Abstract
The longitudinal course and quality of intimate relationships were tested in relation to maternal depressive symptoms in a sample of 1,275 families from the NICHD Study of Early Child Care and Youth Development. Assessments of mothers’ intimate relationship status, intimate relationship quality, and depressive symptoms were obtained on 11 occasions from the birth of a child through age 15. Consistent with predictions, results from hierarchical linear models indicated that maternal depressive symptoms over time were associated with a lower probability of being married and lower levels of relationship quality. The strength of the association between relationship quality and depression was stronger than the linkage between relationship course and depression. Sociodemographic characteristics (e.g., mother age, child gender, ethnicity) were more predictive of trajectories of relationship course than relationship quality. Findings are discussed in terms of efforts to prevent and treat the longitudinal interplay between poor intimate relationship functioning and partners’ psychopathology and its implications for the overall health and well-being of parents, couples, and children.
Intimate partner relationships, including marriage, serve as a central context for adult and child health and development (NICHD, 2006) and as a benchmark of overall family functioning (Greeff, 2000). Parental benefits related to happy partnerships include better health and higher life satisfaction (Dush & Amato, 2005; Lillard & Waite, 1995). Moreover, positive intimate relationships, as indicated by supportive communication exchanges and constructive problem solving skills, reliably co-vary with lower levels of psychological distress among partners (Biglan et al., 1985; Papp, Goeke-Morey, & Cummings, 2007). Despite a strong research base supporting interrelations between intimate partner relationships and parents’ mental health, investigation of the longitudinal associations has received scant attention (see Rehman, Gollan, & Mortimer, 2008). Attention to parents’ relationship functioning over time is well warranted due to implications for their own psychological well-being and their children’s development (NICHD Early Child Care Research Network, 2002).
Empirical and theoretical accounts indicate bi-directional associations between intimate partner relationships and mental health, particularly depression (Beach, Whisman, & O’Leary, 1994; Rehman et al., 2008). Moreover, couple therapies are supported as efficacious treatment of affective disorders such as depression and anxiety (Baucom, Shoham, Mueser, Daiuto, & Stickle, 1998). Partner relationships and depression are uniquely linked in that marital relationships were found to be more affected than other social relationships (i.e., those with relatives and friends) by 6-month prevalence of clinical disorders (Whisman, Sheldon, & Goering, 2000). Furthermore, intimate relationship dysfunction cannot be fully explained by impairment related to psychiatric disorders; associations between marital relationship discord and psychological distress (depression and anxiety symptoms) in a population-based sample remained even after controlling for current mood, anxiety, and substance use disorders (Whisman & Uebelacker, 2006). Thus, the evidence linking relationship functioning and symptoms of psychological distress is robust.
Whereas earlier research in the marital functioning and mental health literature compared married versus non-married individuals and documented that married people generally experience better mental health than non-married individuals (Gove, Hughes, & Style, 1983; Pearlin & Johnson, 1977), recent research has aimed to understand co-variations between intimate relationship functioning and psychological distress. The association between depressive symptoms and interpersonal distress emerges consistently in studies involving both clinical and nonclinical samples (Beach & O’Leary, 1993; Burns, Sayers, & Moras, 1994). Moreover, these associations hold for both men and women and endure across time (e.g., Davila, Karney, Hall, & Bradbury, 2003; see Whisman, 2001). Relational conflict often precedes, maintains, and follows a depressive episode (Barnett & Gotlib, 1988; Burns et al., 1994), although evidence generally supports a bidirectional relationship between relationship processes and partners’ mental health (Davila et al., 2003; Kouros, Papp, & Cummings, 2008).
Given that most research conducted to date has relied on cross-sectional or short-term longitudinal studies (e.g., Davila et al., 2003; Kouros et al., 2008; Whisman & Uebelacker, 2006), there is a pressing need to examine how intimate relationship functioning and maternal depressive symptoms change together over time along a developmental course that maps on to child development. The birth of a child is associated with changes in relationship functioning: not only does the birth of a child predict when some marriages occur, but it also relates to declines in relationship functioning, especially if the parents experienced uncertainty or conflict around the pregnancy (Cox, Paley, Burchinal, & Payne, 1999; Snowden, Schott, Awalt, & Gillis-Knox, 1988). The birth of a child further predicts changes in parents’ psychological distress (Areias, Kumar, Barros, & Figueiredo, 1996), with maternal depressive symptoms increasing as children develop (Najman, Andersen, Bor, O’Callaghan, & Williams, 2000). Thus, capturing the developmental course of linkages between relationship functioning and parental psychological distress as children develop is needed because depressive symptoms and intimate relationships change over time (Rehman et al., 2008; Karney & Bradbury, 1995), and these changes have family-wide effects on parents and children (e.g., parent-child relationships, sibling relationships; Cox & Paley, 1997).
Previous research has suggested that sociodemographic characteristics may place parents at risk for evidencing lower intimate relationship functioning (e.g., less likely to be married and remain married over time, lower levels of marital quality). In addition, such risk characteristics might moderate the associations between maternal depressive symptoms and intimate relationship status or quality (Jones-Webb & Snowden, 1993). As examples, mothers who are younger at the birth of a child or mothers of racial/ethnic minority status are less likely to be married and remain married over time (Graefe & Lichter, 2002). Further evidence suggests that having more children is linked to family members’ stress and declines in marital quality (VanLaningham, Johnson, & Amato, 2001), such that marital functioning may be lower for mothers around the birth of later-born (compared to first-born) children. Finally, although tests of child gender in relation to marital functioning have revealed inconsistent results (Davies & Lindsay, 2001), some research indicates that marriages of parents of children including at least one boy are relatively protected (Katzev, Warner, & Acock, 1994). Studying moderators of the mental health–marital functioning linkage to date has commonly concerned newlywed samples (Davila et al., 2003; Kurdek, 1998), thereby leaving questions about how these processes unfold over time among mothers with young children.
