Abstract
To assess the feasibility of a pediatric primary care based intervention to promote healthful behaviors among 0–6 month old infants and their mothers. We enrolled two intervention practices (60 mother-infant pairs) and one usual care control practice (24 pairs) in a non-randomized controlled trial. We completed visits and interviews with 80 (95%) pairs at birth and 6 months. The intervention included (1) brief focused negotiation by pediatricians, (2) motivational counseling by a health educator, and (3) group parenting workshops. We evaluated the intervention effects on infant feeding, sleep duration, TV viewing, and mothers’ responsiveness to satiety cues. Maternal behavioral targets included postpartum diet, physical activity, TV and sleep. At 6 months, fewer intervention than control infants had been introduced to solid foods (57% vs. 82%; P = 0.04), and intervention infants viewed less TV (mean 1.2 vs. 1.5 h/d; P = 0.07). Compared to control infants, intervention infants had larger increases in their nocturnal sleep duration from baseline to follow up (mean increase 1.9 vs. 1.3 h/d; P = 0.05); larger reductions in settling time (mean reduction −0.70 vs. −0.10 h/d; P = 0.02); and larger reductions in hours/day of nighttime wakefulness (mean reduction −2.9 vs. −1.5 h/d; P = 0.08). There were no differences in breastfeeding, response to satiety cues, or maternal health behaviors. A program of brief focused negotiation by pediatricians, individual coaching by health educators using motivational interviewing, and group parenting workshops tended to improve infant feeding, sleep and media exposure, but had less impact on mothers’ own health-related behaviors.
Keywords: Postpartum women, Infancy, Nutrition, Physical activity, Obesity prevention
Background
Rates of overweight are high, even among infants, [1] with a nationwide prevalence of 10% among infants 0–23 months old [2]. Infants with rapid growth during the first 2 years of life appear more likely to develop obesity in childhood or adulthood [3, 4]. Excess weight gain during infancy has also been associated with higher blood pressure and asthma-related symptoms later in childhood [5]. Few interventions have focused on preventing excess infant weight gain [6].
The postpartum period also represents a critical window for susceptibility to excess weight gain among women. Compared with weight gain during other periods of life, excess maternal weight retained after giving birth appears to be particularly harmful because it is deposited preferentially in central rather than peripheral sites increasing the risk of cardiovascular disease [7, 8]. Previous studies indicate that a large subset of women have substantial weight retention [9] but few interventions have been conducted to improve nutrition and physical activity behaviors in the postpartum period to prevent substantial weight retention.
The pediatric primary care team is uniquely positioned to provide effective interventions to promote healthful nutrition and physical activity behaviors in both mothers and their children. Pediatric well child visits occur more frequently in the first months after birth than at any other time during the lifecourse; the continuity of the relationship between pediatricians and families promotes receptivity to suggestions for changes in health related behaviors; and evidence suggests that pediatrician advice is a strong predictor of maternal health behavior change including prolonged breastfeeding [10–13]. Thus, clinically-based interventions in the postpartum period are particularly likely to be of benefit.
The goal of the proposed study was to develop and test the feasibility of a pediatric, primary care based intervention among 0–6-month-old infants and their mothers to encourage healthful eating and physical activity behaviors in both.
Methods
Overview of Study Design
We enrolled two intervention pediatric primary care practices (60 mother-infant pairs) and one usual care control practice (24 pairs) in a non-randomized controlled trial in the Boston area. The three practices were part of Harvard Vanguard Medical Associates (HVMA), a multi-site group practice caring for a demographically diverse population in Massachusetts. The intervention was 6 months in duration and had dual primary outcomes for mothers and infants.
Participants and Recruitment
Participants included mother-infant pairs who received their pediatric care at the 3 primary care offices, between January and June 2008. All infants aged 0–1 month old with a mother who could respond to interviews and questionnaires in English were considered eligible for this study. We excluded (1) any infant whose mother would not be able to follow study procedures for 6 months, (2) families who planned to leave HVMA within the study time frame, and (3) infants or mothers with severe health conditions. Based on daily reports of newborns at each of the three practices, we identified a total of 160 mother-infant pairs who might be eligible for the intervention. We mailed a letter to each mother introducing the study and encouraging participation. The letter included an opt-out telephone number to call if the family did not want to participate. We telephoned those mothers who did not refuse additional contact within 5 days of mailing the letter. We met mother-infant pairs at their first pediatric primary care visit (~ 10 days after birth) to get written informed consent and perform anthropometric measures. Of the 157 mother-infant pairs who we attempted to contact, we completed a baseline telephone interview and in-person visit with 84 pairs.
Following completion of baseline assessments, participants were informed if they would be receiving regular well child care visits (usual care) or well child care visits plus individualized coaching (intervention). At 6-months postpartum, mothers again completed a telephone interview, and at their child’s 6-month pediatric appointment, we again collected anthropometric measures. We offered participants $25 for completing each of the two assessments. All study procedures were approved by the human subjects committee of Harvard Pilgrim Health Care.
Treatment Groups
Usual Care
Mother-infant pairs in the usual care practices received standard of care offered by their pediatric primary care providers. In both groups this included routine well child care visits and routine anticipatory guidance at 2 weeks, 1 month, 2, 4, and 6 months of age.
Intervention
The 6-month, multifaceted intervention consisted of brief focused negotiation by pediatric primary care providers during five routine well child care visits, four individualized coaching and motivational counseling telephone calls with a study health educator, invitation to four group parenting skills training workshops, and comprehensive educational materials.
