Abstract
Introduction
Central venous oxygen saturation (ScvO2) is a useful therapeutic target in septic shock and high-risk surgery. We tested the hypothesis that central venous-to-arterial carbon dioxide difference (P(cv-a)CO2), a global index of tissue perfusion, could be used as a complementary tool to ScvO2 for goal-directed fluid therapy (GDT) to identify persistent low flow after optimization of preload has been achieved by fluid loading during high-risk surgery.
Methods
This is a secondary analysis of results obtained in a study involving 70 adult patients (ASA I to III), undergoing major abdominal surgery, and treated with an individualized goal-directed fluid replacement therapy. All patients were managed to maintain a respiratory variation in peak aortic flow velocity below 13%. Cardiac index (CI), oxygen delivery index (DO2i), ScvO2, P(cv-a)CO2 and postoperative complications were recorded blindly for all patients.
Results
A total of 34% of patients developed postoperative complications. At baseline, there was no difference in demographic or haemodynamic variables between patients who developed complications and those who did not. In patients with complications, during surgery, both mean ScvO2 (78 ± 4 versus 81 ± 4%, P = 0.017) and minimal ScvO2 (minScvO2) (67 ± 6 versus 72 ± 6%, P = 0.0017) were lower than in patients without complications, despite perfusion of similar volumes of fluids and comparable CI and DO2i values. The optimal ScvO2 cut-off value was 70.6% and minScvO2 < 70% was independently associated with the development of postoperative complications (OR = 4.2 (95% CI: 1.1 to 14.4), P = 0.025). P(cv-a)CO2 was larger in patients with complications (7.8 ± 2 versus 5.6 ± 2 mmHg, P < 10-6). In patients with complications and ScvO2 ≥71%, P(cv-a)CO2 was also significantly larger (7.7 ± 2 versus 5.5 ± 2 mmHg, P < 10-6) than in patients without complications. The area under the receiver operating characteristic (ROC) curve was 0.785 (95% CI: 0.74 to 0.83) for discrimination of patients with ScvO2 ≥71% who did and did not develop complications, with 5 mmHg as the most predictive threshold value.
Conclusions
ScvO2 reflects important changes in O2 delivery in relation to O2 needs during the perioperative period. A P(cv-a)CO2 < 5 mmHg might serve as a complementary target to ScvO2 during GDT to identify persistent inadequacy of the circulatory response in face of metabolic requirements when an ScvO2 ≥71% is achieved.
Trial registration
Clinicaltrials.gov Identifier: NCT00852449.
Introduction
Adequate tissue perfusion is an essential component of oxygenation during high-risk surgery and may improve outcome [1,2]. Careful monitoring of fluid administration by individualized goal-directed therapy (GDT) has been shown to reduce organ failure and hospital stay [3-5]. As a supplement to routine cardiovascular monitoring, GDT aims to optimize O2 delivery (DO2) through defined goals, based on maximization of flow-related haemodynamic parameters [6-10], while avoiding hypovolaemia and fluid overload which may alter tissue oxygenation [11,12].
In addition, the use of early warning signals of tissue hypoxia, such as central venous oxygen saturation (ScvO2), which reflects important changes in the O2 delivery/consumption (DO2/VO2) relationship, has been found to be useful during high-risk surgery [13-15]. Indeed, previous studies have shown that changes in ScvO2 closely reflect circulatory disturbances during periods of tissue hypoxia [16], and that low ScvO2 is associated with increased postoperative complications [13-15]. Furthermore, by closely monitoring of tissue O2 extraction, calculated from ScvO2, early correction of altered tissue oxygenation with appropriate fluid loading in conjunction with low doses of inotropes was found to reduce postoperative organ failure in patients with poor O2 utilization [13].
In a recent randomized study of patients treated with an individualized GDT protocol [17], we found that, despite optimization of preload with repeated fluid loading, excessive fluid restriction increased postoperative complications in parallel with reduced ScvO2 values [17]. The ScvO2threshold value for predicting complications (approximately 71%) was similar to those reported previously [14,15]. Significant ScvO2 fluctuations may occur during both surgery and sepsis, and high ScvO2 values do not necessarily reflect changes in DO2 and macrocirculatory adequacy [18,19], which may therefore limit the clinical relevance of ScvO2 in routine practice. Persistent tissue hypoperfusion with increased ScvO2 and O2 extraction defects might be related to microcirculatory and/or mitochondrial failure [19,20].
Interestingly, central venous-to-arterial PCO2 (Pcv-aCO2), with central venous PCO2 as a surrogate for mixed venous PCO2 [21], has recently been proposed as a useful tool for GDT in ICU-septic patients to identify persistent hypoperfusion when a ScvO2 > 70% has been reached [20]. Decreased tissue blood flow (ischemic hypoxia) represents the major determinant in increased P(v-a)CO2 [22], and P(v-a)CO2 could therefore be considered as an indicator of adequate venous blood flow to remove CO2 produced by peripheral tissues [23,24].
The results of a previous study, which included patients treated with intraoperative GDT [17], were used to investigate whether P(cv-a)CO2 is useful for discriminating patients at risk of developing postoperative complications. It was hypothesized that P(cv-a)CO2 may be a useful complementary tool when a threshold ScvO2 value has been reached by individualized GDT during major abdominal surgery.
Materials and methods
Patients
The study that provided data [17] used here was approved by our Institutional Review Board, and all patients provided written informed consent. Data were collected from eligible patients with an ASA score of I to III scheduled for surgery with an expected duration of > 60 minutes. Surgical procedures included colon/rectum resections, gastric resections, duodenopancreatectomy and hepatectomy. Exclusion criteria included: age < 18 years, body mass index > 35 kg m-2, pregnancy, chronic obstructive pulmonary disease with forced expiratory volume in 1 sec < 50%, emergency surgery, coagulopathy, sepsis or systemic inflammatory response syndrome [25], significant hepatic (prothrombin ratio < 50%, factor V < 50%) or renal failure (creatinine > 50% upper limit of normal value), and those in whom epidural analgesia was contraindicated.
