Abstract
Objective
To evaluate the incidence and treatment of CSF leaks after resection of vestibular schwannomas and to propose a treatment algorithm for their management.
Study Design
Retrospective chart review.
Setting
Tertiary referral center.
Patients
Review of 1,922 subjects who underwent resection of vestibular schwannomas from 1970 through 2010.
Intervention
Surgical resection of vestibular schwannoma.
Main Outcome Measures
Patient demographics, surgical approach used, CSF leak incidence, meningitis, treatment and success in the management of CSF leaks.
Results
Postoperative CSF leaks were observed in 12.9% of our patients. There was no significant difference between the type of approach and the presence of CSF leak with translabyrinthine, suboccipital and middle fossa CSF leak rates of 12%, 12%, and 13% respectively (p=0.07). Patients presented with a wound leak or rhinorrhea almost equally. Ultimately, 92% of patients with rhinorrhea underwent surgical intervention. The probability of a patient with rhinorrhea requiring a second intervention was higher when the initial intervention was conservative rather than surgical. However, the probability of a patient with a wound leak requiring a second intervention was essentially the same when initially treated conservatively or surgically.
Conclusion
Our data suggests that there is no difference in CSF leak rates between the different surgical approaches. The appropriate treatment strategy is dependent on the presentation of the CSF. While conservative treatment is effective for managing wound leaks, it is less effective in managing patients with rhinorrhea. Therefore, surgical treatments should play an early role in the treatment algorithm of patients with CSF rhinorrhea.
Keywords: vestibular schwannoma, acoustic neuroma, CSF leak
Introduction
Since the mid 20th century, postoperative cerebrospinal fluid (CSF) leaks have been a well-established complication of vestibular schwannoma surgery. Dandy first described CSF leaks as a complication after suboccipital craniotomy for the removal of a vestibular schwannoma.1 Because CSF leak rates were common and complications of leaks were significant, multiple attempts have been made to decrease leak rates. In the 1960s, introduction of the abdominal fat graft significantly reduced the postoperative CSF leak rates in the translabyrinthine approach.2 In addition, muscle and bone wax were later introduced for closure in the retrosigmoid approach. Because CSF leaks have continued, surgeons have modified closure techniques and have included a host of different materials to reduce the CSF leak rate even further.3
Today, CSF leaks stand as the second most common complication in the postoperative period. Postoperative CSF leak rates reported in the literature range from 2% to 30%4-7 but the average leak rate appears to be approximately 10%.8 Because CSF leaks can lead to major complications such as meningitis, knowing when to treat a CSF leak conservatively or surgically is the most difficult part of the management.
The objective of this study was to analyze our management experience with postoperative CSF leaks over the last 40 years and present a treatment algorithm based on this data that will help guide future management.
Materials and Methods
Data Collection
A retrospective chart review was conducted on 1,922 patients who had undergone vestibular schwannoma surgery between 1970 and 2010. Incidence and management of postoperative CSF leaks were evaluated. Variables included patient age, gender, approach for tumor resection, tumor size, presentation of CSF leaks, type of interventions to manage the leak, and time periods between surgery and interventions for CSF leaks.
A CSF leak was classified as either a wound leak or rhinorrhea. A CSF leak was defined as a wound leak if clear fluid was observed draining through the wound or if there was a subcutaneous collection of CSF fluid. A CSF leak was defined as rhinorrhea when clear fluid was observed consistently dripping through the ipsilateral nostril.
Conservative treatment is considered an intervention in this study and includes any combination of diamox, elevation of head of bed, oversewing the wound, or placement of a lumbar drain (LD). Surgical treatment includes any reexploration of the wound, shunt placement, or Eustachian tube ablation.
Statistical Analysis
To assess the efficacy of conservative or surgical management and determine the risk of requiring a second intervention, a logistic regression model was fit with the average tumor size (23.8 mm), intervention type, and leak type. Kaplan-Meier curves were plotted separately for each combination of intervention and leak type. Analysis was performed using R version 2.11.1 with significance defined on two-sided tests with a 0.05 significance level.