We trained the pediatric primary care providers in the intervention practices to use brief focused negotiation skills [14] at all routine clinical visits to endorse mother-infant behavior change. Brief focused negotiation is based on the concepts of motivational interviewing (MI) but tailored for brief sessions such as the clinical encounter. We also trained pediatric providers on the epidemiology and health consequences of excess weight gain in mothers and infants.
We trained one health educator to conduct telephone calls with the mothers at 3 weeks, 6 weeks, 3 and 5 months postpartum. The call intervals were scheduled to occur between infant well-child visits. Calls were intended to be approximately 15–20 min in duration. Calls addressed 4 recommendations for mothers (healthful eating, physical activity, sleep, TV) and five recommendations for infants (breastfeeding exclusivity/duration, delayed introduction of solid foods, increased sleep duration and quality, TV avoidance, responsiveness to satiety cues). The health educator used MI techniques during the study calls. MI is a communication technique that enhances self-efficacy, increases recognition of inconsistencies between actual and desired behaviors, teaches skills for reduction of this dissonance, and enhances motivation for change [15–17]. Components include encouraging mothers to clarify and resolve ambivalence about behavior change, and setting goals to initiate the change process [15, 17].
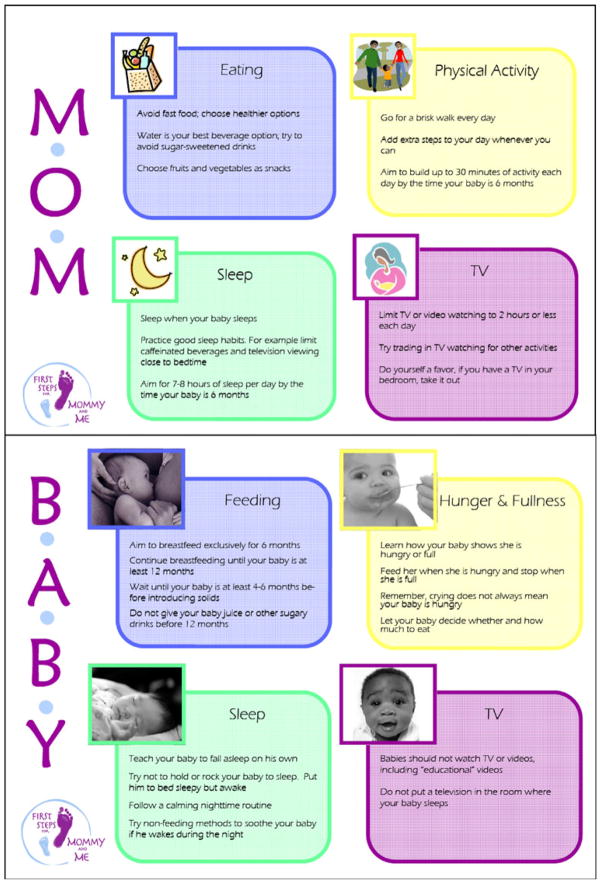
We designed printed materials, including posters and handouts to highlight the targeted behaviors (Fig. 1). These materials served as aids to discussion between the primary care provider or health educator and the mother. To the extent possible, materials were tailored not only to the infant’s developmental stage and mother’s baseline level of behaviors, but also took into account other factors such as neighborhood resources.
Fig. 1.
Sample intervention materials in the First Steps for Mommy and Me study
We also conducted monthly parenting skills training sessions, led by pediatric providers and the study health educator to review general parenting skills, promote peer support, and allow for social networking. The groups provided an opportunity for behavioral skills training, building a community of participants, and giving participants information about community resources.
Outcome Measures
Table 1 shows the behavioral targets, goals for intervention mother-infant pairs, and measures used in the First Steps for Mommy and Me Intervention. On the 6-month questionnaire, we assessed mothers’ dietary intake using a brief food frequency questionnaire [18]. We assessed fast food intake using a question adapted from those used in cohorts of adolescents [19] and adults [20]. We measured intake of sugar-sweetened beverages using validated questions associated with adult BMI [21]. We assessed TV viewing by asking mothers to report the average weekly hours they spend watching television or videos using previously validated questions [22]. To measure sleep duration at baseline and at 6 months, we asked mothers to report their hours of sleep in a 24-h period using a question which we previously related to maternal postpartum weight retention [23]. We also assessed maternal physical activity using a standard questionnaire [24].
Table 1.