Study protocol
The protocol and design of the original study have been described in detail elsewhere [17]. Briefly, patients were randomly assigned by a concealed allocation approach (computer-generated codes), using opaque sealed envelopes containing the randomization schedule, to 6 mL kg-1 h-1(restricted-GDT group) or 12 mL kg-1 h-1(conventional-GDT group) of crystalloids (lactated Ringer's solution), reflecting current clinical practice for restricted (R-GDT group) and more conventional (C-GDT group) fluid administration [26]. Study investigators, but not anaesthesiologists, were blinded to treatment assignments. Immediately after induction of anaesthesia, an oesophageal Doppler probe (HemoSonic 100, Arrow International, Everett, MA, USA) was inserted and adjusted to obtain the highest velocity signal from the descending aorta. Respiratory variations in peak aortic flow velocity (deltaPV) were monitored as described previously [27,28], and stroke volume and cardiac output were recorded continuously. Additional fluid boluses of 250 mL hydroxethylstarch (HES 130/0.4, Voluven®; Fresenius-Kabi, Bad Hamburg, Germany) were given in order to maintain deltaPV below 13% [28]. The fluid challenge was repeated (up to 50 mL kg-1), if necessary, until deltaPV was corrected. In other cases (deltaPV < 13% and evidence of haemodynamic instability), a vasoactive/inotropic support (ephedrine chlorhydrate or dobutamine) could be added. Blood was transfused in order to maintain haemoglobin > 8 g dL-1 in all patients, or > 10 g dL-1 in patients with a history of coronary artery disease. Perioperative management was similar in all patients except for the basal rate of intraoperative crystalloids.
Data collection and outcome measures
Preoperatively, patients were equipped with central venous (positioned with the tip within the superior vena cava) and arterial catheters. Arterial and central venous blood gas analyses were performed by intermittent blood sampling and co-oximetry (IL Synthesis, Instrumentation Laboratory®, Lexington, MA, USA) 10 minutes before surgery (baseline), hourly throughout surgery and until discharge from the post-acute care unit (PACU). This equipment was calibrated each hour, and routine quality control checks were performed. Anaesthesiologists were blinded to ScvO2and Pcv-aCO2 measurements during the course of surgery, which were, therefore, not used to guide clinical management at any stage of the study.
During surgery, the following parameters were recorded: electrocardiogram, pulse oximetry, invasive arterial pressure, cardiac output, oxygen delivery index (DO2i), the infused volume of crystalloids, HES, the need for packed red blood cells (PRBCs) and vasoactive/inotrope support, and urine output. Serum lactate, haemoglobin, creatinine, C-reactive protein (CRP), procalcitonin (PCT) and albumin levels were measured at PACU admission and during the 48 h following surgery. Minimal ScvO2 (minScvO2) was considered as the lowest value during the course of surgery.
Postoperative complications were recorded systematically and assessed according to previously defined criteria [6,29,30]. For the purpose of this study, and to assess the effect of abnormal perfusion on tissue oxygenation, we focused specifically on postoperative septic complications, which seem the most relevant clinically in the context of digestive surgery. Diagnosis of postoperative sepsis was based on international consensus guidelines [25]. Infection consisted of postoperative intraabdominal abscesses, wound infections, pneumonia and urinary tract infections. Cardiovascular (congestive heart failure, pulmonary embolism), postoperative haemorrhage and reintervention, neurological (confusion), renal failure and respiratory complications (pneumothorax and pulmonary embolism) complications were not included in the data analysis, except if associated with sepsis. The definition of the complications has been described in detail elsewhere [17]. Pre- and post-operative data, and post-operative complications were recorded by non-research staff blinded to the patient's allocation group. These were verified, in accordance with predefined criteria, by a member of the research team unaware of study group allocation. This process involved inspection of radiological investigations, laboratory data and clinical assessment.
Statistical analysis
Data in tables are presented as means ± standard deviation (SD) when normally distributed, as medians (interquartile range) when not normally distributed, or as a percentage of the group from which they were derived for categorical data. The chi2 test was used to compare qualitative data. Qualitative and quantitative data were compared using the Student's t-test or analysis of variance (ANOVA) when normally distributed (and variance were equivalent), or the Mann-Whitney U-test or Kruskal-Wallis H test in other circumstances. A multivariate analysis of variance (MANOVA) was used to explore longitudinal data. Multiple logistic regression was employed to identify independent risk factors for postoperative complications. The results of logistic regression are reported as adjusted odds ratios with 95% confidence intervals (CI). The robustness of the model was assessed using a Hosmer-Lemeshow Goodness-of-Fit-Test [31]. Receiver operator characteristic (ROC) curves were constructed to identify optimal cut-off values for outcome associations. The optimal cut-off was defined as the value associated with the highest sum of sensitivity and specificity (Youden's index). Analysis was performed using SEM software [32] and significance was set at P < 0.05.
Results
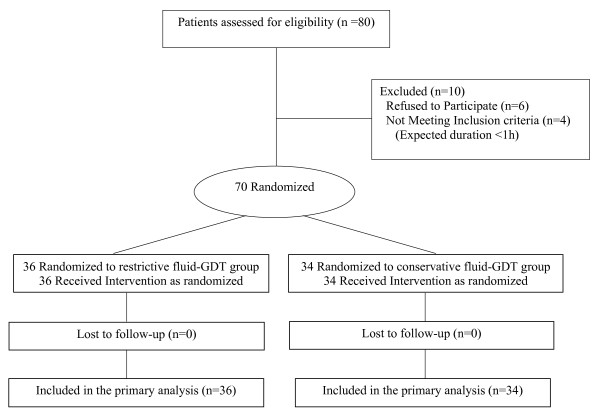
Complete follow-up data were collected from 70 patients included in the original study between May and December 2008 (Figure 1). Thirty patients developed postoperative complications (58% of the R-GDT group and 26% of the C-GDT group, P < 0.01), including 24 who developed at least one of the following: postoperative sepsis (n = 21), intra-abdominal abscess (n = 16), pneumonia (n = 7) and urinary tract infection (n = 4). There were six (8%) who had postoperative acute lung injuries or acute respiratory distress syndrome but none of them was associated with sepsis, and was, therefore, not included in the data analysis. There was no abdominal syndrome. There were two deaths (one in each group, P = 0.50). ScvO2 and P(cv-a)CO2 data were available for all patients. The demographics and commonly measured biological variables for the study participants are shown in Table 1. Surgical procedures consisted of colon/rectum resections (43%), duodenopancreatectomy (20%), gastrectomy (21%) and hepatectomy (16%), and were equally distributed (P = 0.87). There were no differences in operative time and blood loss between the two groups: 248 ± 42 vs. 233 ± 62 min (P = 0.21) and 326 ± 215 vs. 357 ± 373 ml (P = 0.68), respectively, in patients with and without complications. All patients were extubated within two hours after surgery.