Results
Of the 1,922 patients who had undergone primary resection of a vestibular schwannoma, the translabyrinthine (TL) approach was used 75% of the time while the suboccipital (SO), middle fossa (MF), and combined approaches were used 13%, 5%, and 7% respectively. Figure 1 shows when the SO and MF approaches were introduced as surgical options at our institution and how much the TL, SO, and MF approaches were used over a 40-year period divided into 5-year increments.
Figure 1.
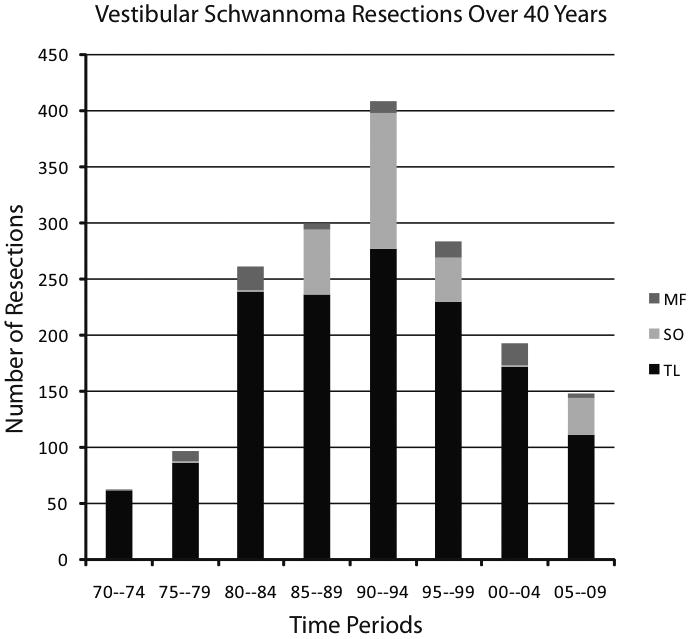
The evolution of surgical approaches and their utilization out our institution over a 40-year period. This figure demonstrates a trend at our institution, given the benign nature of vestibular schwannomas, to observe a large number of small tumors that show no evidence of tumor growth. This figure also demonstrates the influence of radiation therapy as a viable, non-surgical option.
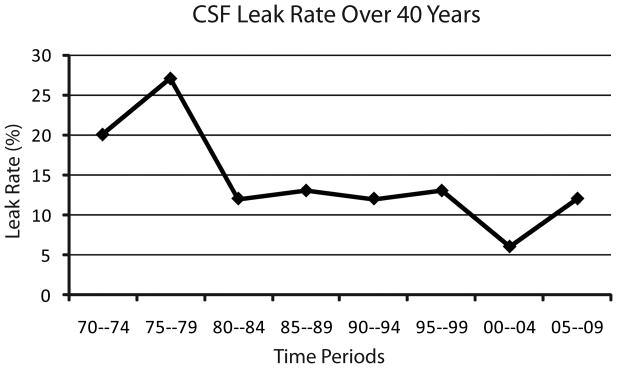
There were 248 postoperative CSF leaks for a rate of 12.9%. The CSF leak rates for the (TL), (SO), and (MF) approaches were 12%, 12%, and 13% respectively with no difference in leak rates between the approaches (p=0.07). However, combined approaches had a significantly higher leak rate of 26% (p<0.01) when compared to single approaches. (Table 1) The CSF leak rate at our institution has changed over time from a high of 27% from 1975-1979 to a low of 6% from 2000-2004. (Fig. 2)
Table 1. Descriptive Statistics by Surgery Type.
| TL (N=167) | SO (N=35) | MF (N=10) | Combined (N=36) | |
|---|---|---|---|---|
| CSF Leak rates | 12% | 12% | 13% | 26% |
| CSF Leak type | ||||
| Wound leak | 54% (91) | 32% (11) | 30% (3) | 64% (23) |
| Rhinorrhea | 46% (76) | 68% (23) | 70% (7) | 36% (13) |
| Initial Management | ||||
| Conservative | 56% (94) | 26% (9) | 40% (4) | 75% (27) |
| Surgical | 44% (73) | 74% (26) | 60% (6) | 25% (9) |
| Required 2nd intervention | 19% (31) | 9% (3) | 10% (1) | 11% (4) |
Abreviations: TL=translabyrinthine, SO=suboccipital, MF=middle fossa
Figure 2.