Behavioral targets, goals for mother-infant pairs, and measures used in the First Steps for Mommy and Me intervention
| Behavioral targets | Mothers’ goals at 6 months | Measures and validity relationships |
|---|---|---|
| Healthful diet | ||
| Fruits and vegetables | Higher daily intake of fruits and vegetables | PrimeScreen [18]. Reproducible and comparable to estimates of intake from a validated full-length food frequency questionnaire [18] |
| Fast food | Lower weekly intake of fast food meals | Modified question adapted from the growing up today study [19] and CARDIA [20]; both associated with BMI |
| Sugar-sweetened beverages | Lower weekly intake of beverages with sugar added | Validated questions associated with adult BMI [21] |
| Television viewing | Lower TV/video viewing in a 24-h period | Average daily hours spent watching TV or videos; related to postpartum weight retention [22] |
| Sleep duration | Increased sleep duration in a 24-h period compared to baseline | Average hours of sleep in a 24-h period; related to postpartum weight retention [23] |
| Physical activity | Higher total daily physical activity (including walking) | Average weekly hours spent in three classes of recreational activity; walking, moderate activities, and vigorous activities [24] |
|
| ||
| Mother-infant goals at 6 months | Measures and validity relationships | |
|
| ||
| Infant feeding | ||
| Breastfeeding | Prolonged duration and exclusive breastfeeding | Questionnaire items on duration and exclusivity; related to child BMI [37] |
| Introduction of solid foods | Delayed introduction of solid foods to 4–6 months | Questionnaire items on timing of introduction of solids; related to increased infant weight gain [38, 39] |
| Feeding behaviors | Higher responsiveness to satiety; less feeding to soothe | Infant feeding questionnaire; [25] and infant feeding style questionnaire inversely related to weight-for-length among 3–20 month old infants [26] |
| Television viewing | Lower TV/video viewing in a 24-h period | Average daily hours spent watching TV or videos; related to BMI [40–42] and body fat [43] and poorer diet quality in children [44] |
| TV in bedroom | No TV in bedroom | Presence of TV in bedroom; related to BMI [45, 46] in children |
| Infant sleep | Increased nocturnal sleep duration; decreased daytime sleep duration, settling time, night awakenings, and nocturnal wakefulness compared to baseline | Brief infant sleep questionnaire (BISQ); [27] related to infant weight-for-length [47] and child BMI [48] |
At baseline, we asked mothers if they had initiated breastfeeding. At 6 months, we asked mothers if they were exclusively breastfeeding, mixed breast and formula feeding, or formula-feeding only. If they had stopped breast-feeding, we asked them the children’s age at cessation. At 6 months, we measured timing of introduction of solids (<4 months, 4–5 months and ≥6 months). We derived a continuous “responsiveness to infant satiety” score from 4 questions of the Infant Feeding Questionnaire developed by Birch et al. [25]. Mother’s reported using 4-point Likert-type scales ranging from strongly agree to strongly disagree. The score ranged from 4 to 16, with higher scores indicating a higher level of maternal responsiveness to her infant’s satiety cues. Internal reliability of the 4 items, measured by standardized Cronbach alpha, was acceptable (α = 0.70). We used one question from the validated Infant Feeding Style Questionnaire to measure maternal “feeding-to-soothe” practices [26]. At 6 months we asked mothers to report the number of hours their infants watched TV/videos on an average weekday and weekend day in the past month. We also asked mothers if their infant had a TV in the room where they slept. At baseline and at 6 months, mothers completed the Brief Infant Sleep Questionnaire (BISQ) [27] that assessed nocturnal sleep duration, daytime sleep duration, settling time, night awakenings, and nocturnal wakefulness.
Secondary Anthropometric Outcomes
At the baseline and follow up visits, a research assistant measured infants’ length using a recumbent Shorr board and mothers’ height using a stadiometer. We measured infant weight using a Seca infant scale and mothers’ weight using an electronic scale. We calculated infant weight-for-length z-score based on CDC references [28]. We calculated mother’s BMI as kg/m2 and defined postpartum weight retention as the difference between measured weight at 6 months after delivery and self-reported pre-pregnancy weight.
Other Measures
At baseline, we assessed several covariates including mothers’ age, race/ethnicity, education level, marital status, type of delivery, household income, and infant gender and birth weight. In addition, we asked mothers to report their pre-pregnancy weight as well as their gestational weight gain. We assessed maternal postpartum depression at baseline with the Edinburgh Postpartum Depression Scale (EPDS) and dichotomized scores ≥13 as depression or <13 no depression [29].
Process Measures
To understand more fully why the intervention worked (or did not work), we asked mothers in the intervention group to report on their satisfaction with the intervention components and to rate how helpful each component was in guiding their approach to their own and their infants’ behaviors. We also sent a brief survey at the end of the study to the 11 pediatricians who practiced at the two intervention practices to assess feasibility and acceptability of the intervention.
Statistical Methods
We performed univariate analyses of variables of interest to test for baseline differences, outliers, and distributional assumptions. We used analysis of variance and non-parametric tests as necessary, to test for group differences in each of the study outcomes. We performed all analyses using SAS version 9.1 (SAS Institute, Cary, NC).
Results
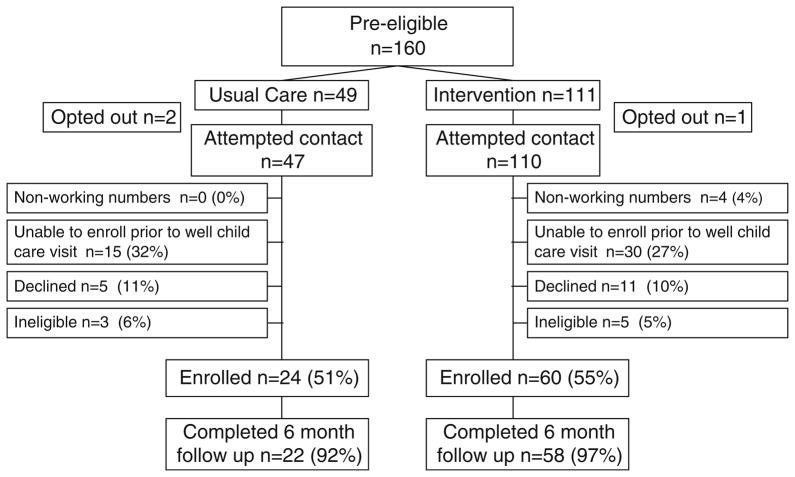
Figure 2 shows the study participant flow. We enrolled 84 mother-infant pairs; 60 in the intervention practices and 24 in the usual care practice. A total of 80 participants (95% of those enrolled at baseline) completed the 6-month follow-up assessments. Baseline characteristics of study participants are shown in Table 2. The mean (SD) age of mothers in this study was 32.9 (4.6) years and 61% were primiparous. Mean (SD) infant birth weight was 3.42 (0.44) kg.