Figure 1.
Flow diagram of the original study.
Table 1.
Demographic and biological data at inclusion for patients with and without postoperative complications
| Patients with complications (n = 24) | Patients without complications (n = 46) | P | |
|---|---|---|---|
| Demographic | |||
| Age (years) | 60 ± 13 | 62 ± 13 | 0.61 |
| Sex M/F (%) | 62/38 | 52/48 | 0.41 |
| BMI (kg m-2) | 28 ± 7 | 25 ± 3 | 0.06 |
| P-POSSUM score | 35 ± 6.6 | 33 ± 5.6 | 0.21 |
| ASA score I/II/III | 12/63/25 | 11/72/17 | 0.71 |
| Hypertension (%) | 54 | 50 | 0.74 |
| Cardiac failure (%) | 8 | 9 | 0.95 |
| Ischemic heart disease (%) | 8 | 13 | 0.55 |
| Diabetes mellitus (%) | 17 | 15 | 0.87 |
| COPD (%) | 17 | 13 | 0.68 |
| Neoplasia (%) | 91 | 85 | 0.41 |
| Biological data | |||
| Haemoglobin (g L-1) | 12 ± 2 | 13 ± 2 | 0.12 |
| Haematocrit (%) | 37 ± 5 | 39 ± 4 | 0.14 |
| Albumin (g L-1) | 36 ± 4 | 35 ± 4 | 0.76 |
| Prealbumin (g L-1) | 0.25 ± 0.07 | 0.24 ± 0.06 | 0.48 |
| Creatinine (μmol L-1) | 82 ± 31 | 78 ± 23 | 0.52 |
| Procalcitonin (mg L-1) | 0.07 ± 0.04 | 0.08 ± 0.11 | 0.76 |
| CRP (mg L-1) | 6 ± 7 | 7 ± 16 | 0.74 |
| Lactate (mmol L-1) | 1.4 ± 0.6 | 1.3 ± 0.5 | 0.48 |
Data are presented as means ± SD, or absolute values (%).
Abbreviations: ASA, American Society of Anaesthesiology physical status; BMI, body mass index; COPD, chronic obstructive pulmonary disease; CRP, C-reactive protein; P-POSSUM, Portsmouth Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity.
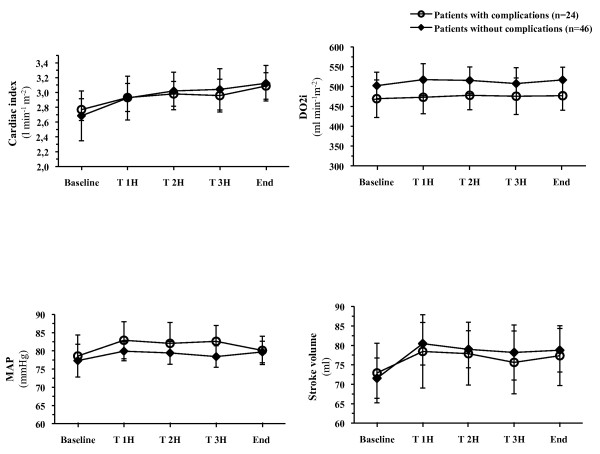
The amounts and types of fluid infused intraoperatively are listed in Table 2. There was no difference in the total volume of fluid infused between groups (P = 0.44), although less crystalloids were administered in patients with complications (P < 0.01). Additional fluid boluses were also significantly higher in these patients (P < 0.01). There was no difference in blood transfusion and in the number of patients who required ephedrine chlorhydrate and dobutamine (Table 2). There were no relevant differences in the principal haemodynamic (Figure 2) and biological variables in patients with and without complications, except for haemoglobin concentration (11.5 ± 1.3 vs. 12.2 ± 1.1 g dL-1, P = 0.04 at the end of surgery) and excess bases (Table 3). There was also no relevant difference regarding serum lactate concentration: (3.1 ± 2.5 vs. 2.3 ± 1.4 mmol L-1, P = 0.16 and 1.7 ± 0.8 vs. 1.6 ± 0.6 mmol L-1, P = 0.59 at PACU admission and at postoperative Day 1, respectively) nor in serum creatinine between patients who did and did not develop postoperative complications.
Table 2.
Intraoperative fluid management in patients with and without postoperative complications
| Patients with complications (n = 24) | Patients without complications (n = 46) | P | |
|---|---|---|---|
| Total volume of fluid infused (mL) | 4,725 (3,600 to 5,300) | 4,525 (3,850 to 6,000) | 0.44 |
| Total volume of crystalloids infused (mL) | 3,255 (2,760 to 4,300) | 4,100 (2,760 to 5,660) | 0.04 |
| Total volume of colloids infused (mL) | 750 (680 to 1,250) | 250 (60 to 500) | < 0.01 |
| Fluid challenge | |||
| No. of challenge per patient | 4 ± 2 | 2 ± 2 | < 0.01 |
| No. (%) of patients who needed | 21 (87) | 34 (74) | 0.19 |
| Blood transfusion, N (%) of patients | 6 (25%) | 7 (15%) | 0.31 |
| Urine output (mL) | |||
| Intraoperative | 600 (390 to 800) | 500 (300 to 975) | 0.46 |
| Day 1 | 1,350 (800 to 1,950) | 2,000 (1,350 to 3,100) | 0.001 |
| Day 2 | 2,000 (1,150 to 2,500) | 2,450 (1,525 to 3,000) | 0.45 |
| Vasoactive support | |||
| Ephedrine chlorhydrate, N (%) of patients | 20 (83%) | 43 (93%) | 0.18 |
| Dobutamine, N (%) of patients | 0 | 1 | NR |
Data are presented as means ± SD, medians (interquartile range) or absolute values (%). NR, not related.