The present study examined the longitudinal associations between maternal depressive symptoms and the course and quality of intimate partnerships over a 15-year span of child development. Both relationship status and quality were examined: Marital status was more predictive than maternal age at first child’s birth of women’s depressive symptoms (Kalil & Kunz, 2002), and relationship theorists have argued that a comprehensive understanding of intimate relationship development is necessary because substantial variation in psychological distress and intimate relationship functioning exists (Rehman et al., 2008). A large community-based sample of families was utilized, facilitating the simultaneous inclusion of multiple covariates previously identified as important to intimate relationship functioning. Levels of psychological distress were investigated because they are highly distressing themselves and predictive of subsequent diagnosable disorders (Lewinsohn, Solomon, Seeley, & Zeiss, 2000).
To test the first hypothesis, multilevel binomial models examined the probability of relationship status (married vs. nonmarried) as a function of partners’ psychological distress. It was hypothesized that depressive symptoms would predict a lower likelihood of being married, given notions of relational rejection or dissolution in contexts of partner depression (Coyne, 1976). Models accounted for sociodemographic covariates of intercept and slope of relationship course, development over time, and previous relationship status to ensure that the associations indicate unique linkages between depression and marital status across time. To test the second hypothesis, multilevel growth models examined levels of and change in relationship quality as a function of psychological distress. Following findings that a depression diagnosis in adolescence predicted marital distress in early adulthood (Gotlib, Lewinsohn, & Seeley, 1998), it was hypothesized that depressive symptoms would predict lower levels of intimate relationship quality among partnered mothers. Models again accounted for covariates of relationship quality at the initial assessment point and in change over time, and further controlled for development or repeated assessment over time, concurrent marital status, and previous marital status. As such, models revealed unique linkages between depression and relationship quality over time.
Method
Study Design
Participants for this study were a subset of families drawn from the National Institute of Child Health and Human Development Study of Early Child Care and Youth Development (NICHD SECCYD), a longitudinal sample of 1,364 children born at 31 hospitals near 10 U.S. research sites during 1991(NICHD Early Child Care Research Network, 2001). The original 1,364 families were selected following a conditional random-sampling plan that ensured the participants reflected the economic, ethnic, and educational diversity of each research site. The SECCYD – designed primarily to examine linkages between variations in childcare characteristics and children’s developmental outcomes over time – collected a wealth of information on childcare, family, and school contexts, and child development. Detailed description of data collection is available on the study Website (http://secc.rti.org). The SECCYD collected extensive information on family members’ characteristics and relationships. As such, the study therefore offers data uniquely suited to examine questions related to maternal development and well-being (Friedman, 2007), in line with the present focus on associations between trajectories of mothers’ intimate relationships and mental health.
Participants
The present study utilizes data from 1,275 families (93.5% of the 1,364 enrolled in the study at birth) for whom a minimum of 3 maternal depression ratings between birth and 15 years were obtained. In the present study’s analysis sample, maternal age at the 0.1-year assessment ranged from 19 to 46 years (M = 28.25, SD = 5.62). An income-to-needs ratio, calculated by dividing the total family income by the U.S. poverty threshold for the appropriate family size, averaged 2.84 (SD = 2.58) at the 0.1-year assessment. Mothers reported the following racial/ethnic distribution: American Indian, Eskimo, and Aleut (0.6%); Asian or Pacific Islander (2.2%); Black or African American (12.1%); White or Caucasian (83.5%); and other (1.6%). Four percent were Hispanic. A dichotomous ethnicity covariate (0 = White, 1 = Racial/Ethnic Minority) was created for analytic purposes. The children of the mothers included in this sample consisted of 661 (51.8%) boys, and nearly half of the children (45%) were first-born.
Overall, the SECCYD maintained very high retention, with over 1,100 (> 80%) of the children and families followed through age 11. Attrition analyses compared the characteristics of the full sample of 1,364 families to the subset included in the present analyses. Based on the 0.1-year assessment, included families had older mothers (M = 28.25 years vs. 26.04 years, t = 3.59, p < .001) and higher financial resources (i.e., income-to-needs ratio) (M = 2.84 vs. 1.94, t = 3.20, p < .01). Also, included mothers were more likely than non-included mothers to be White, 83% vs. 71%, χ2(1, N = 1364) = 9.29, p < .01. Comparisons of included and non-included families indicated no differences in child characteristics of gender or birth order (ps > .10). Important to the present study’s goal of testing intimate relationship status and quality as a function of maternal depressive symptoms, previous analysis of longitudinal SECCYD data revealed no systematic attrition based on maternal depression scores at the 0.1-year assessment (Campbell, Matestic, von Stauffenberg, Mohan, & Kirchner, 2007).