Fig. 2.
Diagram of participant flow of the First Steps for Mommy and Me study
Table 2.
Baseline characteristics of 80 mother-infant pairs in the First Steps for Mommy and Me intervention, overall and by study arm
| Characteristics | Overall N = 80 | Intervention N = 58 | Usual care N = 22 | P-value* |
|---|---|---|---|---|
| % or Mean (SD) | ||||
| Maternal, paternal, and household | ||||
| Maternal age, years | 32.9 (4.6) | 32.7 (4.6) | 33.4 (4.9) | 0.51 |
| Maternal pre-pregnancy BMI, kg/m2 | 23.5 (5.0) | 23.1 (4.6) | 24.4 (5.8) | 0.24 |
| Paternal pre-pregnancy BMI, kg/m2 | 25.5 (3.9) | 25.0 (3.6) | 26.8 (4.4) | 0.09 |
| Maternal gestational weight gain, kg | 14.9 (7.6) | 15.3 (8.3) | 13.8 (5.7) | 0.90 |
| Maternal race/ethnicity, white | 74% | 71% | 79% | 0.46 |
| Education, college graduate | 93% | 92% | 96% | 0.67 |
| Marital status, married/cohabiting | 95% | 93% | 100% | 0.30 |
| Household income | ||||
| ≤$70,000 | 38% | 38% | 38% | 1.00 |
| ≥$70,001 | 62% | 62% | 62% | |
| Parity, primiparous | 61% | 63% | 54% | 0.47 |
| Type of delivery | ||||
| Vaginal | 71% | 73% | 67% | 0.60 |
| Cesarean | 29% | 27% | 33% | |
| Postpartum depression (EPDS ≥ 13)a | 3.1% | 3.4% | 2.4% | 0.91 |
| Initiated breastfeeding | 99% | 98% | 100% | 1.00 |
| Total maternal sleep duration, hours/day | 6.5 (1.7) | 6.6 (1.6) | 6.5 (1.8) | 0.65 |
| % or Mean (SD) | ||||
| Infant | ||||
| Female | 56% | 50% | 71% | 0.09 |
| Birth weight, kg | 3.42 (0.44) | 3.51 (0.45) | 3.40 (0.42) | 0.53 |
| Daytime sleep duration, hours/day | 7.7 (1.7) | 7.6 (1.9) | 7.9 (1.5) | 0.49 |
| Nocturnal sleep duration, hours/day | 8.3 (1.6) | 8.2 (1.6) | 8.5 (1.5) | 0.38 |
| Settling time, hours/day | 0.82 (0.87) | 0.93 (0.95) | 0.42 (0.31) | 0.04 |
| Number of nighttime awakenings | 3.0 (1.2) | 2.9 (1.2) | 3.2 (1.1) | 0.46 |
| Nocturnal wakefulness, hours/day | 2.7 (4.5) | 3.1 (5.3) | 1.9 (1.1) | 0.08 |
P-values are from Fisher’s exact t-test for normally distributed variables or Kruskal–Wallis test for non-normally distributed variables
Based on the edinburgh postpartum depression scale
Primary Behavioral Outcomes
At 6 months postpartum, we did not find any differences in maternal health behaviors between intervention and usual care (Tables 3 and 4). Infants in the intervention practices were less likely than infants in the usual care practice to be introduced to solid foods before 4 months of age (57% vs. 82%; P = 0.04) and viewed slightly less television (1.2 h/day vs. 1.5 h/day; P = 0.07) (Table 3). Compared to usual care infants, intervention infants had larger increases in their nocturnal sleep duration from baseline to follow up (mean increase 1.9 vs. 1.3 h/d; P = 0.05); larger reductions in settling time (mean reduction −0.70 vs. −0.10 h/d; P = 0.02); and larger reductions in hours/day of nighttime wakefulness (mean reduction −2.9 vs. −1.5 h/d; P = 0.08). There were no differences at 6 months on breastfeeding duration or exclusivity, or response to infant satiety cues.
Table 3.