Figure 2.
Cardiac index, oxygen delivery index (DO2i), stroke volume and mean arterial pressure (MAP) in patients who did (n = 24) and did not (n = 46) develop postoperative complications. There was no difference in any variable between groups at any time point. Data are expressed as means ± 95% CI.
Table 3.
Intraoperative biological data
| Patients with complications (n = 24) | Patients without complications (n = 46) | P | |
|---|---|---|---|
| Arterial pH | |||
| Baseline | 7.42 ± 0.03 | 7.43 ± 0.04 | 0.27 |
| T 1H | 7.39 ± 0.04 | 7.41 ± 0.04 | 0.11 |
| T 2H | 7.39 ± 0.04 | 7.40 ± 0.02 | 0.17 |
| T 3H | 7.38 ± 0.05 | 7.39 ± 0.03 | 0.78 |
| End of surgery | 7.37 ± 0.05 | 7.38 ± 0.05 | 0.26 |
| Arterial PO2, mmHg | |||
| Baseline | 186 ± 39 | 195 ± 52 | 0.59 |
| T 1H | 185 ± 43 | 180 ± 41 | 0.56 |
| T 2H | 173 ± 44 | 179 ± 37 | 0.61 |
| T 3H | 172 ± 43 | 178 ± 35 | 0.46 |
| End of surgery | 178 ± 44 | 181 ± 37 | 0.59 |
| Arterial PCO2, mmHg | |||
| Baseline | 36 ± 5 | 36 ± 4 | 0.90 |
| T 1H | 37 ± 4 | 36 ± 3 | 0.41 |
| T 2H | 37 ± 4 | 36 ± 3 | 0.53 |
| T 3H | 36 ± 5 | 36 ± 3 | 0.62 |
| End of surgery | 36 ± 5 | 37 ± 3 | 0.36 |
| BE, mmol L-1 | |||
| Baseline | -1.7 ± 4.3 | -0.5 ± 2.6 | 0.71 |
| T 1H | -3.2 ± 2.7 | -1.1 ± 2.2 | 0.02 |
| T 2H | -2.6 ± 2.9 | -1.5 ± 2.1 | 0.31 |
| T 3H | -2.4 ± 2.8 | -2.4 ± 2.2 | 0.65 |
| End of surgery | -4.0 ± 2.6 | -2.8 ± 2.7 | 0.11 |
| SaO2, % | |||
| Baseline | 98 ± 1.1 | 99 ± 0.8 | 0.03 |
| T 1H | 98 ± 1.0 | 99 ± 0.6 | 0.001 |
| T 2H | 98 ± 1.4 | 98 ± 0.8 | 0.025 |
| T 3H | 98 ± 1.2 | 98 ± 1.0 | 0.16 |
| End of surgery | 98 ± 0.8 | 98 ± 0.7 | 0.21 |
Data are presented as means ± SD.
BE, base excess; SaO2, arterial saturation of oxygen; T, time.
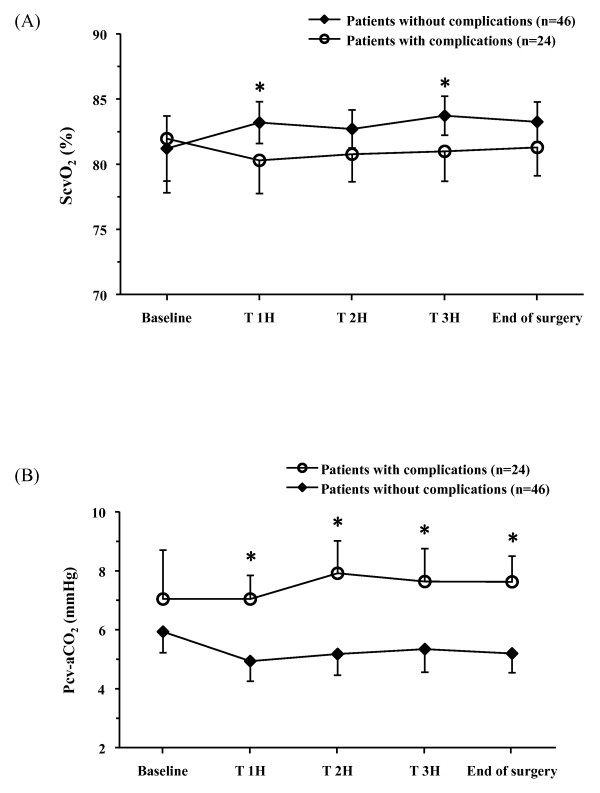
Association with outcome
At baseline there was no difference in ScvO2 values between patients who did and did not develop postoperative complications (82 ± 10 vs. 81 ± 9%, respectively, P = 0.75) (Figure 3a). Compared with uncomplicated patients, mean ScvO2 (78 ± 4 vs. 81 ± 4%, P = 0.017) and minScvO2 (67 ± 6 vs. 72 ± 6%, P = 0.0017) were both lower in patients with complications. Univariate analysis identified four variables associated with postoperative complications: minScvO2 (P = 0.0028), treatment group (C-GDT and R-GDT, P = 0.0067), BMI (P = 0.017) and the need for additional fluid bolus (P = 0.035). Multivariate analysis showed that the need for additional fluid bolus (OR = 1.46 (95% CI: 1.12 to 2), P = 0.005) and minScvO2 < 70% (OR = 4.0 (95% CI: 1.23 to 12.5}, P = 0.019) were independently associated with postoperative complications. The area under the ROC curve for ScvO2 was 0.736 (95 CI%: 0.61 to 0.86) according to the occurrence of postoperative complications. The optimal ScvO2 value was 70.6% (sensitivity 72.9%, specificity 71.4%) for discrimination of patients who did and did not develop complications. Intraoperative characteristics of patients with mean ScvO2 > 71% who did and did not develop postoperative complications are listed in Table 4.
Figure 3.