Measures
Intimate relationship course and quality
At each assessment point a standardized interview was conducted with mothers to obtain information on family living arrangements, child health, and parental employment and income. As part of this regular interview, mothers provided detailed information regarding their partner relationship status, including whether they were married, separated, widowed, or divorced. From this interview data, maternal intimate relationship status was coded as married or not married, which, when collected over time, designates the longitudinal course of mothers’ intimate relationships.
Mothers who were living with a spouse or partner completed measures of relationship quality on the Emotional Intimacy subscale of the Personal Assessment of Intimacy in Relationships (PAIR; Shaefer & Olson, 1981). This subscale includes 6 items that tap feelings of relationship emotional closeness and support. Sample items include, “I can state my feelings without him getting defensive” and “I sometimes feel lonely when we’re together” (reversed). Maternal intimate relationship quality scores demonstrated good internal consistency (Cronbach alphas exceeded .80 across the study). Table 1 presents the percentages of married mothers and the descriptive statistics of maternal intimate relationship quality across child development. Due to variations in data collection procedures (NICHD Early Child Care Research Network, 2001), the measure of intimate relationship quality was administered at 0.5, 1.25, and 2 years only to mothers who were part of a subsample collected with U.S. Department of Health and Human Services (HHS) funding. This subsample was based on 6 of 10 research sites. As described below, the data analytic technique accounted for varying sample sizes collected over time.
Table 1.
Maternal Marital Status, Intimate Relationship Quality, and Depressive Symptoms across Child Development
| Child Age (years) | Marital Status (% married) | Relationship Quality | Depressive Symptoms | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| 0.1 | 78.0 | 4.02 | 0.75 | 11.24 | 9.00 |
| 0.5 | 76.5 | 3.95 | 0.78 | 8.92 | 8.31 |
| 1.25 | 74.9 | 3.89 | 0.81 | 9.02 | 8.14 |
| 2 | 73.0 | 3.76 | 0.90 | 9.41 | 8.63 |
| 3 | 72.2 | 3.76 | 0.89 | 9.22 | 8.31 |
| 4.5 | 65.5 | 3.80 | 0.89 | 9.83 | 8.70 |
| 6 | 62.9 | 3.87 | 0.92 | 8.39 | 8.47 |
| 8 | 62.8 | 3.87 | 0.89 | 9.07 | 8.85 |
| 10 | 59.8 | 3.86 | 0.96 | 8.73 | 8.62 |
| 11 | 58.8 | 3.83 | 0.99 | 8.96 | 8.82 |
| 15 | 53.7 | 3.79 | 0.99 | 10.48 | 9.83 |
Note. Ns for marital status range from 1,273 (at 0.1 years) to 929 (at 15 years). Ns for relationship quality range from 1,197 (at 0.1 years) to 762 (at 15 years), with HHS data collection (at 0.5, 1.25, and 2 years) Ns ranging from 345 to 399. Ns for depressive symptoms range from 1,275 (at 0.1 years) to 973 (at 15 years).
Psychological distress
Maternal depressive symptoms were assessed using the Center for Epidemiological Studies-Depression scale (CES-D; Radloff, 1977), a twenty-item self-report instrument. Respondents indicated how frequently they have been bothered by the listed depressive symptoms during the past week, ranging from 0 (less than one day) to 3 (five to seven days). Examples include “I felt that everything I did was an effort” and “I was bothered by things that usually don’t bother me.” Individuals diagnosed with clinical depression score higher on the CES-D than nondepressed individuals (Weissman et al., 1996). The CES-D is widely used to assess depressive symptoms among normative samples, including research focusing on mental health and family functioning linkages (e.g., Brody & Flor, 1997). Mothers’ CES-D scores demonstrated high internal consistency in the current sample (Cronbach alphas ranged from .88 to .92). Table 1 presents descriptive statistics of maternal depression across child development.
Results
Data Analysis
The present study’s hypotheses were tested with hierarchical linear modeling (HLM; Raudenbush, Bryk, Cheong, & Congdon, 2004). HLM is well-suited to test hypotheses involving variables that have been collected repeatedly over time, and offers the advantages of allowing uneven interval spacing between assessments and accommodating individually-varying number of data points (Papp, 2004; Raudenbush & Bryk, 2002). Of particular relevance to the present study, HLM derives parameters from repeated measurements assessed for each participant over time (in Level 1), which are averaged simultaneously across all participants and related to person-level characteristics (in Level 2). Specifically, HLM estimated longitudinal trajectories (i.e., intercept and slope parameters) of intimate relationship course (Hypothesis 1) and intimate relationship quality (Hypothesis 2) as predicted by other time-varying variables (e.g., maternal depression, child age) for each participating mother, and then related these averaged trajectories to person-level characteristics (i.e., sociodemographic risk variables). All available data were used due to maximum likelihood estimation (Raudenbush, 2001).
In testing the first hypothesis of whether maternal depression predicts lower likelihood of marital course over time, the Level 1 model included repeated assessments of relationship status (0 = not married, 1 = married) as the outcome variable. Accordingly, hierarchical generalized linear modeling (HGLM), an extension of HLM that estimates a Bernoulli sampling model to appropriately predict binary dependent variables, was utilized (Raudenbush & Bryk, 2002). To address the second hypothesis of whether maternal depression and intimate relationship quality are negatively associated over time, HLM for continuous outcomes was utilized.