The change in CSF leak rates over 40 years at our institution.
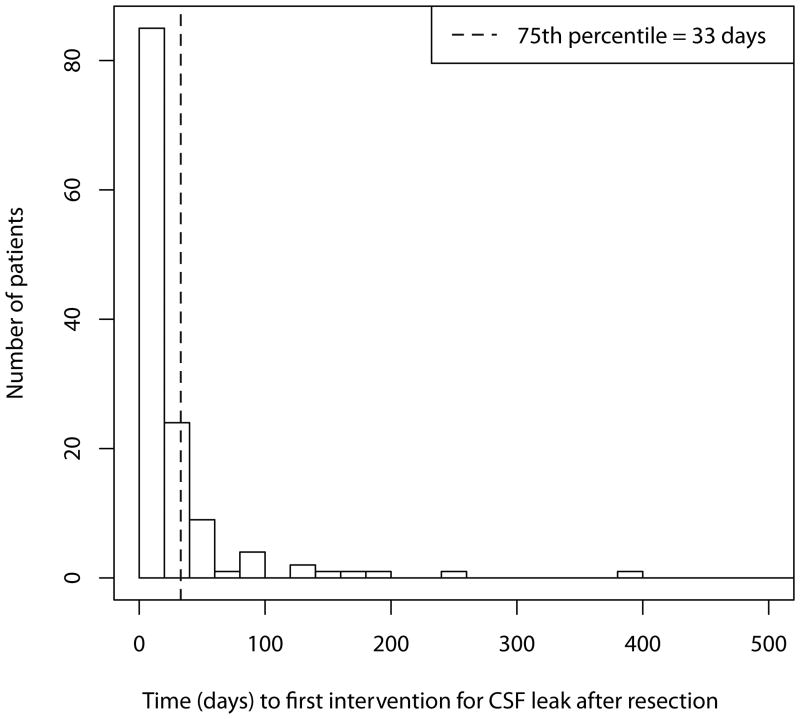
Seventy-five percent of patients who had a postoperative CSF leak had an intervention for the leak within 33 days of their original surgery. (Fig. 3) Those patients who persisted with a leak despite initial management, required subsequent treatment on average 38 days and 43 days after the first and second intervention respectively.
Figure 3.
Time to first intervention for a CSF leak following resection of a vestibular schwannoma. Note that 75% of patients underwent an intervention within 33 days of resection.
Patients presented with a wound leak 51% of the time and with rhinorrhea 49% of the time. Wound leak was the primary presentation after a TL approach 54% of the time (91/167) but only 32% (11/35) and 30% (3/10) after SO and MF approaches respectively. Rhinorrhea was the primary presentation after a TL approach 46% of the time (76/167) but was the primary presentation 68% (23/35) and 70% (7/10) of the time after SO and MF approaches respectively. (Table 1)
Overall, patients who presented with a wound leak were treated conservatively 91% (115/126) of the time, and of those treated conservatively only 10% (12/115) required a second intervention. However, of the 17 patients with rhinorrhea who were initially treated conservatively, 41% (7/17) of them needed a second intervention. Patients with rhinorrhea were initially treated surgically 86% (103/120) of the time and of those treated surgically, 21% (18/103) required a second intervention. (Table 2) Ultimately, 92% of patients with rhinorrhea underwent a surgical intervention at some point in their care.