Trends in ScvO2 (a) and P(cv-a)CO2 (b) in patients who did (n = 24) and did not (n = 46) develop postoperative complications. Data are expressed as means ± 95% CI. * P < 0.05.
Table 4.
Intraoperative haemodynamic data and fluid management in patients with mean ScvO2 > 71%
| Patients with complications (n = 10) | Patients without complications (n = 36) | P | |
|---|---|---|---|
| CI, L min-1 m-2 | |||
| Baseline | 2.9 ± 0.8 | 2.7 ± 0.5 | 0.33 |
| Mean | 3.0 ± 0.7 | 2.9 ± 0.5 | 0.94 |
| End of surgery | 3.2 ± 0.7 | 3.1 ± 0.6 | 0.79 |
| DO2i, mL min-1m-2 | |||
| Baseline | 497 ± 94 | 510 ± 126 | 0.73 |
| Mean | 500 ± 73 | 518 ± 108 | 0.74 |
| End of surgery | 502 ± 74 | 527 ± 113 | 0.65 |
| SV, mL | |||
| Baseline | 75 ± 13 | 74 ± 19 | 0.52 |
| Mean | 79 ± 10 | 78 ± 17 | 0.47 |
| End of surgery | 82 ± 14 | 82 ± 20 | 0.84 |
| MAP, mmHg | |||
| Baseline | 76 ± 14 | 78 ± 17 | 0.93 |
| Mean | 76 ± 8 | 79 ± 11 | 0.81 |
| End of surgery | 75 ± 7 | 79 ± 10 | 0.37 |
| Total volume of fluid Infused | |||
| Crystalloids, mL | 3,375 (2,712 to 4,455) | 4,250 (2,700 to 6,000) | 0.18 |
| Colloids, mL | 5 (500 to 1,188) | 250 (0 to 500) | 0.11 |
| Blood transfusion, N (%) of patients | 2 (20%) | 8 (22%) | 0.63 |
| Vasoactive support | |||
| Ephedrine chlorhydrate, N (%) of patients | 8 (80%) | 34 (94%) | 0.15 |
| Dobutamine, N (%) of patients | 0 | 1 | NR |
Data are presented as means ± SD, median (interquartile range) or absolute values (%).
Abbreviations: CI, cardiac index; DO2i, oxygen delivery index; MAP, mean arterial pressure; NR, not related; ScvO2, central venous oxygen saturation; SV, stroke volume.
Trends in P(cv-a)CO2
At baseline there was no difference in P(cv-a)CO2 values between patients with and without complications (P = 0.22) (Figure 3b). Mean P(cv-a)CO2 was larger in patients who developed complications than in those who did not (7.8 ± 2 vs. 5.6 ± 2 mmHg, P < 10-6). The area under the ROC curve for P(cv-a)CO2 was 0.751 (95% CI: 0.71 to 0.79). The best cut-off P(cv-a)CO2 value was 6 mmHg (sensitivity 79%, specificity 66%, positive predictive value 56%, negative predictive value 85%) for discrimination of patients who did and did not develop complications. When we considered P(cv-a)CO2 with overall complications (not only those associated with sepsis) in all of the 30 patients, the difference between patients who did and did not develop complications still remained significant. We constructed the ROC curve and found that a P(cv-a)CO2 of 6 mmHg predicted the occurrence of complications with 75% sensitivity, 50% specificity, predictive positive value of 0.13 and predictive negative value of 0.95 (AUC 0.648, 95% CI 0.58 to 0.72).
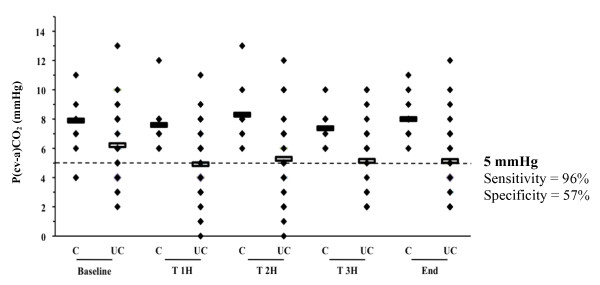
In patients with ScvO2≥71%, mean P(cv-a)CO2 was larger in patients who developed postoperative complications than in patients with ScvO2≥71% who did not (7.7 ± 2 vs. 5 ± 2 mmHg, respectively, P < 10-6). The area under the ROC curve for P(cv-a)CO2 was 0.785 (95% CI: 0.74 to 0.83) with 5 mmHg as the best threshold value (sensitivity 96%, specificity 54%, positive predictive value 41%, negative predictive value 98%) for discrimination of patients with ScvO2 ≥71% who did and did not develop postoperative complications (Figure 4).
Figure 4.
Individual values of P(cv-a)CO2 according to the occurrence of postoperative complications in patients with ScvO2 ≥71%. Abbreviations: C, patients with complications; UC, patients without complications.
Discussion
Recently published data clearly demonstrate that low ScvO2 during major abdominal surgery is associated with an increased risk of postoperative complications [13-15]. In this study, using Doppler-derived deltaPV as a goal-directed approach, it was observed that high ScvO2 (≥71%) did not necessarily preclude postoperative complications. In this context, the presence of a P(cv-a)CO2 value > 5 mmHg may be a useful complementary tool to identify patients with ScvO2≥71% who might remain insufficiently optimized haemodynamically.
There is growing evidence that individualized fluid loading through goal-directed protocols, titrated by dynamic indices of either flow or preload, improves patient outcome, and is superior to the assessment of standard haemodynamic parameters such as mean arterial pressure (MAP), heart rate or central venous pressure, to prevent inadequate or excessive fluid administration [4,9,33,34]. Although the underlying mechanisms remain controversial, most goal-directed therapy (GDT) protocols include fluid loading, alone or combined with inotropes, to prevent O2 debt by maintaining tissue perfusion [3]. In our recently published randomized study of patients treated with an individualized oesophageal Doppler-guided fluid substitution protocol, we found that crystalloid restriction (6 vs. 12 mL kg-1h-1) was associated with increased postoperative complications [17]. Interestingly, the results also indicated that individualized optimization of preload by colloid loading might not have been sufficient to promote optimal tissue perfusion and oxygenation, as indicated by reduced ScvO2 values (69 ± 6 vs. 72 ± 6 mmHg, P = 0.04) in the restricted-GDT group of patients [17].