Maternal and infant health behaviors at 6 months postpartum, by intervention assignment
| Maternal behaviors | Overall N = 80 | Intervention N = 58 | Usual care N = 22 | P-value |
|---|---|---|---|---|
| Mean (SD) | ||||
| Diet | ||||
| Fast food intake, servings/week | 0.5 (0.5) | 0.6 (0.6) | 0.5 (0.4) | 0.68 |
| Fruit and vegetable intake, servings/day | 3.9 (1.3) | 3.7 (1.2) | 4.2 (1.4) | 0.14 |
| Sugar-sweetened beverage intake, servings/day | 3.0 (6.6) | 3.4 (7.6) | 2.0 (2.3) | 0.51 |
| Television viewing | ||||
| Daily TV/video viewing, hours/day | 1.4 (1.1) | 1.4 (1.1) | 1.5 (0.87) | 0.45 |
| Sleep duration | ||||
| Daily sleep duration, hours/day | 6.9 (1.0) | 6.9 (1.1) | 6.9 (1.0) | 0.77 |
| Physical activity | ||||
| Daily physical activity, hours/day | 1.2 (0.89) | 1.1 (0.79) | 1.5 (1.1) | 0.18 |
|
| ||||
| Infant behaviors | Overall N = 80 | Intervention N = 58 | Usual care N = 22 | P-value |
|
| ||||
| % or Mean (SD) | ||||
| Infant feeding | ||||
| Breastfeeding duration, weeks | 22.5 (8.0) | 22.7 (7.8) | 21.9 (8.5) | 0.72 |
| Exclusively breastfeeding at 6 months | 48% | 47% | 50% | 0.78 |
| Solid foods introduced < 4 months | 64% | 57% | 82% | 0.04 |
| Infant feeding behavior | ||||
| Responsiveness to infant satiety score, unitsa | 11.9 (1.7) | 11.9 (1.8) | 11.8 (1.6) | 0.88 |
| The best way to soothe a crying baby is to feed her, % strongly agree/agree | 16% | 12% | 24% | 0.17 |
| Infant TV exposure | ||||
| Daily TV viewing, hours/day | 1.3 (2.0) | 1.2 (2.1) | 1.5 (1.5) | 0.07 |
| TV in the room where infant sleeps | 19% | 21% | 14% | 0.54 |
Score ranges from 4 to 16 with higher score indicating greater responsiveness to satiety
Table 4.
Change from baseline to 6 months postpartum in maternal and infant sleep behaviors, by intervention assignment
| Change in behavior | Intervention (N = 58)
|
Usual care (N = 22)
|
P-value | ||||
|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) |
6-months | Change | Baseline | 6-months | Change | ||
| Maternal behaviors | |||||||
| Daily sleep duration, hours/day | 6.6 (1.6) | 6.9 (1.1) | 0.28 (1.6) | 6.5 (1.8) | 6.9 (1.0) | 0.45 (1.8) | 0.59 |
| Infant behaviors | |||||||
| Daytime sleep duration, hours/day | 7.6 (1.9) | 3.3 (1.1) | −4.3 (1.7) | 7.9 (1.5) | 3.4 (0.9) | −4.6 (1.5) | 0.05 |
| Nocturnal sleep duration, hours/day | 8.2 (1.6) | 10.0 (1.2) | 1.9 (1.7) | 8.5 (1.5) | 9.8 (1.6) | 1.3 (2.5) | 0.05 |
| Settling time, hours/day | 0.90 (0.9) | 0.30 (0.2) | −0.70 (1.0) | 0.40 (0.3) | 0.30 (0.2) | −0.10 (0.4) | 0.02 |
| Number of nighttime awakenings | 2.9 (1.2) | 1.3 (1.0) | −1.6 (1.6) | 3.2 (1.1) | 1.9 (1.2) | −1.2 (1.9) | 0.34 |
| Nocturnal wakefulness, hours/day | 3.1 (5.3) | 0.3 (0.3) | −2.9 (5.8) | 1.9 (1.1) | 0.3 (0.3) | −1.5 (1.1) | 0.08 |
Secondary Anthropometric Outcomes
We did not find any group differences in maternal postpartum weight retention (PPWR) at 6 months (mean PPWR among intervention participants = 1.75 kg vs. 0.48 kg among usual care participants; P = 0.08). Change in weight-for-length z-score from birth to 6 months appeared lower among intervention infants compared to usual care infants (0.24 units vs. 0.50 units) but the difference was not statistically significant (P = 0.44). We also observed a trend toward fewer intervention infants being in the highest quartile of weight-for-length z-score at 6 months of age (22% vs. 42%; P = 0.06).
Process Outcomes
Process feedback suggests the program was helpful in guiding decisions on introducing solid foods, infant sleep, and infant media exposure (32, 27 and 33% of intervention mothers, respectively, found it “a lot helpful”) but less helpful in guiding mothers’ decisions about their own eating, physical activity, and sleep habits (14, 18, and 9%, respectively, found it “a lot helpful”) (Table 5).
Table 5.
Mothers’ and pediatric clinicians’ perceptions of the feasibility and acceptability of the First Steps for Mommy and Me intervention
| Feasibility and acceptability measures of mothers, N = 58 | Response options |
|---|---|
| Mothers’ satisfaction with intervention | N (%) “somewhat or very” |
| Satisfied with experience in the First Steps for Mommy and Me | 55 (97) |
| Satisfied with the counseling received during health educator calls | 52 (90) |
| How helpful was First Steps for Mommy and Me in guiding your approach to | N (%) “a lot” |
| How long you breastfed and when/if to introduce formula | 11 (19) |
| When to introduce solid food or juice to your baby | 18 (32) |
| Your attention to your baby’s hunger and fullness signals | 14 (25) |
| Your approach to your baby’s sleep | 15 (27) |
| Your approach to your baby’s media exposure | 19 (33) |
| How helpful was First Steps for Mommy and Me in guiding your approach to | N (%) “a lot” |
| Your eating habits | 8 (14) |
| Your own media exposure | 9 (16) |
| Your sleep habits | 5 (9) |
| Your physical activity | 10 (18) |
| Would recommend First Steps for Mommy and Me to friends and family | 54 (93) |
|
| |
| Feasibility and acceptability measures of pediatric clinicians, N = 7 | N (%) “very or extremely” |
|
| |
| How successful do you feel the study has been in promoting healthy behaviors in your mommy and me patients | 4 (57) |
| How useful would it be to continue a mommy and me type program in your practice once the study is completed | 4 (57) |
| How willing would you be to incorporate counseling to mothers about their own postpartum health into your routine practice | 2 (29) |
| How confident do you feel in providing counseling to mothers about their own postpartum health | 1 (14) |
| How useful are each of the following mommy and me components for you and your practice | |
| Brief focused negotiation training | 7 (100) |
| Printed educational materials for parents | 7 (100) |
Of the 11 pediatric clinicians at the intervention practices, 7 (64%) completed the brief process survey. The majority of respondents were not confident in their ability to counsel mothers about their own postpartum behaviors. All respondents found the training on brief focused negotiation and parent educational materials to be very or extremely helpful (Table 5).