Table 2. Descriptive Statistics by Leak Type and 1st Intervention.
| Wound Leak/Conservative (N=115) | Wound Leak/Surgical (N=11) | Rhinorrhea/Conservative (N=17) | Rhinorrhea/Surgical (N=103) | |
|---|---|---|---|---|
| Required 1 intervention | 90% (103) | 82% (9) | 59% (10) | 83% (85) |
| Required 2nd intervention | 10% (12) | 18% (2) | 41% (7) | 17% (18) |
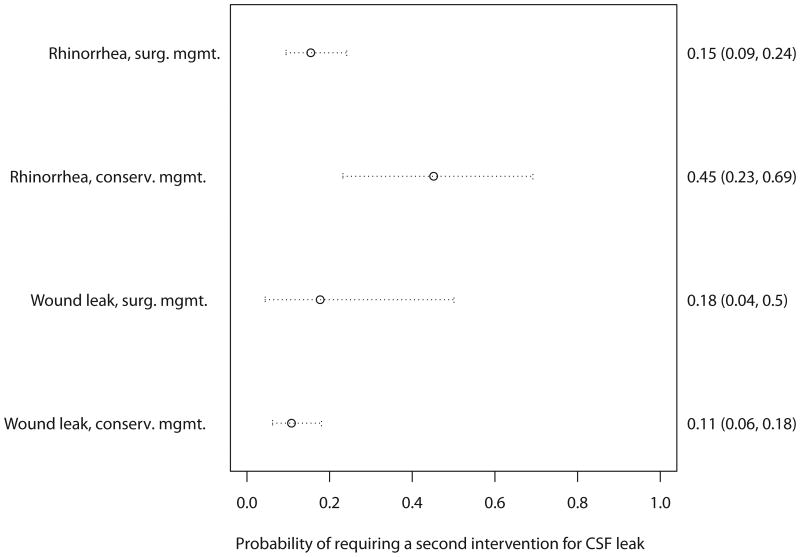
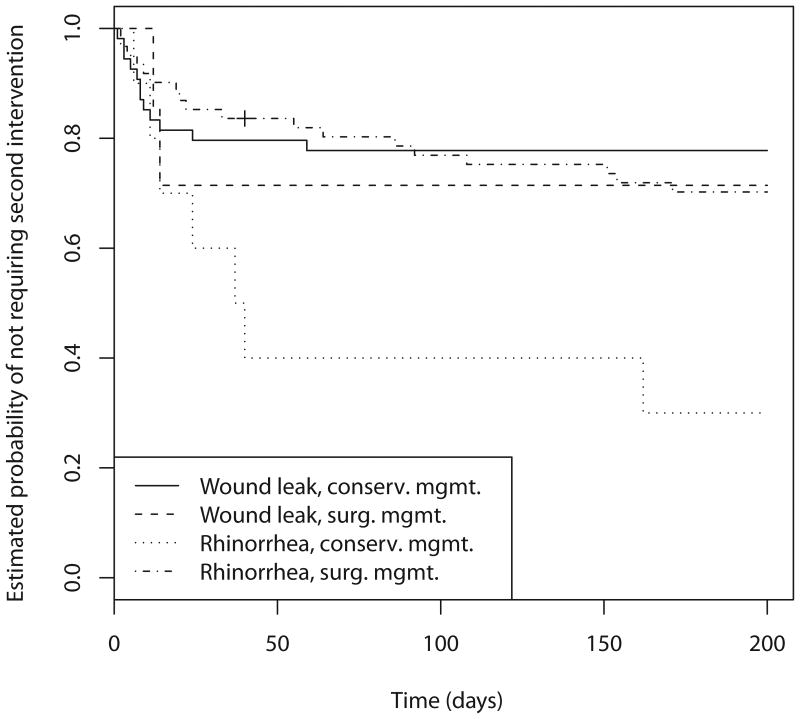
The probability of a patient with rhinorrhea requiring a second intervention was higher when treated conservatively rather than surgically, 0.45 (95% CI (0.23 - 0.69)) versus 0.15 (95% CI (0.09 - 0.24)) respectively. However, the probability of a patient with a wound leak requiring a second intervention was essentially the same when treated conservatively rather than surgically, 0.11 (95% CI (0.06 - 0.18)) versus 0.18 (95% CI (0.04 - 0.5)). (Fig. 4) These findings are also displayed as Kaplan-Meier curves. (Fig. 5)
Figure 4.