Although the prognostic significance of reduced ScvO2 and the benefit of its normalization in early goal-directed protocols have been proposed [13,19,35], both normal and high ScvO2 values do not preclude microcirculatory failure [19]. In this context, in patients treated with an early GDT-based sepsis resuscitation protocol, Jones and colleagues [36] and Vallee and colleagues [20] showed that either lactate clearance or P(cv-a)CO2 might be useful to identify persistent tissue hypoperfusion when the ScvO2 goal has been reached with apparent normal DO2/VO2 ratio. It was also observed that, in surgical patients, an individualized preload-targeted fluid loading to maintain tissue perfusion was not sufficient to prevent significant differences in outcome [17]. Interestingly, mean P(cv-a)CO2 was larger in patients with complications with a "normalized" DO2/VO2 ratio (ScvO2 ≥71%), than in patients without complications, with 5 mmHg as the best threshold value. According to ScvO2, CI and DO2i values, enlarged P(cv-a)CO2 could be explained by a certainly small but persistent tissue hypoperfusion degree in patients who go on to develop postoperative complications. The increase in venous PCO2 would reflect a state of insufficient flow relative to CO2 production [37]. This condition has been demonstrated previously [22,38]. Indeed, Vallet and colleagues [22] evidenced that the venous-to-arterial CO2 gap (PCO2 gap) increased during low blood flow-induced tissue hypoxia (ischemic hypoxia) while it remained unchanged during hypoxemia-induced hypoxia (hypoxic hypoxia).
These results are in agreement with those of Bakker and colleagues [24] who showed that, in patients with septic shock, the PCO2 gap was smaller in survivors than in non-survivors, despite quite similar CI, DO2 and VO2 values. In septic shock patients, characterized by an increased PCO2 gap and a low flow state, fluid challenge was found to lower the PCO2 gap while increasing cardiac output [39]. In contrast, no significant changes in cardiac output and PCO2 gap were found in patients with normal PCO2, thus confirming the relationship between an increased PCO2 gap and insufficient flow [39]. According to our P(cv-a)CO2 values and the associated trends in both lactate and base excess concentrations (Tables 3 and 4), it can be speculated that, despite an optimized preload with fluid challenge, patients with ScvO2 values ≥71% who developed complications might have had a relatively insufficient flow state and might have benefited from an increased CI as suggested by the study of Donati [13]. Previous reports have shown that, under conditions where O2 demand exceeds O2 consumption (VO2), ScvO2 (and O2 extraction) does not accurately reflect the O2demand/DO2 relationship [40]. According to the modified Fick equation applied to CO2, PCO2 gap is linearly related to CO2 production (VCO2) and inversely related to CI [23]. Considering the respiratory quotient (VCO2/VO2 ratio), VCO2 is directly related to O2 consumption (VO2) [23]. Under conditions of adapted cardiac output to VO2, even if the CO2 produced is higher than normal because of an additional anaerobic CO2 production, in the presence of sufficient flow to wash out the CO2 produced by the tissues, the PCO2 gap should not be increased [22]. Conversely, low blood flow can result in a widening of the PCO2 gap even if no additional CO2production occurs because of a CO2 stagnation phenomenon [38,41]. The association of these situations may explain, in the current study, the combination of "normal" ScvO2 values and increased P(cv-a)CO2 values. It can be argued that, despite an apparently normal CI during the entire surgical procedure, this condition could relate to a relatively insufficient flow state, and could be associated with an increased O2 demand and hence increased CO2 production. Whether increasing in the CI may be beneficial in this situation remains to be evaluated.
These findings may be difficult to generalize because the study has several limitations. First, we are aware that the number of patients included was relatively small which could limit the external validity of the study, and that complementary data are needed to confirm the results. Nevertheless, when we considered that at least one measurement of P(cv-a)CO2 > 5 mmHg would represent a risk factor associated with the occurrence of postoperative complications, we found a post-hoc power of 52%. Furthermore, when we considered the number of episodes of P(cv-a)CO2, we found that more than or equal to three episodes of P(cv-a)CO2 > 5 mmHg was associated with a 20% risk of postoperative complications (with a post-hoc power calculation > 90%). Second, while the threshold ScvO2 value is very similar to that described previously in a comparable surgical population, the optimal threshold P(cv-a)CO2 value of 5 mmHg in line with a 71% ScvO2 goal might be subject to criticism. It might be considered that a higher ScvO2 (that is, ≥73%) would represent a more appropriate target value [40]. Third, potential confounders such as hypothermia, which may decrease cellular respiration and, therefore, CO2 generation [21], might have affected the results. Nevertheless, during the entire surgical procedure, special attention was taken to maintain normothermia. In addition, except for fluid therapy, intraoperative management was similar in the two groups of patients. Although there was a significant difference in the volume of fluids infused, this was not associated with postoperative complications with logistic regression (P = 0.16 and P = 0.49 for crystalloids and colloids, respectively). Even after adjustment P(cv-a)CO2 > 5 mmHg still remains associated with the occurrence of postoperative complications (P < 0.001). Fourth, the use of central venous-to-arterial PCO2 difference as a surrogate for mixed venous PCO2 gap might be a further limitation. Nevertheless, it has recently been found that central venous PCO2, obtained from a simple central blood sample instead of a pulmonary arterial blood sample, is a valuable alternative to PvCO2 and that correlation with CI still exists in this context [21]. In addition, measurement of P(cv-a)CO2 instead of P(v-a)CO2 may be more convenient in a surgical context.
Conclusions
There is strong support today for the use of individualized goal-directed fluid substitution during high-risk surgery. Although ScvO2 reflects important changes in the O2 delivery/consumption relationship, it is speculated that P(cv-a)CO2 might reinforce the value of ScvO2 to identify insufficient flow and tissue hypoperfusion during high-risk surgery. In this context, P(cv-a)CO2 could be a useful complementary tool to ScvO2 to identify patients who remain inadequately managed when the optimization goal has been reached by volume loading during a GDT protocol. Future research is needed to validate this finding.