Maternal Depressive Symptoms and Course of Intimate Relationships
An unconditional hierarchical generalized linear model that regressed on intimate relationship status the predictors of maternal depression, child age (i.e., timing of each assessment), and previous relationship status revealed a negative association between maternal depressive symptoms and likelihood of being married, γ100 = −0.027, t = −10.84, p < .001. However, as described above, the aim was to test the hypothesis in a model that appropriately included relevant sociodemographic variables that might account for or moderate the depression – intimate relationship course linkage. Accordingly, at Level 1, a mother’s likelihood of intimate relationship course (0 = not married, 1 = married) was predicted by child age (in years, starting with the 0.1-year assessment) and previous relationship status (0 = not married at previous assessment, 1 = married at previous assessment, to account for autoregressive effects of being married on subsequent status). The remaining variance in mothers’ likelihood of being married, after accounting for timing of child development and previous marital status, was predicted by mothers’ depressive symptoms (matched by child age), such that the resulting Level 1 Bernoulli sampling model is:
At Level 2, child gender (1 = male, 2 = female), child birth order (0 = later born, 1 = first born), maternal age, and maternal racial/ethnic status (0 = White, 1 = Minority) were entered as covariates (all centered on the sample mean) that predicted the relationship status intercept, or the likelihood of being married at the initial assessment (β00), and the relationship status slope, or the change over time in the likelihood of being married (β20):
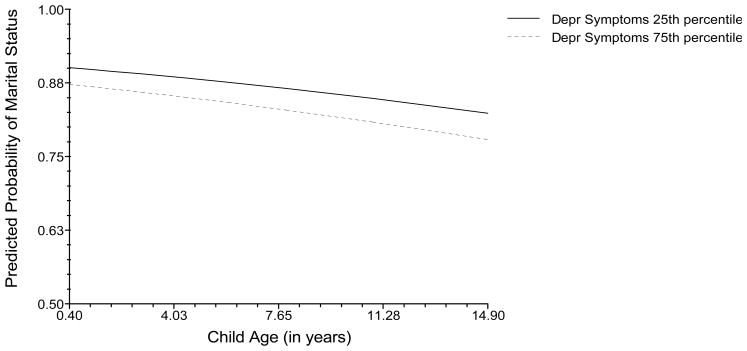
In sum, this hierarchical generalized linear model (shown in Table 2) yields the longitudinal association between maternal depressive symptoms and likelihood of being married, accounting for effects of child development and previous marital status (Level 1) and previously identified sociodemographic covariates (Level 2). As predicted, maternal depressive symptomatology was associated with a lower likelihood of being married across child development (γ100 = −0.028, t = −10.60, p < .001, effect size r = .28). Figure 1 shows the longitudinal association between intimate relationship course and maternal psychological distress at different levels of mothers’ depressive symptoms. Results shown in Table 2 indicate that the likelihood of being married at the initial assessment was higher for older mothers and White mothers. In addition, the significant decline in the likelihood of being married over time was moderated such that the decline was stronger for mothers of boys, younger mothers, and mothers of race/ethnicity minority status. Previous marital status was also a significant positive predictor of current marital status (see Table 2).
Table 2.
Hierarchical Linear Model of Association between Intimate Relationship Course and Maternal Depressive Symptoms across Child Development
| Fixed Effect | Coefficient | SE |
|---|---|---|
| Intercept (Y = Likelihood of being Married), γ000 | −1.342*** | 0.067 |
| Child Gender, γ001 | −0.058 | 0.065 |
| Child Birth Order, γ002 | −0.041 | 0.065 |
| Maternal Age, γ003 | 0.052*** | 0.007 |
| Maternal Ethnicity, γ004 | −0.603*** | 0.084 |
| Maternal Depressive Symptoms, γ100 | −0.028*** | 0.003 |
| Child Age, γ200 | −0.046*** | 0.004 |
| Child Gender, γ201 | −0.018* | 0.009 |
| Child Birth Order, γ202 | 0.009 | 0.009 |
| Maternal Age, γ203 | −0.005*** | 0.001 |
| Maternal Ethnicity, γ204 | 0.028* | 0.012 |
| Previous Marital Status, γ300 | 4.687*** | 0.067 |
p ≤ .05.
p ≤ .001.
Note. Level 1 predictors are uncentered; Level 2 variables are grand mean centered.
Figure 1.
Association between likelihood of being married and maternal depressive symptoms across child development. The model controls for previous marital status and sociodemographic covariates.
Depr = Depression
A final model tested whether the sociodemographic covariates (i.e., child gender, child birth order, mother age, and mother ethnicity) moderated the maternal depression – relationship course linkage (β10j). The HGLM results indicated no significant moderator effects (ps > .05), suggesting that the lower likelihood of being married in relation to depressive symptoms is robust across child and mother characteristics.
