of HIV discordant and concordant couples in Rwanda: effects of a testing and counselling programme for men. Int J STD AIDS. 2001;12(3):181–188. doi: 10.1258/0956462011916992. [DOI] [PubMed] [Google Scholar]
- 48.Fliess J, Levin B, Cho Paik M. Statistical Methods for Rates and Proporations. 3rd ed. Hoboken Wiley-Interscience; 2003. [Google Scholar]
- 49.Kraemer HC, Periyakoil VS, Noda A. Kappa coefficients in medical research. Stat Med. 2002;21(14):2109–2129. doi: 10.1002/sim.1180. [DOI] [PubMed] [Google Scholar]
- 50.Landis J, Koch G. The measure of observer agreement for categorial data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 51.Cicchetti D, Feinstein A. High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. 1990;43:551–558. doi: 10.1016/0895-4356(90)90159-m. [DOI] [PubMed] [Google Scholar]
- 52.Kraemer H, Bloch D. Kappa coefficients in epidemiology: an appraisal of a reappraisal. J Clin Epidemiol. 1988;41(10):959–968. doi: 10.1016/0895-4356(88)90032-7. [DOI] [PubMed] [Google Scholar]
- 53.Ochs EP, Binik YM. The use of couple data to determine the reliability of self-reported sexual behavior. J Sex Res. 1999;36(4):374–384. [Google Scholar]
- 54.Upchurch DM, Weisman CS, Shepherd M, et al. Interpartner reliability of reporting of recent sexual behaviors. Am J Epidemiol. 1991;134(10):1159–1166. doi: 10.1093/oxfordjournals.aje.a116019. [DOI] [PubMed] [Google Scholar]
- 55.Padian NS, Aral S, Vranizan K, Bolan G. Reliability of sexual histories in heterosexual couples. Sex Transm Dis. 1995;22(3):169–172. doi: 10.1097/00007435-199505000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Vos T. Attitudes to sex and sexual behaviour in rural Matabeleland, Zimbabwe. AIDS Care. 1994;6(2):193–203. doi: 10.1080/09540129408258630. [DOI] [PubMed] [Google Scholar]
- 57.Murphy EM, Greene ME, Mihailovic A, Olupot-Olupot P. Was the “ABC” approach (abstinence, being faithful, using condoms) responsible for Uganda’s decline in HIV? PLoS Med. 2006;3(9):e379. doi: 10.1371/journal.pmed.0030379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Serwadda D, Gray RH, Wawer MJ, et al. The social dynamics of HIV transmission as reflected through discordant couples in rural Uganda. AIDS. 1995;9(7):745–750. doi: 10.1097/00002030-199507000-00012. [DOI] [PubMed] [Google Scholar]