The probabilities of requiring a second intervention for a CSF leak based on the presentation of the CSF leak and the initial treatment.
Figure 5.
Kaplan-Meier curves showing the probability of not requiring a second intervention over time is plotted separately for each combination of intervention and leak type. Note that patients with rhinorrhea have a higher probability of needing a second intervention when initially treated conservatively rather than surgically.
The average tumor size in patients with a postoperative CSF leak was 23.8 mm. The median tumor size of patients requiring multiple interventions to repair their CSF leak was 20.0 mm (IQR 13.2 – 27.2) while the median tumor size of those requiring only one intervention was 23.0 mm (IQR 15.0 – 25.0). Among patients presenting with rhinorrhea, the median tumor size of patients requiring multiple interventions to repair their CSF leak was 19.0 mm (IQR 12.0 – 30.0) while the median tumor size of those requiring only one intervention was 16.0 mm (IQR 12.0 – 30.0).
Discussion
Postoperative CSF leaks are the second most common complication following vestibular schwannoma resection. We defined a CSF leak as CSF outside what constitutes a normal CSF barrier. CSF leaks are based on low-pressure flow due to air cell tracts, poor wound closure, or increased intracranial pressure. If an air cell tract is not obliterated during surgery or the wound is not closed sufficiently, then CSF will flow from the relatively high intracranial pressure system (7–15 mmHg) to the relatively low pressure systems of the Eustachian tube, middle ear space, or a dehiscence in the periosteal or skin layers. This same process occurs when there is an increase in CSF pressure caused by increased CSF production or decreased CSF absorption as commonly seen in the postoperative period. With an increase in CSF pressure, CSF needs an outlet, and if low-pressure systems are sealed, CSF can leak into subcutaneous locations.
Because different surgical approaches cause defects in different areas, controversy exists about whether or not different surgical approaches have different CSF leaks. Glasscock et al. showed a difference in CSF leak rates between surgical approaches while Becker et al. and Brennan et al. showed no difference.5,7,9 We encountered no significant difference between the type of surgical approach and the presence of CSF leaks (p>0.07). Translabyrinthine (TL), suboccipital (SO), and middle fossa (MF) approaches had leak rates of 12%, 12%, and 13% respectively. However, when compared to single approaches, combined approaches had a significantly higher leak rate of 26% (p<0.01) and presented as wound leaks 64% of the time. This may be due to the larger dural defect and increased inflammation associated with the combined approach. Figure 1 demonstrates the evolution of surgical approaches and their utilization out our institution over a 40-year period. This figure also demonstrates the influence of radiation therapy as a viable, non-surgical option and a trend at our institution, given the benign nature of vestibular schwannomas, to observe a large number of small tumors that show no evidence of tumor growth decreasing the number of patients requiring hearing preservation surgery. Only those patients with radiological evidence of growth and serviceable hearing are offered hearing preservation surgery. When choosing between TL and SO approaches for non-hearing preservation surgery, we prefer the TL approach. Our combined CSF leak rate averaged over the last 40 years was 12.9%, which is comparable to other studies.4-8 The CSF leak rate at our institution has changed over time from a high of 27% from 1975-1979 to a low of 6% from 2000-2004. (Fig. 2) This downward trend is historically consistent with the downward trend seen since the introduction of the abdominal fat graft in the 1960s and the modifications in closure techniques that have been introduced since then.