Maternal Depressive Symptoms and Quality of Intimate Relationships
An unconditional hierarchical linear model that regressed on intimate relationship quality the predictors of maternal depression, child age (i.e., timing of each assessment), concurrent relationship status, and previous relationship status revealed a negative association between maternal depressive symptoms and quality of intimate relationships, γ100 = −0.037, t = −25.21, p < .001. Again, as described above, the aim was to test the hypothesis in a model that included relevant sociodemographic covariates that might account for or moderate the depression – intimate relationship quality linkage. Accordingly, at Level 1, a mother’s ratings of intimate relationship quality were predicted by child age (in years, starting with the 0.1-year assessment), concurrent marital status (0 = not married, 1 = married), and previous marital status (0 = not married at previous assessment, 1 = married at previous assessment, to account for autoregressive effects of being married on intimate relationship quality). The remaining variance in mothers’ intimate relationship quality, after accounting for child development and marital status, was predicted by mothers’ depressive symptoms (matched by child age), such that the resulting Level 1 model is:
At Level 2, child gender (1 = male, 2 = female), child birth order (0 = later born, 1 = first born), maternal age, and maternal race/ethnicity (0 = White, 1 = Minority) were entered as covariates (all centered on the sample mean) that predicted the intimate relationship quality intercept (β00) and intimate relationship quality slope (β20):
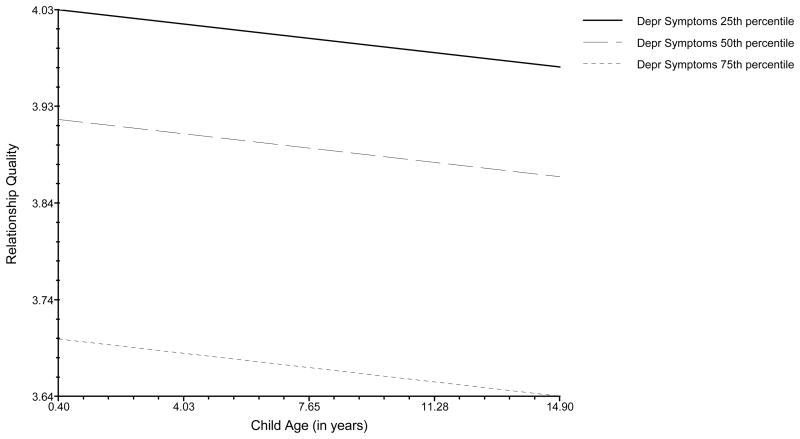
In sum, this model (shown in Table 3) yields the association between maternal depressive symptoms and intimate relationship quality, accounting for effects of child development and marital status (Level 1) and previously identified sociodemographic covariates (Level 2). As predicted, maternal depressive symptomatology was negatively associated with intimate relationship quality across child development, (γ100 = −0.037, t = −25.25, p < .001, effect size r = .59). Figure 2 shows the longitudinal association between intimate relationship quality and maternal psychological distress at different levels of mothers’ depressive symptoms. Results further indicated that mothers of boys reported marginally lower levels of marital quality at the initial assessment, and that the decline of relationship quality over time was stronger for mothers of children who were later-born compared to first-born. In addition, intimate relationship quality was not predicted by concurrent marital status, although being married at the previous assessment was associated with lower levels of intimate relationship functioning over time (see Table 3).
Table 3.
Hierarchical Linear Model of Association between Intimate Relationship Quality and Maternal Depressive Symptoms across Child Development
| Fixed Effect | Coefficient | SE |
|---|---|---|
| Intercept (Y = Relationship Quality), γ000 | 4.304*** | 0.050 |
| Child Gender, γ001 | −0.080† | 0.045 |
| Child Birth Order, γ002 | 0.025 | 0.047 |
| Maternal Age, γ003 | −0.003 | 0.005 |
| Maternal Ethnicity, γ004 | −0.020 | 0.078 |
| Maternal Depressive Symptoms, , γ100 | −0.037*** | 0.001 |
| Child Age, γ200 | −0.004 | 0.002 |
| Child Gender, γ201 | −0.001 | 0.005 |
| Child Birth Order, γ202 | −0.010* | 0.005 |
| Maternal Age, γ203 | −0.001 | 0.0005 |
| Maternal Ethnicity, γ204 | −0.0001 | 0.008 |
| Concurrent Marital Status, γ300 | 0.066 | 0.060 |
| Previous Marital Status, γ400 | −0.248*** | 0.050 |
p ≤ .76.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Note. Level 1 predictors are uncentered; Level 2 variables are grand mean centered.
Figure 2.
Association between intimate relationship quality and maternal depressive symptoms across child development. The model controls for concurrent marital status, previous marital status, and sociodemographic covariates.
Depr = Depression
A final model tested whether the sociodemographic risks (i.e., child gender, child birth order, mother age, and mother ethnicity) moderated the maternal depression – relationship quality linkage (β10j). The HLM results again indicated no significant moderator effects (ps > .05), suggesting that the negative longitudinal association between maternal depressive symptoms and intimate relationship quality is robust across child and mother characteristics.
Discussion
Extending research based on cross-sectional and short-term longitudinal designs, the present study documented associations between intimate relationship functioning and maternal psychological distress across a 15-year span of child development. Specifically, mothers’ depression symptoms over time predicted (1) lower likelihood of marriage and (2) lower levels of intimate relationship functioning among partnered mothers. Both statistical models incorporated time-varying (e.g., previous marital status) and person-level (e.g., sociodemographic risk) covariates, thereby increasing our confidence in the documented longitudinal intimate relationship functioning – mental health linkages.