Key messages
• Early detection and correction of tissue hypoperfusion were shown to improve outcome during high-risk surgery.
• Central venous-to-arterial CO2 difference might serve as a complementary tool to ScvO2 to identify insufficient flow when individualized optimization of intravascular status has been reached with fluid loading.
• Larger randomized trials are now required to confirm the benefit of this approach.
Abbreviations
ASA: American Society of Anaesthesiology; CI: cardiac index; CRP: C-reactive protein; DeltaPV, respiratory variation in peak aortic flow velocity; DO2: oxygen delivery; DO2i: oxygen delivery index; GDT: goal-directed therapy; MAP: mean arterial pressure; PACU: post-acute care unit; PCT: procalcitonin; P(cv-a)CO2: central venous-to-arterial carbon dioxide difference; P-Possum: Portsmouth Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity; PRBCs: packed red blood cells; P(v-a)CO2: mixed venous-to-arterial carbon dioxide difference; ROC: receiver operating characteristic; ScvO2: central venous oxygen saturation; SV: stroke volume; SvO2: mixed venous oxygen saturation; VO2: oxygen consumption.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EF and JMC conceived and designed the original study. BV suggested complementary analysis (assessment of P(cv-a)CO2). MJ and RG were responsible for patient enrolment and participated in data acquisition. EF, ER, BV and JEB drafted the manuscript. All authors read and approved the final manuscript.
Contributor Information
Emmanuel Futier, Email: efutier@chu-clermontferrand.fr.
Emmanuel Robin, Email: emmanuel.robin@chru-lille.fr.
Matthieu Jabaudon, Email: mjabaudon@chu-clermontferrand.fr.
Renaud Guerin, Email: rguerin@chu-clermontferrand.fr.
Antoine Petit, Email: apetit@chu-clermontferrand.fr.
Jean-Etienne Bazin, Email: jebazin@chu-clermontferrand.fr.
Jean-Michel Constantin, Email: jmconstantin@chu-clermontferrand.fr.
Benoit Vallet, Email: benoit.vallet@chru-lille.fr.
Acknowledgements
The authors thank Fabrice Kwiatkowski who performed the statistical data analysis and Laurence Roszyk for biochemical data analysis.
This study was supported by the University Hospital of Clermont-Ferrand (Clermont-Ferrand, France). The sponsor of the study had no role in the study design, data collection, data analysis, interpretation of data or writing of this report.
References
- Shoemaker WC, Appel PL, Kram HB. Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest. 1992;102:208–215. doi: 10.1378/chest.102.1.208. [DOI] [PubMed] [Google Scholar]
- Mythen MG, Webb AR. The role of gut mucosal hypoperfusion in the pathogenesis of post-operative organ dysfunction. Intensive Care Med. 1994;20:203–209. doi: 10.1007/BF01704701. [DOI] [PubMed] [Google Scholar]
- Lees N, Hamilton M, Rhodes A. Clinical review: Goal-directed therapy in high risk surgical patients. Crit Care. 2009;13:231. doi: 10.1186/cc8039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giglio MT, Marucci M, Testini M, Brienza N. Goal-directed haemodynamic therapy and gastrointestinal complications in major surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2009;103:637–646. doi: 10.1093/bja/aep279. [DOI] [PubMed] [Google Scholar]
- Bundgaard-Nielsen M, Holte K, Secher NH, Kehlet H. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand. 2007;51:331–340. doi: 10.1111/j.1399-6576.2006.01221.x. [DOI] [PubMed] [Google Scholar]
- Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial (ISRCTN38797445) Crit Care. 2005;9:R687–693. doi: 10.1186/cc3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan TJ, Soppitt A, Maroof M, el-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PS. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 2002;97:820–826. doi: 10.1097/00000542-200210000-00012. [DOI] [PubMed] [Google Scholar]
- Noblett SE, Snowden CP, Shenton BK, Horgan AF. Randomized clinical trial assessing the effect of Doppler-optimized fluid management on outcome after elective colorectal resection. Br J Surg. 2006;93:1069–1076. doi: 10.1002/bjs.5454. [DOI] [PubMed] [Google Scholar]
- Lopes MR, Oliveira MA, Pereira VO, Lemos IP, Auler JO Jr, Michard F. Goal-directed fluid management based on pulse pressure variation monitoring during high-risk surgery: a pilot randomized controlled trial. Crit Care. 2007;11:R100. doi: 10.1186/cc6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mythen MG, Webb AR. Perioperative plasma volume expansion reduces the incidence of gut mucosal hypoperfusion during cardiac surgery. Arch Surg. 1995;130:423–429. doi: 10.1001/archsurg.1995.01430040085019. [DOI] [PubMed] [Google Scholar]
- Marjanovic G, Villain C, Juettner E, zur Hausen A, Hoeppner J, Hopt UT, Drognitz O, Obermaier R. Impact of different crystalloid volume regimes on intestinal anastomotic stability. Ann Surg. 2009;249:181–185. doi: 10.1097/SLA.0b013e31818b73dc. [DOI] [PubMed] [Google Scholar]
- Kimberger O, Arnberger M, Brandt S, Plock J, Sigurdsson GH, Kurz A, Hiltebrand L. Goal-directed colloid administration improves the microcirculation of healthy and perianastomotic colon. Anesthesiology. 2009;110:496–504. doi: 10.1097/ALN.0b013e31819841f6. [DOI] [PubMed] [Google Scholar]
- Donati A, Loggi S, Preiser JC, Orsetti G, Munch C, Gabbanelli V, Pelaia P, Pietropaoli P. Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk surgical patients. Chest. 2007;132:1817–1824. doi: 10.1378/chest.07-0621. [DOI] [PubMed] [Google Scholar]