Discussion
In this pilot intervention study of postpartum mothers and their infants, we found that a program of brief focused negotiation by pediatricians, individual coaching by health educators using motivational interviewing, and group parenting workshops tended to improve infant feeding (delaying introduction of solids), sleep and media exposure, but had less impact on mothers’ own health-related behaviors. While our study did not have sufficient power to detect differences in maternal and infant weight status, our preliminary results also showed that infants whose mothers participated in the intervention tended towards having lower change in weight-for-length z-score in the first 6 months of life and were less likely to be in the highest quartiles of weight-for-length compared to usual care infants.
The postpartum period is an opportune but understudied time for integrated interventions to promote healthful behaviors for mother-infant pairs [30]. Although there are several published interventions to promote weight loss in the postpartum period for mothers [31] and one published intervention to prevent excess infant weight gain, [6] the review of the literature and currently funded clinical trials indicates that no postpartum interventions have been completed with dual mother-infant behavioral outcomes. Our findings lend support to the feasibility and acceptability of a postpartum intervention for mother-infant pairs and provides evidence that prevention during this period may be effective in influencing mothers’ decision making for their infants’ feeding, media exposure, and sleep practices.
Several interventions to promote weight loss and improve nutrition and physical activity in the postpartum period have been tested. A Cochrane Review of studies published though 2006 identified 6 postpartum trials and found that the combination of both diet and physical activity as intervention targets was most effective in helping women lose weight after childbirth [31]. However, a recent intervention among 450 postpartum overweight and obese women in North Carolina did not achieve any differences in diet, physical activity, or weight change [32, 33]. This intervention included 10 physical activity classes and 8 healthy-eating classes, which were variably attended. The investigators concluded that home-based interventions delivered via mail, telephone, or Internet/e-mail may be more feasible and successful among busy postpartum mothers. Our intervention was similarly not effective in influencing maternal postpartum health behaviors.
Several reasons may explain our null findings for maternal health outcomes. First, given limited resources for our pilot intervention, we were unable to recruit women prior to delivery or engage the obstetric providers in behavioral counseling of women prior to and after delivery. It is possible that preventive efforts beginning in pregnancy could be more effective in engaging women in interventions and in helping women prioritize their own health behavior goals prior to the birth of their newborn. Relationship building with research staff during pregnancy could also be helpful in sustaining mothers’ level of interest in intervention components. Second, although the pediatric clinicians expressed willingness to counsel women about their own postpartum health, they lacked confidence in their ability to do so. Thus, interventions delivered solely through pediatric primary care practices to support maternal postpartum health are likely to not be effective unless pediatricians are better trained in this area. Third, although we attempted to address maternal-infant behaviors as combined outcomes, e.g. improving infant sleep to improve maternal sleep, greater efforts may be required that use infant health and well being as a motivator for maternal behavior change or that involve activities that a mother could do with her infant, e.g. Stroller Fit®, a physical fitness program for postpartum mothers and their babies.
Few interventions have focused on improving healthful nutrition and physical activity behaviors in infancy to promote weight management. A systematic review by Whitlock et al. [34] that examined weight management interventions in clinical and non-clinical community settings found that available research studies primarily enrolled children and adolescents ages 4–18 years and no studies targeted those less than 2 years of age, suggesting a significant research gap for this age range. To our knowledge, only one published intervention has focused on preventing excess infant weight gain. In a randomized controlled trial of 1,000 formula-fed infants, decreasing the protein content of formula resulted in a lower weight-for-length z-score at 2 years (β 0.20; 95% CI: 0.06, 0.34) compared to infants who received formula with higher protein content [6]. Other infant interventions are planned or ongoing but exclude maternal outcomes. Our study was unique in aiming to change both mother and infant behaviors, in effecting change at multiple levels (clinic and home via telephone and local workshops), and targeting multiple behaviors (not just choice of infant feeding) to influence early weight gain.
When interpreting our study, several limitations should be considered. First, the educational and income levels of mothers in this study were relatively high. Our results may not be generalizable to more socio-economically disadvantaged populations. Second, most of our measures were from maternal report, including breastfeeding duration and infant sleep. Mothers could exaggerate self-reported improvements in behaviors. This is a limitation of all behavioral interventions. Finally, the relatively small sample size did not allow enough power to detect significant changes in our weight-related behaviors.
In summary, we found that a multi-component postpartum intervention tended to improve infant weight-related behaviors. Our findings suggest that interventions targeting this life period are feasible, well accepted by parents and clinicians, can fill a significant gap in current obesity research, and provides a strong rationale for testing comprehensive interventions in early life to prevent obesity. However, to be maximally effective in improving outcomes for both mothers and infants, future interventions in this life period will need to include more pediatric clinician training and must actively engage women in setting their own behavior change goals [35, 36].
Acknowledgments
The authors would like to thank the participants and research staff for the First Steps for Mommy and Me study. This study was supported in part by grants from Harvard Medical School, Harvard Pilgrim Health Care, and by the Physician Faculty Scholars Program of the Robert Wood Johnson Foundation.