Interestingly, examination of HLM effect sizes indicated that maternal depressive symptoms were more strongly associated with intimate relationship quality than relationship course. At the same time, sociodemographic covariates were more predictive of relationship course than quality, with mothers who were older at time of the child’s birth and White mothers having a higher likelihood of being married at the initial assessment. In addition, the significant decline in the likelihood of being married over time was more pronounced for mothers of boys, younger mothers, and racial/ethnic Minority mothers. Taken together, results indicate that the status of the marital partnership may be more connected than relationship quality to broader demographic characteristics, but that among partnered parents, quality of intimate relationships is strongly predicted by mothers’ depressive symptoms. These findings extend research on the mental health – relationship functioning linkage based overwhelmingly on cross-sectional or short-term longitudinal studies that have limited ability to account for previous marital status and capture long-term associations. The present study offered the advantage of a large, diverse sample that allowed sociodemographic covariates to be modeled simultaneously. Moreover, the sociodemographic risk factors did not attenuate longitudinal associations between depressive symptoms and intimate relationship functioning, indicating that the connection between intimate relationship functioning and mental health is relatively robust across multiple maternal and child characteristics (e.g., ethnicity, birth order).
The present study’s findings are line with Coyne’s interactional theory of depression (1976) that posits depression elicits rejection or relationship dissolution, broadly indexed in this sample of mothers as nonmarried status and relationship dissatisfaction, which may be predictive of relationship dissolution. A necessary next step is research to examine the processes through which such rejection or dissolution occurs. For example, Coyne’s model further posits that excessive reassurance seeking by a person with depression, and negative affect induced in the depressed person’s partner, lead to eventual rejection. It would be interesting for future research to test the role of reassurance seeking and negativity in parents’ depression-relationship functioning processes. Other theoretical frameworks contribute alternate pathways for investigation, perhaps through lower levels of available support or disrupted communication among parents with elevated depressive symptoms (Beach, Sandeen, & O’Leary, 1990). Clearly, additional research is needed to identify underpinnings of the longitudinal association between intimate relationship functioning and psychological distress.
Given that the associations between intimate relationship functioning and psychological distress were studied over the course of child development, the present study also contributes to our understanding of parental and child development in family contexts. First, family systems theory posits inter-connections among family members and family processes (Cox & Paley, 1997). Accordingly, associations found in the present results are hypothesized to impact parent-child relationships, sibling relationships, and broader family processes. Second, the findings also contribute to a developmental psychopathology perspective, (Cummings, Davies, & Campbell, 2000), which posits children’s development to occur in contexts of multiple positive and negative processes. As such, future research should examine associations between parents’ relationship development, mental health, and a range of child developmental outcomes (e.g., behavior problems, psychological distress, conflictual relationships with siblings or peers) in light of the results documented here.
The present study’s contributions should be considered keeping in mind several limitations. First, although previous research has documented concurrent and short-term longitudinal relations between marital relationship functioning and mental health for both men and women (Davila et al., 2003), the present analyses included assessments of mothers only. Future research should study mothers and partners across child development to test whether relations vary for men versus women in context of dyadic data. Second, similar to other research on mental health and interpersonal processes, the diversity along some of the sociodemographic characteristics was restricted (Glass, Mendes De Leon, Bassuk, & Berkman, 2006; Kalil & Kunz, 2002). For example, limiting the racial/ethnicity status variable to a White versus Minority dichotomy was statistically necessary, but does not reflect the sociocultural landscape of families in the U.S. Also, testing the associations in samples with more variability in partner status is needed, as the present study’s variability on partnered and cohabiting couples was too limited to analyze. Studying the present questions in a broader range of samples of families is needed to reflect the diversity of household structures in which children live and develop (Adam & Chase-Lansdale, 2002). Finally, intimate relationship functioning was treated as the outcome variable here given the aim of understanding the longitudinal course and quality of parents’ intimate relationships. However, the results are correlational in nature and do not indicate whether (1) depressive symptoms predict future relationship distress or (2) problematic intimate relationships predict subsequent parental depression. The present results establish a foundation for future work to incorporate causal modeling (i.e., latent difference score models, McArdle & Hamagami, 2001) in order to determine whether one process is leading the other over time, or whether reciprocal, dynamic relations exist.
In summary, the present study’s results point to significant longitudinal co-variation between intimate relationship functioning and depression symptoms among mothers across the course of children’s development. The results were unique of effects of current relationship status and a number of potential sociodemographic covariates. Continued investigation of subthreshold symptom processes holds particular promise for improving effectiveness of clinical treatment and intervention (Rivas-Vazquez, Saffa-Biller, Ruiz, Blais, & Rivas-Vazquez, 2004). The results also support interventions for mothers around the time of a child’s birth (Misri, Reebye, Milis, & Shah, 2006) as well as couple therapy approaches to treat partners’ depression symptoms (Baucom et al., 1998; Denton, Golden, & Walsh, 2003). The present results document significant connections between intimate relationship functioning and mothers’ depression across time, and thereby elucidate characteristics that place parents and children at risk for experiencing a negative cycle between interpersonal processes and mental health. Continued research efforts are needed to improve our ability to prevent and treat the longitudinal interplay between poor intimate relationship functioning and partners’ psychopathology, in line with broader goals of improving overall health and well-being of parents, couples, and children (NICHD, 2006).
Acknowledgments
This study was conducted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Early Child Care Research Network supported by NICHD through a cooperative agreement that calls for scientific collaboration between the grantees and the NICHD staff. I gratefully acknowledge the use of the NICHD Study of Early Child Care and Youth Development data, and express my appreciation to the study investigators and personnel, including those who facilitated the 2004 American Psychological Association Advanced Training Institute on using large-scale databases, and the study participants. This research was supported by Grant R03 HD057346.