- Collaborative Study Group on Perioperative ScvO2 Monitoring. Multicentre study on peri- and postoperative central venous oxygen saturation in high-risk surgical patients. Crit Care. 2006;10:R158. doi: 10.1186/cc5094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Changes in central venous saturation after major surgery, and association with outcome. Crit Care. 2005;9:R694–699. doi: 10.1186/cc3888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhart K, Rudolph T, Bredle DL, Hannemann L, Cain SM. Comparison of central-venous to mixed-venous oxygen saturation during changes in oxygen supply/demand. Chest. 1989;95:1216–1221. doi: 10.1378/chest.95.6.1216. [DOI] [PubMed] [Google Scholar]
- Futier E, Constantin JM, Petit A, Chanques G, Kwiatkowski F, Flamein R, Slim K, Sapin V, Jaber S, Bazin JE. Conservative versus restrictive individualized goal-directed fluid administration in major abdominal surgery: a prospective randomized trial. Arch Surg. 2010. in press . [DOI] [PubMed]
- Pearse RM, Hinds CJ. Should we use central venous saturation to guide management in high-risk surgical patients? Crit Care. 2006;10:181. doi: 10.1186/cc5122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope JV, Jones AE, Gaieski DF, Arnold RC, Trzeciak S, Shapiro NI. Multicenter study of central venous oxygen saturation (ScvO(2)) as a predictor of mortality in patients with sepsis. Ann Emerg Med. 2010;55:40.e1–46.e1. doi: 10.1016/j.annemergmed.2009.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallee F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, Samii K, Fourcade O, Genestal M. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med. 2008;34:2218–2225. doi: 10.1007/s00134-008-1199-0. [DOI] [PubMed] [Google Scholar]
- Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB, Pamukov N, Horst HM. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med. 2005;31:818–822. doi: 10.1007/s00134-005-2602-8. [DOI] [PubMed] [Google Scholar]
- Vallet B, Teboul JL, Cain S, Curtis S. Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J Appl Physiol. 2000;89:1317–1321. doi: 10.1152/jappl.2000.89.4.1317. [DOI] [PubMed] [Google Scholar]
- Lamia B, Monnet X, Teboul JL. Meaning of arterio-venous PCO2 difference in circulatory shock. Minerva Anestesiol. 2006;72:597–604. [PubMed] [Google Scholar]
- Bakker J, Vincent JL, Gris P, Leon M, Coffernils M, Kahn RJ. Veno-arterial carbon dioxide gradient in human septic shock. Chest. 1992;101:509–515. doi: 10.1378/chest.101.2.509. [DOI] [PubMed] [Google Scholar]
- Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- Rahbari NN, Zimmermann JB, Schmidt T, Koch M, Weigand MA, Weitz J. Meta-analysis of standard, restrictive and supplemental fluid administration in colorectal surgery. Br J Surg. 2009;96:331–341. doi: 10.1002/bjs.6552. [DOI] [PubMed] [Google Scholar]
- Slama M, Masson H, Teboul JL, Arnould ML, Nait-Kaoudjt R, Colas B, Peltier M, Tribouilloy C, Susic D, Frohlich E, Andrejak M. Monitoring of respiratory variations of aortic blood flow velocity using esophageal Doppler. Intensive Care Med. 2004;30:1182–1187. doi: 10.1007/s00134-004-2190-z. [DOI] [PubMed] [Google Scholar]
- Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, Teboul JL. Esophageal Doppler monitoring predicts fluid responsiveness in critically ill ventilated patients. Intensive Care Med. 2005;31:1195–1201. doi: 10.1007/s00134-005-2731-0. [DOI] [PubMed] [Google Scholar]
- Bennett-Guerrero E, Welsby I, Dunn TJ, Young LR, Wahl TA, Diers TL, Phillips-Bute BG, Newman MF, Mythen MG. The use of a postoperative morbidity survey to evaluate patients with prolonged hospitalization after routine, moderate-risk, elective surgery. Anesth Analg. 1999;89:514–519. doi: 10.1097/00000539-199908000-00050. [DOI] [PubMed] [Google Scholar]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16:965–980. doi: 10.1002/(SICI)1097-0258(19970515)16:9<965::AID-SIM509>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Kwiatkowski F, Girard M, Hacene K, Berlie J. Sem: a suitable statistical software adaptated for research in oncology. Bull Cancer. 2000;87:715–721. [PubMed] [Google Scholar]
- Grocott MP, Mythen MG, Gan TJ. Perioperative fluid management and clinical outcomes in adults. Anesth Analg. 2005;100:1093–1106. doi: 10.1213/01.ANE.0000148691.33690.AC. [DOI] [PubMed] [Google Scholar]
- Chappell D, Jacob M, Hofmann-Kiefer K, Conzen P, Rehm M. A rational approach to perioperative fluid management. Anesthesiology. 2008;109:723–740. doi: 10.1097/ALN.0b013e3181863117. [DOI] [PubMed] [Google Scholar]
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739–746. doi: 10.1001/jama.2010.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeneveld AB. Interpreting the venous-arterial PCO2 difference. Crit Care Med. 1998;26:979–980. doi: 10.1097/00003246-199806000-00002. [DOI] [PubMed] [Google Scholar]
- Neviere R, Chagnon JL, Teboul JL, Vallet B, Wattel F. Small intestine intramucosal PCO(2) and microvascular blood flow during hypoxic and ischemic hypoxia. Crit Care Med. 2002;30:379–384. doi: 10.1097/00003246-200202000-00019. [DOI] [PubMed] [Google Scholar]
- Mecher CE, Rackow EC, Astiz ME, Weil MH. Venous hypercarbia associated with severe sepsis and systemic hypoperfusion. Crit Care Med. 1990;18:585–589. doi: 10.1097/00003246-199006000-00001. [DOI] [PubMed] [Google Scholar]
- Shepherd SJ, Pearse RM. Role of central and mixed venous oxygen saturation measurement in perioperative care. Anesthesiology. 2009;111:649–656. doi: 10.1097/ALN.0b013e3181af59aa. [DOI] [PubMed] [Google Scholar]
- Mekontso-Dessap A, Castelain V, Anguel N, Bahloul M, Schauvliege F, Richard C, Teboul JL. Combination of venoarterial PCO2 difference with arteriovenous O2 content difference to detect anaerobic metabolism in patients. Intensive Care Med. 2002;28:272–277. doi: 10.1007/s00134-002-1215-8. [DOI] [PubMed] [Google Scholar]