Footnotes
Conflicts of interest The authors have no conflicts of interest to disclose.
Contributor Information
Elsie M. Taveras, Email: Elsie_Taveras@hphc.org, Obesity Prevention Program, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, 133 Brookline Avenue, 6th Floor, Boston, MA 02215, USA. Division of General Pediatrics, Children’s Hospital, Boston, MA, USA
Katherine Blackburn, Department of Pediatrics, Children’s Mercy Hospitals and Clinics, Center for Weight Management, Kansas City, MO, USA.
Matthew W. Gillman, Obesity Prevention Program, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, 133 Brookline Avenue, 6th Floor, Boston, MA 02215, USA. Department of Nutrition, Harvard School of Public Health, Boston, MA, USA
Jess Haines, Obesity Prevention Program, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, 133 Brookline Avenue, 6th Floor, Boston, MA 02215, USA.
Julia McDonald, Obesity Prevention Program, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, 133 Brookline Avenue, 6th Floor, Boston, MA 02215, USA.
Sarah Price, Obesity Prevention Program, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, 133 Brookline Avenue, 6th Floor, Boston, MA 02215, USA.
Emily Oken, Obesity Prevention Program, Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, 133 Brookline Avenue, 6th Floor, Boston, MA 02215, USA.
References
- 1.Kim J, et al. Trends in overweight from 1980 through 2001 among preschool-aged children enrolled in a health maintenance organization. Obesity. 2006;14(7):1107–1112. doi: 10.1038/oby.2006.126. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Baird J, et al. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331(7522):929. doi: 10.1136/bmj.38586.411273.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monteiro PO, Victora CG. Rapid growth in infancy and childhood and obesity in later life—a systematic review. Obesity Reviews. 2005;6(2):143–154. doi: 10.1111/j.1467-789X.2005.00183.x. [DOI] [PubMed] [Google Scholar]
- 5.Taveras EM, et al. Higher adiposity in infancy associated with recurrent wheeze in a prospective cohort of children. Journal of Allergy Clinical Immunology. 2008;121(5):1161–1166. doi: 10.1016/j.jaci.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koletzko B, et al. Lower protein in infant formula is associated with lower weight up to age 2 y: A randomized clinical trial. American Journal of Clinical Nutrition. 2009;89(6):1836–1845. doi: 10.3945/ajcn.2008.27091. [DOI] [PubMed] [Google Scholar]
- 7.Gunderson EP, et al. Excess gains in weight and waist circumference associated with childbearing: The coronary artery risk development in young adults study (CARDIA) International Journal of Obesity and Related Metabolic Disorders. 2004;28:525–535. doi: 10.1038/sj.ijo.0802551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith DE, et al. Longitudinal changes in adiposity associated with pregnancy. The CARDIA Study. JAMA. 1994;271:1747–1751. [PubMed] [Google Scholar]
- 9.Ohlin A, Rossner S. Maternal body weight development after pregnancy. International Journal of Obesity. 1990;14:159–173. [PubMed] [Google Scholar]
- 10.Stotland NE, et al. Body mass index, provider advice, and target gestational weight gain. Obstetrics and Gynecology. 2005;105(3):633–638. doi: 10.1097/01.AOG.0000152349.84025.35. [DOI] [PubMed] [Google Scholar]
- 11.Taffel SM, Keppel KG, Jones GK. Medical advice on maternal weight gain and actual weight gain. Results from the 1988 national maternal and infant health survey. Annals of the New York Academy of Sciences. 1993;678:293–305. doi: 10.1111/j.1749-6632.1993.tb26132.x. [DOI] [PubMed] [Google Scholar]
- 12.Cogswell ME, et al. Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstetrics and Gynecology. 1999;94(4):616–622. doi: 10.1016/s0029-7844(99)00375-0. [DOI] [PubMed] [Google Scholar]
- 13.Taveras EM, et al. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics. 2003;112(1):108–115. doi: 10.1542/peds.112.1.108. [DOI] [PubMed] [Google Scholar]
- 14.Tyler DO, Horner SD. Family-centered collaborative negotiation: a model for facilitating behavior change in primary care. Journal of the American Academy of Nurse Practitioners. 2008;20(4):194–203. doi: 10.1111/j.1745-7599.2007.00298.x. [DOI] [PubMed] [Google Scholar]
- 15.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. American Journal of Preventive Medicine. 2001;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 16.Miller W, Rollnick S. Motivational interviewing. 2. New York: Guilford Press; 2002. [Google Scholar]
- 17.Rollnick S, Butler C. Health behavior change: A guide for practitioners. Edinburgh, Scotland: Churchill Livingstone; 1999. [Google Scholar]
- 18.Rifas-Shiman SL, et al. PrimeScreen, a brief dietary screening tool: Reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutrition. 2001;4:249–254. doi: 10.1079/phn200061. [DOI] [PubMed] [Google Scholar]
- 19.Taveras EM, et al. Association of consumption of fried food away from home with body mass index and diet quality in older children and adolescents. Pediatrics. 2005;116(4):e518–e524. doi: 10.1542/peds.2004-2732. [DOI] [PubMed] [Google Scholar]
- 20.Pereira MA, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 21.Greenwood JL, et al. Creating a clinical screening questionnaire for eating behaviors associated with overweight and obesity. Journal of the American Board of Family Medicine. 2008;21(6):539–548. doi: 10.3122/jabfm.2008.06.070265. [DOI] [PubMed] [Google Scholar]
- 22.Oken E, et al. Television, walking, and diet: Associations with postpartum weight retention. American Journal of Preventive Medicine. 2007;32(4):305–311. doi: 10.1016/j.amepre.2006.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gunderson EP, et al. Association of fewer hours of sleep at 6 months postpartum with substantial weight retention at 1 year postpartum. American Journal of Epidemiology. 2008;167(2):178–187. doi: 10.1093/aje/kwm298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oken E, et al. Associations of physical activity and inactivity before and during pregnancy with glucose tolerance. Obstetrics and Gynecology. 2006;108(5):1200–1207. doi: 10.1097/01.AOG.0000241088.60745.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–548. [PubMed] [Google Scholar]
- 26.Thompson AL, et al. Development and validation of the infant feeding style questionnaire. Appetite. 2009;53(2):210–221. doi: 10.1016/j.appet.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sadeh A. A brief screening questionnaire for infant sleep problems: Validation and findings for an internet sample. Pediatrics. 2004;113(6):e570–e577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention and National Center for Health Statistics. CDC growth charts: United States. 2000 Available at: http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/datafiles.htm.