References
- Adam EK, Chase-Lansdale PL. Home sweet home(s): Parental separations, residential moves, and adjustment problems in low-income adolescent girls. Developmental Psychology. 2002;38:792–805. [PubMed] [Google Scholar]
- Areias MEG, Kumar R, Barros H, Figueiredo E. Comparative incidence of depression in women and men, during pregnancy and after childbirth. Validation of the Edinburgh postnatal depression scale in Portuguese mothers. British Journal of Psychiatry. 1996;169:30–35. doi: 10.1192/bjp.169.1.30. [DOI] [PubMed] [Google Scholar]
- Barnett PA, Gotlib IH. Psychosocial functioning and depression: Distinguishing among antecedents, concomitants, and consequences. Psychological Bulletin. 1988;104:97–126. doi: 10.1037/0033-2909.104.1.97. [DOI] [PubMed] [Google Scholar]
- Baucom DH, Shoham V, Mueser KT, Daiuto AD, Stickle TR. Empirically supported couple and family interventions for marital distress and adult mental health problems. Journal of Consulting and Clinical Psychology. 1998;66:53–88. doi: 10.1037//0022-006x.66.1.53. [DOI] [PubMed] [Google Scholar]
- Beach SRH, O’Leary KD. Dysphoria and marital discord: Are dysphoric individuals at risk for maladjustment? Journal of Marital and Family Therapy. 1993;19:355–368. doi: 10.1111/j.1752-0606.1993.tb00998.x. [DOI] [PubMed] [Google Scholar]
- Beach SRH, Sandeen EE, O’Leary KD. Depression in marriage: A model for etiology and treatment. New York: Guilford Press; 1990. [Google Scholar]
- Beach SRH, Whisman MA, O’Leary KD. Marital therapy for depression: Theoretical foundation, current status, and future directions. Behavior Therapy. 1994;25:345–371. [Google Scholar]
- Biglan A, Hops H, Sherman L, Friedman LS, Arthur J, Osteen V. Problem- solving interactions of depressed women and their husbands. Behavior Therapy. 1985;16:431–451. [Google Scholar]
- Brody GH, Flor DL. Maternal psychological functioning, family processes, and child adjustment in rural, single-parent, African American families. Developmental Psychology. 1997;33:1000–1011. doi: 10.1037//0012-1649.33.6.1000. [DOI] [PubMed] [Google Scholar]
- Burns DD, Sayers SL, Moras K. Intimate relationships and depression: Is there a causal connection? Journal of Consulting and Clinical Psychology. 1994;62:1033–1043. doi: 10.1037//0022-006x.62.5.1033. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Cox MJ, Paley B. Families as systems. Annual Review of Psychology. 1997;48:243–267. doi: 10.1146/annurev.psych.48.1.243. [DOI] [PubMed] [Google Scholar]
- Cox MJ, Paley B, Burchinal M, Payne CC. Marital perceptions and interactions across the transition to parenthood. Journal of Marriage and the Family. 1999;61:611–625. [Google Scholar]
- Coyne JC. Toward an interactional description of depression. Psychiatry. 1976;39:28–40. doi: 10.1080/00332747.1976.11023874. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Developmental psychopathology and family process: Theory, research, and clinical implications. New York: Guilford Press; 2000. [Google Scholar]
- Davies PT, Lindsay LL. Does gender moderate the effects of marital conflict on children? In: Grych JH, Fincham FD, editors. Interparental conflict and child development: Theory, research, and applications. New York: Cambridge; 2001. pp. 64–97. [Google Scholar]
- Davila J, Karney BR, Hall TW, Bradbury TN. Depressive symptoms and marital satisfaction: Within-subject associations and the moderating effects of gender and neuroticism. Journal of Family Psychology. 2003;17:557–570. doi: 10.1037/0893-3200.17.4.557. [DOI] [PubMed] [Google Scholar]
- Denton WH, Golden RN, Walsh SR. Depression, marital discord and couple therapy. Current Opinion in Psychiatry. 2003;16:29–34. [Google Scholar]
- Dush CMK, Amato PA. Consequences of relationship status and quality for subjective well-being. Journal of Social and Personal Relationships. 2005;22:607–627. [Google Scholar]
- Friedman SL. Finding treasure: Data sharing and secondary analysis in developmental science. Journal of Applied Developmental Psychology. 2007;28:384–389. [Google Scholar]
- Gotlib IH, Lewinsohn PM, Seeley JR. Consequences of depression during adolescence: Marital status and marital functioning in early adulthood. Journal of Abnormal Psychology. 1998;107:686–690. doi: 10.1037//0021-843x.107.4.686. [DOI] [PubMed] [Google Scholar]
- Gove WR, Hughes M, Style CB. Does marriage have positive effects on the psychological well-being of the individual? Journal of Health and Social Behavior. 1983;24:122–131. [PubMed] [Google Scholar]
- Graefe DR, Lichter DT. Marriage among unwed mothers: Whites, Blacks and Hispanics compared. Perspectives on Sexual and Reproductive Health. 2002;34:286–293. [PubMed] [Google Scholar]
- Greeff AP. Characteristics of families that function well. Journal of Family Issues. 2000;21:948–962. [Google Scholar]
- Jones-Webb RJ, Snowden LR. Symptoms of depression among Blacks and Whites. American Journal of Public Health. 1993;83:240–244. doi: 10.2105/ajph.83.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalil A, Kunz J. Teenage childbearing, marital status, and depressive symptoms later in life. Child Development. 2002;73:1748–1760. doi: 10.1111/1467-8624.00503. [DOI] [PubMed] [Google Scholar]