Though we found no significant difference in leak rates between the different surgical approaches, we did find a difference in the presentation of CSF leaks between the different surgical approaches. Our study showed that a wound leak is the most common CSF leak presentation following the TL approach (54%) but rhinorrhea is the most common CSF leak presentation following the SO (68%) and MF (70%) approaches. (Table 1) This can be explained by the meticulous obliteration of the Eustachian tube and middle ear space with fat and muscle grafts during the TL approach. Also, the MF and SO approaches require only bone waxing of the air cells and an occasional muscle graft in the IAC. If an air cell tract persists at the end of the IAC or into the mastoid, then CSF has an unobstructed path into the middle ear space and the Eustachian tube resulting in rhinorrhea.
Postoperative CSF leaks are associated with an increased risk of meningitis, prolonged hospital stay, and the possible need for revision surgery.5,7 Selesnick et al. reported that a CSF leak raises the postoperative risk of meningitis from 3% to 14%.8 In this study, 24% of our CSF patients developed either aseptic or bacterial meningitis.
Given the associated morbidities with postoperative CSF leaks, it is imperative to choose the right treatment modality. Conservative treatment includes any combination of diamox, elevation of head of bed, oversewing the wound, bed rest, or placing a lumbar drain.6,7,9,10 Surgical treatment includes reexploration of the wound, mastoid obliteration, eustachian tube obliteration, or shunt placement.6,7,9,10 Several studies suggest treatment algorithms that start with a trial of conservative management for almost all leaks and then escalate the treatments to surgical treatments if conservative management fails.6,7,10 Using a similar treatment algorithm, Becker et al. and Fishman et al. reported that the rate of return to the operating room for definitive treatment of CSF leaks was 27% and 46% respectively.6,7
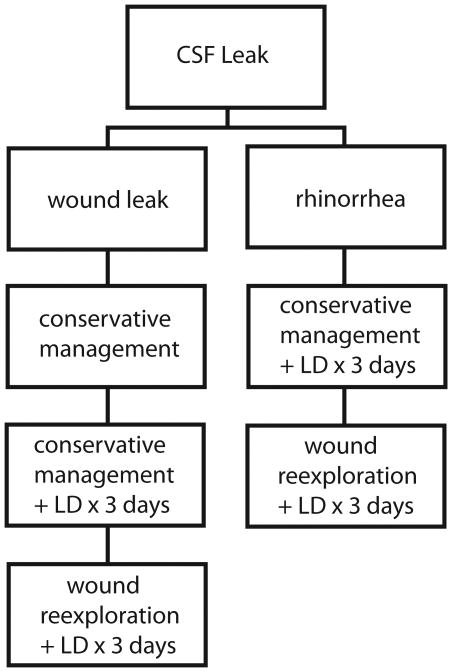
Our study showed that the presentation of the CSF leak could help guide management. In patients presenting with wound leaks, conservative management was effective 90% of time as the initial treatment. (Table 2) The probability of that patient requiring another intervention to stop the leak was 0.11. (Fig. 4) In patients presenting with rhinorrhea, conservative management was effective only 59% of the time as the initial treatment. (Table 2) The probability of that patient requiring a second intervention was 0.45. However, if a patient with rhinorrhea were treated initially with a surgical intervention, the probability of requiring a second intervention was only 0.15. (Fig. 4) Ultimately, 92% of patients with rhinorrhea underwent a surgical intervention for their CSF leak, but it must be noted that 86% of patients with rhinorrhea were initially treated with a surgical intervention. These results suggest that conservative management of wound leaks is an effective strategy. Initial conservative management of CSF rhinorrhea is a reasonable treatment strategy because sometimes it is successful allowing 59% of patients to avoid another trip to the operating room. However, it is imperative to be more aggressive with CSF rhinorrhea when initial conservative management fails due to the decreased success when treating rhinorrhea conservatively. Based on the results from this study, we have proposed a treatment algorithm based on CSF leak presentation. (Fig. 6)
Figure 6.
A treatment algorithm showing the treatment strategies of CSF leaks based on the presentation of the leak.