- 29.Cox JL, et al. Validation of the edinburgh postnatal depression scale (EPDS) in non-postnatal women. Journal of Affective Disorders. 1996;39(3):185–189. doi: 10.1016/0165-0327(96)00008-0. [DOI] [PubMed] [Google Scholar]
- 30.Paul IM, et al. Opportunities for the primary prevention of obesity during infancy. Advances in Pediatrics. 2009;56:107–133. doi: 10.1016/j.yapd.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amorim AR, Linne YM, Lourenco PM. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database of Systematic Reviews. 2007;3:CD005627. doi: 10.1002/14651858.CD005627.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Ostbye T, et al. Active mothers postpartum (AMP): Rationale, design, and baseline characteristics. Journal of Womens Health (Larchmt) 2008;17(10):1567–1575. doi: 10.1089/jwh.2007.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ostbye T, et al. Active mothers postpartum: A randomized controlled weight-loss intervention trial. American Journal of Preventive Medicine. 2009;37(3):173–180. doi: 10.1016/j.amepre.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whitlock EP, et al. Effectiveness of weight management interventions in children: A targeted systematic review for the USPSTF. Pediatrics. 2010;125(2):e396–e418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 35.Olson CM, Strawderman MS, Reed RG. Efficacy of an intervention to prevent excessive gestational weight gain. American Journal of Obstetrics and Gynecology. 2004;191(2):530–536. doi: 10.1016/j.ajog.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 36.Claesson IM, et al. Weight gain restriction for obese pregnant women: a case-control intervention study. BJOG. 2008;115(1):44–50. doi: 10.1111/j.1471-0528.2007.01531.x. [DOI] [PubMed] [Google Scholar]
- 37.Taveras EM, et al. To what extent is the protective effect of breastfeeding on future overweight explained by decreased maternal feeding restriction? Pediatrics. 2006;118(6):2341–2348. doi: 10.1542/peds.2006-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim J, Peterson KE. Association of infant child care with infant feeding practices and weight gain among US infants. Archives of Pediatrics and Adolescent Medicine. 2008;162(7):627–633. doi: 10.1001/archpedi.162.7.627. [DOI] [PubMed] [Google Scholar]
- 39.Baker JL, et al. Maternal prepregnant body mass index, duration of breastfeeding, and timing of complementary food introduction are associated with infant weight gain. American Journal of Clinical Nutrition. 2004;80(6):1579–1588. doi: 10.1093/ajcn/80.6.1579. [DOI] [PubMed] [Google Scholar]
- 40.Gortmaker SL, et al. Television viewing as a cause of increasing obesity among children in the United States, 1986–1990. Archives of Pediatrics and Adolescent Medicine. 1996;150(4):356–362. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- 41.Robinson TN. Reducing children’s television viewing to prevent obesity: A randomized controlled trial. JAMA. 1999;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 42.Armstrong CA, et al. Children’s television viewing, body fat, and physical fitness. American Journal of Health Promotion. 1998;12(6):363–368. doi: 10.4278/0890-1171-12.6.363. [DOI] [PubMed] [Google Scholar]
- 43.Proctor MH, et al. Television viewing and change in body fat from preschool to early adolescence: The Framingham children’s study. International Journal of Obesity and Related Metabolic Disorders. 2003;27(7):827–833. doi: 10.1038/sj.ijo.0802294. [DOI] [PubMed] [Google Scholar]
- 44.Miller SA, et al. Association between television viewing and poor diet quality in young children. International Journal of Pediatric Obesity. 2008;3(3):168–176. doi: 10.1080/17477160801915935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adachi-Meija AM, et al. Children with a TV in their bedroom at higher risk for being overweight. International Journal of Obesity (Lond) 2007;31(4):644–651. doi: 10.1038/sj.ijo.0803455. [DOI] [PubMed] [Google Scholar]
- 46.Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. Journal of the American Dietetic Association. 2007;107(1):53–61. doi: 10.1016/j.jada.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 47.Tikotzky L, et al. Sleep and physical growth in infants during the first 6 months. Journal of Sleep Research. 2009;19(1):103–110. doi: 10.1111/j.1365-2869.2009.00772.x. [DOI] [PubMed] [Google Scholar]
- 48.Taveras EM, et al. Short sleep duration in infancy and risk of childhood overweight. Archives of Pediatrics and Adolescent Medicine. 2008;162(4):305–311. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]