- Karney BR, Bradbury TN. The longitudinal course of marital quality and stability: A review of theory, methods, and research. Psychological Bulletin. 1995;118:3–34. doi: 10.1037/0033-2909.118.1.3. [DOI] [PubMed] [Google Scholar]
- Katzev AR, Warner RL, Acock AC. Girls or boys? Relationship of child gender to marital instability. Journal of Marriage and the Family. 1994;56:89–100. [Google Scholar]
- Kouros CD, Papp LM, Cummings EM. Interrelations and moderators of longitudinal links between marital satisfaction and depressive symptoms among couples in established relationships. Journal of Family Psychology. 2008;22:667–677. doi: 10.1037/0893-3200.22.5.667. [DOI] [PubMed] [Google Scholar]
- Kurdek LA. The nature and predictors of the trajectory of change in marital quality over the first 4 years of marriage for first-married husbands and wives. Journal of Family Psychology. 1998;12:494–510. doi: 10.1037//0012-1649.35.5.1283. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. Journal of Abnormal Psychology. 2000;109:345–351. [PubMed] [Google Scholar]
- Lillard LE, Waite LJ. Til death do us part: Marital disruption and mortality. American Journal of Sociology. 1995;100:1131–1156. [Google Scholar]
- McArdle JJ, Hamagami F. Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. In: Collins LM, Sayer AG, editors. New methods for the analysis of change. Washington, DC: American Psychological Association; 2001. pp. 137–175. [Google Scholar]
- Misri S, Reebye P, Milis L, Shah S. The impact of treatment intervention on parenting stress in postpartum depressed mothers: A prospective study. American Journal of Orthopsychiatry. 2006;76:115–119. doi: 10.1037/0002-9432.76.1.115. [DOI] [PubMed] [Google Scholar]
- Najman JM, Andersen MJ, Bor W, O’Callaghan MJ, Williams GM. Postnatal depression--myth and reality: Maternal depression before and after the birth of a child. Social Psychiatry and Psychiatric Epidemiology. 2000;35:19–27. doi: 10.1007/s001270050004. [DOI] [PubMed] [Google Scholar]
- NICHD. Marriage and couple relationships. 2006 October 18; Retrieved December 12, 2006, from http://www.nichd.nih.gov/about/org/cpr/dbs/prog_dem/marriage.cfm.
- NICHD Early Child Care Research Network. Nonmaternal care and family factors in early development: An overview of the NICHD Study of Early Child Care. Journal of Applied Developmental Psychology. 2001;22:457–492. [Google Scholar]
- NICHD Early Child Care Research Network. The interaction of child care and family risk in relation to child development at 24 and 36 months. Applied Developmental Science. 2002;6:144–156. [Google Scholar]
- Papp LM. Capturing the interplay among within- and between-person processes using multilevel modeling techniques. Applied and Preventive Psychology. 2004;11:115–124. [Google Scholar]
- Papp LM, Goeke-Morey MC, Cummings EM. Linkages between spouses’ psychological distress and marital conflict in the home. Journal of Family Psychology. 2007;21:533–537. doi: 10.1037/0893-3200.21.3.533. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Johnson JS. Marital status, life-strains and depression. American Sociological Review. 1977;42:704–715. [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raudenbush SW. Toward a coherent framework for comparing trajectories of individual change. In: Collins LM, Sayer AG, editors. New methods for the analysis of change. Washington, DC: American Psychological Association; 2001. pp. 33–64. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon RT. HLM6: Hierarchical linear and nonlinear modeling. Chicago, IL: Scientific Software International; 2004. [Google Scholar]
- Rehman US, Gollan J, Mortimer AR. The marital context of depression: Research, limitations, and new directions. Clinical Psychology Review. 2008;28:179–198. doi: 10.1016/j.cpr.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Rivas-Vazquez RA, Saffa-Biller D, Ruiz I, Blais MA, Rivas-Vazquez A. Current issues in anxiety and depression: Comorbid, mixed, and subthreshold disorders. Professional Psychology: Research and Practice. 2004;35:74–83. [Google Scholar]
- Shaefer MT, Olson DH. Assessing intimacy: The PAIR inventory. Journal of Marital and Family Therapy. 1981;7:640–653. [Google Scholar]
- Snowden LR, Schott TL, Awalt SJ, Gillis-Knox J. Marital satisfaction in pregnancy: Stability and change. Journal of Marriage and the Family. 1988;50:325–333. [Google Scholar]
- VanLaningham J, Johnson DR, Amato P. Marital happiness, marital duration, and the U-shaped curve: Evidence from a five-wave panel study. Social Forces. 2001;79:1313–1341. [Google Scholar]
- Weissman MM, Bland RC, Canino GF, Faravelli C, Greenwald S, Hwu HG, et al. Cross-national epidemiology of major depression and bipolar disorder. Journal of the American Medical Association. 1996;276:293–299. [PubMed] [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family processes in depression: A scientific foundation for clinical practice. Washington, DC: American Psychological Association; 2001. pp. 3–24. [Google Scholar]
- Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology. 2000;109:803–808. doi: 10.1037//0021-843x.109.4.803. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA. Impairment and distress associated with relationship discord in a national sample of married or cohabitating adults. Journal of Family Psychology. 2006;20:369–377. doi: 10.1037/0893-3200.20.3.369. [DOI] [PubMed] [Google Scholar]