We recognize the limitations that accompany a non-randomized, retrospective study of this magnitude. Because this study includes patients treated over a 40-year time span, the surgical techniques and postoperative treatment strategies changed over time. Also, older charts were thinned to the most essential notes making it possible to miss documentation of conservative management. This could explain why so many of the CSF rhinorrhea patients appear to have been initially treated with surgery rather than conservative management. However, even if we assume that some if not many of the patients with rhinorrhea were initially treated with conservative management, the point of this study becomes even more pronounced: surgical interventions should play an early role in the treatment algorithm of patients with CSF rhinorrhea.
Conclusion
Our data suggests that there is no difference in CSF leak rates between the different surgical approaches. When CSF leaks do occur, they present almost equally as rhinorrhea or wound leaks. The presentation of the CSF leak seems to play an important role in determining the appropriate treatment strategy. Conservative treatment is an effective strategy for managing wound leaks but is much less effective in managing patients with rhinorrhea. Therefore, surgical treatments should play an early role in the treatment algorithm of patients with CSF rhinorrhea.
Acknowledgments
Supported in part by Vanderbilt CTSA grant 1 UL1 RR024975-01 from the National Center for Research Resources, National Institutes of Health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dandy W. Treatment of rhinorrhea and otorrhea. Arch Surg. 1944:75–85. [Google Scholar]
- 2.Montgomery WW, Ojemann RG, Weiss AD. Suboccipital-translabyrinthine approach for acoustic neuroma. Arch Otolaryngol. 1966;83:566–9. doi: 10.1001/archotol.1966.00760020568013. [DOI] [PubMed] [Google Scholar]
- 3.Goddard JC, Oliver ER, Lambert PR. Prevention of cerebrospinal fluid leak after translabyrinthine resection of vestibular schwannoma. Otol Neurotol. 2010;31:473–7. doi: 10.1097/MAO.0b013e3181cdd8fc. [DOI] [PubMed] [Google Scholar]
- 4.Fishman AJ, Hoffman RA, Roland JT, Jr, Lebowitz RA, Cohen NL. Cerebrospinal fluid drainage in the management of CSF leak following acoustic neuroma surgery. Laryngoscope. 1996;106:1002–4. doi: 10.1097/00005537-199608000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Glasscock ME, 3rd, Kveton JF, Jackson CG, Levine SC, McKennan KX. A systematic approach to the surgical management of acoustic neuroma. Laryngoscope. 1986;96:1088–94. doi: 10.1288/00005537-198610000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Fishman AJ, Marrinan MS, Golfinos JG, Cohen NL, Roland JT., Jr Prevention and management of cerebrospinal fluid leak following vestibular schwannoma surgery. Laryngoscope. 2004;114:501–5. doi: 10.1097/00005537-200403000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Becker SS, Jackler RK, Pitts LH. Cerebrospinal fluid leak after acoustic neuroma surgery: a comparison of the translabyrinthine, middle fossa, and retrosigmoid approaches. Otol Neurotol. 2003;24:107–12. doi: 10.1097/00129492-200301000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Selesnick SH, Liu JC, Jen A, Newman J. The incidence of cerebrospinal fluid leak after vestibular schwannoma surgery. Otol Neurotol. 2004;25:387–93. doi: 10.1097/00129492-200405000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Brennan JW, Rowed DW, Nedzelski JM, Chen JM. Cerebrospinal fluid leak after acoustic neuroma surgery: influence of tumor size and surgical approach on incidence and response to treatment. J Neurosurg. 2001;94:217–23. doi: 10.3171/jns.2001.94.2.0217. [DOI] [PubMed] [Google Scholar]
- 10.Selesnick SH, Liu JC, Jen A, Carew JF. Management options for cerebrospinal fluid leak after vestibular schwannoma surgery and introduction of an innovative treatment. Otol Neurotol. 2004;25:580–6. doi: 10.1097/00129492-200407000-00027. [DOI] [PubMed] [Google Scholar]